Abstract
Background
Despite 82% of patients reporting psychosocial improvement following breast reconstruction, only 33% patients choose to undergo surgery. Implant reconstruction outnumbers autologous reconstruction in many centres.
Methods
A systematic review of the literature was undertaken. Inclusion required: (I) Meta-analyses or review articles; (II) adult patients aged 18 years or over undergoing alloplastic breast reconstruction; (III) studies including outcome measures; (IV) case series with more than 10 patients; (V) English language; and (VI) publication after 1st January, 2000.
Results
After full text review, analysis and data extraction was conducted for a total of 63 articles. Definitive reconstruction with an implant can be immediate or delayed. Older patients have similar or even lower complication rates to younger patients. Complications include capsular contracture, hematoma and infection. Obesity, smoking, large breasts, diabetes and higher grade tumors are associated with increased risk of wound problems and reconstructive failure. Silicone implant patients have higher capsular contracture rates but have higher physical and psychosocial function. There were no associations made between silicone implants and cancer or systemic disease. There were no differences in outcomes or complications between round and shaped implants. Textured implants have a lower risk of capsular contracture than smooth implants. Smooth implants are more likely to be displaced as well as having higher rates of infection. Immediate breast reconstruction (IBR) gives the best aesthetic outcome if radiotherapy is not required but has a higher rate of capsular contracture and implant failure. Delayed-immediate reconstruction patients can achieve similar aesthetic results to IBR whilst preserving the breast skin if radiotherapy is required. Delayed breast reconstruction (DBR) patients have fewer complications than IBR patients.
Conclusions
Implant reconstruction is a safe and popular mode of post-mastectomy reconstruction. Evidence exists for the settings in which complications are more likely, and we can now more reliably predict outcomes of reconstruction on an individual basis and assess patient suitability.
Keywords: Breast cancer, breast implant, prosthesis, reconstruction, tissue expander, alloplastic
Introduction
In 2010, breast cancer was the most common cancer amongst Australian women, with 14,181 new diagnoses (1). Breast cancer comprises 28% of all new cancers in women and the risk of developing breast cancer before the age of 85 is 1 in 8 (1). Approximately 35-40% of women diagnosed with breast cancer undergo a total mastectomy, a trend which is increasing (2). Fewer than 33% of those who are suitable undergo breast reconstruction (2) despite 82% of women reporting psychosocial improvement following reconstruction (3).
Although reconstruction using a transverse rectus abdominis musculocutaneous (TRAM) flap or a deep inferior epigastric artery perforator (DIEP) flap offers women the option of autologous reconstruction, prosthetic reconstruction is still widely used. Data from the United States indicate that between 1998 and 2008, there was an 11% increase in the use of implants per year, whereas autologous reconstruction rates remained stable (4,5). Indeed, the data shows that prior to 2002, autologous reconstructions were the more frequently chosen method of reconstruction compared with the use of prostheses. However, after 2002, this relationship was reversed and in 2008 implants outnumbered autologous reconstructions by a ratio of 2:1 (258 vs. 120 per 1,000 mastectomies) (4). Albornoz et al. (4) suggests a number of reasons behind this change in trend; the longer time it takes to perform autologous reconstruction, a cultural shift towards acceptance of breast implants, and the way in which reconstruction is funded. In the US Medicare funding for autologous implants decreased between 1998 and 2008. Also private insurance companies increased payment for implant reconstruction by 64%, while reimbursement for autologous reconstruction was unchanged (4).
In the 1960s silicone breast implants were introduced, launching the era of modern breast reconstruction. Radovan (6) pioneered the use of tissue expanders in the early 1980s which has allowed for further reconstructive options. Since then, there have been great advances in the both the technique of expander/implant breast reconstruction and in the prostheses themselves (7).
The decision for autologous vs. prosthetic reconstruction is a decision that requires a long discussion between the patient and surgeon which must take into account many factors. There are many advantages and disadvantages that autologous reconstruction has over prosthetic reconstruction which is outside the scope of this article. Once the decision has been made to pursue prosthetic breast reconstruction, the aim of this article is to provide a summary of the current data to assist the clinician in the complex decision making process that follows.
In considering prosthetic breast reconstruction, a number of factors need to be considered by both surgeon and patient. The indications and selection of patients for prosthetic reconstruction will be discussed as will the timing of reconstruction following mastectomy. Integral to this is determining whether or not adjunctive therapy is required as this can greatly affect the outcome of prosthetic reconstruction.
Methods
The current study comprises a systematic review of the literature focusing on the evidence for prosthetic breast reconstruction.
Study identification
Multiple databases were searched independently by two authors (TQ and GM), including: Ovid Medline (1950 to present), EMBASE (1980 to 2015), PubMed and Cochrane Database of Systematic Reviews.
The following search terms and Boolean operators were used: (I) “breast reconstruction” or “breast neoplasm,” or “breast implants” or “breast” and (II) “alloplastic” or “prosthesis” or “implants”. Additional searches were conducted using (I) and (II) and “tissue expansion devices” or tissue expander”; (I) and (II) and “surgical flaps” or “mammoplasty” or “mastectomy” as well as (I) and (II) and “reconstructive surgical procedure”.
Inclusion criteria
Inclusion criteria for studies reviewed included: (I) meta-analyses or review articles; (II) adult patients aged 18 years or over undergoing post-mastectomy alloplastic breast reconstruction (i.e., tissue expander or implant based); (III) studies including outcome measures; (IV) case series with more than 10 patients; (V) published since 1 January 2000; and (VI) English language.
Data extraction
A systematic review was conducted using the PRISMA 2009 statement. Data was extracted by two authors (TQ and GM), and included author, year, journal, study design, level of evidence, outcome details, number of patients (if applicable), and follow up period. Differences in data extraction were corrected via discussion.
Literature search results
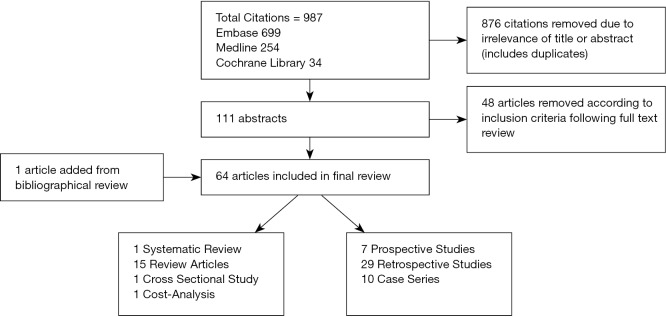
The search was conducted on April 10, 2015, resulting in 987 articles, managed using Endnote X7TM (Thomson Reuters, Philadelphia, PA). A summary of the literature review process is shown in Figure 1. After the authors independently assessed the titles a total of 876 articles were removed for irrelevance or duplication. The abstracts for the remaining articles were then reviewed based on the inclusion criteria, leaving a total of 111 articles for full review. A further one article was added based on review of bibliographies. Fifty studies were eliminated after full review (due to publication date prior to the year 2000, inadequate outcome measures, and case series fewer than 10 patients). After full text review, analysis and data extraction was conducted for a total of 62 articles, summarized in Table S1.
Figure 1.
Article selection.
Outcomes on the 62 articles that met the inclusion criteria were summarized and analyzed. The breakdown of the types of articles included was 1 systematic review, 14 reviews, 7 prospective studies, 26 retrospective studies, 10 case series, 1 cost-analysis, and 3 cross-sectional studies).
Discussion
Indications and patient selection
Most patients who undergo mastectomy for breast cancers are candidates for prosthetic reconstruction. There are factors that limit a patient’s ability to undergo autologous reconstruction. This may include general medical health, an unsuitable donor site, lifestyle factors and availability of resources. Prosthetic breast reconstruction, however, can be a safe and viable option, even for older patients. Indeed, Hershman et al. [2012] reported that the immediate in-hospital complication rate was significantly higher in patients who underwent autologous reconstruction when compared to those who had prosthetic reconstruction (8).
The choice of whether or not to undergo reconstruction can be a complex. This has been studied by Reaby et al. [1998] (9) and by Ng et al. [2014] (10). Many patients choose not to undergo reconstruction. This may be because they lack information about the procedures, do not feel that it was necessary for their physical or emotional well-being or that due to fears that it would mask cancer recurrence (9). Of the approximately 33% (2), however that do choose reconstruction, they report that they did so because they could get rid of external prostheses, be able to wear many types of clothing, regain their femininity and to feel “whole” again after the surviving breast cancer (9). In the areas of social functioning and emotional wellbeing, it has been reported that patients who underwent reconstruction did better than those who did not have reconstruction (11). Some patients may have unclear and potentially inaccurate expectations of the appearance of, and physical sensation, in particular the “unnatural feel”, firmness and lack of movement, associated with prosthetic breast reconstruction which can lead to dissatisfaction with the outcome (12).
Definitive reconstruction with an implant can be done either at the time of the mastectomy, referred to in this article as immediate breast reconstruction (IBR), or as a two-stage reconstruction with a tissue expander followed by a permanent implant and most of the time with intervening (13) adjuvant therapy, a process referred to in this article as delayed breast reconstruction (DBR). Clinicopathological features which are considered when making decision regarding the type of reconstruction include cancer stage, status of the sentinel node, smoking, body habitus, pre-existing scars and prior radio or chemotherapy (14).
