Abstract
The eponym “Guyon canal” refers to the ulnar tunnel at the wrist that was named after the French surgeon Jean Casimir Félix Guyon who first described this space in 1861. After Guyon’s discovery, clinicians have focused their interest on symptoms caused by compression of structures occupying this canal (later named ulnar tunnel syndrome, or Guyon syndrome). However disagreement and confusion persisted over the correct anatomical boundaries and terminology used to describe the ulnar tunnel. Through anatomical investigation and evolving clinical case studies, the current understanding of the anatomy of the ulnar tunnel was established. This article examines the evolution of the anatomical description of the ulnar tunnel and its relevant clinical associations, and casts light on the life and contributions of Jean Casimir Félix Guyon.
Keywords: Guyon canal, Jean Casimir Félix Guyon, Ulnar tunnel, Ulnar tunnel syndrome, Pisohamate hiatus
Jean Casimir Félix Guyon described the ulnar tunnel at the wrist in 1861. The French surgeon observed what he described as “petits lobules”(1) appearing on the palmar aspect of his own wrist when applying pressure to the hypothenar eminence. Intrigued by this discovery, Guyon studied the anatomical dissection of the wrist. He was the first to provide an anatomical description of the ulnar tunnel and its contents, from which he believed those fat lobules to have protruded. His description of the ulnar tunnel was first presented and published in the Bulletin de la Societe de Anatomique de Paris in 1861. (1,2) From 1861–1953, numerous studies refined the anatomic description of the ulnar tunnel, but it was not until 1953 that the first piece of English literature appeared to link Guyon to the ulnar tunnel. (3) It has since received the eponym Guyon canal. As more studies were conducted on the anatomy of the ulnar tunnel, an additional tunnel containing the deep branch of the ulnar nerve was discovered distal to the ulnar tunnel, the pisohamate hiatus. The study of the anatomy of these two tunnels has led to a better understanding of how pathoanatomy may lead to compression of the ulnar nerve at the wrist joint. In this article we investigate the appropriate terminology of the ulnar “tunnel” and see how the evolving anatomical descriptions helped surgeons better understand the symptoms associated with compression at the ulnar tunnel.
An extensive literature search was conducted which included the archives of the libraries of our home institution, the Island of Reunion of France, the Inter-University Science Library (BIUS) affiliated with Paris Descartes University, the National Academy of Medicine, and the Pierre and Marie Curie University in Paris. Additionally, we collected information from online databases such as the History of Medicine and Sudoc, and translated original articles from French, German, Italian, and Spanish.
Discovery of the ulnar tunnel
After making his first observation, Guyon thought that subcutaneous “lobules”(1) of his wrist were a result of synovial thickening in the area under the skin where the wrist connects with the hand. Initially, Guyon consulted Dr. Ollier, who was a surgeon at Hotel Dieu hospital in Lyon, France. (4) Dr. Ollier had made similar observations in the past of what Guyon described as “petits lobules”. Dr. Ollier informed Guyon that this finding was rather common, and he had concurred that this was due to synovial thickening where the wrist meets the hand. (1,2) Curious by the idea that these subcutaneous lobules could be present in all wrists, Guyon performed a cadaveric dissection of the wrist. After removing the subcutaneous layer, Guyon found a few small fatty masses protruding through the palmar fascia when he applied pressure to the area. He concluded that these masses were similar to the “lobules” he initially palpated on his wrist. After further dissection, he discovered a “loge” or a space which he described as “une petite loge intra-aponévrotique” [a small intra-aponeurotic space]. (1,2) The anterior wall of this space was made of a fibrous bed that merged with the palmar aponeurosis, while the posterior wall was made of the transverse carpal ligament. The medial boundary consisted of the pisiform bone. Distally this space ended at a level of the middle of what was known at the time as the ‘anterior ligament of the carpus’. The total dimension of the tunnel Guyon described was one centimeter to one and a half centimeters in all directions. During his dissections he could see a large, mobile, fatty mass loosely attached to the lateral walls of the tunnel and concluded that this was the fatty “lobule” he had first observed. (1) Guyon’s fascination with his newly discovered tunnel continued as he made further discoveries. He noted that both the ulnar artery and nerve run against the posterior wall of the tunnel, seemingly protected by the fatty mass. At this point, he came to realize that this canal is a host of vital structures of the hand and not simply a space occupied by fatty lumps. Guided by his findings, Guyon was the first to hypothesize that the ulnar tunnel could be a potential site for ulnar nerve compression at the wrist. Guyon’s findings and hypothesis opened the door for future research concerning the anatomy of the ulnar tunnel and pathogenesis of ulnar compression neuropathy at the wrist.
