Abstract
Objectives
Type of surgery for rectal cancer (RC), including permanent ostomy (PO), temporary ostomy followed by anastomosis (TO), or initial anastomosis (AN), can affect psychological and financial well-being during active treatment. However, this relationship has not been well-studied among long-term survivors (≥5 years post-diagnosis).
Methods
A mailed survey with 576 long-term RC survivors who were members of Kaiser Permanente was conducted in 2010–2011. Prevalence of current depression was ascertained using a score of ≤45.6 on the Short Form-12 version 2 mental component summary. Perceived financial burden was assessed using a Likert scale ranging from 0 (none) to 10 (severe). Regression analyses were used to measure associations after adjustment for covariates.
Results
The overall prevalence of depression was 24% among RC survivors with the highest prevalence among those with history of PO (31%). The adjusted odds of depression among TO and AN survivors was lower than among PO survivors, 0.42 (CI95% 0.20–0.89) and 0.59 (CI95% 0.37–0.93), respectively. Twenty two percent perceived moderate-to-high current financial burden (≥4 points). PO survivors also reported higher mean financial burden than AN survivors (2.6 vs. 1.6, respectively; p=0.002), but perceived burden comparably to TO survivors (2.3). Self-reported depression was associated with higher perceived financial burden (p<0.001); surgical procedure history did not modify this relationship.
Conclusions
Depression was reported frequently among these long-term RC survivors, particularly among PO survivors. Depression was associated with greater perception of financial burden. Screening for depression and assessing financial well-being might improve care among long-term RC survivors.
Keywords: Rectal Cancer, Depression, Financial Burden, Cancer Survivors, Oncology
Background
Many cancers have become survivable diseases. Understanding the long-term impacts that diagnosis and treatment have on survivors’ quality of life, even years after the diagnosis, is becoming increasingly important [1,2]. Rectal cancer (RC) 5-year survival has increased from 58% of those diagnosed in 1987–1989 to 68% of those diagnosed in 2003–2009 [3].
Cancer survivors exhibit higher depression prevalence than those without cancer and those with chronic lung and heart diseases [4,5]. Based on the Diagnostic and Statistical Manual of Mental Disorder, 4th edition (DSM-IV) criteria, 18.3% of cancer survivors in the United States (US) experience depression with the highest prevalence occurring within the first two years of diagnosis [5,6]. The psychological toll of cancer varies by cancer type and treatment [2]. Higher depression prevalence is reported among pancreatic (33–50%) and breast (1.5–46%) cancer survivors, while lower prevalence is reported among gynecological (12–23%) and colon (8%) cancer survivors [7,8].
Few studies have assessed the prevalence of depression among RC survivors. One study from the United Kingdom reported that the prevalence of depression among RC survivors with 1–11 years post diagnosis was 25% [9]. Another study reported variation by surgery type—32% among those who had colostomies, and 10% among those who had anastomoses [10].
Financial burden imposed by illness (loss of income) and treatment (out-of-pocket medical care spending) is another factor that may affect survivors’ emotional state and quality of life [11,12]. Cancer survivors often experience financial burden during treatment, which can persist long after the initial treatment [13]. Financial burden and depression tend to reinforce each other [12,14]. Depression can lead to greater perceptions of financial burden [14], and financial burden can cause emotional stress and depression. Depression tends to be cyclical such that individuals who experience one episode of depression are at risk of another in the future [15]. While many cancer survivors feel depressed after their diagnosis and treatment [16], how survivors perceive financial burden over time remains unexplored. A recent cross-sectional study showed that higher financial burden was reported among depressed breast cancer survivors than among those without depression [17].
The surgical treatment of RC typically involves a rectal resection followed by a permanent ostomy, an immediate anastomosis, or a temporary colostomy which is subsequently reversed (temporary ostomy). The choice of treatment impacts immediate quality of life and may influence long-term quality of life [18–20]. Prior studies suggest that gender is an effect modifying factor of this experience. Women with permanent ostomies experience more psychological and social concerns than men with permanent ostomies [21]. Furthermore, the associations between initial surgery type and various health outcomes, e.g., overall health-related quality of life and psychological well-being, appear to differ by gender [18].
