Abstract
Background
Fracture-risk assessment tool (FRAX) using just clinical risk factors of osteoporosis has been developed to estimate individual risk of osteoporotic fractures. We developed prediction model of fracture risk using bone mineral density (BMD) as well as clinical risk factors in Korean, and assessed the validity of the final model.
Methods
To develop and validate an osteoporotic FRAX, a total of 768 Korean men and women aged 50 to 90 years were followed for 7 years in a community-based cohort study. BMD as well as clinical risk factors for osteoporotic fracture including age, sex, body mass index, history of fragility fracture, family history of fracture, smoking status, alcohol intake, use of oral glucocorticoid, rheumatoid arthritis, and other causes of secondary osteoporosis were assessed biannually.
Results
During the follow-up period, 86 osteoporotic fractures identified (36 in men and 50 in women). The developed prediction models showed high discriminatory power and had goodness of fit.
Conclusions
The developed a Korean specific prediction model for osteoporotic fractures can be easily used as a screening tool to identify individual with high risk of osteoporotic fracture. Further studies for validation are required to confirm the clinical feasibility in general Korean population.
Keywords: Bone density, Korea, Osteoporotic fractures, Risk assessment
INTRODUCTION
Osteoporosis is characterized as skeletal condition with low bone mass, microarchitectural deterioration of bone, and reduced bone strength.[1] Osteoporosis increases the risk of fragile osteoporotic fractures. Osteoporotic fractures have become a major health and economic burden worldwide, because it is associated with high morbidity and mortality.[2,3,4] In Korea, 12.3% of women aged 50 years experience a hip fracture in their life. In addition, 59.5% have osteoporotic fractures during their lifetime.[5] The socioeconomic burden of osteoporotic fractures will increase dramatically in the future, because the elderly population will increase in Korea.[3] Therefore, early detection of individuals with high risk of fracture would be helpful to reduce burden caused by osteoporotic fractures.
Low bone mineral density (BMD) is a strong predictor of osteoporotic fracture risk,[6] and dual energy X-ray absorptiometry (DXA; Lunar Prodigy, GE Medical Systems, Madison, WI, USA) is the most widely accepted method to diagnose osteoporosis. However, DXA has been limited to use for postmenopausal women aged 65 years or older, and younger adults with known risk factors.[7] DXA is not recommended as a routine screening test for the general population. Several fracture-risk assessment tools (FRAXs) have been developed from some clinical variables. However, most of tools have been developed for the Western population.[8,9,10,11] The risk and incidence of osteoporotic fractures varies widely between populations.[12] Thus, population-specific data are required to predict the risk of fracture in each population. However, few studies have developed assessment model from the clinical risk factors of osteoporotic fractures in Korean population.
Our purpose was to develop and validate an osteoporotic FRAX to identify high-risk Korean, based on community-based cohort dataset.
METHODS
1. Study population
The study population consisted of 363 men and 405 women from a prospective community-based cohort (Ansung cohort).
The Ansung cohort was established for Korean Health and Genome Study (KHGS) in 2001 to investigate the prevalence and determinants of chronic diseases in Korea. The Ansung cohort participants include rural residents, and the farming community of Ansung had a population of 123,906 in 2000.[13] Details of this cohort have been previously described.[14] Eligibility criteria of the Ansung cohort were residents of 5 randomly selected governing rural regions (Myons) (7,192 subjects) from a total of 11 (123,906 subjects), age between 40 and 69 at year 2001 and available to participate clinical examinations. Total of 5,018 subjects (2,240 men and 2,778 women) were surveyed among 7,192 eligible subjects (response rate 70%), and followed up for clinical examination, anthropometric measurements, blood sampling and a questionnaire biennially. Among these 5,018 subjects of Ansung cohort, 1,547 male and 1,991 female underwent BMD measurements during 2006 to 2007. Among them, 768 subjects (363 men and 405 women), who did not have a history of anti-osteoporotic drug, were included in this study.