Evolution of anatomy of the ulnar tunnel
After Guyon’s discovery in 1861, research concerning the ulnar tunnel of the wrist was predominantly focused on compression neuropathy of the ulnar nerve and only little attention was directed towards the anatomy of the ulnar tunnel. In 1908, Hunt et al(5) were first to formally discuss the etiology of the ulnar nerve compression at the wrist. When Hunt and colleagues clinically evaluated patients with wrist injuries, they noted (according to anatomic descriptions made by Testut)(6) that within the ulnar tunnel, the ulnar nerve divides into two terminal branches: the deep motor branch and the superficial sensory branch. After branching, the deep motor branch passes through the hypothenar muscles. On reviewing their case reports, only symptoms of motor nerve deficits were clinically evident. This led the authors to conclude that compression neuropathy occurring at the ulnar tunnel only involves the deep motor branch of the ulnar nerve. Furthermore, they proposed that the hypothenar muscles may cause compression of the deep branch of the ulnar nerve as the nerve passes through the muscle bellies.
From 1952–1955, many cases of ganglionic compression of the deep motor branch of the ulnar nerve at the wrist were reported. (7–9) From these reports surgeons noted that removal of ganglions results in improvements of both motor and sensory function of the ulnar nerve. This was in contrast to the proposed theory of ulnar nerve compression made earlier by Hunt and colleagues, (5) that indicated compression of the deep branch of the ulnar nerve by hypothenar muscles. Through constant correlation between symptoms and anatomical compression sites of the ulnar nerve, it became clear that knowledge of the anatomy of the ulnar tunnel was paramount to better understand symptoms arising from ulnar nerve compression at the wrist.
The first known mention of Guyon in relation to the ulnar tunnel was in 1953 when Kaplan gave a brief account of the ulnar tunnel in his book entitled ‘Functional and Surgical Anatomy of the Hand’. (3) Kaplan noted that in French literature the ulnar tunnel was referred to as the tunnel of Guyon. (3) To this point it was not clear who should be credited for giving the eponym Guyon canal, but at least for the English-speaking world, Kaplan should be acknowledged for bringing attention to this important anatomical structure and to its founder Guyon.
In 1965, Dupont et al(10) were first to propose the term “ulnar tunnel syndrome” for patients who were suffering symptoms of ulnar nerve compression at the wrist. As the authors were operating on a hand of a patient suffering from acute thromboangiitis of the ulnar artery at the wrist, they noticed that the ulnar artery ran within a close proximity to the ulnar nerve. The authors proposed that pressure on the ulnar nerve could arise from structures within the ulnar tunnel, such as the ulnar artery and/or ganglions. They also stated that the ulnar tunnel is triangular in shape, and that the anterior border was made of the volar carpal ligament, the posterior border was made of the transverse carpal ligament, while the medial border was made of the pisiform bone and flexor carpi ulnaris tendon. No proximal or distal boundaries were given (Fig. 1). (10) This description of ulnar tunnel anatomy was similar to the one described earlier by Guyon. (1,2) Dupont and colleagues further suggested that pathology involving any of the boundaries of the ulnar tunnel could possibly lead to compression neuritis of the ulnar nerve.
Figure 1.