A recently completed survey of RC survivors enrolled in Kaiser Permanente, a large integrated healthcare delivery system, provides an opportunity to explore the relationships between depression and perceived financial burden among long-term RC survivors (diagnosed ≥5 years). This survey sought to evaluate health-related quality of life using the Short-Form 12 Health Survey version 2 (SF-12v2), and the City of Hope Quality of Life Colorectal Cancer (COH-QOL-CRC). The present study utilizes these data in a secondary analysis to explore the prevalence of self-reported depression and perceived financial burden and the influence of initial surgery type, depression at the time of surgery, and gender. Findings could identify whether the need is present to conduct more in-depth assessments of depression among this population, relate such depression to perceived financial burden, and inform specific aspects of survivorship care planning.
Methods
Population
The survey was conducted in 2010–2011 and targeted long-term RC survivors from Kaiser Permanente. A more detailed description of the population and survey methods is available elsewhere [22]. Briefly, participants were selected if they were at least 5 years post cancer diagnosis in 2010, had received a permanent ostomy or an anastomosis with or without a temporary stoma as part of their treatment, and were Kaiser Permanente members in Northern California or Oregon/Southwest Washington. Members were excluded if they had requested no contact for research purposes or had severe mental illness or cognitive impairment, which were determined from two or more ICD-9-CM diagnosis codes 290–299 recorded in the electronic medical record.
Survey Instruments and Variables
In addition to COH-QOL-CRC [23] and SF-12v2 [24], the survey included additional psychological and socio-demographic questions.
The COH-QOL-CRC was used to identify current perceived financial burden. The questionnaire consists of 43 questions divided into four subscales: physical, psychological, social, and spiritual well-being. Each question used a 10-point Likert scale. Depending on the surgery type, questions were preceded by “In relation to your ostomy, to…” or “In relation to your operation, to what extent are the following a problem for you at this time.” Subsets of the COH-QOL-CRC questions were used to create perceived financial burden and physical well-being variables. Perceived financial burden was obtained from the response, “How much financial burden resulted from your illness and treatment?” Participants could choose one response ranging from 0 (none) to 10 (severe). The COH-QOL-CRC physical well-being subscale score was the average of the 11 items addressing concerns about physical strength, aches or pains, gas, and diarrhea and ranged from 0 – 10, where lower scores signified a lower physical well-being.
The SF12v2 was used to identify patient-defined depression occurring within the last 30 days. It assesses eight domains – physical function, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. Two component summary measures, the physical (PCS) and mental component summaries (MCS) were weighted based on scoring algorithms across all 12 items [25]. Patient-defined current depression was defined as participants whose SF-12v2 MCS scores were ≤45.6 at the time of the survey. Vilagut et al. (2013) recommended a cutoff score of ≤45.6 as a screening tool for 30-day depressive disorders encompassing a major depressive episode or less severe and chronic forms of major depression (i.e., dysthymia)[26]. This cutoff point had a sensitivity of 0.86, a specificity of 0.88, and an area under the receiver operating characteristic curve of 0.92, demonstrating high discriminative ability. MCS scores for participants in the study were calculated using QualityMetric Health Outcomes Scoring Software 4.5 (©QualityMetric, Lincoln, Rhode Island, USA 2004–2011) and were scored against 1998 US norms, results of which were comparable to MCS scores used by Vilagut et al. (2013) [26]. Since the survey’s primary purpose was not to ascertain clinical depression and SF-12 has been useful in screening for depression in various population [26–29], it could be useful in exploring self-defined depression burden among this group. The term ‘depression’ is used in this report to describe self-reported depressive symptoms.
Additional variables from the survey were included in this analysis: recall of depression immediately after surgery, race, gender, education, employment status, and household income. Recall of depression immediately after surgery was based on answering ‘yes’ to the psychological question, “Were you depressed after having your ostomy [operation]?” Age, time since diagnosis, initial surgery types, and the Charlson-Deyo co-morbidity index were derived from patients’ electronic medical records.
Analytic Methods
Frequency and percentage of socio-demographic characteristics were calculated. Prevalence of self-reported depression and mean (standard deviation, SD) scores for perceived financial burden were calculated for the total group and by gender, initial surgery type, and recall of depression immediately after surgery. Chi-square tests, Student’s t-tests, and analysis of variance (ANOVA) were used to assess statistical significance of differences by demographic characteristics and initial surgery type. Tukey’s Honestly Significant Difference test was used when overall F-tests were statistically significant.
