Abstract
Objective
This study was conducted to examine the 12-month effects on depression and depressive symptoms of a group-based cognitive-behavioral preventive intervention for middle school students (Positive Thoughts and Actions, or PTA), relative to a brief, individually administered supportive intervention (Individual Support Program, or ISP).
Method
A randomized clinical trial was conducted with 120 early adolescents (73 girls and 47 boys; age 12–14 years) drawn from a school-based population who had elevated depressive symptoms. Youths completed measures of depressive symptoms at baseline, post-intervention, and 6 and 12 months into the follow-up phase. Measures of internalizing problems, externalizing problems, school adjustment, interpersonal relationships, and health behavior were obtained from parents and/or youth.
Results
Multilevel models indicated that the effect of PTA on youth-reported depressive symptoms persisted until 12-month follow-up; d = .36 at post-intervention, d =.24 at 6-month follow-up, and d = .21 at 12-month follow-up. PTA youths also reported lower internalizing symptoms at post-intervention, d = .44, and at 12-month follow-up, d = .39. Time-limited effects were found for parent-reported internalizing symptoms and health behavior. Onset of new depressive episodes did not differ based on intervention group (21% ISP; 17% PTA).
Conclusions
Results demonstrate support for the long-term efficacy of PTA, a cognitive-behavioral preventive intervention in which youths engage in personal goal-setting and practice social-emotional skills.
Keywords: depression, prevention, intervention, indicated, school-based
The proportion of youth experiencing depressive disorders increases sharply from childhood to late adolescence (Lewinsohn, Clarke, Seeley, & Rohde, 1994). Even at sub-clinical levels, depressive symptoms impair functioning (Fergusson, Horwood, Ridder, & Beautrais, 2005) and increase risk for later depression (Klein, Shankman, Lewinsohn, & Seeley, 2009). Financial expenditures to treat youth depression are significant (Lynch & Clarke, 2006). In light of the negative ramifications of youth depression, efforts to prevent youth depression are important, especially those that maintain effects after the program ends. According to recent meta-analyses, depression prevention programs are efficacious at post-intervention (Cohen’s d ranges from .16 to .30), but effects diminish at follow-up (d ranges from .10 to .20) (Horowitz & Garber, 2006; Merry & Stasiak, 2012; Stice, Shaw, Bohon, Marti, & Rohde, 2009).
Although evidence is limited, longer-sustained effects of prevention programs may be even more difficult to achieve when the comparison condition controls for some therapeutic components. For instance, Gillham et al. (2007) compared the effects of Penn Resiliency Program (PRP) to a control that included adult attention and social support, the Penn Enhancement Program (PEP), for middle school students not meeting criteria for major depressive disorder (MDD) including those with elevated symptoms. Relative to PEP, PRP participants did not show reductions in depressive symptoms over the 3-year follow-up. Stice, Rohde, Gau, & Wade (2010) evaluated the effects of a brief cognitive-behavioral program for high school students with elevated depressive symptoms, compared to three active control conditions. In the first control condition, students attended weekly groups that provided support but did not address cognitive-behavioral skills (supportive expressive). In the second control condition, participants were provided with a cognitive-behavioral self-help book for depression (bibliotherapy). In the third control condition, youths received educational pamphlets that described major depression and treatment options (brochure). Although intervention group participants showed greater reduction in symptoms compared to the supportive-expressive, bibliotherapy, and brochure controls at post-intervention (Stice, Rohde, Seeley, & Gau, 2008), these differences disappeared by one-year follow-up (Stice, Rohde, Gau, & Wade, 2010).
Data supporting the efficacy of prevention programs in reducing risk for onset of a mood disorder are similarly mixed. Some studies show that episodes of depression and/or dysthymia are significantly reduced in the intervention group relative to no-treatment control (Arnarson & Craighead, 2011; Clarke et al., 1995; Stice et al., 2010), while others find no differences (Sheffield et al., 2006). Only one trial to date has tested the impact of school-based depression prevention on the onset of diagnostic outcomes against an active control. In that trial, 14% of cognitive-behavioral participants developed major depression, not significantly lower than supportive-expressive condition (14%) or cognitive-behavioral bibliotherapy (3%), but significantly lower than brochure controls (23%) (Stice et al., 2010). The limited data to date suggest that the development of depression prevention programs that have sustained efficacy over the long term remains a public health priority.
We previously described the post-intervention outcomes (McCarty, Violette, Duong, Cruz, & McCauley, 2013) for Positive Thoughts and Actions (PTA), a manualized and developmentally tailored school-based depression prevention program. PTA was designed to address key factors that impact depressive symptoms, including diminished health behaviors, academic stress, and interpersonal problems. Control group participants received an Individual Support Program (ISP), a 45–90 minute interview in which the interviewer summarized and empathized with the student’s perspective, and formulated an overall sense of the youth’s areas of strength and need and a brief action plan. Both ISP and PTA involved supportive adult contact with problem-solving, though intervention dose was smaller for ISP.
We previously showed that PTA participants, relative to ISP, demonstrated significant improvements on child-reported depressive symptoms at post-intervention, d = .34. PTA youths also had significantly lower levels of child-reported internalizing symptoms and improved health behavior (McCarty et al., 2013). PTA specifically aimed to promote the maintenance of gains by: (a) teaching students to apply cognitive-behavioral skills to individualized goals related to school, interpersonal, and health functioning; (b) focusing on generalization of skills through weekly homework followed by feedback during sessions; and (c) involving parents to support home practice and continued use of skills post-intervention. Given PTA’s demonstrated efficacy over ISP at post-intervention and the intervention’s explicit attention to long-term maintenance, we hypothesized that PTA gains relative to ISP will persist until 12 months post intervention. We expected that PTA participants would evidence improvement on symptomatology, including child-reported depressive symptoms, and child- and parent-reported internalizing and externalizing symptoms. We further expected that PTA would lead to improved functional outcomes, including school adjustment, interpersonal functioning with parents and peers, and health behavior. Finally, we expected that PTA participants would evidence a lower rate of DSM-IV diagnosis of depressive disorders over the 12-month follow-up period.