Immediate reconstruction is preferred where possible because of the psychological and physical benefits attained from restoration of mammary volume and shape (15) and is associated with a high level of patient satisfaction (16). Prosthetic breast reconstruction has the advantages of shorter procedure time, hospital stay and recovery as well as being lower cost (17) and not having an additional donor site associated with an autologous reconstruction (18). Unfortunately, having prosthetic IBR is associated with requiring unplanned surgery in the future to revise the reconstruction (19,20) and a higher complication rate related to prosthesis failure (21). Patients with small, minimally ptotic breasts are ideal candidates for single-stage reconstruction (22) as are patients who have a good cancer prognosis, who are sentinel node negative and therefore do not require axillary surgery and have late local recurrence (LR) in a previously treated breast (23). Patients with larger and/or ptotic breasts are not ideal candidates for IBR as they often need contralateral balancing procedures to achieve symmetry which can be difficult to judge at the time of immediate reconstruction (24).
Delayed or two-stage reconstruction with a tissue expander followed by a permanent implant is an alternative pathway for prosthetic reconstruction. Tissue expansion is simple, safe and allows for preservation of the skin envelope and allows for better matched color, texture and hair-bearing qualities of the skin (25). It also allows for implantation of synthetic materials underneath the expanded tissue as the skin flaps are vascularized (25). Tissue expansion is recommended in patients who require adjuvant radiotherapy as radiotherapy can adversely affect the aesthetic outcome, and tissue expanders can impede effective and safe radiation delivery to the internal mammary and axillary lymph nodes (26).
Breast reconstruction in the elderly
Despite the recent increase in the rate of immediate reconstruction, many older women choose not to undergo breast reconstruction following mastectomy due to the fear of complications and the perception that they are “too old” for the procedure (9).
The literature indicates that older patients tolerate breast reconstruction well. Walton et al. [2011] reports similar complication rates in older compared to younger patients but that autologous reconstruction result in better outcomes than implant reconstruction (11). August et al. [1994] reported, in a patient cohort of 242, that there were significantly fewer complications in women over the age of 60 following both IBR and DBR. It was also noted that older women tended to require fewer operations to achieve the final results compared to their younger counterparts (27).
Risks and complications of prosthetic reconstruction
The most common complications associated with prosthetic reconstruction include capsular contracture, hematoma and infection (28). The complication rate was significantly lower when implants were inserted for cosmetic reasons (6.5% at 1 year and 12% at 5 years) compared to those who had expanders inserted either following prophylactic mastectomy (17.3% at 1 year and 30.4% at 5 years) or mastectomy for cancer (21.8% at 1 year and 34% at 5 years) (28). In a systematic review of 14 observational studies, which included more than 3,000 breasts, Tsoi et al. [2014] concluded that reconstructive failure and surgical site infection was higher in patients who had prosthetic reconstruction compared to those who underwent autologous reconstruction (29).
Wound complications are associated with large breast volume (greater than 750 g) and sternal notch to nipple length of greater than 26 cm (30). Significant risk factors for reconstructive failure include smoking (31), obesity (32), incomplete muscle coverage (31), implant volume >400 mL (31), type 2 diabetes mellitus (32), higher grade tumors and nodal involvement (33). Although not a statistically significant risk factors for complications, older age was associated with a borderline increased risk of complications in both IBR and DBR (31). Tamoxifen, an oestrogen receptor antagonist use is associated with a borderline risk of complications but a significant risk of reconstructive failure in patients who undergo expander/implant reconstruction (34).
Capsular contracture
Capsular contracture development is multifactorial. Numerous potential aetiologies and contributing factors have been described including bacterial colonization, the type and texture of the implant, the placement of the implant and the use of radiotherapy (35). Overall incidence of significant capsular contracture (Baker classification III or IV) ranges from 10.4% (36) to 29% (37). Capsular contracture rates in immediate reconstruction has been reported as being between 20% (38) to 40.4% (39) and rates for delayed reconstruction range from 17% (39) to 26.4% (38). Smoking, use of smooth implants (40) and hematoma increased the risk of developing contractures, as does the duration of implantation (41).
Staphylococcus epidermis’s is the bacteria most implicated in capsular contracture. It exists in the ductal system in the breast and has been cultured from breast milk, nipple secretions and biopsied from breast parenchyma (42). Bacterial etiology is a likely major contributor of capsular contracture. Bacteria adhere easily to silicone and form a biofilm comprised of extracellular polysaccharides and glycoprotein. Virden et al. (42) cultured 55 silicone implants at the time of removal. Bacterial growth was detected in 56% of implants surrounded by contracted capsules compared to 18% of implants without contracted capsules, a significant difference. Patients who undergo radiotherapy are at significant risk of developing capsular contracture. Patani et al. [2008] reports a rate of capsular contracture requiring capsulotomy as a staggering 87%, compared to 13% in those who did not have radiotherapy (43). Of the 71% of patients receiving radiotherapy who developed capsular contracture in the study conducted by Ringberg et al. [1999], 8% had Baker classification III and IV contractures (44). The use of a flap with the implant seems to mitigate capsular contracture, reducing the risk of capsular contracture to 6.8% compared to a rate of 25% of those who had implants alone (41).
In a series of 326 tissue expanders, Rheingold et al. [1994] reported an overall contracture rate of 78.5% Baker I, 12% Baker II, 8.6% Baker III and 0.9% Baker IV contractures (45). Holmes et al. [1989] reported that neither the speed of expansion, nor the degree of over-expansion influenced the onset of contracture. However, patients with Baker I contractures had a significantly longer interval been full expansion and definitive recon than did those who developed Baker III contractures (37).
Types of prostheses
Silicone vs. saline implants
Gylbert et al. [1990] reported a higher capsular contracture rate in silicone implants (50%) compared to 16% of saline implants. However, 16% of the saline implants deflated. Despite the higher contracture rates amongst the silicone implant group, 85% of the patients in this study reported that they were satisfied with the reconstruction (46). Both Macadam et al. [2010] (47) and McCarthy et al. [2010] (48) report that patients who have silicone implants have higher quality of life and satisfaction scores than those with saline implants. There is also a statistically significant difference in overall physical function (silicone implants performed better) and systemic side effects (higher in patents with saline implants).
Despite concerns, there has been no associations found between silicone implants and cancer, immunological or systemic disease (49).
A prospective review from 1990 to 1997 by Spear et al. [2000] reviewed 40 consecutive patients with saline implants (50). Almost half (47.5%) of irradiated breasts with saline implants required revision or replacement by a flap (compared to 10% of control group who required revision with a flap but none required replacement). Patients with saline implants also had higher contracture rate of 32.5%
One type of implant containing hydrogel filler (polyvinylpyrrolidone and guar gum) was reported as having similar contracture rates to saline implants but twice the rupture rate. This was subsequently withdrawn from use in the United Kingdom market in 2000 (51).
Round vs. anatomic implants
The consensus is that there is no difference seen between round and shaped implants including rippling, overall satisfaction with breast and outcome (52).
Cohesive gel implants are comprised of a textured silicone elastomer shell filled with cohesive silicone gel. There is increased number of cross links between gel molecules which results in better shape retention and less likely to collapse (53). Highly cohesive shaped devices have been reported to be firmer than the less cohesive round implants. In addition, because of the added cohesivity of the shaped implant, there may be less rippling (52). In cases that involve reconstructing an upper pole deficiency of the breast an anatomic implant is favoured. Round implants are usually favoured when there is no appreciable upper pole deficiency. Nahabedian et al. [2014] reported similar complication rates between the two strategies (54).
Textured vs. smooth implants
Textured implants form thinner and more pliable capsules that are less likely to contract than smooth implants. In a review of 16 randomized control trials and two retrospective trials, Liu et al. [2015] found that smooth implants were more likely to be associated with capsular contracture than textured implants (55). About 96% of textured implants were reported to have a satisfactory (Baker classification Grade II or better) result compared to 72% of patients who had a smooth implant inserted (56).
The contracture rate reported by Embrey et al. [1999] was 58% for smooth implants compared to 8% for textured implants (35). Hakelius et al. [1992] performed bilateral, sub-glandular implant insertion in 25 patients for mammary hypoplasia. In each case one smooth and one textured implant was inserted. It was found that at 1 year, the textured implant was less likely to develop contractures (57). Longer-term follow up at 10 years found a reduced rate of contractures in textured implants compared to smooth implants (58) with a reported contracture rate of 65% in smooth implants vs. 11% in textured implants (40). Not only are smooth implants associated with significant capsular contracture they also are more likely to be displaced as well as having higher rates of infection and pain on expansion (59). Textured implants, in contrast, maintained their position and expanded easily with minimal pain (59).
Integrated port vs. distant port tissue expanders
The Becker Expander, (TM) a textured tissue expander produced by Mentor, which has a distant port, offers the advantage of single-stage reconstruction. The expander is filled until the desired volume is reached prior to the ports being removed under local anesthetic and the expanders being left in-situ as implants. Large series have reported good outcomes at 3 years. However at 5 years Chew et al. [2010] found that 68% were removed due to complications (poor aesthetics, capsular contracture, infection). The congenital hypoplasia group had better retention rates (67% at 10 years) than oncological (2%) or risk reducing mastectomy (5%) groups (60).
Spear et al. [1998] performed 171 consecutive reconstructions using textured, integrated valve expanders. All were two-stage reconstructions. Four percent deflated over 7 years, 2 were removed for infection and 1 electively. About 98% of a subgroup of 42 patients were satisfied with their reconstructions (61). Yanko-Arzi et al. [2009] found more complications with integrated-valve expanders compared to those with distant inflation ports (62).