Association between initial surgery type and self-reported depression
Logistic regression was used to calculate crude and adjusted odds ratios (AOR), and 95% confidence intervals (CI95%) were also calculated. The following variables were considered as potential confounders: age, gender, race, educational attainment, time since diagnosis, Charlson-Deyo co-morbidity index, and physical well-being. Variables were included in the adjusted model if they changed the crude OR by more than 10% for any surgical type. Log-likelihood ratio tests were used to evaluate whether gender and recall of depression immediately after surgery were effect modifiers.
Association between perceived financial burden (0–10) and self-reported depression (yes/no)
Linear regression was used to evaluate this association. Potential confounding variables were initial surgery type, gender, age, time since diagnosis, Charlson Deyo co-morbidity index, employment status, and household income. Confounding variables were included in the final model if they changed the β-coefficient of the depression variable by more than 10%. Interaction terms were used to determine effect modifications by gender, recall of depression immediately after surgery, and surgery type. The interaction term was included in the final model if the associated p-value for the coefficient estimate was <0.10. Adjusted means (Madj) from the final model were reported.
Results
Characteristics of the study population
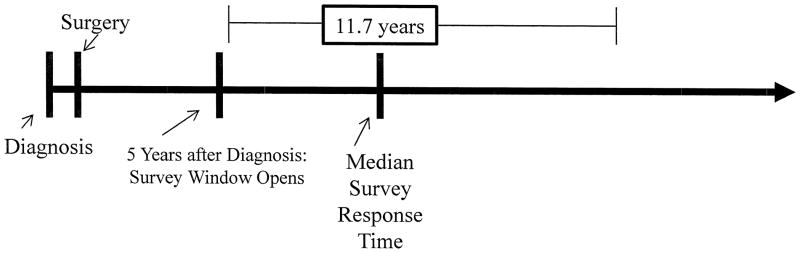
Detailed characteristics of the 576 participants by initial surgery group are presented elsewhere [22]. Approximately 57% of the participants had received an anastomosis, 32% received a permanent ostomy, and 11% had a temporary ostomy followed by an anastomosis. Fifty-nine percent of participants were male and 83% were white. Survivors with permanent ostomies were older than those with anastomoses or temporary ostomies [74.7 (SD=11.1) versus 72.9 (10.6) or 69.3 (10.9) years, respectively]. The median time since cancer diagnosis was 11.7 years (Figure 1). Survivors with permanent ostomies also had longer time since diagnosis than those with anastomoses or temporary ostomies, 14.9 (7.8) versus 12.8 (5.6) or 11.1 (4.6) years, respectively. Survivors with anastomoses were more likely to be female (45.3% versus 34.4%), to have completed college (45.3% versus 27.5%), and to have a lower co-morbidity index [0.64 (1.1) versus 1.08 (1.5)] than those who had received permanent ostomies. Characteristics of survivors with anastomoses and temporary ostomies were comparable.
Figure 1.
Median Time from Diagnosis (years)
Prevalence of self-reported depression
The prevalence of depression was 24.7% among the entire group of survivors (Table 1). Survivors with permanent ostomies had the highest prevalence (31%) compared to those with anastomoses (22.2%) or temporary ostomies (20.0%). Depression prevalence was also higher among survivors with depression immediately after surgery (38.5%), females (30.5%), those with ≤ high school education (32.9%), individuals with incomes ≤30K (33.5%), and individuals who were unemployed (50%) or on permanent disability (46.7%).
Table 1.