Method
Participants and Procedure
Recruitment and enrollment
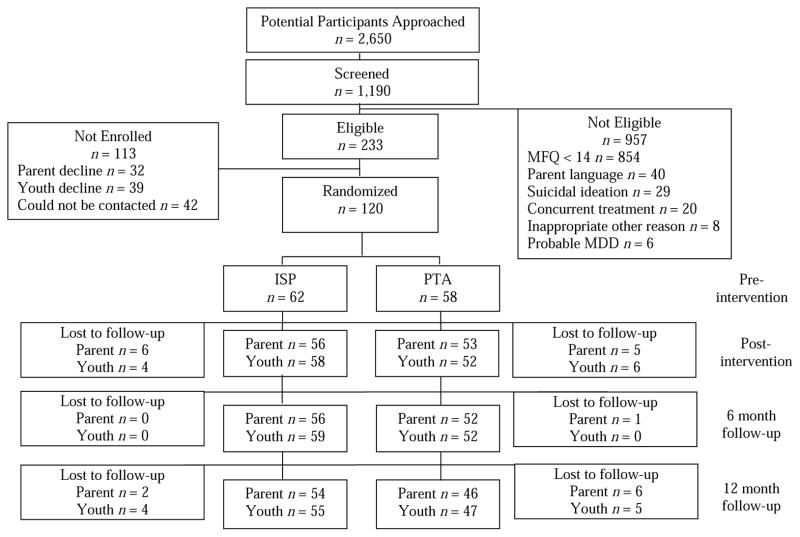
Participants included 120 7th- and 8th-graders attending four Seattle public schools who were at elevated risk for depression, as indicated by a score of 14 or higher (top 25%) on the Mood and Feelings Questionnaire, administered at screening. Randomization was stratified by school, grade, and gender, and yielded assignment of 58 students to PTA and 62 students to ISP. Demographic characteristics of participating students and their families are provided in Table 1, separated by condition. PTA parents were more likely to have Bachelors degrees, and ISP parents were more likely to have high school diplomas or Masters, professional, or doctoral degrees. As shown in Figure 1, we retained 102 of the original 120 students (85.0%) and parents of 100 (83.3%) students, at 12-month follow-up. Retained and attrited youths did not differ on any demographic or outcome variables (all ps > .10).
Table 1.
Sample Demographic Characteristics
| Characteristics | ISP n = 62 |
PTA n = 58 |
t or χ2 | p |
|---|---|---|---|---|
| Mean Age (SD) | 12.7 (.77) | 12.8 (.69) | −0.13 | .45 |
| Sex, n (%) | 1.03 | .31 | ||
| Female | 35 (56.5) | 38 (65.5) | ||
| Male | 27 (43.5) | 20 (34.5) | ||
| Grade, n (%) | 0.02 | .89 | ||
| 7th | 35 (56.5) | 32 (55.2) | ||
| 8th | 27 (43.5) | 26 (44.8) | ||
| Race, n (%) | 3.04 | .69 | ||
| White | 38 (62.9) | 28 (48.3) | ||
| African American | 3 (4.8) | 5 (8.6) | ||
| Asian | 9 (14.5) | 11 (19.0) | ||
| Native American | 5 (8.1) | 7 (12.1) | ||
| Native Hawaiian/Pacific Islander | 1 (1.6) | 2 (3.4) | ||
| Other/Multiracial | 5 (8.1) | 5 (8.6) | ||
| Ethnicity, n (%) | 1.14 | .29 | ||
| Hispanic | 4 (6.5) | 7 (12.0) | ||
| Non-Hispanic | 58 (93.5) | 51 (88.0) | ||
| Parental Education, n (%) | 14.97 | .001 | ||
| HS Diploma/GED/Some College/AA | 32 (51.6) | 21 (36.2) | ||
| Bachelor’s Degree | 14 (22.6) | 32 (55.2) | ||
| Masters/Professional/Doctoral Degree | 16 (25.8) | 5 (8.6) | ||
| Family Constellation, n (%) | 0.01 | .93 | ||
| Single (never married, divorced, widowed, long-term separated) | 23 (37.1) | 22 (38.0) | ||
| Married (or 2 cohabitating parents) | 39 (62.9) | 36 (62.0) | ||
| Annual Household Income, n (%) | 3.35 | .17 | ||
| ≤ 50,000 | 23 (37.7) | 21 (36.2) | ||
| 50,000 to 100,000 | 16 (25.8) | 23 (39.7) | ||
| ≥ 100,000 | 22 (35.5) | 13 (22.8) |
Figure 1.
Participant flow from pre-intervention to 12-month follow-up.
Measures
Assessments occurred at four time points: baseline (Time 0), after the 6-month acute intervention phase (Time 1), 6 months into follow-up (Time 2), and 12 months into follow-up (Time 3). Trained interviewers blinded to intervention status conducted structured interviews and administered self-report questionnaires at the families’ homes or at our research offices.