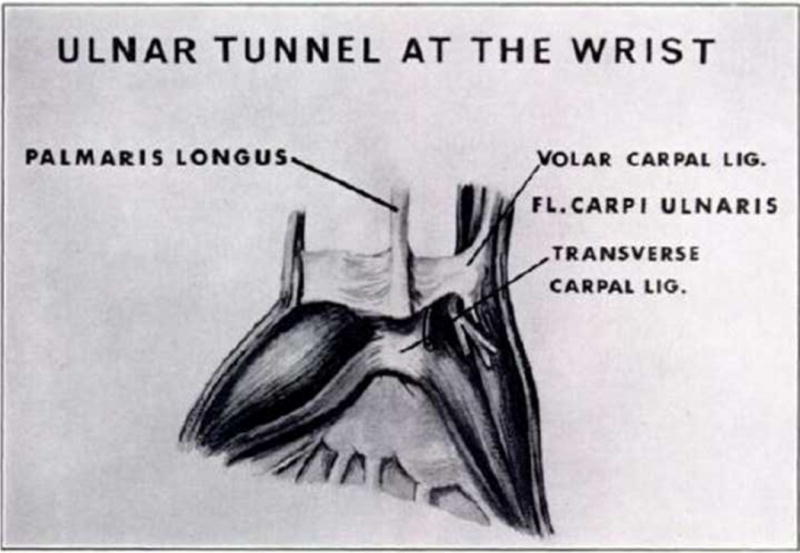
Anterior view of the wrist. Shows the location of the volar carpal ligament and the transverse carpal ligament in relation to the ulnar tunnel. (Reprinted with permission from Dupont C, Cloutier GE, Prevost Y, Dion MA. Ulnar-tunnel syndrome at the wrist. A report of four cases of ulnar-nerve compression at the wrist. J Bone Joint Surg Am. Jun 1965;47:757–761. Copyright © 1965 Journal of Bone and Joint Surgery American.)
New ideas about the shape of the ulnar tunnel were proposed by Grantham(11) in 1966 and Vanderpool et al(12) in 1968. Grantham(11) stated that using the term canal (or tunnel) to describe the space described by Guyon was wrong, since the ulnar tunnel was more comparable to a “lean-to” as the roof was oriented obliquely. Vanderpool et al(12) also described the ulnar tunnel as triangular, but more importantly stated that the ulnar nerve runs in more than one tunnel at the wrist. They noted that the ulnar nerve runs first within the known boundaries of the ulnar tunnel, and then branches as it emerges from its distal end to enter into a second tunnel. This second tunnel was later called the pisohamate hiatus. (13) Vanderpool described the pisohamate hiatus as a small tunnel located just distal to the ulnar tunnel, and containing only the deep branch of the ulnar nerve. Specifically, the pisohamate hiatus is located posteriolateral to the pisiform bone and is bound proximally by the pisohamate ligament and distally by the origin of the hypothenar muscles (Fig. 2 A). In 1969, Hayes et al(14) elaborated on the anatomy of the pisohamate hiatus, stating that it was bound deeply by the pisohamate ligament and superficially by a fibrous arch. This fibrous arch is a sling of the hypothenar muscle fascia, and connects the pisiform bone to the hook of the hamate (Fig. 2 A–C). The current anatomical description of the pisohamate tunnel is similar to this description provided by Hayes et al. (14–16) Hayes and colleagues(14) also commented that pressure from this fibrous arch during hypothenar muscle contraction may compress the deep branch of the ulnar nerve, thus supporting the hypothesis made by Hunt and colleagues(5) in 1908 when they stated that the ulnar nerve could be compressed as it passes in between the hypothenar muscles.
Figure 2.