Timing of reconstruction with prostheses
Albornoz et al. [2013] reports that from 1998 to 2008, there was a 78% increase in the rate of IBR from 20.8% to 37.8%, an average of 5% per year (4). IBR gives the best aesthetic outcome if radiotherapy is not required (63), and patients who received IBR had better physical and psychosocial scores than those undergoing DBR (64). As mastectomy defects can result in the loss of body integrity and femininity, patients who have IBR have higher satisfaction levels than those who have delayed reconstructions (32). Factors associated with an increase likelihood of IBR included large hospital size with a high number of patients requiring IBR and surgeons who perform IBR regularly. Decreased likelihood was associated with increased age, black race, patients who were married, patients from rural locations and patients with increased comorbidities (8).
The early complication rate ranges from 9.2% (65) to 16% (66) and include skin flap necrosis, infection, sarcoma, hematoma and a 1.7% risk of explantation (65). Late complication rates have been reported to be as high as 23% (65). Unfortunately the cosmetic outcome following IBR diminished over time from 86% acceptable cosmetic appearance at 2 years to 54% acceptable cosmetic appearance at 5 years, independent of radiotherapy, type of implant, volume of implant, age of the patient or the type of mastectomy incision used (65).
There is a reported revisional surgery rate of 30.2% following IBR (65). Fifty seven percent of IBR required revision compared to 27% of DBR (67), although the two groups had similar complication rates and failure rates. Patients undergoing IBR also need more capsular intervention procedures which leads to greater expense but they can obtain good results due to revisional surgery (68). The risk of requiring revision is higher if the patient has undergone radiotherapy, is D-cup size or larger, or has grade 2 or 3 ptosis of the breast (67).
The rate of complications is higher in patients who have IBR compared to the DBR group (69), with capsular contracture being the most significant complication (40.4% vs. 17%) (39). The negative effect of radiotherapy is more significant with IBR than DBR groups (70). The rate of implant loss has been reported from 1.7% (65) to 18% (31). IBR is reported to have a higher overall complication and implant failure rate than DBR (71).
Delayed-immediate reconstruction
Patients who are anticipated to require radiotherapy who desire breast reconstruction are considered candidate for delayed-IBR (63). Using the delayed-immediate protocol enables surgeons to provide the near optimal reconstruction despite whether radiotherapy eventuates or not. Those patients who do not end up needing radiotherapy achieve aesthetic results comparable to patients who undergo IBR. For the patients who do end up receiving radiotherapy, the aesthetic problems usually associated with radiotherapy following IBR are avoided (30). This protocol of breast reconstruction also allows for skin-preserving DBR after radiotherapy for patients in whom radiotherapy only becomes apparent after review of the pathological sections post mastectomy. Preserving the breast skin envelope in patients who have undergone radiotherapy allows for the direct placement of an implant and decreases the need for addition of autologous flaps or at least minimizes the dimensions of the skin island required from an autologous flap.
In stage 1 of a delayed-immediate reconstruction, patients undergo a skin sparing mastectomy plus the insertion of an expander, with or without the addition of an acellular dermal matrix (ADM). The expander is then filled to the required volume intraoperatively. The pathology is subsequently examined and the patient discussed at a multidisciplinary team (MDT) meeting. If radiotherapy is not required, the patient proceeds to have definitive reconstruction (stage 2) with an autologous flap, flap plus implant or implant alone. If radiotherapy is required, however, the expander is deflated following the course of chemotherapy (if the patient is having it) and prior to radiotherapy planning. She then undergoes radiotherapy, has the expander re-expanded then completes stage 2 of the reconstruction three months after radiotherapy is completed.
Delayed breast reconstruction (DBR)
DBR is significantly more common in the USA than elsewhere in the world (72). A two-stage reconstruction gives a more predictable result as it can be adjusted at the second operation (24). Multiple authors have suggested that patients who undergo DBR have fewer complications than patients who have IBR. Francel et al. [1993] found that patients who had DBR were less likely to require surgery to correct capsular contracture (67). Cosmetic results in patients who have DBR 6 weeks after radiotherapy were found to be superior when compared to those who had IBR (73). The timing of reconstruction after radiotherapy is also important. Lentz et al. [2013] studied patients who had reconstruction within 4 months following compared to patients who had reconstruction greater than 4 months after radiotherapy. The former group had a non-significant trend towards increased infection whilst the latter tended to have a higher capsular contracture rate (74).
The concept of “delayed-delayed” prosthetic reconstruction is described by Kronowitz et al. [2015] (26). Neoadjuvant chemotherapy and radiotherapy in conjunction with skin sparing mastectomy in patients who have locally advanced breast cancer is increasingly resulting in good long-term disease control and survival (26). Following neoadjuvant chemotherapy, which decreases the need to resect skin at the time of mastectomy, patients with locally advanced breast cancer are discussed at an MDT and eligibility for skin sparing DBR is decided. For those that are deemed suitable, they undergo a skin-sparing mastectomy with insertion of a tissue expander with or without ADM. The expander is filled intra-operatively but then is partially deflated immediately prior to planning for radiotherapy. After the resolution of any radiation induced skin desquamation the expander is re-inflated to the pre-deflation volume and 3 months after radiotherapy and re-inflation, the definitive reconstruction is performed. The aim of this is protocol is to improve aesthetic outcome, decrease complications and reduce psychological disadvantages associated with DBR after radiotherapy.
Radiotherapy and prosthetic breast reconstruction
More centers globally are recommending radiotherapy for patients with breast cancer, including early breast cancer, which increases the complexity of reconstructive planning (26). The USA has been reported to have higher rates of reconstruction prior to radiotherapy than elsewhere in the world (72). Chen et al. [2013] found that 57% of 358 surveyed radiation oncologists felt that breast reconstruction challenged their ability to deliver effective radiation. Sixty percent preferred a moderately inflated expander (150-250 CC) compared to completely deflated (13%) or completely inflated (28%) (72).
In a review article by Fodor et al. [2003] the most common type of complication associated with radiotherapy was significant capsular contracture (Grade III or IV) (69). Rates of capsular contracture varied from 29% (75) to 68% (76) in patients who had radiotherapy compared to 10% (77) to 40% (34) of those who did not have radiotherapy. The risk of significant capsular contracture (Baker Grade III or IV) was also higher in irradiated breasts (33). Patients who had moderate skin changes and no induration had similar aesthetic outcomes to non-irradiated chest walls. However those who developed induration or severe post-radiotherapy skin changes had a greater chance of Baker IV contracture (78). Capsular contracture was also found to be associated with a significant increase in persistent pain 2 years following surgery (79).
The risk of overall complications was also found to be significantly higher in patients who had radiotherapy (80). Fodor et al. [2003] reports that 0-64% of IBR patients and 22-55% of DBR developed complications compared to 0-12% of IBR patients and 13-34% of DBR who did not have radiotherapy (70). Radiotherapy is also associated with significantly higher rates of reconstruction failure with rates varying from 22.7% (33) to 37% (34). As such, radiotherapy significantly increases the number of secondary procedures required in both unilateral and bilateral reconstruction (81,82). Reconstruction with prostheses following radiotherapy was found to be much more reliable when used in conjunction with a flap (83,84). Overall, patients who have radiotherapy have significantly lower satisfaction with their physical and psychosocial outcomes compared with non-irradiated patients when adjusted for other treatment factors (85).
Outcomes
Satisfaction rates following prosthetic breast reconstruction is up to 85% (16,44). Lifestyle and social relations had improved in 82% and 53% of patients respectively post reconstruction (3). Klit et al. [2013] reported that there was no significant difference in the reported levels of pain experienced by patients who had prosthetic reconstruction compared to those who did not. Also, the timing of the reconstruction (immediate vs. delayed) did was not associated with a significant difference in pain (86). Although 60% of reconstructions resulted in some complication or complaint, patients feel more balanced and whole, are less depressed and were glad they had the reconstruction (87).
The patient’s acceptance of cosmesis was found to be better if she could see photos or have a discussion with patients who had previously undergone similar process (88). Having bilateral (vs. unilateral) and not having radiotherapy were significant predictors in good cosmetic outcomes (36). Understandably, failure of the reconstruction was associated with significantly decreased aesthetic satisfaction (34).
In order to give all eligible patients equal opportunity to have the best possible outcomes with breast reconstruction, treatment should be centralized in hospitals with a MDT team comprising of, amongst others, an oncological breast surgeon, pathologist, radiologist, oncologists and plastic surgeons (89).
Conclusions
Implant reconstruction following mastectomy has increased at a steady rate since 1998 and is now utilized more frequently than autologous reconstruction. This trend can be attributed to the increased understanding of indications and patient selection for implant reconstruction. This understanding is derived from evidence regarding common and long-term complications, as well as evidence regarding type of prostheses; timing options for reconstruction; and the adjuvant use of radiotherapy (Table 1). We can now more reliably predict outcomes of reconstruction on an individual basis and assess patient suitability to many different reconstructive options.