Depressive symptoms
The Mood and Feelings Questionnaire (MFQ) (Costello & Angold, 1988) is a 33-item self-report questionnaire designed for children aged 8 to 18. Students are asked to report on their depressive symptoms for the last two weeks on a 3-point scale (Not True, Sometimes, True). The MFQ has previously demonstrated high content and criterion validity (Angold, Costello, Messer, & Pickles, 1995), and has high internal consistency in our sample (Cronbach’s αs range from .84 to .91 at each time point). The Patient Health Questionnaire (PHQ-9) was administered individually to students who scored 14 or above on the MFQ, as part of a brief clinical assessment to determine eligibility for the trial, within a few days of screening. The PHQ-9 includes nine questions based upon DSM-IV major depression criteria (Kroenke, Spitzer, & Williams, 2001). It has been found to have high sensitivity (90%) and acceptable specificity (73%) for the diagnosis of major depression in adolescent populations (Richardson et al., 2012).
Internalizing and externalizing symptoms
The Behavior Assessment Scale for Children-Second Edition (BASC-2) was administered to parents and adolescents (Reynolds & Kamphaus, 2004). Most items are rated on a 4-point scale (Never, Sometimes, Often, Almost Always), with some true/false items on the student form. Both youths and parents rated internalizing problems, whereas only parents rated externalizing behavior. BASC-2 scores correlate highly with corresponding scales on the Achenbach System of Empirically Based Assessment (Reynolds & Kamphaus, 2004). Internal consistency for internalizing and externalizing scales in the current sample ranged from α = .78 to .93. The BASC-2 was administered at three time points (pre-intervention, post-intervention, and 12-month follow-up). T-scores were used in all analyses.
Functional outcomes
Adolescent-reported measures of school adjustment, interpersonal relationships, and health behavior were used as secondary functional outcomes. School adjustment was measured with the BASC-2 Attitude to Teachers and Attitude to School subscales. High scores on the Attitude to Teachers scale suggest a perception of teachers as uncaring, unfair, and unmotivated to help them (internal consistency in the current sample ranged from α = .81 to .87). High scores on Attitude to School indicate relative dissatisfaction and discomfort with school (α = .86 to .87). Interpersonal functioning was measured with the BASC-2 subscales Relations with Parents and Interpersonal Relations. High scores on Relations with Parents indicate perception of being important in the family, positive child-parent relationship, and parental trust and concern (α = .89 to .91). High scores on Interpersonal Relations indicate perceptions of difficulty relating to others, particularly peers (α = .78 to .85). Finally, students reported on their health behavior using the Health-Enhancing Behavior Index (HEBI), which contains 12 items assessing healthy eating, regular exercise, and number of hours of sleep. A composite index is calculated by summing the average of each scale, with higher scores indicating better health behavior. In the current sample, internal consistency ranged from α = .80 to .88 over the four time points.
Diagnostic interviews
The Washington University at St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) (Geller, Zimerman, Williams, & Frazier, 1996) is semi-structured parent- and child- clinical interview for the diagnosis of mental health disorders according to DSM-IV criteria. The diagnostic interviews were administered at 12-month follow-up; youths were asked to report on the occurrence of new depressive episodes for the 18 months prior to assessment (coinciding with the period from pre-intervention through 12-month follow-up). Interviewers were bachelors or masters level trainees in psychology, educational psychology, or social work. Inter-rater reliability was assessed for 2 interviews per interviewer. Reliability for diagnosis of a major depressive episode was excellent (κ = 1.00).
Procedures
Figure 1 depicts the screening and enrollment process. From a population of 2,650 7th- and 8th- grade students, 1,190 (45%) returned parental consent forms, assented to participation, and were administered the MFQ. Our goal was to identify a symptomatic sample of youth who did not yet have depressive disorders. Students who scored 14 or higher (top 25%) on the MFQ were seen individually by study staff to assess study eligibility. Exclusion criteria for students were: (a) parents did not understand English, (b) current suicidal ideation, (c) currently enrolled in mental health treatment for depression or to cope with stressors, (d) symptoms consistent with probable major depressive disorder (MDD) based on responses to the PHQ-9, or (e) student was deemed to be inappropriate for a group-based intervention due to clear intellectual disability or behavioral problems. Parents of students who had unmet clinical needs were contacted by phone to provide feedback about their child’s needs and referral information. From the screened sample, 120 were enrolled in the prevention trial and included in the final analyses.
Intervention and Control Conditions
Interventionists were masters or doctoral level therapists who received one (ISP) or two full days of training (PTA), and only delivered one of the two interventions.
PTA
PTA is a manualized, developmentally tailored program focused on cognitive-behavioral skills, including coping, cognitive style, and problem-solving, with application of skills to broader areas including school functioning, interpersonal relations, and health behavior (McCarty et al., 2013; McCarty, Violette, & McCauley, 2011). PTA groups took place at school during or after school. Groups consisted of 50-minute sessions once a week for 12 weeks with groups of four to six students. PTA also promotes parent involvement and support through the inclusion of two home visits with parents and students together, and two separate parent workshops, conducted in the evenings at the school. Topics addressed during parent sessions included setting personal goals for students and parents, adolescent development, teaching parents cognitive and behavioral skills, and communication skills. All PTA sessions were recorded, and 17% were randomly rated for adherence. Overall mean intervention adherence across group leaders was 92%.
