Abstract
Purpose
To evaluate the clinical reliability of the Bosniak classification in Korea, and to identify independent predictors of malignancy in complicated renal cysts.
Materials and Methods
We reviewed the records of 368 patients with renal cysts between January 2001 and December 2014; 14 patients were excluded, due to interobserver variability in Bosniak classification between the radiologist and urologist. Clinical characteristics and radiologic findings of malignant cystic masses were analyzed, retrospectively.
Results
In 324 surgically excised lesions from patients (n=312) with renal cysts, the percentages of malignancy in the different Bosniak classifications were as follows: category I, 1.0% (1 of 103); II, 3.8% (2 of 53); IIF, 17.1% (7 of 41); III, 38.0% (27 of 71); and IV, 82.1% (46 of 56). Mean age and lesion size were 59.88±11.9 years (180 men, 144 women) and 5.47±3.51 cm, respectively. Univariate analysis identified hypertension (p=0.011), a history of smoking (p=0.038), and obesity (p=0.015) as the strongest risk factors of malignancy. In a study of Bosniak category III patients, hypertension (p=0.018), lesion size (p<0.001), and difference of Hounsfield Unit (HU) (p=0.027) were the strongest risk factors of malignancy. Multivariate analysis identified lesion size as the strongest potential predictor of malignancy, followed by hypertension and difference of HU.
Conclusions
Risk factors of malignancy in complicated renal cyst patients were not different from those published previously. In Bosniak category III lesions, hypertension and lesion size were the strongest predictors of malignancy. Characteristically, the lesion size was smaller than in benign complicated renal cysts, in contrast with other categories.
Keywords: Classification, Diagnostic imaging, Renal cell carcinoma
INTRODUCTION
Since radiologic diagnostic criteria were first published for the classification of renal cysts in 1986 [1], the Bosniak classification system has been widely implemented as a diagnostic method, which uses computed tomography (CT) findings to categorize cystic renal masses, based on imaging features associated with malignancy (e.g., septa formation, wall thickening including nodal components, septa and/or wall calcification, hyperdense cystic content, and contract enhancement following intravenous contrast injection).
Introduction of the Bosniak category IIF in 1993 was thought to increase the accuracy of the classification system by downgrading lesions not complex enough to be characterized as III, but more complex than II category lesions.
The limited ability to predict malignancy in category IIF and III lesions cause some patients to undergo unnecessary surgical procedures, and cancer may be missed. Malignancy rates in category III lesions have been reported at 50% (range, 31%–100%) [2]. A further limitation of the Bosniak classification system is interobserver variation (e.g., differences in interobserver agreement), especially concerning category IIF and III lesions. Some authors recommended biopsy of the infectious nature mass or an indeterminate category. Renal biopsy is unreliable due to high numbers of false negative results and the diagnostic efficacy of small renal mass and complicated renal cyst biopsies remains controversial [3].
Since a significant difference to the quality of life of patients and oncological outcomes depend on the Bosniak category, accurate classification can be regarded as the most important clinical indicator in the management of renal cysts. Some reports of the clinical characteristics of category IIF and III complicated renal cysts in Western countries have been published [4]. However, the study of renal cysts and their clinical characteristics in Korea is still insufficient.
We aimed to evaluate the clinical reliability of Bosniak classification as the main preoperative diagnostic imaging method of renal cysts in Korea, and to identify preoperative predictors of malignancy in complicated renal cysts.
MATERIALS AND METHODS
1. Patients
Between January 2001 and December 2014, 368 patients with renal cysts were recruited. All renal cystic lesions were surgically removed. Patients (n=24) with magnetic resonance imaging examination only, CT performed at a different hospital or insufficient CT protocols were excluded due to a lack of data. Three patients with polycystic kidneys; 14 patients subject to interobserver variations in Bosniak classification between the radiologist and urologist; and a further 15 patients with a pathologic diagnosis at percutaneous biopsy were excluded because of potential sampling errors. Thus, in total, 324 surgically excised renal cystic lesions from 312 patients (12 patients had 2 renal cystic lesions each) were included in the final analysis. The operation in classification I, II and IIF cyst were performed by laparoscopic cyst unroofing followed by inspection or frozen-biopsy of cyst basal lesion. We performed the laparoscopic partial or radical nephrectomy depending on the size and location of tumor in classification III, IV. This study was approved by the Institutional Review Board for Wonkwang University Hospital and School of Medicine (WKUHIRB-1529).