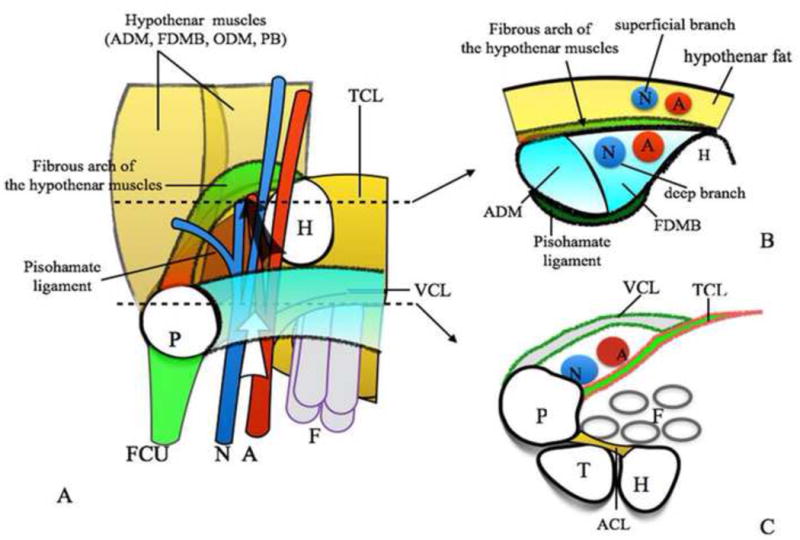
A. Antero-posterior view of Guyon canal/ulnar tunnel (white arrow) and pisohamate hiatus (black arrow). TCL, transverse carpal ligament ; VCL, volar carpal ligament; FCU, flexor carpi ulnaris; PB, palmaris brevis; ODM, opponens digiti minimi; ADM, abductor digiti minimi; FDMB, flexor digiti minimi brevis; F, finger flexor tendons; N, ulnar nerve; A, ulnar artery; H, hamate.
B. Axial view of pisohamate hiatus. (Uriburu et al., 1976(13)) Ulnar nerve and artery are divided into superficial and deep branches by the fibrous arch of the hypothenar muscles.
C. Axial view of Guyon canal/ulnar tunnel. (Guyon, 1861(1,2)) ACL, anterior carpal ligament.
The comprehensive assessment of anatomy has improved surgeons’ understanding of the pathogenesis of ulnar nerve compression within the ulnar tunnel. Perhaps this was most evident when Shea and McClain in 1969(17) utilized this wealth of knowledge regarding the anatomy of the ulnar tunnel to give a detailed account on ulnar nerve compression pathology. They were the first to propose a classification of ulnar nerve compression syndrome into three types based on the site of ulnar nerve compression.
Type I: Compression of the common ulnar nerve bundle causing sensory loss and motor weakness.
Type II: Compression of the deep motor branch of the ulnar nerve, leading to motor weakness of muscles innervated by this branch.
Type III: Compression of the superficial sensory branch of the ulnar nerve, which leads to sensory deficits.
Shea and McClain’s description of the ulnar tunnel is similar to the description provided by Dupont et al,(10) but they added that the pisiform formed the proximal and medial border while the hook of the hamate formed the lateral and distal border of the ulnar tunnel. (17) Furthermore, their work provided supporting evidence of Hunt et al(5) and Hayes et al(14) findings of compression of deep branch of the ulnar nerve by the fibrous arch of the pisohamate hiatus.
Four years later in 1973, Lotem et al(18) revisited the anatomy of the ulnar tunnel and the fibrous arch of the pisohamate hiatus and provided more details on its clinical relevance. They confirmed a secondary compression site of the ulnar nerve at the pisohamate hiatus and its fibrous arch inlet. In both their cases and other cases,(19,20) they found that surgeons might sometimes and unknowingly cut the fibrous arch of the pisohamate hiatus opening when performing ulnar nerve decompression, consequently resulting in unintentional decompression of the deep branch of the ulnar nerve. A patient’s subsequent recovery would lead surgeons to believe that they had successfully found and relieved the correct site of ulnar nerve compression. (18)
To resolve any remaining ambiguity related to the anatomy of the ulnar tunnel, Gross and Gelberman in 1985(21) proposed the three zone theory of the anatomy of the ulnar tunnel at the wrist according to the level of branching of the ulnar nerve. This is the most accepted description of the ulnar tunnel today.