Individual Support Program
The control group participants received ISP, a modified version of the Measurement for Adolescent Potential for Suicide intervention (, Thompson, Herting, & Nicholas, 1995b). The original MAPS interview has shown to be associated with significant decreases in depression, hopelessness, stress, and anger at 5- and 10-month follow-ups (Eggert et al., 1995). Our modification involved removal of modules on suicide risk (because youth with suicidal ideation were excluded during recruitment), and adapting questions to a middle school population. The ISP intervention consisted of a 45–90 minute supportive interview regarding the student’s stressors, depression and anxiety, personal control/hopelessness, coping strategies, and support resources. The interviewer summarized and empathized with the student’s perspective, and formulated an overall sense of the youth’s areas of strength and need. The student and interventionist worked together on a brief action plan to address problems, and the student was asked to follow up with a school counselor or teacher that they chose for future support. The interventionist called the youth’s parent to discuss the student’s plan and any areas of need in which the parent could be helpful, and also contacted the student’s chosen supportive school staff member. Sixteen percent of audio recorded ISP interviews were rated, and with mean overall adherence of 91%.
Data Analyses
We previously reported findings that PTA was more efficacious at ISP at post-intervention (McCarty et al., 2013). The current analyses thus focused on effects over the 12-month follow-up. We specified three plausible growth models for each of the continuous outcome variables: a traditional linear growth model, a time-limited effect model, and a persistent effect model. In the traditional linear growth model, the rate of improvement from pre- to post-intervention is the same as the rate of improvement from post-intervention through 12-month follow-up. However, change processes in an intervention and follow-up design may not follow a linear growth trajectory. Indeed, it is likely unrealistic to expect that participants in any psychological intervention would benefit just as much after the program ends as when they were actively participating.
The statistical innovation of piecewise growth modeling (see McCoach & Kaniskan, 2010) allowed us to model non-linear trajectories, with differing change rates for each segment of time. To more accurately capture the hypothesized rate of change, we specified one slope for the pre- to post-intervention period, and a different slope for the post-intervention to 12-month follow-up. In our second model, the time-limited model, the rate of growth from pre- to post-intervention is different from the rate of growth from post-intervention to 12-month follow-up. In our third model, the persistent effect model, there is change from pre- to post-intervention and no change from post-intervention to 12-month follow-up.
In all models, we followed procedures for longitudinal analysis using multilevel modeling (MLM) framework with time nested within individuals (Snijders & Bosker, 2012). The intra-class correlation coefficient (ICCs) for intervention group, interventionist, and school were all below 0.01, and were not accounted for in the analyses. In all models, we first added a time effect coded as 0 = pre-intervention, 1 = post-intervention, 2 = 6-month follow-up, and 3 = 12-month follow-up for all participants. Then, in the time-limited and persistent effect models, we added a time-varying covariate (TVC) at Level 1 to capture the hypothesized discontinuity in growth. In both Models 2 and 3, ISP, as our reference group, had designated TVC values of 0 across the four time points. The coding of the TVC for the PTA group differed across Models 2 and 3. In the time-limited model, the TVC was coded 0, 1, 0, 0 across the four time points. In the persistent effect model, the TVC was coded as 0, 1, 1, 1 across the four time points. The TVC coding does not imply a direction of effects— greater effects for PTA or ISP can both fit the model. The sign of the parameter estimate (i.e., whether the TVC is positive or negative) indicates whether PTA or ISP is more efficacious. When both the time effect and the TVC were included in the model, the multilevel model intercept and slope terms are estimates for the ISP group as the reference, while the estimates from the TVC term illustrate the deviation of the PTA group from the ISP group.
We selected the final model by comparing the Akaike Information Criteria (AIC) and the Bayesian Information Criteria (BIC) of competing non-nested models. Smaller values of AIC and BIC indicate better model fit. Absolute differences in BIC are not as straightforward as with other fit indices. Since differences in BIC across models can be considered to reflect the posterior odds that the first model is correct relative to the odds that the second model is correct (Raftery, 1995), even small differences in BIC can reflect large differences in the odds.
Consistent with the intent-to-treat framework, data from all students who completed baseline measures were included in the analyses even if post-intervention or follow-up data were unavailable. Maximum likelihood estimation was used. Effect sizes (ESs) were computed using the procedures for Cohen’s d (Cohen, 1988). All ESs were calculated such that positive values indicated an advantage for PTA over ISP.
Intervention effects on dichotomous diagnostic outcomes were examined with survival analysis (Singer & Willett, 2003). Consistent with the intent-to-treat approach, participants who were lost to the 12-month follow-up were included in the analyses as censored observations. A Cox proportional hazard regression was used to test the main effect of the intervention on likelihood of any depressive episode by 12-month follow-up.
Results
Preintervention Comparisons
At baseline, there were no significant differences between intervention and control conditions for any measures of symptoms or functional outcomes (all ps > .10). Table 2 shows descriptive statistics on outcome variables for PTA and ISP participants at baseline, post-intervention, 6-month follow-up and 12-month follow-up.
Table 2.