2. Data collection
Patient data was recorded, retrospectively from electronic medical records and imaging reports. Clinical data included age, sex, and body mass index, as well as, history of smoking, hypertension, hemodialysis, or history of malignancy such as primary renal cell carcinoma (RCC), or neoplasm originating in another organ. Imaging data included initial category of Bosniak classification, largest diameter of the cystic lesion, number and laterality, Hounsfield unit (HU) difference (def ined as a corticomedullary phase enhancement minus precontrast phase enhancement on CT at highest enhancement of cystic mass area), coexisting Bosniak category III or IV lesion.
A radiologist and urologist reclassified cystic lesions identified through CT imaging, according to the Bosniak classification system [5]. After excluding for interobserver variation in classification, imaging analysis was performed in consensus. Histopathological reports were reviewed, and cystic mass lesions classified as benign or malignant.
3. Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). Averaged data are presented as means plus/minus the standard deviation for continuous variables. Student t-test was used to compare means for continuous variable factors. Chi-squar test was used to analyze categorical variables. Univariate and multivariate analyses were performed to identify significant predictive variables. Two-tailed p-value less than 0.05 was considered statistically significant.
RESULTS
Clinical characteristics of the patients and pathological findings in Bosniak classification are shown in Table 1. According to the Bosniak classification system, cystic renal masses were recorded as category I, II, IIF, III, or IV in 31.8% (103 of 324), 16.4% (53 of 324), 12.7% (41 of 324), 21.9% (71 of 324), and 17.3% (56 of 324) of cases, respectively. Mean age and lesion size were 59.88±11.9 years and 5.47±3.51 cm, respectively including 180 men and 144 women with cystic lesions presenting on the left side in 66.9% (217 of 324) of cases.
Table 1. Patients' characteristics and pathologic results in Bosniak classification.
| Variable | Bosniak classification | ||||
|---|---|---|---|---|---|
| I | II | IIF | III | IV | |
| No. of lesions | 103 | 53 | 41 | 71 | 56 |
| Age (y) | 60.96±10.34 | 61.47±12.49 | 59.01±12.09 | 55.89±13.81 | 61.29±13.28 |
| Sex, male:female | 59:44 | 33:20 | 25:16 | 28:43 | 35:21 |
| Body mass index (kg/m2) | 24.68±2.68 | 23.99±2.85 | 24.64±3.39 | 23.79±3.35 | 24.96±3.38 |
| Cyst size (cm) | 5.60±2.93 | 4.95±2.57 | 5.58±3.55 | 5.32±3.81 | 6.51±5.06 |
| Cyst laterality, right:left | 39:64 | 23:30 | 9:32 | 22:49 | 14:42 |
| Malignant cyst | 1 (1.0) | 2 (3.8) | 7 (17.1) | 27 (38.0) | 46 (82.1) |
| Incidence of malignancy (%) [19] | - | 13.7 | 14.3 | 50.8 | 90.1 |
Values are presented as mean±standard deviation or number (%).
Of 324 surgically excised lesions, from 312 patients with renal cysts, 25.6% (83 of 324) were malignant (Fig. 1) and 74.4% (241 of 324) were benign. The percentages of malignancy in the different Bosniak classifications were as follows: category I, 1.0% (1 of 103); II, 3.8% (2 of 53); IIF, 17.1% (7 of 41); III, 38.0% (27 of 71); and IV, 82.1% (46 of 56). There were no significant differences in the malignancy rates of Bosniak classification between ours and other previously published studies (Table 1). Surgical pathological findings of malignant cystic lesions included clear cell 69.9% (58 of 83), papillary 20.5% (17 of 83), and multilocular cystic renal cell 9.6% (8 of 83) carcinomas.