Characteristics of long-term RC survivors, prevalence of depression within the last 30 days, and perceived financial burden mean scores
| Characteristics | All | Depressed in the past 30 Days± (N=554) | Perceived Financial Burden Scores+ (N=506) | |
|---|---|---|---|---|
|
| ||||
| N | % | % | Mean (SD) | |
|
| ||||
| All | 576 | 24.7 | 1.99 (2.78) | |
| Surgery Treatment | ||||
| Permanent Ostomy | 183 | 31.7 | 31.2 | 2.56 (3.01)2 |
| Temporary Ostomy | 66 | 11.5 | 20.0 | 2.28 (2.74) |
| Anastomosis | 327 | 56.7 | 22.2 | 1.63 (2.62) |
| Recall of depression after surgeryǂ | ||||
| Yes | 203 | 36.1 | 38.53 | 3.22 (3.34)3 |
| No | 360 | 63.9 | 17.0 | 1.35 (2.18) |
| Gender | ||||
| Male | 341 | 59.0 | 20.72 | 2.04 (2.75) |
| Female | 235 | 41.0 | 30.5 | 1.94 (2.86) |
| Race | ||||
| White | 454 | 82.7 | 24.0 | 1.87 (2.64) |
| African American | 19 | 3.5 | 42.1 | 3.25 (3.68) |
| Asian | 45 | 8.2 | 23.1 | 2.64 (3.42) |
| Other races | 31 | 5.6 | 17.2 | 2.65 (3.51) |
| Ethnicity | ||||
| Non-Hispanic | 518 | 93.5 | 23.6 | 1.99 (2.76) |
| Hispanic | 36 | 6.5 | 28.6 | 1.72 (2.96) |
| Educational Level | ||||
| High school or less | 158 | 30.2 | 32.92 | 2.41 (3.06)1 |
| Some college or vocational training | 167 | 31.9 | 27.3 | 2.13 (2.88) |
| College grad or higher | 198 | 37.9 | 16.0 | 1.59 (2.39) |
| Time since diagnosis | ||||
| 5–8 years | 129 | 22.6 | 30.0 | 2.38 (3.00) |
| 8–12 years | 171 | 30.0 | 22.8 | 2.11 (2.83) |
| 12–17 years | 132 | 23.1 | 23.4 | 1.47 (2.35) |
| >17 years | 139 | 24.3 | 22.6 | 1.93 (2.78) |
| Household Income | ||||
| ≤$30,000 | 160 | 30.3 | 33.52 | 3.11 (3.34)3 |
| $30,001–$75,000 | 231 | 43.8 | 19.4 | 1.76 (2.56) |
| >$75,000 | 137 | 25.9 | 21.8 | 1.13 (1.94) |
| Employment | ||||
| Full time or part time | 162 | 28.5 | 27.51 | 2.09 (2.83)3 |
| Retired and not working | 377 | 66.4 | 21.6 | 1.69 (2.55) |
| Unemployed | 14 | 2.4 | 50.0 | 5.27 (3.77) |
| On disability or other | 15 | 2.6 | 46.7 | 5.33 (3.06) |
Based on SF-12v2 MCS ≤45.6.
Perceived financial burden related to the disease and treatment – on the scale question on mCOH-QOL, 0=none, 10=severe.
Based on a question, ‘were you depressed after having your ostomy [operation]?’ Chi-squared test, Student’s t test, or ANOVA overall F-test:
p<0.05,
p<0.01,
p<0.001
Association between initial surgery type and self-reported depression
In these analyses, individuals with missing values were excluded. The final models included 554 participants and included age and physical well-being as confounding variables. Table 2 shows crude and adjusted associations.
Table 2.
Adjusted associations for self-reported current depression± by type of RC surgery among long-term survivors for all participants and stratified by gender and recall of depression after surgery (N = 554).
| Permanent Ostomy | Temporary Ostomy | Anastomosis | |||
|---|---|---|---|---|---|
|
| |||||
| Crude OR (CI95%) | AOR (CI95%)* | Crude OR (CI95%) | AOR (CI95%)* | ||
|
| |||||
| All | Ref. | 0.55 (0.28–1.10) | 0.42 (0.20–0.89) | 0.63 (0.41–0.95) | 0.59 (0.37–0.93) |
| Gender | |||||
| Male | Ref. | 0.74 (0.29–1.87) | 0.46 (0.17–1.29) | 0.95 (0.54–1.69) | 0.93 (0.49–1.77) |
| Female | Ref. | 0.33 (0.12–0.96) | 0.33 (0.11–1.04) | 0.31 (0.16–0.59) | 0.29 (0.15–0.60) |
| Recall of depression after surgeryǂ | |||||
| Yes | Ref. | 0.20 (0.05–0.72) | 0.24 (0.06–0.95) | 0.80 (0.44–1.46) | 0.77 (0.39–1.48) |
| No | Ref. | 1.56 (0.62–3.93) | 0.85 (0.31–2.37) | 0.98 (0.50–1.96) | 0.80 (0.38–1.69) |
Note: OR=odds ratio, AOR=adjusted odds ratio, CI95%=95% confidence interval.
Based on SF-12v2 MCS ≤45.6.
Based on answering “yes” on a psychological question, “Were you depressed after having your ostomy [operation]?”