Means (Standard Deviations) for Outcomes by Group and Time
| Outcome (Reporter) | PTA
|
ISP
|
||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | 6 month | 12 month | Pre | Post | 6 month | 12 month | |
| Depressive Symptoms (C) | 15.11 (7.86) | 12.33 (8.85) | 13.40 (8.94) | 12.34 (9.00) | 14.41 (7.97) | 15.59 (9.24) | 15.81 (10.96) | 14.28 (9.03) |
| BASC–2 Internalizing (C) | 50.07 (8.32) | 47.06 (8.17) | — | 45.33 (8.59) | 50.84 (9.36) | 50.79 (8.75) | — | 48.57 (7.97) |
| BASC–2 Internalizing (P) | 52.23 (10.88) | 48.92 (10.32) | — | 50.48 (11.25) | 54.18 (11.61) | 50.57 (11.31) | — | 48.39 (9.79) |
| BASC-2 Externalizing (P) | 48.57 (7.57) | 47.28 (7.65) | — | 47.96 (7.68) | 50.64 (9.65) | 49.57 (8.82) | — | 49.59 (8.10) |
| Health Behavior (C) | 9.80 (1.73) | 10.24 (1.81) | 10.01 (1.87) | 10.08 (2.03) | 9.60 (1.87) | 9.54 (1.99) | 9.22 (2.03) | 9.62 (2.06) |
| BASC–2 Attitude to Teachers (C) | 48.86 (9.39) | 48.47 (8.54) | — | 46.14 (9.34) | 50.82 (9.79) | 51.09 (9.30) | — | 49.94 (10.27) |
| BASC–2 Attitude to School (C) | 48.07 (8.62) | 47.31 (9.68) | — | 44.10 (7.13) | 50.00 (9.22) | 51.27 (9.75) | — | 48.73 (8.94) |
| BASC-2 Relations with Parents (C) | 49.28 (10.63) | 49.73 (9.36) | — | 51.12 (8.48) | 47.42 (10.49) | 45.98 (10.87) | — | 50.12 (8.99) |
| BASC-2 Interpersonal Relations (C) | 49.95 (10.48) | 51.21 (10.57) | — | 53.14 (8.40) | 50.24 (9.39) | 48.79 (10.01) | — | 50.96 (8.86) |
Note. (C) = child report. (P) = parent report. The BASC-2 was not administered at 6 month follow-up.
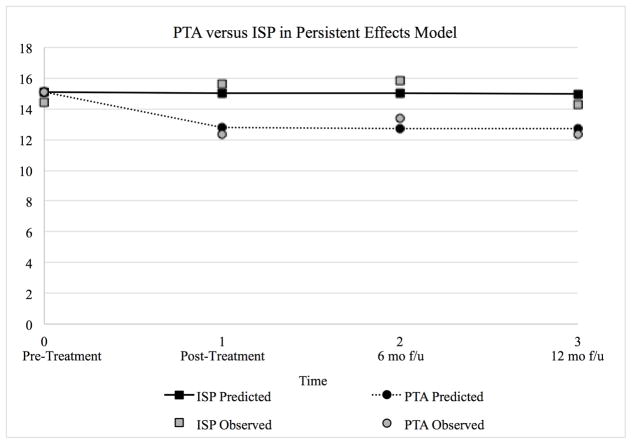
Intervention Effects on Symptoms
We first modeled intervention effects on child-reported depressive symptoms. First, we specified a linear growth model with Time as a predictor, coded 0 1 2 3, but did not include the TVC. Then, we added the TVC under the time-limited effect model (coded 0 0 0 0 for ISP participants and 0 1 0 0 for PTA participants). We compared this model to one in which the TVC reflected a persisting effect of the intervention (coded 0 0 0 0 for ISP participants and 0 1 1 1 for PTA participants). Table 3 summarizes the AIC and BIC values used to evaluate whether a linear growth model, a time-limited model, or a persisting effect model better accounted for the data. The fit indices suggested that the persistent effect model better accounted for students’ change on depressive symptoms. At baseline, the average MFQ score for all participants was 15.06. The time effect indicated that the ISP group decreased at a rate of 0.03 units per wave. The TVC estimate suggested that PTA decreased 2.26 units more than ISP from pre- to post-intervention, and this was maintained over time with a 0.03 decrease per wave after post-intervention. Overall, our findings suggested that relative to ISP, PTA participants showed an improvement in depressive symptoms across the intervention period that was maintained across the 12 months of follow-up. Figure 2 illustrates depressive symptoms for ISP and PTA participants over time.
Table 3.
Summary of Hierarchical Linear Modeling (HLM) Analyses
| Outcome (Reporter) | Linear growth model
|
Time-limited model
|
Persisting effect model
|
Best fitting model parameters
|
|||||
|---|---|---|---|---|---|---|---|---|---|
| AIC | BIC | AIC | BIC | AIC | BIC | Intercept | Time | Time Varying Covariate [95% CI] | |
| Depressive Symptoms (C) | 3154.32 | 3182.90 | 3153.98 | 3182.55 | 3151.82 | 3180.39 | 15.06 | −0.03 | −2.26 [−4.34, −0.19] |
| BASC–2 Internalizing (C) | 2194.35 | 2220.75 | 2193.22 | 2219.62 | 2190.69 | 2217.09 | 50.62 | −0.85 | −2.38 [−4.19, −0.58] |
| BASC–2 Internalizing (P) | 2333.28 | 2359.97 | 2319.94 | 2346.53 | 2331.01 | 2357.61 | 52.96 | −1.28 | −3.20 [−4.88, −1.52] |
| BASC-2 Externalizing (P) | 2173.98 | 2200.57 | 2172.63 | 2199.22 | 2173.33 | 2199.92 | 49.46 | −0.35 | −1.23 [−2.57, 0.11] |
| Health Behavior (C) | 1576.61 | 1605.17 | 1572.72 | 1601.28 | 1574.03 | 1602.59 | 9.65 | 0.41 | 0.42 [0.08, 0.74] |
| BASC–2 Attitudes to Teachers (C) | 2247.53 | 2273.90 | 2250.31 | 2276.69 | 2249.68 | 2276.06 | 53.73 | −0.46 | −2.50 [−5.44, 0.44] |
| BASC–2 Attitudes to School (C) | 2247.04 | 2273.44 | 2252.20 | 2278.60 | 2250.47 | 2276.87 | 54.24 | −0.83 | −3.22 [−5.95, −0.48] |
| BASC–2 Relations with Parents (C) | 2271.57 | 2297.97 | 2272.98 | 2299.38 | 2272.98 | 2299.38 | 45.04 | 0.92 | 1.88 [−1.23, 4.99] |
| BASC–2 Interpersonal Relations (C) | 2265.05 | 2291.45 | 2265.67 | 2292.07 | 2264.63 | 2291.03 | 49.69 | 0.53 | 1.12 [−0.84, 3.08] |
Note. (C) = child report. (P) = parent report. The BASC-2 was not administered at 6 month follow-up. Bolded font indicates the best fitting model for each outcome.