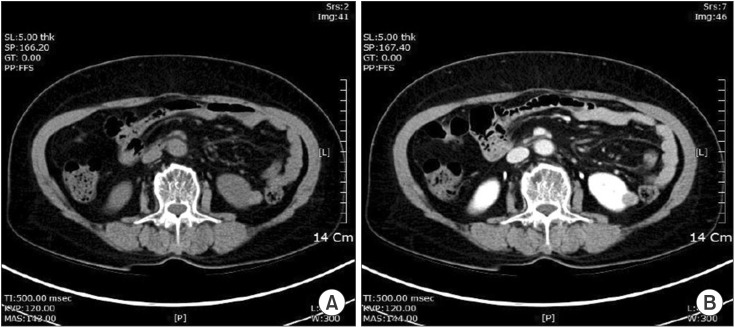
Fig. 1. A 62-year-old woman with a category II cystic lesion (hyperdense cyst) in the left kidney. The patient underwent laparoscopic partial nephrectomy. The final pathological diagnosis is renal cell carcinoma (papillary renal cell carcinoma). (A) Unenhanced computed tomography (CT) scan shows small, smooth-walled, high-density left renal cyst. (B) CT scan after administration of contrast material shows no enhancement of the cyst.
Table 2 summarizes a comparison of parameters between benign and malignant cysts, in patients with complicated renal cysts, including Bosniak categories II, IIF, III, and IV. There were significant differences in risk factors associated with RCCs between benign and malignant patients with complicated renal cysts (e.g., hypertension [p=0.011], smoking history [p=0.038], and obesity [p=0.015]). In the analysis of radiologic parameters, however, no significant differences were observed between cystic lesion diameter (5.95±2.76 cm vs. 6.68±4.95 cm, p=0.250), number or laterality (left and/or right) and malignancy. Multivariate analysis identified hypertension, smoking history, and obesity as risk factors for RCCs that were statistically significant predictors of malignancy in complicated renal cysts (Table 2).
Table 2. Comparison of parameter between benign and malignant patients with category II, IIF, III, IV.
| Variable | Benign cyst (n=139) | Malignant cyst (n=82) | p-value | |
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| Clinical parameter | ||||
| Hypertension | 41 (29.3) | 39 (47.7) | 0.011 | 0.013 |
| Smoking | 32 (23.3) | 30 (36.9) | 0.038 | 0.028 |
| Obesity | 42 (30.2) | 37 (45.1) | 0.015 | 0.010 |
| Radiologic parameter | ||||
| Cyst size (cm) | 5.95±2.76 | 6.68±4.95 | 0.250 | 0.250 |
| Coexisting BIII, IV | 0 (0) | 6 (7.3) | - | - |
Values are presented as number (%) or mean±standard deviation.
BIII, Bosniak classification III; BIV, Bosniak classification IV.
Obesity was defined as body mass index >25 kg/m2.
In the study of Bosniak category III patients, the strongest potential predictors of malignancy included hypertension (p=0.018), cystic lesion diameter (6.43±4.98 cm vs. 3.66±2.40 cm, p<0.001) and difference of HU (36±8.7 vs. 61±12.3, p=0.027), whereas smoking history and obesity were not significant. Multivariate analysis identified cystic lesion diameter as the strongest independent predictor of malignancy, followed by hypertension and difference of HU (Table 3).
Table 3. Comparison of parameter between benign and malignant patients with Bosniak category III.
| Variable | Benign cyst (n=44) | Malignant cyst (n=27) | p-value | |
|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||
| Clinical parameter | ||||
| Hypertension | 11 (25.0) | 14 (53.3) | 0.018 | 0.010 |
| Smoking | 17 (37.5) | 9 (33.3) | 0.305 | 0.261 |
| Obesity | 12 (27.3) | 11 (40.7) | 0.478 | 0.336 |
| Radiologic parameter | ||||
| Cyst size (cm) | 6.43±4.98 | 3.66±2.40 | <0.001 | 0.001 |
| Hounsfield unit | 36±8.7 | 61±12.3 | 0.027 | 0.019 |
| Coexisting BIII, IV | 0 (0) | 5 (20.0) | - | - |
Values are presented as mean±standard deviation or number (%).