Information on potentially significant risk factors for osteoporotic fractures was obtained from self-administered questionnaires. The questionnaire included asked about age, history of fracture, family history of osteoporotic fracture, smoking status, alcohol consumption, use of oral glucocorticoid, rheumatoid arthritis, and secondary osteoporosis. A positive history of fracture was defined as any type of fracture of and at any age. A positive family history of osteoporotic fracture was defined as a history of physician diagnosed osteoporotic fracture in the first-degree relatives. Smoking status was evaluated by using daily amount of cigarettes. Total alcohol intake was measured by the number of glasses of "Soju" consumed. One glass of Soju contains about one unit of ethanol. In this study, three or more units of alcohol intake were considered high alcohol intake. Use of an oral glucocorticoid was defined if prescribed >30 days in the 1 year. All data were collected by trained staff using standardized questionnaire and the face-to-face interview method.
2. Measurements of anthropometric parameters and BMD
Height and body weight were measured with subjects wearing light clothes. The BMD (g/cm2) measurements of central skeletal sites (lumbar spine, femoral neck and total hip) were obtained using DXA. For lumbar spine BMD, L1-4 value was chosen for analyses, and when L1-4 was not suitable for analysis due to compression fracture or severe sclerotic change, L2-4 or L1-3 was used.
Our primary outcome was an osteoporotic fracture (hip, vertebral, upper arm, or wrist).
3. Model development and validation
The osteoporotic fracture predictive models for men and women were developed separately. Baseline characteristics are summarized mean and standard deviation for continuous variables and frequencies and percentages for categorical variables, respectively. The following variables were initially identified from the literature as traditional risk factors for osteoporotic fracture: age, height, weight, prior fracture, current smoking status, high alcohol intake, use of steroids, rheumatoid arthritis, and BMD. These covariates were screened with a significance level of P=0.05. The predictive models were estimated using logistic regression model in the modeling set, because the date of fracture could not be exactly identified. We followed each patient from the examination date in 2006 until the fracture or December 2012. The logistic regression model with k risk factors for time t (t=7) was estimated for each sex using the following equation:
where f(x,M)=β1(x1 - M1) + β2(x2 - M2) + ··· + βk (xk - Mk). Here, β1, β2, ···, βk are the regression coefficients; x1, x2, ···, xk are the risk factors for each individual; and M1, M2, ···, Mk are the mean values for each risk factor in the cohort.
The predictive accuracy for the occurrence of a fracture within a 7-year period was assessed for discrimination and validation. Discrimination or the ability to distinguish between those who experienced the event and those who did not was assessed using c-statistics.[15]
When c-statistics become closer to 1.0, it means that the discriminatory power is higher.
To test goodness of fit for logistic regression models, Hosmer-Lemeshow test was used.
Statistical analyses were performed using SAS version 9.3 (SAS Institute, Cary, NC, USA), P-values <0.05 were considered significant. Study protocols were in accordance with institutional guidelines and approved by an Institutional Review Board. Informed consent was obtained from the study participants.
RESULTS
Total number of participants was 768. There were 363 men (47.3%) and 405 women (52.7%). Table 1 showed the baseline characteristics. Osteoporotic fracture occurred in 36 men (9.9%) and in 50 women (12.3%).
Table 1. Baseline characteristic of study population.