Figure 2.
Observed and predicted depressive symptom scores for PTA and ISP participants separately, under the persistent effects model.
To further understand who most benefited from the intervention, we conducted post-hoc analyses examining baseline depressive symptoms as a potential moderator of intervention impact by adding a multiplicative term between the intervention condition and baseline depressive symptoms, constituting a three-way cross-level interaction with time (Snijders & Bosker, 2012). The results indicated that baseline symptoms did not significantly moderate PTA effects (B = .01, 95% CI [−.20, .22], p = .93).
Similar analytic procedures were conducted to examine other symptom outcomes, including measures of child- and parent-reported internalizing and externalizing symptoms. As shown in Table 3, comparison of model fit suggests a persisting effect of PTA on child-reported internalizing symptoms. Effect sizes, shown in Table 4, indicated a moderate advantage of PTA at both post-intervention and 12-month follow-up. In contrast, the advantage of PTA on parent-reported internalizing symptoms is much smaller and time-limited. Although the time-limited model fits best in predicting changes in parent-reported externalizing behavior, the parameter estimate for PTA effects included 0.
Intervention Effects on Functional Outcomes
Next, we used the analytic procedures described above to examine the effects of the intervention on school adjustment, interpersonal relationships, and health behavior. As shown in Table 3, we found a time-limited PTA effect for health behavior. Effect sizes in Table 4 indicated diminishing effects on health behavior over time. PTA showed a linear effect on attitudes to school. Effect sizes (Table 4) for attitudes to school favored PTA and were moderate in magnitude at both post-intervention and 12-month follow-up. Although the linear growth model fit the data best for Attitudes to Teachers and Relations with Parents, parameter estimate confidence intervals included 0. While the persisting effect model fit the data best for Interpersonal Relations, the parameter estimate also included 0.
Table 4.
Cohen’s d [95% Confidence Interval] for Outcomes by Group and Time
| Outcome (reporter) | Post | 6 month | 12 month |
|---|---|---|---|
| Depressive Symptoms (C) | .36 [−.02, .73] | .24 [−.14, .61] | .21 [−.18, .61] |
| BASC–2 Internalizing (C) | .44 [.05, .82] | — | .39 [−.02, .80] |
| BASC–2 Internalizing (P) | .15 [−.22, .52] | — | −.20 (−.59, .20] |
| BASC-2 Externalizing (P) | .27 [−.10, .65] | — | .20 [−.19, .60] |
| Health Behavior (C) | .36 [−.01, .74] | .40 [.02, .78] | .22 [−0.18, .62] |
| BASC–2 Attitude to Teachers (C) | .29 [−.09, .67] | — | .38 [−.03, .79] |
| BASC–2 Attitude to School (C) | .40 [.02, .79] | — | .56 [.15, .98] |
| BASC-2 Relations with Parents (C) | .36 [−.02, .74] | — | .11 [−.30, .52] |
| BASC-2 Interpersonal Relations (C) | .23 [−.15, .61] | — | .25 [−.16, .66] |
Note. (C) = child report. (P) = parent report. The BASC-2 was not administered at 6 month follow-up.
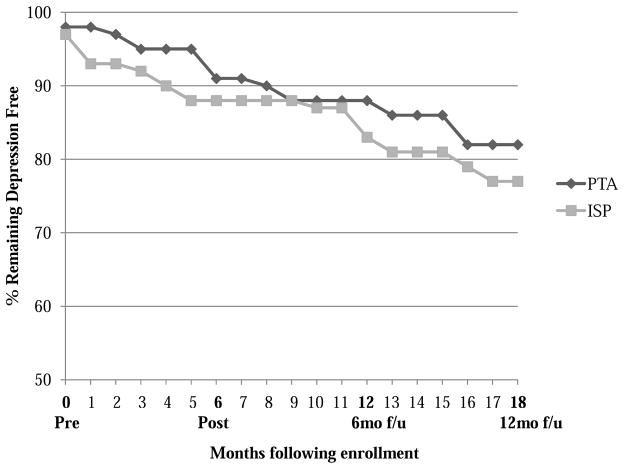
Intervention Effects on Depressive Disorder Onset
By 12-month follow-up, new (initial) episodes of major depression and/or dysthymia were experienced by 13/62 (21%) of ISP participants, compared to 10/58 (17%) of PTA participants. Figure 2 illustrate the cumulative proportion surviving (no depressive episode) for PTA and ISP groups. Cox proportional hazard models indicated that the difference between intervention and control groups was not significant (Δχ2 = .22, p = .64), with an odds ratio for any depressive episode of 1.27 (95% CI [0.51 to 3.18]).