Zone I: Begins from the proximal edge of the palmar carpal ligament and ends distally at the bifurcation of the ulnar nerve.
Zone II: Runs from just distal to the bifurcation of the ulnar nerve to the fibrous arch of the hypothenar muscles and contains the deep branch of the ulnar nerve.
Zone III: Begins just distal to the bifurcation of the ulnar nerve and contains the superficial branch of the ulnar nerve.
This three zone anatomy classification proposed by Gross and Gelberman(21) perfectly matched with the clinical classification of symptoms of ulnar tunnel syndrome made by Shea and McClain in 1969. (17)
Guyon’s anatomical description of the ulnar tunnel and his suggestion of possible compression issues of the ulnar nerve set the stage for further investigation into the anatomy of the ulnar tunnel and compression neuropathy of the ulnar nerve. The discovery of the pisohamate hiatus as a second site of ulnar nerve compression made it clear that the anatomy of all structures surrounding the ulnar nerve needs to be taken into account when diagnosing ulnar nerve compression neuropathy. Compression of the ulnar nerve can happen in various locations, and this may result in patients complaining of different symptoms, making it important for surgeons to have a detailed understanding of the ulnar tunnel and its surrounding structures (Figs. 3 & 4).
Figure 3.
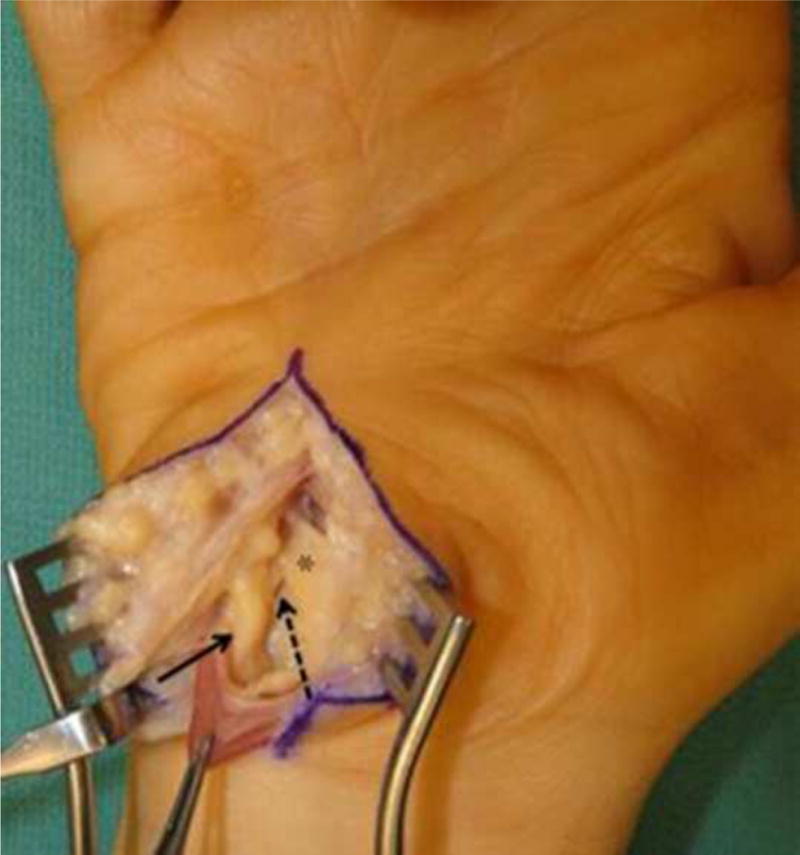
Intraoperative photograph of the right hand. Shown are the ulnar nerve (solid arrow), deep motor branch of the ulnar nerve (dotted arrow), and the pisohamate arch (*).
Figure 4.