Adjusted for age, and physical well-being.
Adjusted for confounders, survivors with anastomoses (AOR=0.59, CI95% 0.37–0.93) and those with temporary ostomies (AOR=0.42, CI95% 0.20–0.89) were less likely to have current depression compared to those with permanent ostomies. However, age and physical well-being were both negatively associated with reporting current depression. The likelihood ratio tests suggested that gender modified the relationship between surgical type and current depression (p=0.04). Among females, the odds of reporting current depression were lower in those with anastomoses than those with permanent ostomies (AOR=0.29, CI95% 0.15–0.60). Current depression reporting among males did not differ by initial surgery type.
Among those who recalled being depressed immediately after surgery, survivors with anastomoses had a similar prevalence of current depression (AOR=0.77, CI95% 0.39–1.48) compared to those with permanent ostomies; however, the odds of current depression among survivors with temporary ostomies was significantly less (AOR=0.24, CI95% 0.06–0.95). The odds of reporting current depression among those with no recall of depression immediately after surgery did not vary by surgery type.
Association between perceived financial burden and self-reported depression
A total of 506 participants were included in these analyses. When participants were asked how much financial burden they currently had resulted from illness and treatment, they reported a mean financial burden score of 2 (SD = 2.8) on a scale of 0–10; 22% perceived their current financial burden as moderate-to-high (≥ 4 points). Survivors with depression reported higher crude mean scores for financial burden than those who were not depressed [3.3 (3.2) versus 1.5 (2.4); p<0.001]. Table 1 shows crude mean scores for financial burden by surgery type, recall of depression immediately after surgery, and demographic characteristics. Financial burden scores were higher among survivors who reported depression immediately after surgery, individuals with ≤high school education, those with household income ≤30 K, and individuals who were unemployed or on permanent disability.
Survivors with self-reported current depression perceived high financial burden even after adjusting for confounders (currently depressed: Madj=3.0 versus no depression Madj=1.7, Table 3). Initial surgery type, gender, age, employment status, and household income were included in the final model. After adjustment, survivors with permanent ostomies reported the highest financial burden, although there was no interaction between type of surgery and current depression for the association with financial burden. Among currently-depressed survivors, the adjusted means for those with permanent ostomies, temporary ostomies, or anastomoses were 3.3, 3.1, or 2.9, respectively (NS). Recall of depression at the time of surgery did not modify the association between current depression and current perception of financial burden. However, we observed survivors who reported depression at two points in time perceived moderate-to-high financial burden (Madj=3.8), and those with no depression at either time point had a very low financial burden (Madj=1.3).
Table 3.
Adjusted* mean scores of perceived financial burden by self-reported current depression, surgery type and recall of depression after surgery (N=506).
| Depression in the past 30 days Madj (CI95%) | ||
|---|---|---|
|
| ||
| Yes | No | |
|
| ||
| All | 3.01 (2.57–3.45) | 1.67 (1.43–1.91) |
| Surgery | ||
| Permanent Ostomy | 3.25 (2.72–3.79) | 1.91 (1.51–2.32) |
| Temporary Ostomy | 3.09 (2.36–3.83) | 1.76 (1.14–2.38) |
| Anastomosis | 2.86 (2.39–3.34) | 1.53 (1.22–1.83) |
|
| ||
| Recall of depression after surgery | ||
| Yes | 3.81 (3.33–4.29) | 2.47 (2.06–2.88) |
| No | 2.59 (2.10–3.08) | 1.25 (0.97–1.52) |
Adjusted for reporting depressed in the past 30 days, surgery type, recall of depression immediately after surgery, age, gender, employment status, and household income
Madj = adjusted mean scores, CI95% = 95% confidence interval
Note: A model without any interaction terms was used to estimate the adjusted mean scores
Discussion
We observed the prevalence of self-reported current depression to be 24.7% among long-term RC survivors, with a higher prevalence among those with permanent ostomies (31%). While it is difficult to compare across studies because of varying definitions, it appears that the prevalence of depression in this group is high. The 12-month prevalence of major depressive disorder and dysthymia among the general US population were 6.7% and 1.5%, respectively [30]. The depression prevalence in long-term colorectal cancer survivors was 14% and the prevalence based on DSM-IV criteria in all US cancer survivors was 18.3% [6,31].