BIII, Bosniak classification III; BIV, Bosniak classification IV.
Obesity was defined as body mass index >25 kg/m2.
Coexisting cystic lesions of category III and IV were highly likely to cause malignancy, but this was not enough to be statistically significant owing to small numbers of lesions.
DISCUSSION
Previous studies of category IIF and III lesions have demonstrated surprising variability in the rates of malignancy. The malignancy rates of surgically treated category IIF lesions are historically 0%–25% [6], whilst those pertaining to category III lesions are approximately 50% (range, 25%–100%) [2,7]. According to the wide range of malignancy rates, it is evident that a significant proportion of patients will undergo surgery for benign pathologies. In our study, 62% of category III patients had surgery for benign complicated cystic lesions. A weighted average from six cohorts, each including >30 complicated renal cysts, reported 65% of category III lesions to be malignant [6]. However, this study was based on a small number of patients that used various CT protocols, and no randomized controlled trials were conducted to evaluate different approaches for the management of complicated renal cysts. Whilst some reports of clinical characteristics of category IIF and III complicated renal cysts have been published in Western countries [4,8], studies examining renal cyst characteristics in Korea are still required. Since a significant difference to the quality of life of patients and oncological outcomes depend on the Bosniak category, accurate classifications and determination of risk factors for malignancy are regarded as the most important clinical indicators in the treatment of renal cysts [9].
In a meta-analysis of nine retrospective studies, including 521 complex renal cysts, the percentages of malignancy in the different Bosniak classifications was as follows: category I, 1.7% (1 of 57); II, 18.5% (10 of 54); III, 33.0% (109 of 330); and IV, 92.5% (74 of 80) [10]. In our study, the malignancy rates of resected category IIF, III, and IV lesions were 17.1% (7 of 41), 38.0% (27 of 71), and 82.1% (46 of 56) respectively, which are consistent with the results of a number of previously published reports [2,4,10].
In the present study, 20.7% of malignant resected renal cystic lesions were diagnosed as papillary RCCs on histopathological examination. Typically, there are rarely papillary RCCs in cases of complicated renal cysts [4,11]; papillary RCCs are hyperdense and homogeneously enhancing on CT (Fig. 1) [12]. A papillary RCC can occasionally manifest as a cystic mass, which has been attributed to the inherent architecture, or secondary to cystic degeneration and extensive necrosis [13]. It may also occur due to interobserver error (e.g., mistaken for a cystic lesion at the time of imaging interpretation), especially if near water attenuation was measured on a precontrast CT image.
As is the case in other studies, risk factors associated with RCCs (e.g., hypertension, smoking, and obesity) were found to be statistically significant as risk factors of malignancy in complicated renal cysts.
The relationship of size of a complex renal cystic lesion and its malignancy potential has received little attention in the literature. Size is not considered an important feature of the Bosniak classification system, and large cystic lesions are not necessarily more likely to be malignant [14]. In fact, there was no significant difference between cystic lesion diameter and the rate of malignancy in our study.
A recent meta-analysis of nine studies with >30 cases in each, showed that inclusion of category IIF led to a reduction in the proportion of category III cases and, consequently, to a decrease in the number of surgical explorations of benign lesions [6]. However, the limited ability to predict malignancy in category IIF and III lesions mean some patients undergo unnecessary surgery, and a diagnosis of malignancy can be missed.
Although category II and IIF masses are generally surgically explored in our hospital when they progress over time, become symptomatic, or according to the wishes of the patient themselves, for fear of harboring malignancy, 62% of patients with category III masses underwent surgery for benign complicated cystic lesions.
A difficult dilemma in the management of Bosniak IIF and III category lesions is due to the preferential practice of the urologist, who is treating the patient with indeterminate lesions [14], and the radiologist who, in case of doubt, considers the patient to have category III lesions to avoid underdiagnosing malignancy. Consequently, it is important to find strong independent predictors of malignancy in category III cystic masses. In our study of Bosniak category III patients, the strongest potential predictors of malignancy were hypertension, cystic lesion diameter, and difference of HU, whereas, smoking history and obesity were not significant. In the case of smoking and obesity, that study was a retrospective analysis that studied the smoking history and BMI. Therefore, our study will require additional analysis such as smoking pattern, smoking status, visceral obesity and central obesity.