Table 1. Key points.
| Incidence of breast cancer 1 in 8 in Australia |
| Only 33% choose to have reconstruction despite an 82% psychosocial improvement |
| Implant use has increased by 11% per year from 1998-2008 and now exceeds autologous reconstruction |
| Indication and patient selection |
| Most patients are candidates for prosthetic reconstruction |
| Consider clinicopathological features when making decision |
| Patients with small, minimally ptotic breasts are suitable for immediate reconstruction |
| Patients with large, ptotic breasts or who need radiotherapy are better suited to delayed reconstruction |
| Breast reconstruction in the elderly |
| Older patients tolerate reconstruction well and can have fewer complications |
| Risks and complications |
| Common complications-capsular contracture, hematoma and infection |
| Risks for complications-smoking, obesity, large breast volume, diabetes, higher grade tumors |
| Multifactorial-bacterial colonization, type/texture/placement of implant and radiotherapy |
| Incidence of significant capsular contracture up to 209% |
| Types of prostheses |
| Silicone vs. saline |
| Higher capsular contracture rate in silicone |
| Higher satisfaction and quality of life scores for silicone |
| Silicone not associated with cancer, immunological or systemic disease |
| Round vs. anatomic |
| No significant difference |
| Anatomic implants may feel firmer and have less rippling |
| Textured vs. smooth |
| Textured have lower risk of capsular contracture |
| Smooth more likely to be displaced and cause more pain on expansion |
| Integrated vs. distant port |
| No significant difference |
| Timing of reconstruction |
| Immediate |
| Best aesthetic outcomes if no radiotherapy needed |
| Higher rate of complications, capsular contracture, implant failure and revision surgery |
| Delayed-immediate |
| Achieve similar aesthetic results to immediate reconstruction |
| Preserves the breast skin if radiotherapy required |
| Delayed |
| Fewer complications than immediate reconstruction |
| Better aesthetic results if radiotherapy required compared to immediate reconstruction |
| “Delayed-delayed”-for locally advanced breast cancer patients requiring neoadjuvant chemotherapy. Improves aesthetics and reduces psychological disadvantages associated with DBR |
| Radiotherapy |
| Increases risk of capsular contracture-occurs in 68% of irradiated breasts |
| Higher risk of complications and reconstruction failure |
| More likely to need revision surgery |
| Lower patient satisfaction with outcome |
| Outcomes |
| High satisfaction rates with prosthetic reconstruction |
| Cosmesis better accepted if patient better informed |
| Better aesthetic outcomes associated with having bilateral reconstruction and not having radiotherapy |
| Patients receive best treatment in hospitals with multidisciplinary breast team |
DBR, delayed breast reconstruction.
Acknowledgements
None.
Table S1. Summary of articles.
| Author, country | Title | Year | Level of evidence | Type of article | Timing of reconstruction | Sample population | Follow up | Summary of recommendations | |
|---|---|---|---|---|---|---|---|---|---|
| Kronowitz, USA (63) | Delayed-IBR | 2004 | IV | Case Series | Delayed-immediate | 14 patients (16 breast reconstructions) | Where no radiotherapy is required immediate reconstruction gives the best aesthetic outcome. Where radiotherapy is required, delayed-immediate reconstruction is technically feasible and safe in patients with early-stage breast cancer. With this approach, patients who do not require post-mastectomy radiation therapy can achieve aesthetic outcomes essentially the same as those with immediate reconstruction, and patients who require post-mastectomy radiation therapy can avoid the aesthetic and radiation-delivery problems that can occur after an IBR | ||
| Racano, Italy (15) | Immediate and delayed two-stage post-mastectomy breast reconstruction with implants. Our experience of general surgeons | 2002 | IV | Case Series | Immediate and delayed | 63 patients | 10-36 months | 78% of the women have judged the final aesthetic results the same or better than expected. Reconstruction with prosthesis is the preferred procedure, even with serious complications which do not always influence the final results. This preference is because of the reduced operation time and the psychological and physical benefits due to immediate restoral of the mammary volume and shape | |
| Radovanovic, Serbia (66) | Early complications after nipple-sparing mastectomy and IBR with silicone prosthesis: results of 214 procedures | 2010 | IV | Case Series | Immediate | 205 patients (214 breast reconstructions) | 6 weeks | The overall complication rate at 6-week follow up was 16%. Neoadjuvant chemotherapy and radiotherapy were not associated with higher complication rates. Nipple-sparing mastectomy with immediate implant reconstruction has acceptable morbidity rate in the hand of experienced neoplastic surgeon and therefore should be considered as treatment option to women requiring mastectomy | |
| Robertson, Sweden (19) | Breast surgeons performing IBR with implants - assessment of resource-use and patient-reported outcome measures | 2012 | IV | Case Series | Immediate | 223 patients | 4 years | 41% of patients had received post-mastectomy radiation therapy. A total major complication rate was reported of 19.7%. A total of 1.1 revision operations were required per patient. Our audit showed that trained breast surgeon specialists perform implant-based IBRs and maintain low complication rates. This audit also showed that the IBR does not have a negative impact on the patients’ current state of health | |
| Roostaeian, USA (22) | Immediate placement of implants in breast reconstruction: patient selection and outcomes | 2011 | IV | Case Series | Immediate | 35 patients (43 breast reconstructions) | 15 months | A total of 13 patients (37%) required additional surgery for revision. Revisions were necessary significantly more commonly in patients with a history of radiotherapy, D-cup breast size or greater, and ptosis of grade 2 or more. Immediate implant-based breast reconstruction is a safe and viable option that can provide a very good aesthetic result in appropriately selected candidates. The authors recommend caution and appropriate patient counseling in patients with a history of radiotherapy, larger breasts, and/or ptotic breasts | |
| Rosson, USA (64) | Quality of life before reconstructive breast surgery: A preoperative comparison of patients with immediate, delayed, and major revision reconstruction | 2013 | IV | Case Series | Immediate and delayed | 176 patients | Response rate 76% | The three groups differed significantly (P<0.05) across four of the six domains: body image (satisfaction with breasts), psychosocial well-being, sexual well-being, and physical well-being of the chest and upper body. The immediate reconstruction group had higher (better) scores than the delayed reconstruction group, which had higher (better) scores than the major revision group | |
| Rusby, UK (80) | IBR after mastectomy: what are the long-term prospects? | 2010 | IV | Case Series | Immediate | 95 patients (110 breast reconstructions) | Although more intervention was seen in patients with implant-based reconstruction and the time-course over which autologous and implant-based reconstructions fail is different these did not reach statistical significance. Radiotherapy has a significant effect on failure of implant-based reconstruction | ||
| Salhab, UK (13) | Skin-sparing mastectomy and immediate breast reconstruction: patient satisfaction and clinical outcome. | 2006 | IV | Case Series | Immediate | 21 patients (25 breast reconstructions) | 13.5 months | Skin sparing mastectomy and immediate breast reconstruction for operable breast cancer is associated with a high level of patient satisfaction and low morbidity. The procedure seems to be oncologically safe, even in patients with high-risk (T3 or node-positive) carcinoma. The latter needs to be confirmed with greater numbers of patients and longer follow-up | |
| Snell, USA (12) | Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study | 2010 | IV | Case Series | N/A | 28 patients | Implant-based breast reconstruction patients may have inaccurate expectations regarding the results of their surgery despite having received standard preoperative teaching. Specifically, patients often had unclear expectations regarding the appearance and physical outcome of the reconstructed breast(s). Some patients were surprised by the “flatness” of the tissue expander immediately after its insertion. Most patients felt unprepared for the “unnatural” final appearance of the breast(s). This study has important implications for preoperative education of women undergoing implant breast reconstruction. Physicians and nurses involved in the preoperative preparation process should take care to explore patients’ expectations regarding the appearance, feel, sensation, and movement of reconstructed breasts to increase overall postoperative satisfaction | ||
| Yanko-Arzi, Israel (62) | Breast reconstruction: complication rate and tissue expander type | 2009 | IV | Case Series | Immediate and delayed | 140 patients (170 breast reconstructions) | This study compared the incidence of significant complications according type of implant used in breast reconstruction. In reconstructions using anatomic implants a total major complication rate of 41% was found, competed to 20% in round implant use, and 11.7% in Becker implants. We found a significantly higher complication rate with the use of the integrated-valve biodimensional expander than with either the distant port round expander or the Becker expander-implant. Benefits attributed to the integrated valve do not outweigh the complications encountered while using it | ||