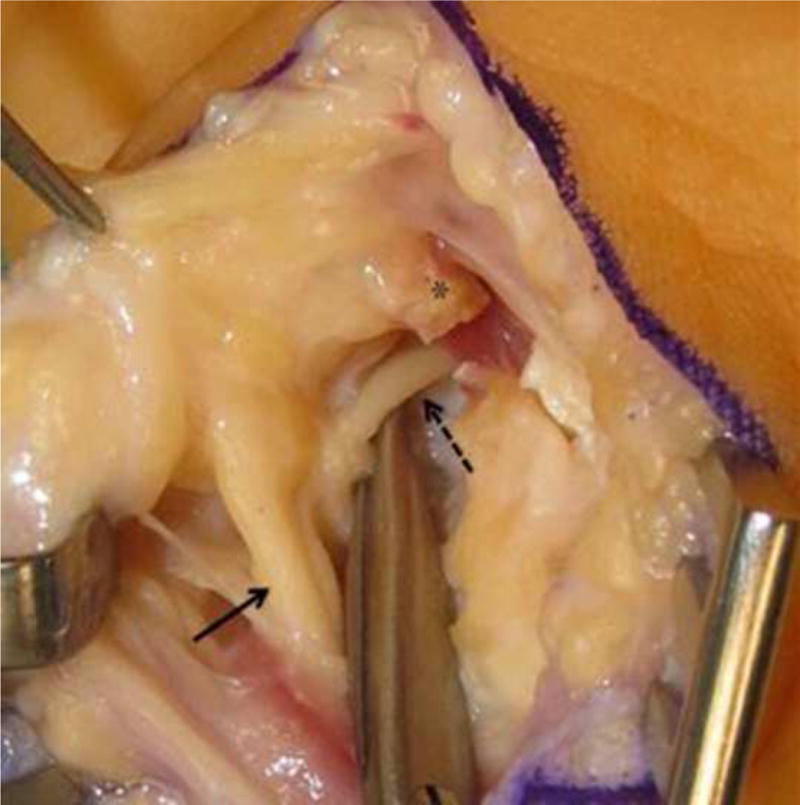
Magnified intraoperative photograph after pisohamate arch released. Shown are the ulnar nerve (solid arrow), the deep motor branch of the ulnar nerve (dotted arrow), and the stump of cut pisohamate arch (*).
Who is Guyon (1831–1920)?
Jean Casimir Félix Guyon (Fig. 5) was born in 1831 in the city of Saint Denis on the island of Reunion, a French colony located east of Madagascar. Guyon lived on this island with his family until he was three years old, when his family decided to relocate to France. Guyon lived initially with his family in Cherbourg and eventually they settled in Nantes. (22) As a young boy, Guyon was encouraged by his grandfather, a chief pharmacist in the French Navy, to pursue a career in medicine. Guyon eventually attended the Nantes school of medicine in his hometown and was the top performer of his class in medical school and throughout placements that followed. (23,24)
Figure 5.
Jean Casimir Félix Guyon (1831–1920) (BIU Health Medicine: Ref Image 02672 http://www2.biusante.parisdescartes.fr/img/?refphot=02672&mod=s)
In 1858, Guyon received his doctorate degree from the University of Paris, after defending his thesis under the direction of his mentor Dr. Velpeau, a French anatomist and surgeon. (25,26) Upon graduation Guyon was initially interested in gynecology, as can be seen by the topic of his thesis, “Étude sur les cavités de l’utérus à l’état de vacuité” [Study on the uterine cavity in the state of emptiness]. (26) After completing his surgical training in 1861, Guyon’s interest suddenly switched to urology. (22) For him, being a physician meant an innate sense of curiosity, and it was this quality that led him to discover the ulnar tunnel in the wrist, that carried his name thereafter.