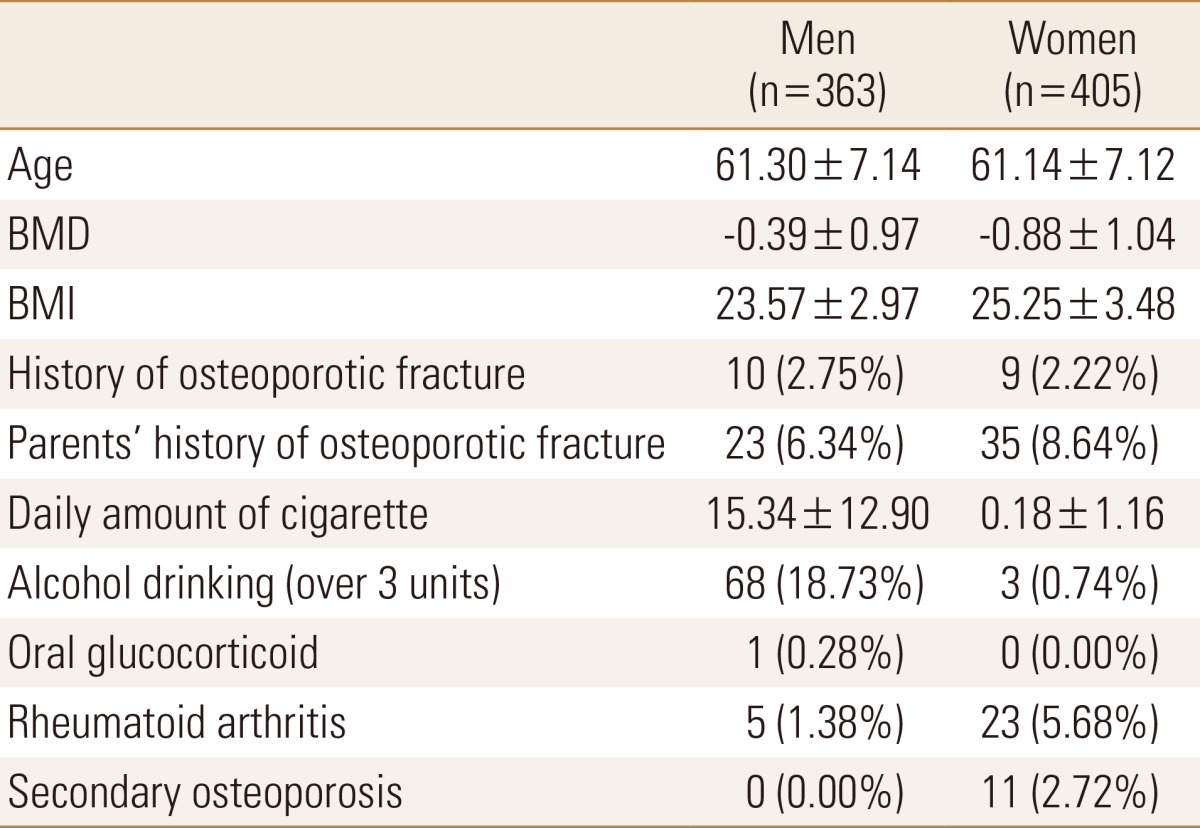
BMD, bone mineral density; BMI, body mass index.
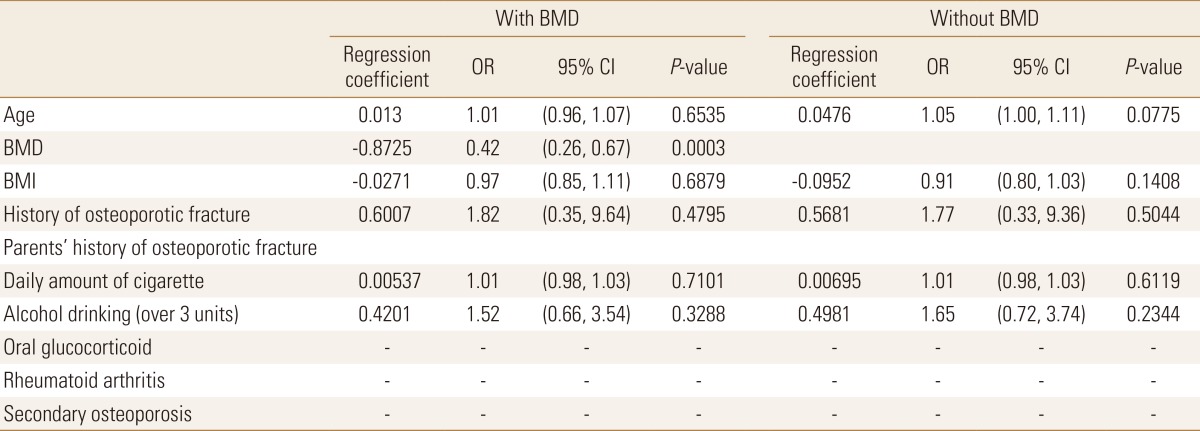
The major risk factor of osteoporotic fracture was BMD in men, and the risk of osteoporotic fracture decreased 58% in men, when one unit of BMD increased. Regression coefficient of each variable in the final multiple regression model are shown in Table 2. FRAX for Korean men was developed as follows;
| f(x) with BMD=-2.5346+0.013×(age-61.30)-0.8725×(BMD+0.39)-0.0271×(BMI-23.57)+0.6007×(history of osteoporotic fracture-0.0275)+0.00537×(daily smoking-15.34)+0.4201×(alcohol-0.1873) |
| f(x) without BMD=-2.3166+0.0476×(age-61.30)-0.0952×(BMI-23.57)+0.5681×(history of osteoporotic fracture-0.0275)+0.00695×(daily smoking-15.34)+0.4201×(alcohol-0.1873) |
Table 2. Regression coefficient in the final multiple regression model for men.