| Singh, USA (68) | Cost comparison of immediate one-stage and tissue-expander breast reconstructions after mastectomy in commercially insured patients | 2013 | IV | Cost-Analysis | Immediate | 1,316 breast reconstructions | The data showed a modest, non-significant trend toward fewer return visits after one-stage reconstruction vs. TE reconstruction. Patients with TE reconstructions returned more often for planned returns and planned returns with revisions. Patients with one-stage reconstructions returned more often for unplanned events. The total costs over 18 months were $34,839 and $39,062 for one-stage and TE reconstructions, respectively. The initial reconstruction, including the mastectomy, accounted for 64% of the 18-month costs with one-stage reconstructions and for 54% of the 18-month costs for TE reconstructions. Costs and utilization trended lower over 18 months for one-stage vs. TE reconstructions following post-mastectomy breast reconstructions but did not achieve statistical significance | ||
| Albornoz, USA (4) | A paradigm shift in U.S. Breast reconstruction: increasing implant rates | 2013 | III | Cross-sectional study | The recent significant rise in immediate reconstruction rates in the United States correlates closely to a 203% expansion in implant use. Although the reason for the increase in implant use is multifactorial, changes in mastectomy patterns, such as increased use of bilateral mastectomies, are one important contributor | ||||
| Hershman, USA (8) | Influence of health insurance, hospital factors and physician volume on receipt of immediate post-mastectomy reconstruction in women with invasive and non-invasive breast cancer | 2012 | III | Cross-sectional study | Immediate | 108,992 patients with invasive breast cancer & 14,710 women with DCIS | Increasing age, black race, being married, rural location, and increased comorbidities were associated with decreased rates of immediate breast reconstruction following mastectomy. Immediate in-hospital complication rates were higher for flap reconstruction compared to implant or no reconstruction (15.2%, 4.0%, and 6.1%, respectively, P<0.0001) | ||
| Klit, Denmark (86) | Breast reconstruction with an expander prosthesis following mastectomy does not cause additional persistent pain: a nationwide cross-sectional study | 2013 | III | Cross-sectional study | Immediate | 129 patients | 83% response rate | Breast reconstruction with a sub-pectoral implant after tissue expansion does not confer increased prevalence of persistent pain. We found no increased risk of persistent pain in patients having a reconstruction with an implant compared with mastectomy without reconstruction. There was also no difference between patients treated with immediate or DBR | |
| Alderman, USA (71) | Complications in post-mastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study | 2002 | II | Prospective Analysis | Immediate and delayed | 326 patients | 2 years | (I) Immediate reconstructions were associated with significantly higher complication rates than delayed procedures, and (II) procedure type had no significant effect on complication rates although a trend was noted for higher complication rates in implant patients who received radiotherapy | |
| Behranwala, UK (79) | The influence of radiotherapy on capsule formation and aesthetic outcome after IBR using biodimensional anatomical expander implants | 2006 | II | Prospective Analysis | Immediate | 114 patients (136 breast reconstructions) | 4 years | Radiotherapy is associated with a higher capsule formation rate | |
| Clough, France (65) | Prospective evaluation of late cosmetic results following breast reconstruction: I. Implant reconstruction | 2001 | III | Prospective Analysis | Immediate | 360 breast reconstructions | 4.2 years | Deterioration of the cosmetic appearance of implant breast reconstruction was noted in this study. The overall acceptable cosmetic outcome deteriorated from 86% at 2 years after patients completed their reconstruction to only 54% at 5 years. This deterioration was irrespective of the type of implant used | |
| Cowen, USA (33) | Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications | 2010 | II | Prospective Analysis | Immediate | 141 patients | 37 months | Reconstruction failure was analyzed in this study. Three predictors of immediate post-mastectomy breast reconstruction using tissue expanders and implants were identified. These predictors were smoking, T3 or T4 tumors, and axillary lymph node invasion. Also of note, grade 3 or 4 capsular contracture was related to adjuvant hormone therapy, the surgeon, and smoking | |
| Giacalone, France (69) | New concept for IBR for invasive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy IBR vs. DBR: a prospective pilot study | 2010 | II | Prospective Analysis | Immediate and delayed | 104 patients | 4.5- 4.7 years | IBR is a valuable addition to the oncological surgical armamentarium for primary treatment of breast cancer. Our study shows that the feasibility and oncological safety of immediate are comparable to DBR. Total early complications (<30 days) 61.5% (IBR) vs. 56.4% (DBR). Total late complications 30.7% (IBR) vs. 21.7% (DBR) | |
| Krueger, USA (34) | Complications and patient satisfaction following expander/implant breast reconstruction with and without radiotherapy | 2001 | III | Prospective Analysis | Immediate | 81 patients | Mean 31 months | Reconstructive failure was significantly associated with the use of radiotherapy (P=0.005). The observed reconstruction failure rates were 37% for irradiated patients compared with 8% for non-irradiated patients. Despite these differences, our pilot data suggest that both general satisfaction and patient aesthetic satisfaction were not significantly different. In addition, tamoxifen use was associated with a significantly decreased aesthetic satisfaction (P=0.03) | |
| Patani, UK (43) | Oncological safety and patient satisfaction with skin-sparing mastectomy and IBR | 2008 | II | Prospective Analysis | Immediate | 83 patients (93 breast reconstructions) | 34 months | Skin sparing mastectomy with IBR is associated with low morbidity, high levels of patient satisfaction and is oncologically adequate for T (is), T1 and T2 tumors without extensive skin involvement. There was no LR after a median follow-up of 34 months (range, 3-79 months). Overall survival was 98.8%. Significant capsule formation, requiring capsulotomy, was observed in 87% of patients who had radiotherapy compared with 13% for those who did not have radiotherapy | |
| Albornoz, USA (5) | Diminishing relative contraindications for immediate breast reconstruction: a multicenter study | 2014 | III | Retrospective Analysis | Breast reconstruction with implant. There was a greater rate increase in implant than autologous reconstructions for both high-risk and low-risk groups. Breast reconstruction increased in high-risk surgical and oncologic patients, suggestive of a diminishing set of relative contraindications. Increased implant use in high-risk patients might be a contributing factor toward the preferential national expansion of prosthetic techniques | ||||
| Albornoz, USA (85) | Implant breast reconstruction and radiation: a multicenter analysis of long-term health-related quality of life and satisfaction | 2014 | III | Retrospective Analysis | 3.3 years | Radiotherapy has a negative effect on quality of life and satisfaction with breasts in patients with implant reconstruction compared with non-irradiated patients | |||
| Brown, Canada (53) | Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery | 2005 | III | Retrospective Analysis | Immediate | 32 patients (50 breast reconstructions) | Results in our initial 150 patients have been excellent, with a high degree of patient satisfaction, excellent aesthetic outcomes, and very few implant-related complications. Cohesive gel implants are likely to play an important role in aesthetic and reconstructive breast surgery | ||
| Chang, USA (83) | Effects of an autologous flap combined with an implant for breast reconstruction: an evaluation of 1000 consecutive reconstructions of previously irradiated breasts | 2008 | III | Retrospective Analysis | Immediate and delayed | 706 patient (1,000 breast reconstructions) | 22.2 months | The use of preoperative or postoperative radiation therapy to the reconstructed breast significantly increased the incidence of most implant-associated complications compared with no radiation therapy. An autologous flap, when combined with an implant for breast reconstruction, appears to reduce the incidence of implant-related complications in previously irradiated breasts | |
| Chang, Australia (18) | Experience in dermomyofascial pouch coverage of immediate implants following skin sparing reduction mastectomy | 2013 | III | Retrospective Analysis | Immediate | 6 patients (11 breast reconstructions) | 5-19 months | In our initial experience, SSRM is a safe and effective method of immediate implant-based breast reconstruction | |
| Chew, UK (60) | Becker expander implants: truly a long term single stage reconstruction? | 2010 | III | Retrospective Analysis | Immediate | 68 breast reconstructions | 12.5 years | The use of Becker expanders may be hard to justify in post-mastectomy reconstruction if most patients go on to require removal and replacement of the expander. Reported rates in this study are as high as 94% removal at 10 years | |
| Cordeiro, USA (36) | A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part II. An analysis of long-term complications, aesthetic outcomes, and patient satisfaction | 2006 | III | Retrospective Analysis | Immediate and delayed | 315 patients (410 breast reconstructions) | 36.7 months | Tissue expander/implant reconstruction yields well to excellent long-term aesthetic results in the majority of patients. In this study 95% of patients were satisfied with their reconstruction and 88% had a good to excellent aesthetic result. Bilateral reconstructions have higher overall aesthetic grades. Radiation history was a significant predictor of overall cosmesis; however acceptable results are attainable in irradiated patients | |
| Cordeiro, USA (76) | Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients | 2004 | III | Retrospective Analysis | Immediate | 687 patients | The overall success rate for implant reconstruction in irradiated patients was 90% compared to 99% in non-irradiated patients (P<0.000). Of the irradiated patients 80% were noted to have well to excellent aesthetic results, compared to 88% in the non-irradiated group. For the many women who are not candidates for autologous tissue reconstruction or who do not wish to undergo more involved flap surgical procedures, immediate tissue expander/implant reconstruction can be safely recommended even when postoperative irradiation is planned | ||