Discussion
The current study evaluated the 12-month effects of Positive Thoughts and Actions (PTA), a school-based group cognitive-behavioral depression prevention program for middle school students. Our effect sizes are consistent with those from prior depression prevention trials, which has been estimated in meta-analysis to be d = .20 at 12-month follow-up (Merry & Stasiak, 2012). The effect sizes found in this study are noteworthy given a comparison condition that controlled for adult support and problem-solving. Baseline depressive symptoms did not moderate intervention effects. The sizeable percentage of ethnic minorities in our sample (44%) suggests that this prevention program may be efficacious for diverse populations of adolescents. The demonstrated success with our middle school sample (mean age = 12.8 years) suggests that PTA is a promising program in this younger age range. Depression prevention effects are especially difficult to achieve with younger samples. The meta-analysis by Stice et al. (2009) showed that depression prevention is efficacious with older samples, but have negligible effects with children younger than 13.5 years of age (d = .04). We believe that a number of factors contribute to the efficacy of PTA. The program was developed specifically for early adolescents with curriculum material that uses concrete, age-appropriate language and examples of stressors faced by middle-school students. Our interventionists were well-trained, and parents were actively involved via workshops and home visits.
It is worth noting that the 95% confidence intervals for group differences on depressive symptoms included 0 at all three time points. Given our original sample size of 120, we had power (1- β) = .80 at p < .05 to detect average differences between groups at any given time point as small as Cohen’s d = .52. These effect sizes provide a cross-sectional estimate of group differences at any given assessment, not accounting for scores at other assessments. Growth models, on the other hand, estimate model parameters based on scores at all four time points.
The current findings suggest an effect of PTA on depressive symptoms at post-intervention (d = .36) that persists, but with diminishing magnitude of effects over time (d = .24 and d = .21 at 6- and 12-month follow-ups, respectively). The pattern of depressive symptoms illustrated in Figure 2 suggests that the effects of PTA might be more accurately described as a health promotive rather than a prevention effect. Prevention effects would be indicated by worsening symptoms in the control group, and a prevention of such worsening in the intervention group. Health promotive effects, in contrast, are indicated by a relative decline in symptoms for the intervention as compared to the control group. Our results are consistent with meta-analytic findings that many depression “prevention” programs are effective by reducing subclinical depressive symptoms (Horowitz & Garber, 2006), consistent with a health promotive effect.
The issue of characterization of program effects as “health promotion” or “disease prevention” is also intertwined with methods of identifying youth who are at risk for developing later MDD. In this study, we relied on elevated scores on a questionnaire at screening, and invited students in the top 25% to participate in this study. Although the 12-month prevalence of MDD in adolescence is 10.7% (Substance Abuse and Mental Health Services Administration, 2014), we chose to recruit a larger portion of the school population because of research suggesting that subclinical levels of depressive symptoms can contribute to functional impairment (Fergusson et al., 2005). Across groups, many students showed a reduction in symptoms between screening and pre-intervention, which may be due to regression to the mean, the episodic nature of depression, a placebo effect due to enrollment in the study, or “false positives” identified at screening. On average, our sample was at elevated risk compared to the general population: Our survival analysis shows that 19% percent went on to develop MDD in the 18 months following baseline. However, substantial heterogeneity in severity of symptoms was also evident. Thus, our study sample likely consists of some students that never would have developed MDD even without intervention, and students who would more imminently develop MDD.
Although our control group, ISP, received a lower dose of intervention than PTA, ISP was designed to control for non-specific support and empathy with an engaged adult and is a more active control than a no-treatment comparison. To our knowledge, only two other trials to date have shown an advantage of a cognitive-behavioral depression prevention program over plausibly efficacious active control conditions (Stice, Burton, Bearman, & Rohde, 2007; Stice et al., 2008). At the same time, future work should compare PTA to an active comparison condition that also controls for intervention dose and the effects of being involved in a group of peers.
No significant differences in the prevention of new depressive episodes between PTA and ISP were found at 12-month follow-up. This result is consistent with the only other trial to date testing the impact of school-based depression prevention on the onset of diagnostic outcomes against active control groups (Stice et al., 2010), which found significant differences only for an inactive brochure control. In our study, onset of new depressive episodes occurred for 21% of control participants, compared to 17% of PTA members. Visual examination of the data in Figure 3 suggests that, in all time periods following the beginning of the intervention, PTA participants developed depressive episodes at a lower rate than their peers in ISP. Longer term follow-up would be needed to determine whether this pattern continues past 12 months.
Figure 3.
Cumulative percent remaining depression free for intervention and control groups over follow-up.
Our findings suggest that PTA effects may have been noticeable to parents, as indicated by a time-limited effect on parent-reported internalizing symptoms. Previous work by Clarke and colleagues has suggested benefits of the Coping with Stress program mainly on youth-reported depressive symptoms at post-test (Clarke et al., 1995). Similarly, meta-analyses of treatment studies for youth depression have found that effect sizes for depression treatment based on parent-reported outcomes do not differ from zero, and are significantly lower than youth reported effect sizes (Weisz, McCarty, & Valeri, 2006). Our relatively intensive efforts to provide skills-based training and psychoeducation to parents in the format of workshops and home visits may have improved PTA parents’ ability to identify and address depressive symptoms in their children, although our results suggest that this effect may diminish over time.
PTA participants demonstrated changes in two of the three domains of functioning examined, health behavior and attitudes towards school. The relationship between health and mood was emphasized in PTA, with all youths creating specific target goals related to improving their physical health. It may be that health behaviors are easier to change in the short term, compared to interpersonal outcomes, because adolescents have greater control over these behaviors and they can evidence change in a short span of time. PTA also included a significant focus on school adjustment (e.g., by identifying and challenging negative thoughts about school). Contrary to hypotheses, we did not find effects of PTA on interpersonal functioning with parents and peers. It may be that a more robust or more specifically targeted intervention is needed to affect interpersonal outcomes, and that cognitive-behavioral skills training is not sufficient.