In addition to his contributions to the field of hand surgery, Guyon made contributions to other fields and medicine in general throughout his career. Guyon is known as the “father of modern day urology”, and he was an outstanding teacher in this subject, attracting students from all over the world. He authored numerous medical books and journal articles, on both urology and general surgery. (27,28) He founded the medical school of Necker at Necker Hospital in Paris,(29) and was named professor of Surgical Pathology in 1877 and of Genitourinary Surgery in 1890. (22,23) After retiring from Chief of Urology at Necker Hospital in 1906, he was succeeded by one of his most favored students, Joaquin Albarrán, a Cuban surgeon. Ironically, Albarrán died in 1912, eight years before his famed master. (29) Guyon quietly retired on his two properties in France,(25,29) and died peacefully after 13 years of retirement in 1920 on the eve of his 90th birthday. (22,23,30) In 1979, France issued a stamp honoring Guyon to acknowledge his numerous impacts on the medical field. His birthplace of Reunion also issued this stamp, but it was never sold (Fig. 6). (31)
Figure 6.
A stamp issued by France in 1979 in honor of Guyon. (Reproduced from [Felix Guyon 1831–1920; Haas, L.F.; Volume 74; Page 698; 2003] with permission from BMJ Publishing Group Ltd.)
Acknowledgments
Disclosure: Research reported in this publication was supported by awards from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (2R01 AR047328 – 06), the National Institute on Aging and National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR062066), and a Midcareer Investigator Award in Patient-Oriented Research (2K24 AR053120-06) to Dr. Kevin C. Chung. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Guyon F. Note sure une disposition anatomique prope a la face antericure de la region du poignet et non encore decrite par le docteur. Bulletin de la societe de anatomique de Paris. 1861;6:184–186. [Google Scholar]
- 2.Guyon F. Note on the anatomical condition affecting the underside of the wrist not previously reported. J Hand Surg Br. 2006 Apr;31(2):147–148. doi: 10.1016/j.jhsb.2005.12.008. 1861. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan E. Functional and Surgical Anatomy of the Hand. Philadelphia London, Montreal: J.B. Lippincott Company; 1953. [Google Scholar]
- 4.Sournia JC. [Leopold Ollier (1830–1900)] Hist Sci Med. 1994;28(2):109–114. [PubMed] [Google Scholar]
- 5.Hunt JR. Occupation neuritis of the deep palmar branch of the ulnar nerve. The Journal of Nervous and Mental Disease. 1908;35(11):673–689. [Google Scholar]
- 6.Testut L. Traité d’anatomie humaine. Paris: Gaston Doin et Cie; 1899. [Google Scholar]
- 7.Brooks DM. Nerve compression by simple ganglia. J Bone Joint Surg Br. 1952 Aug;34-B(3):391–400. doi: 10.1302/0301-620X.34B3.391. [DOI] [PubMed] [Google Scholar]
- 8.Seddon HJ. Carpal ganglion as a cause of paralysis of the deep branch of the ulnar nerve. J Bone Joint Surg Br. 1952 Aug;34-B(3):386–390. doi: 10.1302/0301-620X.34B3.386. [DOI] [PubMed] [Google Scholar]
- 9.Mallett BL, Zilkha KJ. Compression of the ulnar nerve at the wrist by a ganglion. Lancet. 1955 Apr 30;268(6870):890–891. doi: 10.1016/s0140-6736(55)90379-2. [DOI] [PubMed] [Google Scholar]