| Davila, USA (21) | Immediate two-stage tissue expander breast reconstruction compared with one-stage permanent implant breast reconstruction: a multi-institutional comparison of short-term complications | 2013 | III | Retrospective Analysis | Immediate | 10,561 patients | 30 days | Immediate one-stage, direct-to-implant, and two-stage tissue expander reconstructions result in low rates of morbidity. One-stage reconstruction suggests a slightly higher complication rate related to prosthesis failure | |
| Handel, USA (58) | A long-term study of outcomes, complications, and patient satisfaction with breast implants | 2006 | II | Retrospective Analysis | N/A | 264 patients (352 breast implant reconstructions) | 37.4 months | Breast implants are associated with a significant rate of local complications and reoperation. There are marked differences in outcomes as a function of implant surface type and surgical indication. Despite relatively frequent complications and reoperations, implant recipients are largely satisfied. Smooth and textured implants had similar contracture rates; polyurethane foam-covered implants had a reduced risk of contracture persisting for at least 10 years after implantation | |
| Hardwicke, UK (51) | A retrospective audit of Novagold ‘hydrogel’ breast implants | 2007 | III | Retrospective Analysis | N/A | 250 patients | Of the 250 patients who underwent implantation of these implants 44% of cases needed further surgery for complications. Capsular contracture requiring surgical intervention occurred in 32%. Symptomatic ruptures occurred in 10.5%. From comparison with published data, the incidence of capsular contracture is comparable, but the occurrence of rupture is almost twice that of saline-filled implants. The results of this study show that this composition of implant poses potential risks, which should be considered by manufacturers in the future. We advise removal of symptomatic implants, as rupture is likely to have occurred | ||
| Jónsdóttir, Iceland (90) | Results of immediate breast reconstructions at Landspitali-The National University Hospital of Iceland, in 2008-2010 | 2012 | III | Retrospective Analysis | Immediate and delayed | 157 breast reconstructions | As a result of the establishment of an oncoplastic breast surgical service at Landspítali, the rates of immediate breast reconstruction have increased significantly (from 5% to 31%). The rates of autologous flap reconstructions were significantly higher than in this study (63% vs. 26%) | ||
| Kim, Korea (16) | Short-term outcomes of IBR using an implant or tissue expander after mastectomy in breast cancer patients | 2014 | III | Retrospective Analysis | Immediate | 63 patients | 22.4 months | 63 patients had immediate reconstruction with expanders or implants. Major complications included nipple areolar complex (NAC) necrosis and implant removal in 11.1% of the patients. 3 patients had their implant removed due to severe infection, leakage and dissatisfaction. 84.1% of patients were satisfied with the overall result and 77.8% were satisfied with the cosmesis of their reconstructions | |
| Lentz, USA (74) | Radiation therapy and expander-implant breast reconstruction: an analysis of timing and comparison of complications | 2013 | III | Retrospective Analysis | Immediate | 55 patients (56 breast reconstructions) | 27.3 months | No significance was found in overall complication rates or reconstruction failure rate between cohorts of patients who had exchange prior to radiotherapy compared to after radiotherapy. Nor was a significance found between early exchanges in comparison to late exchange following radiotherapy. Trends suggest a higher rate of infection in patients who underwent exchange earlier (30% vs. 14.29%, P=0.422) and a higher rate of capsular contracture in patients who underwent exchange later (5% vs. 21.43%, P=0.283); however, statistical significance was not reached. Our findings suggest that neither the sequencing nor timing of expander-implant exchange in the setting of post-mastectomy radiotherapy (PMRT) affects overall complication or reconstruction failure rate. However, the timing of exchange may impact the type of complication encountered | |
| Losken, USA (81) | Factors that influence the completion of breast reconstruction | 2004 | III | Retrospective Analysis | Immediate and delayed | 888 patients (1038 breast reconstructions) | Delayed reconstructions had a higher number of secondary procedures compared to immediate reconstructions. TRAM flap reconstructions tended to have more secondary procedures than implant or latissimus dorsa reconstructions. Radiation therapy is also associated with an increased number of secondary procedures. Autologous tissue reconstructions in general required more secondary procedures-hypothesized in this study to be partly due to donor site revisions | ||
| Macadam, Canada (47) | Patient satisfaction and health-related quality of life following breast reconstruction: patient-reported outcomes among saline and silicone implant recipients | 2010 | III | Retrospective Analysis | N/A | 143 breast reconstructions | 58% response rate | This study has shown higher satisfaction with breast reconstruction in silicone gel implant recipients compared with saline recipients using the BREAST-Q. There was no difference in overall global health status between the 2 patient groups. Silicone recipients had higher overall physical function, and saline recipients had higher systemic side effects | |
| Macadam, Canada (52) | Patient-reported satisfaction and health-related quality of life following breast reconstruction: a comparison of shaped cohesive gel and round cohesive gel implant recipients | 2013 | III | Retrospective Analysis | N/A | 128 patients | 75% response rate | There was no difference appreciable between round and shaped implants on any scale including overall satisfaction with breast and outcome. Shaped implants were significantly firmer than round. There was no difference in rippling of the implant between the 2 types | |
| McCarthy, USA (48) | Patient satisfaction with postmastectomy breast reconstruction: a comparison of saline and silicone implants | 2010 | III | Retrospective Analysis | N/A | 482 patients | 72% response rate | Patients’ satisfaction with their breasts was significantly higher in patients with silicone implants (P=0.016) compared to saline implants. The receipt of post-mastectomy radiotherapy was found to have a significant, negative effect on breast satisfaction (P<0.000) in both silicone and saline implant recipients. In addition, for women who received either silicone or saline implants, satisfaction diminished over time (P=0.017) |
|
| Parsa, USA (78) | Selection criteria for expander/implant breast reconstruction following radiation therapy | 2009 | III | Retrospective Analysis | Delayed | 27 patients | Irradiated chest walls with moderate skin changes and absent induration have aesthetic outcomes comparable to the non-irradiated chest walls (P>0.50). In contrast, patients who develop induration or severe post-radiation skin changes have a greater rate of modified Baker class IV capsular contracture and poor results that range from 75% to 100% of reconstructed breasts. A history of chest wall radiation should not itself exclude patients from receiving expander/implant reconstruction. Patients who develop neither severe skin changes nor induration may still be considered for prostheses | ||
| Pinsolle, France (41) | Complications analysis of 266 IBRs | 2006 | III | Retrospective Analysis | Immediate | 249 patients (266 breast reconstructions) | 7 years | The complication rate for IBR with implant alone (39%) was lower than that associated with latissimus dorsi with or without implant (51%), but the difference was not significant. The risk factors for complications were smoking (skin necrosis), obesity (infection), and radiotherapy. Capsular contractures were more frequent when implants were used alone (25%) as well as when used along with a flap (6.8%). In our opinion, latissimus dorsa myocutaneous flap with or without an implant is a good compromise between complication risk and necessity of good cosmetic result requirement. These results have led us to delay or contraindicate reconstruction in the case of obesity or heavy smoking. In the case of probable post-operative radiotherapy, we prefer to delay the breast reconstruction. | |
| Roostaeian, USA (17) | Comparison of immediate implant placement versus the staged tissue expander technique in breast reconstruction | 2012 | III | Retrospective Analysis | Immediate | 35 patients (62 breast reconstructions) | 14 months | The overall complication rates of immediate implant-based reconstructions and immediate tissue expander reconstructions were similar, and the need for revision surgery was also similar. Mean final implant volume did not differ between the two groups. However, mean number of office visits/time to nipple reconstruction was significantly reduced (P<0.001) in the implant group. Aesthetic evaluation revealed no significant differences. In the appropriately selected patient, it is a safe option that provides similar outcomes in less time compared with staged expander-based reconstruction | |
| Singh, USA (38) | Immediate 1-stage vs. tissue expander post-mastectomy implant breast reconstructions: a retrospective real-world comparison over 18 months | 2012 | III | Retrospective Analysis | Immediate | 1,316 breast reconstructions | Overall survival in this study was 100%. The incidence of flap necrosis/loss, implant loss, wound infection, or hematoma requiring surgical evacuation was 0%, 0%, 0%, and 0%, respectively. Capsule formation requiring capsulotomy was observed in 3 of 21 patients (14%). The median patient satisfaction score was 10 (range, 6-10). The results show that surgeons in the United States achieved substantially similar results in immediate post-mastectomy implant breast reconstructions with 1-stage and TE approaches in terms of patient complications and returns for reconstruction-related services over 18 months. As evolving mastectomy techniques make 1-stage implant reconstructions more attractive, we hope these findings will motivate researchers to compare the approaches in more strictly controlled clinical studies | ||