In the multivariate analysis, cystic lesion diameter was the strongest predictor of malignancy. Han et al. have reported that smaller lesion sizes (<2 cm) were more likely to be benign than larger lesions [15]. However, that study was a retrospective analysis that did not perform a multiple-variable analysis because of small sample sizes.
In a recent study by Goenka et al. [8], smaller lesion size was the strongest independent predictor of malignancy in category III lesions. The authors predicted a probability of malignancy by lesion size of 76.1% if the lesion was <5 cm in diameter. In the multivariate analysis of our study, a smaller lesion diameter was also the strongest independent predictor of malignancy (p=0.001). Likewise, according to previous studies where potentially few malignant cystic masses were included, all had slow growth rates in each Bosniak category, and metastasis of the malignant cystic masses was rare [16,17].
In 2006, Benjaminov et al. [11] reported that septal and nodular enhancements had the highest sensitivity and specificity in predicting malignancy at 100% and 86%, respectively. Song et al. [18] reported an enhancement dif ference of 42 HU between the precontrast and corticomedullary phase at the highest enhancement area as being significantly correlated with an increased risk of malignancy (HU, 31.5). Although 27 malignant category III lesions in our present study represent fewer cases than in previous reports, difference of HU was still the strongest independent predictor of malignancy, followed by hypertension. Coexisting cystic lesions of category III and IV, and multiplicity of category III were highly likely malignancy, but in our study were not sufficient to be statistically significant, due to the small number of lesions.
The present study had a few limitations. Although, our study collected data over 14 years, its retrospective nature had a some interobserver variations including performance on a variety of helical and conventional CT scanners, and bias of imaging analysis by various radiologists. Second, this study has an element of selection bias due to the inclusion of only surgically excised cystic lesions. Surgical excision was influenced by clinical and radiological parameters such as age, symptoms, patient wants, criteria of the American Society of Anesthesiologists, and size, progression. Third, the number of lesions classified as category IIF and III were larger than in previous studies, but were still insufficient to be diagnostically definitive. Therefore, our results represent preliminary findings that will need to be confirmed in the future.
CONCLUSIONS
Risk factors of malignancy in complicated renal cyst patients were not different from those published previously. In Bosniak category III lesions, lesion size was the strongest predictor of malignancy, followed by hypertension and HU. Characteristically, the lesion size was smaller than in benign complicated renal cysts, in contrast with other categories. The present study of the strongest independent predictors of malignancy in Bosniak category III lesions may be beneficial for patient counseling, risk stratification, and clinical assessments of the need for surgical treatment or imaging surveillance, in the future.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
References
- 1.Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1–10. doi: 10.1148/radiology.158.1.3510019. [DOI] [PubMed] [Google Scholar]
- 2.Smith AD, Remer EM, Cox KL, Lieber ML, Allen BC, Shah SN, et al. Bosniak category IIF and III cystic renal lesions: outcomes and associations. Radiology. 2012;262:152–160. doi: 10.1148/radiol.11110888. [DOI] [PubMed] [Google Scholar]
- 3.Remzi M, Marberger M. Renal tumor biopsies for evaluation of small renal tumors: why, in whom, and how? Eur Urol. 2009;55:359–367. doi: 10.1016/j.eururo.2008.09.053. [DOI] [PubMed] [Google Scholar]