- 10.Dupont C, Cloutier GE, Prevost Y, Dion MA. Ulnar-tunnel syndrome at the wrist. A report of four cases of ulnar-nerve compression at the wrist. J Bone Joint Surg Am. 1965 Jun;47:757–761. [PubMed] [Google Scholar]
- 11.Grantham SA. Ulnar compression in the loge de Guyon. Jama. 1966 Aug 8;197(6):509–510. [PubMed] [Google Scholar]
- 12.Vanderpool DW, Chalmers J, Lamb DW, Whiston TB. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg Br. 1968 Nov;50(4):792–803. [PubMed] [Google Scholar]
- 13.Uriburu IJ, Morchio FJ, Marin JC. Compression syndrome of the deep motor branch of the ulnar nerve. J Bone Joint Surg. 1976;58(1):145–147. [PubMed] [Google Scholar]
- 14.Hayes JR, Mulholland RC, O’Connor BT. Compression of the deep palmar branch of the ulnar nerve. Case report and anatomical study. J Bone Joint Surg Br. 1969 Aug;51(3):469–472. [PubMed] [Google Scholar]
- 15.Almeida V, de Carvalho M. Lesion of the deep palmar branch of the ulnar nerve: Causes and clinical outcome. Neurophysiologie Clinique/Clinical Neurophysiology. 2010;40(3):159–164. doi: 10.1016/j.neucli.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 16.Chen SH, Tsai TM. Ulnar tunnel syndrome. J Hand Surg Am. 2014 Mar;39(3):571–579. doi: 10.1016/j.jhsa.2013.08.102. [DOI] [PubMed] [Google Scholar]
- 17.Shea JD, McClain EJ. Ulnar-nerve compression syndromes at and below the wrist. J Bone Joint Surg Am. 1969 Sep;51(6):1095–1103. [PubMed] [Google Scholar]
- 18.Lotem M, Gloobe H, Nathan H. Fibrotic arch around the deep branch of the ulnar nerve in the hand. Anatomical observations. Plast Reconstr Surg. 1973 Nov;52(5):553–556. doi: 10.1097/00006534-197311000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Lotem M, Fried A, Solzi P, Najenson T. Ulnar tunnel syndrome. A case report and review of the anatomy and literature. Europa Medicophysica [Google Scholar]
- 20.Kleinert HE, Hayes JE. The ulnar tunnel syndrome. Plast Reconstr Surg. 1971 Jan;47(1):21–24. doi: 10.1097/00006534-197101000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel. Clin Orthop Relat Res. 1985 Jun;(196):238–247. [PubMed] [Google Scholar]
- 22.Loukas M, Linganna S, Jordan R. Jean Casimir Felix Guyon–urologist and anatomist. Clin Anat. 2007 Jan;20(1):1–2. doi: 10.1002/ca.20411. [DOI] [PubMed] [Google Scholar]
- 23.Death of Professor Guyon. Jama. 1920;75(7):489. [Google Scholar]
- 24.LaHuppe E. Felix Guyon. In: Roussin A, editor. Album de l’ile de La Reunion. pp. 160–162. [Google Scholar]
- 25.Felix Guyon (1831–1920) 2014 http://translate.google.com/translate?hl=en&sl=fr<=en&u=http%3A%2F%2Fwww.patrimoine-reunion.org%2Fnotre-histoire%2Fla-reunion-des-grands-hommes%2Fsciences%2F113-guyon-felix-1831–1920&sandbox=1, 2014. Accessed 6/11/2014.
- 26.Guyon F. Etude sur les cavités de l’utérus à l’état de vacuité. Medicine; Paris: 1858. [Google Scholar]
- 27.Malgaigne J. Lecons d’orthopedie. 1862 [Google Scholar]
- 28.Guyon JCF. Ėléments de chirurgie clinique coaprenant le diagnostic chirurgical, les opérations en général, les méthodes opératoires, l’hygiène, le traitement des blessés et des opérés. Paris: J. -B. Bailliére et fils; 1873. [Google Scholar]
- 29.Shampo M, Kyle R. Jean Casimir Felix Guyon. Jama. 1981;246(6):644. doi: 10.1001/jama.246.6.644. [DOI] [PubMed] [Google Scholar]
- 30.Professor JCF Guyon. Nature. 1920;105:721. [Google Scholar]
- 31.Haas LF. Felix Guyon 1831–1920. J Neurol Neurosurg Psychiatry. 2003 Jun;74(6):698. doi: 10.1136/jnnp.74.6.698. [DOI] [PMC free article] [PubMed] [Google Scholar]