| Spear, USA (50) | Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications | 2000 | III | Retrospective Analysis | Immediate and delayed | 40 patients | Using a scoring system for judging cosmetic results of breast reconstructions 40 patients were reviewed by a panel. Cosmesis was given a score by the judges between 1.4 and 4.0. Those patients who had undergone radiation therapy during expansion scored from 1.4 to 3.85 (mean, 2.925). Those radiated after reconstruction ranged from 1.75 to 4.0 (mean, 3.25). The control group was scored between 2.125 and 3.875 (mean, 3.28). The increasing use of radiation after mastectomy has important implications for breast reconstruction. The possibility for radiation should be thoroughly investigated and anticipated preoperatively before IBR. Patients with invasive disease, particularly with large tumors or palpable axillary lymph nodes, are especially likely to be encouraged to undergo post-mastectomy radiation therapy | ||
| Sullivan, USA (39) | True incidence of all complications following immediate and DBR | 2008 | III | Retrospective Analysis | Immediate and delayed | 240 patients (334 breast reconstructions) | Autologous reconstruction can be performed immediately or delayed, with optimal aesthetic outcome and low flap loss risk. However, the overall complication rate and capsular contracture incidence following immediate tissue expander/implant reconstruction was much higher than when performed delayed. Capsular contracture was a significantly more common late complication following immediate (40.4%) vs. delayed (17.0%) reconstruction (P<0.001). Thus, tissue expander placement at the time of mastectomy may not necessarily save the patient an extra operation and may compromise the final aesthetic outcome | ||
| Wong, USA (82) | Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy | 2008 | III | Retrospective Analysis | Immediate | 62 patients | 10-13 months | Major corrective surgery was undertaken by 16% of total patients studied following radiotherapy. This incorporated 9% of non-implant based reconstructions compared to 40% of implant based reconstructions. Patients who undergo immediate reconstruction after mastectomy using an implant followed by radiation have a high rate of subsequent major corrective surgery. The difference between the implant and non-implant groups is significant in early follow-up. Patients considering implant reconstruction followed by radiotherapy should be made aware of this risk |
. IBR, Immediate breast reconstruction; DBR, delayed breast reconstruction; LR, local recurrence; TRAM, transverse rectus abdominis musculocutaneous; ADM, acellular dermal matrix; DCIS, ductal carcinoma in situ; SSRM, skin sparing reduction mastectomy.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Australian Institute of Health and Welfare (AIHW) 2015. Australian Cancer Incidence and Mortality (ACIM) books. Available online: http://www.aihw.gov.au/acim-books
- 2.DellaCroce FJ, Wolfe ET. Breast reconstruction. Surg Clin North Am 2013;93:445-54. [DOI] [PubMed] [Google Scholar]
- 3.Asplund O, Körlof B. Late results following mastectomy for cancer and breast reconstruction. Scand J Plast Reconstr Surg 1984;18:221-5. [DOI] [PubMed] [Google Scholar]
- 4.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131:15-23. [DOI] [PubMed] [Google Scholar]
- 5.Albornoz CR, Cordeiro PG, Pusic AL, et al. Diminishing relative contraindications for immediate breast reconstruction: a multicenter study. J Am Coll Surg 2014;219:788-95. [DOI] [PubMed] [Google Scholar]
- 6.Radovan C. Breast reconstruction after mastectomy using the temporary expander. Plast Reconstr Surg 1982;69:195-208. [DOI] [PubMed] [Google Scholar]
- 7.Elliott LF, Hartrampf CR, Jr. Breast reconstruction: progress in the past decade. World J Surg 1990;14:763-75. [DOI] [PubMed] [Google Scholar]
- 8.Hershman DL, Richards CA, Kalinsky K, et al. Influence of health insurance, hospital factors and physician volume on receipt of immediate post-mastectomy reconstruction in women with invasive and non-invasive breast cancer. Breast Cancer Res Treat 2012;136:535-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reaby LL. Reasons why women who have mastectomy decide to have or not to have breast recon-struction. Plast Reconstr Surg 1998;101:1810-8. [DOI] [PubMed] [Google Scholar]
- 10.Ng SK, Hare RM, Kuang RJ, et al. Breast reconstruction post mastectomy: patient satisfaction and decision making. Ann Plast Surg 2014. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 11.Walton L, Ommen K, Audisio RA. Breast reconstruction in elderly women breast cancer: a review. Cancer Treat Rev 2011;37:353-7. [DOI] [PubMed] [Google Scholar]
- 12.Snell L, McCarthy C, Klassen A, et al. Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study. Plast Reconstr Surg 2010;126:1825-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salhab M, Al Sarakbi W, Joseph A, et al. Skin-sparing mastectomy and immediate breast reconstruction: patient satisfaction and clinical outcome. Int J Clin Oncol 2006;11:51-4. [DOI] [PubMed] [Google Scholar]
- 14.Kronowitz SJ, Kuerer HM. Advances and surgical decision-making for breast reconstruction. Cancer 2006;107:893-907. [DOI] [PubMed] [Google Scholar]
- 15.Racano C, Fania PL, Motta GB, et al. Immediate and delayed two-stage post-mastectomy breast recon-struction with implants. Our experience of general surgeons. Minerva Chir 2002;57:135-49. [PubMed] [Google Scholar]
- 16.Kim SW, Lee HK, Kang SM, et al. Short-term outcomes of immediate breast reconstruction using an implant or tissue expander after mastectomy in breast cancer patients. Breast Cancer 2014. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 17.Roostaeian J, Sanchez I, Vardanian A, et al. Comparison of immediate implant placement versus the staged tissue expander technique in breast reconstruction, Plast Reconstr Surg 2012;129:909e-18e. [DOI] [PubMed] [Google Scholar]
- 18.Chang LY, Hargreaves W, Segara D, et al. Experience in dermomyofascial pouch coverage of imme-diate implants following skin sparing reduction mastectomy. ANZ J Surg 2013;83:135-8. [DOI] [PubMed] [Google Scholar]
- 19.Robertson S, Wengström Y, Eriksen C, et al. Breast surgeons performing immediate breast reconstruc-tion with implants - assessment of resource-use and patient-reported outcome measures. Breast 2012;21:590-6. [DOI] [PubMed] [Google Scholar]
- 20.Gibney J. Use of a permanent tissue expander for breast reconstruction. Plast Reconstr Surg 1989;84:607-17; discussion 618-20. [PubMed] [Google Scholar]
- 21.Davila AA, Mioton LM, Chow G, et al. Immediate two-stage tissue expander breast reconstruction compared with one-stage permanent implant breast reconstruction: a multi-institutional comparison of short-term complications. J Plast Surg Hand Surg 2013;47:344-9. [DOI] [PubMed] [Google Scholar]
- 22.Roostaeian J, Pavone L, Da Lio A, et al. Immediate placement of implants in breast reconstruction: patients selection and outcomes. Plast Reconstr Surg 2011;127:1407-16 [DOI] [PubMed] [Google Scholar]
- 23.Spear SL, Spittler CJ, et al. Breast reconstruction with implants and expanders. Plast Reconstr Surg 2001;107:177-87; quiz 188. [DOI] [PubMed] [Google Scholar]
- 24.Hodgson EL, Malata CM. Implant-based breast reconstruction following mastectomy. Breast Dis 2002;16:47-63. [DOI] [PubMed] [Google Scholar]
- 25.Argenta LC. Controlled tissue expansion in reconstructive surgery. Br J Plast Surg 1984;37:520-9. [DOI] [PubMed] [Google Scholar]
- 26.Kronowitz SJ. State of the art and science in postmastectomy breast reconstruction. Plast Reconstr Surg 2015;135:755e-71e. [DOI] [PubMed] [Google Scholar]
- 27.August DA, Wilkins E, Rea T. Breast reconstruction in older women. Surgery 1994;115:663-8. [PubMed] [Google Scholar]
- 28.Gabriel SE, Woods JE, O'Fallon WM, et al. Complications leading to surgery after breast implantation. N Engl J Med 1997;336:677-82. [DOI] [PubMed] [Google Scholar]
- 29.Tsoi B, Ziolkowski NI, Thoma A, et al. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg 2014;133:234-49. [DOI] [PubMed] [Google Scholar]
- 30.Davies K, Allan L, Roblin P, et al. Factors affecting post-operative complications following skin spar-ing mastectomy with immediate breast reconstruction. Breast 2011;20:21-5. [DOI] [PubMed] [Google Scholar]
- 31.Bailey MH, Smith JW, Casas L, et al. Immediate breast reconstruction: reducing the risks. Plast Reconstr Surg 1989;83:845-51. [DOI] [PubMed] [Google Scholar]
- 32.Miller AP, Falcone RE. Breast reconstruction: systemic factors influencing local complications. Ann Plast Surg 1991;27:115-20. [DOI] [PubMed] [Google Scholar]
- 33.Cowen D, Gross E, Rouannet P, et al. Immediate post-mastectomy breast reconstruction followed by radiotherapy: risk factors for complications. Breast Cancer Res Treat 2010;121:627-34. [DOI] [PubMed] [Google Scholar]
- 34.Krueger EA, Wilkins EG, Strawderman M, et al. Complications and patient satisfaction following ex-pander/implant breast reconstruction with and without radiotherapy. Int J Radiat Oncol Biol Phys 2001;49:713-21. [DOI] [PubMed] [Google Scholar]
- 35.Embrey M, Adams EE, Cunningham B, et al. A review of the literature on the etiology of capsular contracture and a pilot study to determine the outcome of capsular contracture interventions. Aesthetic Plast Surg 1999;23:197-206. [DOI] [PubMed] [Google Scholar]
- 36.Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part II. An analysis of long-term complications, aesthetic outcomes, and patient satis-faction. Plast Reconstr Surg 2006;118:832-9. [DOI] [PubMed] [Google Scholar]
- 37.Holmes JD. Capsular contracture after breast reconstruction with tissue expansion. Br J Plast Surg 1989;42:591-4. [DOI] [PubMed] [Google Scholar]
- 38.Singh N, Reaven NL, Funk SE. Immediate 1-stage vs. tissue expander postmastectomy implant breast reconstructions: a retrospective real-world comparison over 18 months. J Plast Reconstr Aesthet Surg 2012;65:917-23. [DOI] [PubMed] [Google Scholar]
- 39.Sullivan SR, Fletcher DR, Isom CD, et al. True incidence of all complications following immediate and delayed breast reconstruction. Plast Reconstr Surg 2008;122:19-28. [DOI] [PubMed] [Google Scholar]