Females with permanent ostomies were significantly more likely to report depression than those with anastomoses; however, no significant differences were observed among men by type of surgery. This difference was consistent with a prior study [18].
Regardless of surgery type, survivors who also recalled experiencing depression immediately after surgery were more likely to report feeling depressed again at the time of the survey. This observation was consistent with a prior study suggesting that those who were once depressed were more likely to develop future episodes [32]. Among those who recalled being depressed after surgery, those who had temporary ostomies were less likely to be depressed at the time of the survey than those with permanent ostomies, whereas similar prevalence was observed among those who received either anastomoses or permanent ostomies. Since choice of surgical strategy was not determined randomly, this finding may be due to selection bias.
The association between current depression and perceived financial burden might be explained by prior evidence that depression may increase spending on medical services and decrease an individual’s ability to work productively through having increased limitations in job functioning and higher number of days off work [14,33,34]. People with major depressive disorders have markedly lower personal earnings and household income than those without depression [15].
Perceived financial burden was relatively high among those who both recalled their depression immediately after surgery and were currently depressed. This may imply that those with chronic depression suffer more financially (and financial burden presents higher emotional stress and depressed mood). As those with depression incur high expenses and have diminished financial resources, if chronic depression develops, more financial burden may be added. Few studies have shown the impact of chronic depression on financial attainment. We might be able to draw an analogy from the long-term prospective studies suggesting that early-onset of depression in childhood predicts lower income-earning in adulthood [15].
Importantly, we have to carefully interpret the impact of depression after surgery on our outcomes of interest, since the information on depression after surgery is based on solely patient recall. Answering ‘yes’ on the question – “were you depressed after having your ostomy [operation]?” – can be construed as reflecting the truth (i.e., actual depression) or their present mental stage, which could cloud their report of the past event. Future studies using medical records or diagnostic codes to identify clinical depression are needed to discern the initial episode and assess the chronicity of depression among long-term survivors. This will allow a better evaluation of the implications of being depressed after surgery on survivors’ quality of life in both the short and long term.
This study is the first to investigate relationships between type of surgery and quality of life measures, such as depression and perceived financial burden, within a large group of RC survivors. Strengths of the current study include the use of a validated screening tool for depression, the diverse study population, standardized survey methods and questionnaires, and similar levels of health insurance coverage. In addition to recall bias, potential issues with this cross-sectional study include misclassification of depression. The screening tool used, although valid and reliable, is not the gold standard as compared to use of a semi-structured diagnostic interview [35]. Furthermore, the prevalence of depression among all long-term survivors is underestimated because individuals were excluded from the study if they had a history of more than two mental illnesses, one of which might have included depression. Another potential issue for the study is that the measure used to assess perceived financial burden resulted from illness and treatment was only one item and was based on a subjective measure of the individual’s perception of burden. Future studies could include additional objective measures of financial burden, including total household indebtedness, household income, and rate of household saving and dissaving.
Conclusions
Depressive symptoms are present among long-term RC survivors long after treatment is concluded and the type of surgery performed is associated with this depression. The greatest burden is observed among females with permanent ostomies. Although average perceived financial burden level is low in this population of insured cancer survivors, 20% still reported moderate-to-high burden. Furthermore, current depression is associated with greater perceived financial burden. These findings suggest that depression screening and treatment as well as discussion of financial issues may have important roles in survivorship care planning, particularly for those with permanent ostomies. Special attention may be needed for survivors reporting multiple depressive episodes. Future studies of these survivors should examine the relationships among the timing of the initial occurrence of depression and severity and chronicity of subsequent depression episodes. This would help distinguish those who are in need of extensive interventions from those who may be suitable for less intensive forms of intervention.
Acknowledgments
Dr. Leslie Dennis provided suggestions on early development of the manuscript. Dr. Carmit McMullen provided insightful comments on the manuscript. Also, we thank Mary Wagner, Administrative Assistant, University of Arizona Cancer Center, for help with this work. This manuscript was completed as part of dissertation work for the Epidemiology Graduate Program at the Mel and Enid Zuckerman College of Public Health, The University of Arizona.
Funding Sources:
This research was supported by National Cancer Institute Grant R01 CA106912 and Arizona Cancer Center Support Grant CA023074.
Footnotes
Disclaimer:
The views expressed in this report are those of the authors and do not necessarily represent the views of the University of Arizona or Kaiser Permanente.