A number of potential limitations of this project should be considered. First, although both PTA and ISP were portrayed as potentially useful interventions, parents, youth, and interventionists were not blinded to allocation, and dose of intervention was not equal. Second, it will be important in future studies to examine what mediators might account for changes in youth depressive symptoms. Research designs that allow for the dismantling of both specific and non-specific components will be helpful in this regard. Third, possible moderators of PTA efficacy should be examined, including gender, age, and race/ethnicity. We are currently proceeding with analyses examining the mediators and moderators of PTA program effects. Fourth, continued follow-up over longer periods of time would be informative about the maintenance of prevention effects achieved by PTA, and whether booster sessions would be needed to sustain skills.
To summarize, the current findings provide further support for the efficacy of Positive Thoughts and Action, a school-based prevention program for those at elevated risk for depression onset. Further attention to the impact of depression prevention programs on outcomes beyond the timeframe of delivery of intervention will be useful in weighing the public health impact of school-based preventive interventions.
Acknowledgments
Funding: This study was funded by the National Institute of Mental Health (R34 MH083076).
Footnotes
Disclosure of potential conflicts of interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Compliance with Ethical Standards
Informed consent: Informed consent was obtained from all individual participants included in the study.
Contributor Information
Mylien T. Duong, University of Washington
Rick A. Cruz, Utah State University
Kevin M. King, University of Washington
Heather D. Violette, Seattle Children’s Research Institute
Carolyn A. McCarty, University of Washington and Seattle Children’s Research Institute
References
- Angold A, Costello EJ, Messer SC, Pickles A. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–249. [Google Scholar]
- Arnarson EO, Craighead WE. Prevention of depression among Icelandic adolescents: a 12-month follow-up. Behaviour Research and Therapy. 2011;49:170–174. doi: 10.1016/j.brat.2010.12.008. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of a group cognitive intervention. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:312–321. doi: 10.1097/00004583-199503000-00016. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Costello EJ, Angold AA. Scales to assess child and adolescent depression: Checklists, screens, and nets. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27(6):726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- Eggert LL, Thompson EA, Herting JR, Nicholas LJ. Reducing suicide potential among high-risk youth: Tests of a school-based prevention program. Suicide and Life Threatening Behavior. 1995;25:276–296. doi: 10.1111/j.1943-278X.1995.tb00926.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Archives of General Psychiatry. 2005;62:66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Frazier J. WASH-U-KSADS (Washington University at St. Louis Kiddie and Young Adult Schedule for Affective Disorders and Schizophrenia - Lifetime and Present Episode Version for DSM-IV) St Louis, MO: Washington University; 1996. [Google Scholar]
- Gillham JE, Reivich KJ, Freres DR, Chaplin TM, Shatté AJ, Samuels B, Seligman ME. School-based prevention of depressive symptoms: A randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program. Journal of Consulting and Clinical Psychology. 2007;75:9–19. doi: 10.1037/0022-006X.75.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74:401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- Klein DN, Shankman SA, Lewinsohn PM, Seeley JR. Subthreshold depressive disorder in adolescents: Predictors of escalation to full-syndrome depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:703–710. doi: 10.1097/CHI.0b013e3181a56606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33(6):809–818. doi: 10.1097/00004583-199407000-00006. [DOI] [PubMed] [Google Scholar]
- Lynch FL, Clarke GN. Estimating the economic burden of depression in children and adolescents. American Journal of Preventive Medicine. 2006;31:S143–151. doi: 10.1016/j.amepre.2006.07.001. [DOI] [PubMed] [Google Scholar]
- McCarty CA, Violette HD, Duong MT, Cruz RA, McCauley E. A randomized trial of the Positive Thoughts and Action program for depression among early adolescents. Journal of Clinical Child and Adolescent Psychology. 2013;42:554–563. doi: 10.1080/15374416.2013.782817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty CA, Violette HD, McCauley E. Feasibility of the positive thoughts and actions prevention program for middle schoolers at risk for depression. Depression Research and Treatment. 2011;2011:241386. doi: 10.1155/2011/241386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoach DB, Kaniskan B. Using time-varying covariates in multilevel growth models. Frontiers in Psychology. 2010;1:17. doi: 10.3389/fpsyg.2010.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merry SN, Stasiak K. Preventing depression in adolescents. BMJ. 2012;345:e6720. doi: 10.1136/bmj.e6720. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. BASC-2: Behavior Assessment System for Children. 2. Circle Pines, MN: American Guidance Service; 2004. [Google Scholar]
- Richardson LP, McCauley E, McCarty CA, Grossman DC, Myaing M, Zhou C, Katon W. Predictors of persistence after positive depression screen among adolescents. Pediatrics. 2012;130:e1541–e1548. doi: 10.1542/peds.2012-0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, McLoone J. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. Journal of Consulting and Clinical Psychology. 2006;74:66–79. doi: 10.1037/0022-006X.74.1.66. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. Thousand Oaks, CA: Sage; 2012. [Google Scholar]
- Stice E, Burton E, Bearman SK, Rohde P. Randomized trial of a brief depression prevention program: An elusive search for a psychosocial placebo control condition. Behaviour Research and Therapy. 2007;45:863–876. doi: 10.1016/j.brat.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau JM, Wade E. Efficacy trial of a brief cognitive-behavioral depression prevention program for high-risk adolescents: Effects at 1- and 2-year follow-up. Journal of Consulting and Clinical Psychology. 2010;78:856–867. doi: 10.1037/a0020544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76(4):595–606. doi: 10.1037/a0012645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. Journal of Consulting and Clinical Psychology. 2009;77:486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. [Google Scholar]
- Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychological Bulletin. 2006;132:132–149. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]