- 40.Collis N, Coleman D, Foo IT, et al. Ten-year review of a prospective randomized controlled trial of textured versus smooth subglandular silicone gel breast implants. Plast Reconstr Surg 2000;106:786-91. [DOI] [PubMed] [Google Scholar]
- 41.Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, et al. Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg 2006;59:1017-24. [DOI] [PubMed] [Google Scholar]
- 42.Virden CP, Dobke MK, Stein P, et al. Subclinical infection of the silicone breast implant surface as a possible cause of capsular contracture. Aesthetic Plast Surg 1992;16:173-9. [DOI] [PubMed] [Google Scholar]
- 43.Patani N, Devalia H, Anderson A, et al. Oncological safety and patient satisfaction with skin-sparing mastectomy and immediate breast reconstruction. Surg Oncol 2008;17:97-105. [DOI] [PubMed] [Google Scholar]
- 44.Ringberg A, Tengrup I, Aspegren K, et al. Immediate breast reconstruction after mastectomy for can-cer. Eur J Surg Oncol 1999;25:470-6. [DOI] [PubMed] [Google Scholar]
- 45.Rheingold LM, Yoo RP, Courtiss EH. Experience with 326 inflatable breast implants. Plast Reconstr Surg 1994;93:118-22. [DOI] [PubMed] [Google Scholar]
- 46.Gylbert L, Asplund O, Jurell G. Capsular contracture after breast reconstruction with silicone-gel and saline-filled implants: a 6-year follow-up. Plast Reconstr Surg 1990;85:373-7. [DOI] [PubMed] [Google Scholar]
- 47.Macadam SA, Ho AL, Cook EF, Jr, et al. Patient satisfaction and health-related quality of life follow-ing breast reconstruction: patient-reported outcomes among saline and silicone implant recipients. Plast Reconstr Surg 2010;125:761-71. [DOI] [PubMed] [Google Scholar]
- 48.McCarthy CM, Klassen AF, Cano SJ, et al. Patient satisfaction with post-mastectomy breast recon-struction: a comparison of saline and silicone implants. Cancer 2010;116:5584-91. [DOI] [PubMed] [Google Scholar]
- 49.Schusterman MA, Kroll SS, Reece GP, et al. Incidence of autoimmune disease in patients after breast reconstruction with silicone gel implants versus autogenous tissue: a preliminary report. Ann Plast Surg 1993;31:1-6. [PubMed] [Google Scholar]
- 50.Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg 2000;105:930-42. [DOI] [PubMed] [Google Scholar]
- 51.Hardwicke J, Gaze NR, Laitung JK. A retrospective audit of Novagold “hydrogel” breast implants. J Plast Reconstr Aesthet Surg 2007;60:1313-6. [DOI] [PubMed] [Google Scholar]
- 52.Macadam SA, Ho AL, Lennox PA, et al. Patient-reported satisfaction and health-related quality of life following breast reconstruction: a comparison of shaped cohesive gel and round cohesive gel implant recip-ients. Plast Reconstr Surg 2013;131:431-41. [DOI] [PubMed] [Google Scholar]
- 53.Brown MH, Shenker R, Silver SA. Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery. Plast Reconstr Surg 2005;116:768-79; discussion 780-1. [DOI] [PubMed] [Google Scholar]
- 54.Nahabedian MY. Shaped versus round implants for breast reconstruction: indications and outcomes. Plast Reconstr Surg Glob Open 2014;2:e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu X, Zhou L, Pan F, et al. Comparison of the postoperative incidence rate of capsular contracture among different breast implants: a cumulative meta-analysis. PLoS One 2015;10:e0116071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shapiro MA. Smooth vs. rough: an 8-year survey of mammary prostheses. Plast Reconstr Surg 1989;84:449-57. [PubMed] [Google Scholar]
- 57.Hakelius L, Ohlsén L. A clinical comparison of the tendency to capsular contracture between smooth and textured gel-filled silicone mammary implants. Plast Reconstr Surg 1992;90:247-54. [PubMed] [Google Scholar]
- 58.Handel N, Cordray T, Gutierrez J, et al. A long-term study of outcomes, complications, and patient satisfaction with breast implants. Plast Reconstr Surg 2006;117:757-67; discussion 768-72. [DOI] [PubMed] [Google Scholar]
- 59.Maxwell GP, Falcone PA. Eighty-four consecutive breast reconstructions using a textured silicone tis-sue expander. Plast Reconstr Surg 1992;89:1022-34; discussion 1035-6. [PubMed] [Google Scholar]
- 60.Chew BK, Yip C, Malyon AD, et al. Becker expander implants: truly a long term single stage recon-struction? J Plast Reconstr Aesthet Surg 2010;63:1300-4. [DOI] [PubMed] [Google Scholar]
- 61.Spear SL, Majidian A. Immediate breast reconstruction in two stages using textured, integrated-valve tissue expanders and breast implants: a retrospective review of 171 consecutive breast reconstructions from 1989 to 1996. Plast Reconstr Surg 1998;101:53-63. [DOI] [PubMed] [Google Scholar]
- 62.Yanko-Arzi R, Cohen MJ, Braunstein R, et al. Breast reconstruction: complication rate and tissue ex-pander type. Aesthetic Plast Surg 2009;33:489-96. [DOI] [PubMed] [Google Scholar]
- 63.Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plast Reconstr Surg 2004;113:1617-28. [DOI] [PubMed] [Google Scholar]
- 64.Rosson GD, Shridharani SM, Magarakis M, et al. Quality of life before reconstructive breast surgery: A preoperative comparison of patients with immediate, delayed, and major revision reconstruction. Microsurgery 2013;33:253-8. [DOI] [PubMed] [Google Scholar]
- 65.Clough KB, O'Donoghue JM, Fitoussi AD, et al. Prospective evaluation of late cosmetic results fol-lowing breast reconstruction: I. Implant reconstruction. Plast Reconstr Surg 2001;107:1702-9. [DOI] [PubMed] [Google Scholar]
- 66.Radovanovic Z, Radovanovic D, Golubovic A, et al. Early complications after nipple-sparing mastec-tomy and immediate breast reconstruction with silicone prosthesis: results of 214 procedures. Scand J Surg 2010;99:115-8. [DOI] [PubMed] [Google Scholar]
- 67.Francel TJ, Ryan JJ, Manson PN. Breast reconstruction utilizing implants: a local experience and comparison of three techniques. Plast Reconstr Surg 1993;92:786-94. [PubMed] [Google Scholar]
- 68.Singh NK, Reaven NL, Funk SE. Cost comparison of immediate one-stage and tissue-expander breast reconstructions after mastectomy in commercially insured patients. Manag Care 2013;22:36-43. [PubMed] [Google Scholar]
- 69.Giacalone PL, Rathat G, Daures JP, et al. New concept for immediate breast reconstruction for inva-sive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat 2010;122:439-51. [DOI] [PubMed] [Google Scholar]
- 70.Fodor J, Gulyás G, Polgár C, et al. Radiotherapy and breast reconstruction: the issue of compatibility. Orv Hetil 2003;144:549-55. [PubMed] [Google Scholar]
- 71.Alderman AK, Wilkins EG, Kim HM, et al. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 2002;109:2265-74. [DOI] [PubMed] [Google Scholar]
- 72.Chen SA, Hiley C, Nickleach D, et al. Breast reconstruction and post-mastectomy radiation practice. Radiat Oncol 2013;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kuske RR, Schuster R, Klein E, et al. Radiotherapy and breast reconstruction: clinical results and do-simetry. Int J Radiat Oncol Biol Phys 1991;21:339-46. [DOI] [PubMed] [Google Scholar]
- 74.Lentz R, Ng R, Higgins SA, et al. Radiation therapy and expander-implant breast reconstruction: an analysis of timing and comparison of complications. Ann Plast Surg 2013;71:269-73. [DOI] [PubMed] [Google Scholar]
- 75.Fodor J, Gulyás G, Polgár C, et al. Radiotherapy and delayed breast reconstruction with implant: ex-amination of compatibility. Magy Onkol 2002;46:323-6. [PubMed] [Google Scholar]
- 76.Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast re-construction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 2004;113:877-81. [DOI] [PubMed] [Google Scholar]
- 77.Rosato RM, Dowden RV. Radiation therapy as a cause of capsular contracture. Ann Plast Surg 1994;32:342-5. [DOI] [PubMed] [Google Scholar]
- 78.Parsa AA, Jackowe DJ, Johnson EW, et al. Selection criteria for expander/implant breast reconstruction following radiation therapy. Hawaii Med J 2009;68:66-8. [PubMed] [Google Scholar]
- 79.Behranwala KA, Dua RS, Ross GM, et al. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg 2006;59:1043-51. [DOI] [PubMed] [Google Scholar]
- 80.Rusby JE, Waters RA, Nightingale PG, et al. Immediate breast reconstruction after mastectomy: what are the long-term prospects? Ann R Coll Surg Engl 2010;92:193-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Losken A, Carlson GW, Schoemann MB, et al. Factors that influence the completion of breast recon-struction. Ann Plast Surg 2004;52:258-61; discussion 262. [DOI] [PubMed] [Google Scholar]
- 82.Wong JS, Ho AY, Kaelin CM, et al. Incidence of major corrective surgery after post-mastectomy breast reconstruction and radiation therapy. Breast J 2008;14:49-54. [DOI] [PubMed] [Google Scholar]
- 83.Chang DW, Barnea Y, Robb GL. Effects of an autologous flap combined with an implant for breast reconstruction: an evaluation of 1000 consecutive reconstructions of previously irradiated breasts. Plast Reconstr Surg 2008;122:356-62. [DOI] [PubMed] [Google Scholar]
- 84.Jugenburg M, Disa JJ, Pusic AL, et al. Impact of radiotherapy on breast reconstruction. Clin Plast Surg 2007;34:29-37; abstract v-vi. [DOI] [PubMed] [Google Scholar]
- 85.Albornoz CR, Matros E, McCarthy CM, et al. Implant breast reconstruction and radiation: a multicen-ter analysis of long-term health-related quality of life and satisfaction. Ann Surg Oncol 2014;21:2159-64. [DOI] [PubMed] [Google Scholar]
- 86.Klit A, Mejdahl MK, Gärtner R, et al. Breast reconstruction with an expander prosthesis following mastectomy does not cause additional persistent pain: a nationwide cross-sectional study. J Plast Reconstr Aesthet Surg 2013;66:1652-8. [DOI] [PubMed] [Google Scholar]
- 87.Corsten LA, Suduikis SV, Donegan WL. Patient satisfaction with breast reconstruction. Wis Med J 1992;91:125-6, 129. [PubMed] [Google Scholar]
- 88.Baker RR. The management of breast cancer with immediate or delayed reconstruction. Adv Surg 1992;25:51-64. [PubMed] [Google Scholar]
- 89.Jahkola T, Asko-Seljavaara S, von Smitten K. Immediate breast reconstruction. Scand J Surg 2003;92:249-56 [DOI] [PubMed] [Google Scholar]
- 90.Jónsdóttir K, Rafnsdóttir SL, Kjartansdottir T, et al. Results of immediate breast reconstructions at Landspítali-The National University Hospital of Iceland, in 2008-2010. Laeknabladid 2012;98:459-63. [DOI] [PubMed] [Google Scholar]