Conflicts of Interest:
Dr. Herrinton has had research contracts in the past three years with Proctor and Gamble, Centocor, Genentech, and Medimmune. Dr. Hornbrook has a research contract with Medial Research Inc. The other authors have no conflicts of interest to disclose.
Details of Ethical Committee Review:
All studies were approved by the University of Arizona Institutional Review Board and other collaborating sites where survivors were accrued.
References
- 1.Siegel R, Desantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E. Cancer treatment and survivorship statistics, 2012. CA: a cancer journal for clinicians. 2012 Jul;62(4):220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 2.Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112(S11):2577–2592. doi: 10.1002/cncr.23448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA: a cancer journal for clinicians. 2014 Jan;64(1):9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 4.Honda K, Goodwin RD. Cancer and mental disorders in a national community sample: findings from the national comorbidity survey. Psychother Psychosom. 2004 Jul-Aug;73(4):235–242. doi: 10.1159/000077742. [DOI] [PubMed] [Google Scholar]
- 5.Polsky D, Doshi JA, Marcus S, Oslin D, Rothbard A, Thomas N, Thompson CL. Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med. 2005 Jun 13;165(11):1260–1266. doi: 10.1001/archinte.165.11.1260. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011 Feb;12(2):160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 7.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;(32):57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 8.Brintzenhofe-Szoc KM, Levin TT, Li Y, Kissane DW, Zabora JR. Mixed Anxiety/Depression Symptoms in a Large Cancer Cohort: Prevalence by Cancer Type. Psychosomatics. 2009 Jul;50(4):383–391. doi: 10.1176/appi.psy.50.4.383. [DOI] [PubMed] [Google Scholar]
- 9.MacDonald LD, Anderson HR. Stigma in Patients with Rectal Cancer: A Community Study. Journal of Epidemiology and Community Health (1979-) 1984;38(4):284–290. doi: 10.1136/jech.38.4.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Williams NS, Johnston D. The quality of life after rectal excision for low rectal cancer. Br J Surg. 1983 Aug;70(8):460–462. doi: 10.1002/bjs.1800700805. [DOI] [PubMed] [Google Scholar]
- 11.American Cancer Society. Cancer Treatment and Survivorship Facts & Figures 2012–2013. Atlanta: American Cancer Society; 2012. [Google Scholar]
- 12.Adler NE, Page AEK, editors. Institute of Medicine (IOM) Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academies Press; 2008. [PubMed] [Google Scholar]
- 13.Yabroff KR, Lund J, Kepka D, Mariotto A. Economic burden of cancer in the United States: estimates, projections, and future research. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2011 Oct;20(10):2006–2014. doi: 10.1158/1055-9965.EPI-11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henk HJ, Katzelnick DJ, Kobak KA, Greist JH, Jefferson JW. Medical costs attributed to depression among patients with a history of high medical expenses in a health maintenance organization. Arch Gen Psychiatry. 1996 Oct;53(10):899–904. doi: 10.1001/archpsyc.1996.01830100045006. [DOI] [PubMed] [Google Scholar]
- 15.Kessler RC. The costs of depression. Psychiatr Clin North Am. 2012 Mar;35(1):1–14. doi: 10.1016/j.psc.2011.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richardson A, Addington-Hall J, Amir Z, Foster C, Stark D, Armes J, Brearley SG, Hodges L, Hook J, Jarrett N, Stamataki Z, Scott I, Walker J, Ziegler L, Sharpe M. Knowledge, ignorance and priorities for research in key areas of cancer survivorship: findings from a scoping review. Br J Cancer. 2011 Nov 8;105( Suppl 1):S82–94. doi: 10.1038/bjc.2011.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reyes-Gibby CC, Anderson KO, Morrow PK, Shete S, Hassan S. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health (Larchmt) 2012 Mar;21(3):311–318. doi: 10.1089/jwh.2011.2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krouse RS, Herrinton LJ, Grant M, Wendel CS, Green SB, Mohler MJ, Baldwin CM, McMullen CK, Rawl SM, Matayoshi E, Coons SJ, Hornbrook MC. Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. J Clin Oncol. 