BMD, bone mineral density; OR, odds ratio; CI, confidence interval; BMI, body mass index.
Model including BMD and model without BMD showed same c-statistics of 0.739 in men, indicating that the discriminatory power is high. Hosmer-Lemeshow test showed that both models had goodness of fit.
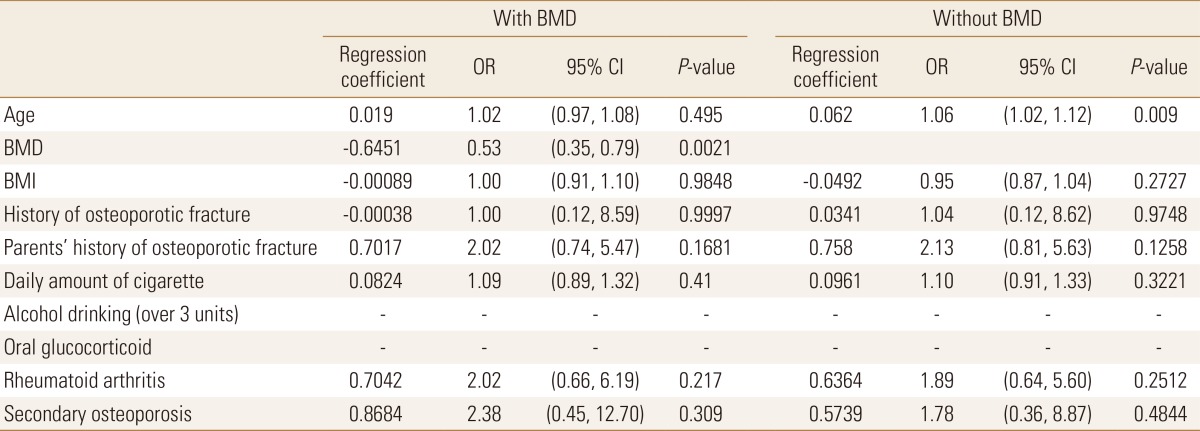
The major risk factor of osteoporotic fracture was also BMD in women, and the risk of osteoporotic fracture decreased 47% in women, when one unit of BMD increased. In model without BMD, the risk of osteoporotic fracture increased 6% in women, when age of women increased 1. Regression coefficient of each variable in the final multiple regression model are shown in Table 3. FRAX for Korean women was developed as follows;
| f(x) with BMD=-2.1858+0.019×(age-61.14)-0.6452×(BMD+0.88)-0.00089×(BMI-25.25)-0.00038×(history of osteoporotic fracture-0.0222)+0.7017×(family history of fractures-0.0864)+0.0824×(daily smoking-0.18)+0.7042× (RA-0.0568)+0.8684×(secondary osteoporosis-0.0272) |
| f(x) without BMD=-2.0808+0.062×(age-61.14)-0.0492×(BMI-25.25)+0.0341×(history of osteoporotic fracture-0.0222) +0.758×(family history of fractures-0.0864)+0.0961×(daily smoking-0.18)+0.6364×(RA-0.0568)+0.5739×(secondary osteoporosis-0.0272) |
Table 3. Regression coefficient in the final multiple regression model for women.
BMD, bone mineral density; OR, odds ratio; CI, confidence interval; BMI, body mass index.
Model including BMD showed c-statistics of 0.718 in women, and model without BMD showed c-statistics of 0.73 in women, indicating that the discriminatory power of each model is high. Hosmer-Lemeshow test showed that both models had goodness of fit.