- 4.O'Malley RL, Godoy G, Hecht EM, Stifelman MD, Taneja SS. Bosniak category IIF designation and surgery for complex renal cysts. J Urol. 2009;182:1091–1095. doi: 10.1016/j.juro.2009.05.046. [DOI] [PubMed] [Google Scholar]
- 5.Israel GM, Bosniak MA. An update of the Bosniak renal cyst classification system. Urology. 2005;66:484–488. doi: 10.1016/j.urology.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Graumann O, Osther SS, Osther PJ. Characterization of complex renal cysts: a critical evaluation of the Bosniak classification. Scand J Urol Nephrol. 2011;45:84–90. doi: 10.3109/00365599.2010.533695. [DOI] [PubMed] [Google Scholar]
- 7.Curry NS, Cochran ST, Bissada NK. Cystic renal masses: accurate Bosniak classification requires adequate renal CT. AJR Am J Roentgenol. 2000;175:339–342. doi: 10.2214/ajr.175.2.1750339. [DOI] [PubMed] [Google Scholar]
- 8.Goenka AH, Remer EM, Smith AD, Obuchowski NA, Klink J, Campbell SC. Development of a clinical prediction model for assessment of malignancy risk in Bosniak III renal lesions. Urology. 2013;82:630–635. doi: 10.1016/j.urology.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Park HS, Jeong KS, Cheon J, Yoon DK, Jeong KB. The clinical significance of Bosniak classification in cystic renal masses : usefulness of preoperative computerized tomography in cystic renal masses. Korean J Urol. 1994;35:498–503. [Google Scholar]
- 10.Warren KS, McFarlane J. The Bosniak classification of renal cystic masses. BJU Int. 2005;95:939–942. doi: 10.1111/j.1464-410X.2005.05442.x. [DOI] [PubMed] [Google Scholar]
- 11.Benjaminov O, Atri M, O'Malley M, Lobo K, Tomlinson G. Enhancing component on CT to predict malignancy in cystic renal masses and interobserver agreement of different CT features. AJR Am J Roentgenol. 2006;186:665–672. doi: 10.2214/AJR.04.0372. [DOI] [PubMed] [Google Scholar]
- 12.Silverman SG, Mortele KJ, Tuncali K, Jinzaki M, Cibas ES. Hyperattenuating renal masses: etiologies, pathogenesis, and imaging evaluation. Radiographics. 2007;27:1131–1143. doi: 10.1148/rg.274065147. [DOI] [PubMed] [Google Scholar]
- 13.Vikram R, Ng CS, Tamboli P, Tannir NM, Jonasch E, Matin SF, et al. Papillary renal cell carcinoma: radiologic-pathologic correlation and spectrum of disease. Radiographics. 2009;29:741–754. doi: 10.1148/rg.293085190. [DOI] [PubMed] [Google Scholar]
- 14.Silverman SG, Israel GM, Herts BR, Richie JP. Management of the incidental renal mass. Radiology. 2008;249:16–31. doi: 10.1148/radiol.2491070783. [DOI] [PubMed] [Google Scholar]
- 15.Han HH, Choi KH, Oh YT, Yang SC, Han WK. Differential diagnosis of complex renal cysts based on lesion size along with the Bosniak renal cyst classification. Yonsei Med J. 2012;53:729–733. doi: 10.3349/ymj.2012.53.4.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kouba E, Smith A, McRackan D, Wallen EM, Pruthi RS. Watchful waiting for solid renal masses: insight into the natural history and results of delayed intervention. J Urol. 2007;177:466–470. doi: 10.1016/j.juro.2006.09.064. [DOI] [PubMed] [Google Scholar]
- 17.Volpe A, Panzarella T, Rendon RA, Haider MA, Kondylis FI, Jewett MA. The natural history of incidentally detected small renal masses. Cancer. 2004;100:738–745. doi: 10.1002/cncr.20025. [DOI] [PubMed] [Google Scholar]
- 18.Song C, Min GE, Song K, Kim JK, Hong B, Kim CS, et al. Differential diagnosis of complex cystic renal mass using multiphase computerized tomography. J Urol. 2009;181:2446–2450. doi: 10.1016/j.juro.2009.01.111. [DOI] [PubMed] [Google Scholar]
- 19.Weibl P, Klatte T, Waldert M, Remzi M. Complex renal cystic masses: current standards and controversies. Int Urol Nephrol. 2012;44:13–18. doi: 10.1007/s11255-010-9864-y. [DOI] [PubMed] [Google Scholar]