2009 Oct 1;27(28):4664–4670. doi: 10.1200/JCO.2008.20.9502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hornbrook MC, Wendel CS, Coons SJ, Grant M, Herrinton LJ, Mohler MJ, Baldwin CM, McMullen CK, Green SB, Altschuler A, Rawl SM, Krouse RS. Complications among colorectal cancer survivors: SF-6D preference-weighted quality of life scores. Med Care. 2011 Mar;49(3):321–326. doi: 10.1097/MLR.0b013e31820194c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jansen L, Herrmann A, Stegmaier C, Singer S, Brenner H, Arndt V. Health-related quality of life during the 10 years after diagnosis of colorectal cancer: a population-based study. J Clin Oncol. 2011 Aug 20;29(24):3263–3269. doi: 10.1200/JCO.2010.31.4013. [DOI] [PubMed] [Google Scholar]
- 21.Grant M, McMullen CK, Altschuler A, Mohler MJ, Hornbrook MC, Herrinton LJ, Wendel CS, Baldwin CM, Krouse RS. Gender differences in quality of life among long-term colorectal cancer survivors with ostomies. Oncol Nurs Forum. 2011 Sep;38(5):587–596. doi: 10.1188/11.ONF.587-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wendel CS, Grant M, Herrinton L, Temple LK, Hornbrook MC, McMullen CK, Bulkley JE, Altschuler A, Krouse RS. Reliability and validity of a survey to measure bowel function and quality of life in long-term rectal cancer survivors. Qual Life Res. 2014 Jun 3; doi: 10.1007/s11136-014-0724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant M, Ferrell B, Dean G, Uman G, Chu D, Krouse R. Revision and psychometric testing of the City of Hope Quality of Life-Ostomy Questionnaire. Qual Life Res. 2004 Oct;13(8):1445–1457. doi: 10.1023/B:QURE.0000040784.65830.9f. [DOI] [PubMed] [Google Scholar]
- 24.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996 Mar;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Maruish ME, DeRosa MA. A guide to the integration of certified Short Form survey scoring and data quality evaluation capabilities. Lincoln, RI: QualityMetric Incorporated; 2009. [Google Scholar]
- 26.Vilagut G, Forero CG, Pinto-Meza A, Haro JM, de Graaf R, Bruffaerts R, Kovess V, de Girolamo G, Matschinger H, Ferrer M, Alonso J. The mental component of the short-form 12 health survey (SF-12) as a measure of depressive disorders in the general population: results with three alternative scoring methods. Value Health. 2013 Jun;16(4):564–573. doi: 10.1016/j.jval.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 27.Paz SH, Globe DR, Wu J, Azen SP, Varma R. Relationship between self-reported depression and self-reported visual function in Latinos. Arch Ophthalmol. 2003 Jul;121(7):1021–1027. doi: 10.1001/archopht.121.7.1021. [DOI] [PubMed] [Google Scholar]
- 28.Yochim BP, Kerkar SP, Lichtenberg PA. Cerebrovascular risk factors, activity limitations, and depressed mood in African American older adults. Psychology and Aging. 2006;21(1):186–189. doi: 10.1037/0882-7974.21.1.186. [DOI] [PubMed] [Google Scholar]
- 29.Reyes-Gibby CC, Swartz MD, Yu X, Wu X, Yennurajalingam S, Anderson KO, Spitz MR, Shete S. Symptom clusters of pain, depressed mood, and fatigue in lung cancer: assessing the role of cytokine genes. Support Care Cancer. 2013 Jul 13; doi: 10.1007/s00520-013-1885-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005 Jun;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramsey SD, Berry K, Moinpour C, Giedzinska A, Andersen MR. Quality of life in long term survivors of colorectal cancer. Am J Gastroenterol. 2002 May;97(5):1228–1234. doi: 10.1111/j.1572-0241.2002.05694.x. [DOI] [PubMed] [Google Scholar]
- 32.Kiloh LG, Andrews G, Neilson M. The long-term outcome of depressive illness. Br J Psychiatry. 1988 Dec;153:752–757. doi: 10.1192/bjp.153.6.752. [DOI] [PubMed] [Google Scholar]
- 33.Spiegel D, Giese-Davis J. Depression and cancer: mechanisms and disease progression. Biol Psychiatry. 2003 Aug 1;54(3):269–282. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- 34.Judd LL, Paulus MP, Wells KB, Rapaport MH. Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry. 1996 Nov;153(11):1411–1417. doi: 10.1176/ajp.153.11.1411. [DOI] [PubMed] [Google Scholar]
- 35.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; Nov, 2002. [Google Scholar]