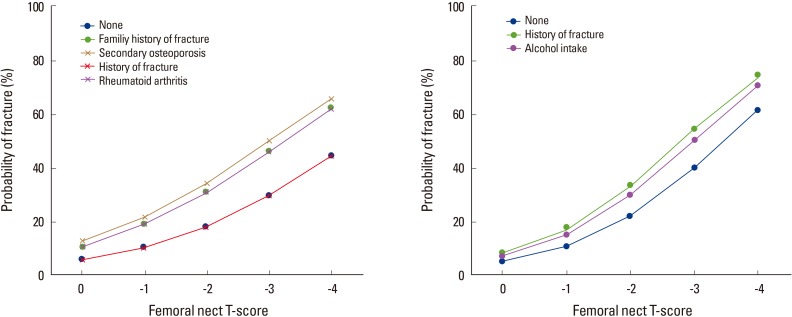
Figure 1 showed the probability of 7-year fracture risk according to T-score of BMD in 65-year old non-smoking Korean men and women with body mass index (BMI) of 25.
Fig. 1. The probability of 7-year fracture risk according to T-score of bone mineral density in 65-year-old non-smoking Korean men and women with body mass index of 25.
DISCUSSION
In this study, osteoporotic FRAX for Korean was developed and validated in Korean population based on community-based cohort.
To develop this model, we included simple variables, which have been identified in the literature as traditional risk factors for osteoporotic fracture; age, height, weight, prior fracture, current smoking status, high alcohol intake, use of steroids, rheumatoid arthritis, and BMD. Moreover, we presented the assessment model even without BMD. This means that the estimation can be easily used for primary care setting to decide whether to evaluate BMD as well as for self-screening purposes in the general population.
Major risk factor for osteoporotic fracture identified in this study was BMD, and this confirmed results of previous studies showing that higher BMD decreases the risk of osteoporotic fracture.[16,17,18,19] Adding BMD to the risk factor assessment could improve the prediction for osteoporotic fracture. However, in the some situation, which is limited to access DXA due to high cost or primary care, prediction model without BMD could be also helpful to determine whether to evaluate BMD.
There are some limitations in this study. First, we evaluated our main outcome, osteoporotic fracture, by using self-administration questionnaire. This might result in recall bias. Second, this model has not been validated in an independent population. There might be selection bias during developing cohort. Therefore, validation study is needed in an independent population or with other FRAXs, such as FRAX.[20,21]
However, this study is the first study of community-based cohort to develop estimation model of osteoporotic fracture risk. This study presented that prediction model is useful in primary care setting and in self-screening for osteoporosis in Korean population.
Footnotes
No potential conflict of interest relevant to this article was reported.
National Health Insurance Database was provided by the National Health Insurance Service (NHIS) of Korea. The authors would like to thank the National Health Insurance Service for cooperation. This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Korea (grant number: HI13C1522).
This study was provided with biospecimens and data from the Korean Genome Analysis Project (4845-301), the Korean Genome and Epidemiology Study (4851-302), and Korea Biobank project (4851-307, KBP-2014-25) that were supported by the Korea Center for Disease Control and Prevention, Republic of Korea.
References
- 1.Peck WA, Burckhardt P, Christiansen C, et al. Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993;94:646–650. doi: 10.1016/0002-9343(93)90218-e. [DOI] [PubMed] [Google Scholar]
- 2.Kang BJ, Lee YK, Lee KW, et al. Mortality after hip fractures in nonagenarians. J Bone Metab. 2012;19:83–86. doi: 10.11005/jbm.2012.19.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoon HK, Park C, Jang S, et al. Incidence and mortality following hip fracture in Korea. J Korean Med Sci. 2011;26:1087–1092. doi: 10.3346/jkms.2011.26.8.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee YK, Jang S, Jang S, et al. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int. 2012;23:1859–1865. doi: 10.1007/s00198-011-1833-5. [DOI] [PubMed] [Google Scholar]
- 5.Park C, Ha YC, Jang S, et al. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011;29:744–751. doi: 10.1007/s00774-011-0279-3. [DOI] [PubMed] [Google Scholar]
- 6.Johnell O, Kanis JA, Oden A, et al. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185–1194. doi: 10.1359/JBMR.050304. [DOI] [PubMed] [Google Scholar]
- 7.Lim LS, Hoeksema LJ, Sherin K, et al. Screening for osteoporosis in the adult U.S. population: ACPM position statement on preventive practice. Am J Prev Med. 2009;36:366–375. doi: 10.1016/j.amepre.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 8.Cadarette SM, Jaglal SB, Kreiger N, et al. Development and validation of the Osteoporosis Risk Assessment Instrument to facilitate selection of women for bone densitometry. CMAJ. 2000;162:1289–1294. [PMC free article] [PubMed] [Google Scholar]
- 9.Salaffi F, Silveri F, Stancati A, et al. Development and validation of the osteoporosis prescreening risk assessment (OPERA) tool to facilitate identification of women likely to have low bone density. Clin Rheumatol. 2005;24:203–211. doi: 10.1007/s10067-004-1014-4. [DOI] [PubMed] [Google Scholar]
- 10.Middleton RG, Shabani F, Uzoigwe CE, et al. FRAX and the assessment of the risk of developing a fragility fracture. J Bone Joint Surg Br. 2012;94:1313–1320. doi: 10.1302/0301-620X.94B10.28889. [DOI] [PubMed] [Google Scholar]
- 11.Min YK, Lee DY, Park YS, et al. A FRAX Experience in Korea: fracture risk probabilities with a country-specific versus a surrogate model. J Bone Metab. 2015;22:113–118. doi: 10.11005/jbm.2015.22.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barrett-Connor E, Siris ES, Wehren LE, et al. Osteoporosis and fracture risk in women of different ethnic groups. J Bone Miner Res. 2005;20:185–194. doi: 10.1359/JBMR.041007. [DOI] [PubMed] [Google Scholar]
- 13.STAT-Korea. Census 2000. 2001. [cited by 2016 Feb 26]. Available from: http://www.kosis.kr.
- 14.Shin C, Abbott RD, Lee H, et al. Prevalence and correlates of orthostatic hypotension in middle-aged men and women in Korea: the Korean Health and Genome Study. J Hum Hypertens. 2004;18:717–723. doi: 10.1038/sj.jhh.1001732. [DOI] [PubMed] [Google Scholar]
- 15.Han JH, Park HS, Kim JA, et al. Apolipoprotein B is a better marker than non-HDL-cholesterol for the metabolic syndrome in Koreans. Atherosclerosis. 2008;197:333–338. doi: 10.1016/j.atherosclerosis.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 16.Hung LK, Wu HT, Leung PC, et al. Low BMD is a risk factor for low-energy Colles' fractures in women before and after menopause. Clin Orthop Relat Res. 2005:219–225. doi: 10.1097/01.blo.0000155345.04782.14. [DOI] [PubMed] [Google Scholar]
- 17.Siris ES, Miller PD, Barrett-Connor E, et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001;286:2815–2822. doi: 10.1001/jama.286.22.2815. [DOI] [PubMed] [Google Scholar]
- 18.Cawthon PM, Ewing SK, Mackey DC, et al. Change in hip bone mineral density and risk of subsequent fractures in older men. J Bone Miner Res. 2012;27:2179–2188. doi: 10.1002/jbmr.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau EM, Woo J, Leung PC, et al. Low bone mineral density, grip strength and skinfold thickness are important risk factors for hip fracture in Hong Kong Chinese. Osteoporos Int. 1993;3:66–70. doi: 10.1007/BF01623375. [DOI] [PubMed] [Google Scholar]
- 20.Kanis JA, Johnell O, De Laet C, et al. International variations in hip fracture probabilities: implications for risk assessment. J Bone Miner Res. 2002;17:1237–1244. doi: 10.1359/jbmr.2002.17.7.1237. [DOI] [PubMed] [Google Scholar]
- 21.Kanis JA, Odén A, McCloskey EV, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23:2239–2256. doi: 10.1007/s00198-012-1964-3. [DOI] [PMC free article] [PubMed] [Google Scholar]