Abstract
Bochdalek hernia (BH) is an uncommon form of diaphragmatic hernia. The rarity of this hernia and its nonspecific presentation leads to delay in the diagnosis, with the potential risk of complications. This review summarizes the relevant aspects of its presentation and management, based on the present evidence in the literature. A literature search was performed on PubMed, Google Scholar, and EMBASE for articles in English on BH in adults. All case reports and series from the period after 1955 till January 2015 were included. A total of 180 articles comprising 368 cases were studied. The mean age of these patients was 51 years (range 15-90 years) with a male preponderance of 57% (211/368). Significantly, 6.5% of patients were above 70 years, with 3.5% of these being above 80 years. The majority of the hernias were on the left side (63%), with right-sided hernias and bilateral occurring in 27% and 10%, respectively. Precipitating factors were noted in 24%, with 5.3% of them being pregnant. Congenital anomalies were seen in 11%. The presenting symptoms included abdominal (62%), respiratory (40%), obstructive (vomiting/abdominal distension; 36%), strangulation (26%); 14% of them were asymptomatic (detected incidentally). In the 184 patients who underwent surgical intervention, the surgical approach involved laparotomy in 74 (40.27%), thoracotomy in 50 (27.7%), combined thoracoabdominal approach in 27 (14.6%), laparoscopy in 23 (12.5%), and thoracoscopic repair in 9 (4.89%). An overall recurrence rate of 1.6% was noted. Among these patients who underwent laparoscopic repair, 82% underwent elective procedure; 66% underwent primary repair, with 61% requiring interposition of mesh or reenforcement with or without primary repair. The overall mortality was 2.7%. Therefore, BH should form one of the differential diagnoses in patients who present with simultaneous abdominal and chest symptoms. Minimal access surgery offers a good alternative with short hospital stay and is associated with minimum morbidity and mortality.
Keywords: Bochdalek hernia (BH), congential diaphragmatic hernia (CDH), laparoscopic repair
Introduction
Congenital diaphragmatic hernia (CDH) has an incidence of 1:2000-1:12,500 live births and accounts for 8% of all the major congenital anomalies.[1,2] It is caused by the failure of diaphragmatic closure and usually presents in neonates with respiratory distress. It is associated with 40-50% mortality.[1,2] The commonest CDH is Bochdalek hernia (BH). Adult presentation, however, is rare. The incidence is reported to be 0.17%, with the majority of hernias occurring on the left side.[3] The diagnosis of BH is often difficult to make in adults due to the wide variation in their presenting symptoms and the rarity of this hernial defect.[1,4,5,6,7,8] Several factors that raise the intraabdominal pressure may predispose to it, with pregnancy being the most predominant.[9,10,11,12] While most of these hernias are symptomatic and present with pain or complications such as strangulation,[4,6,8,11,13,14] there are others that are detected incidentally during investigations for another cause.[3,15] Unfortunately, some of these patients are misdiagnosed, leading to serious consequence.[16,17,18,19] Historically these patients have been managed by laparotomy[1,4,5,20,21,22] or thoracotomy,[1,6,23] and primary repair with or without mesh reenforcement was performed. With the expansion of laparoscopic experience in various intraabdominal surgeries, there are several reports now of BH being successfully managed by a laparoscopic approach.[4,7,8,9,10,24,25,26,27,28] This article reviews the literature with regard to the clinical features, complications, predisposing factors, investigations, various surgical approaches, and the feasibility and outcome of laparoscopic approach in patients with BH.
A search was conducted using PubMed, EMBASE, and Google Scholar for every case report, series, and literature review in English relating to BH in adults. Key words included were “congenital diaphragmatic hernia,” “Bochdalek hernia,” and “posterolateral hernia in adults.” All patients aged 15 years and above were considered as adults and were included in the study. The review extended from 1955 to January 2015. The data studied included demographic details, presenting symptoms, predisposing factors (including pregnancy), recurrent hernias, intraoperative findings, various surgical approaches, and laparoscopic surgical procedure and its outcome.
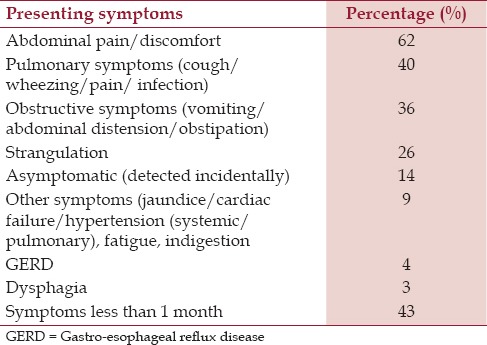
A total of 368 cases of BH were found among the 180 articles studied [Table 1]. Among these, 57% were males, with a mean age of 51 years (range 15-90 years). Eight among these (3.5%) were above 80 years and 7 (3%) were aged 70-80 years. The majority of the BHs were on the left side (63%), with the incidence of right-sided and bilateral hernias being 27% and 10%, respectively [Table 1]. However, one study with 142 cases had lacked some of the details; hence this study predominately deals with 226 cases from 179 articles. Among these 226 patients, precipitating factors was reported in 24%, 5.3% of them being pregnancy. In 11%, congenital anomalies were noted. The most predominant symptoms were abdominal (pain/discomfort) (62%); others included pulmonary symptoms (cough, chest pain, wheezing, infection; 40%), obstructive symptoms (abdominal distension, vomiting, obstipation; 36%), and strangulation (26%); 14% were asymptomatic [Table 2]. Among these 226 patients, 42 (18.8%) did not undergo any procedure (unfit for surgery, too old, or not willing for surgery). Among the remaining 184 patients who underwent surgical intervention, the approach included laparotomy [74 (40.27%)], thoracotomy [50 (27.7%)], combined thoracoabdominal approach [27 (14.6%)], laparoscopy [23 (12.5%)], and thoracoscopic repair [9 (4.89%)]. In those with laparoscopic repair, 82% had elective surgery, with 66% of them being primary repair. Interposition of mesh or mesh reenforcement was required in 61% of them. There was 9% morbidity and no mortality in the laparoscopy group. The mean hospital stay was 4 days.
Table 1.
Literature review (1955-2015) - Demographic details
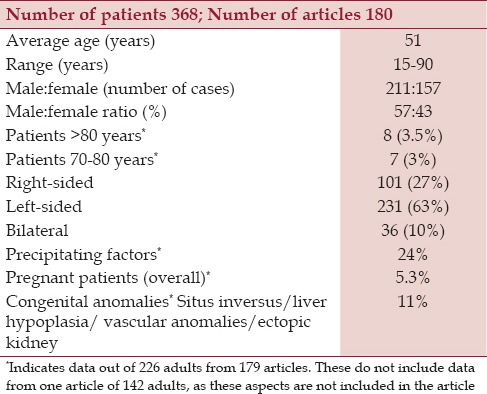
Table 2.
Presenting symptoms and the percentage (226 adults)
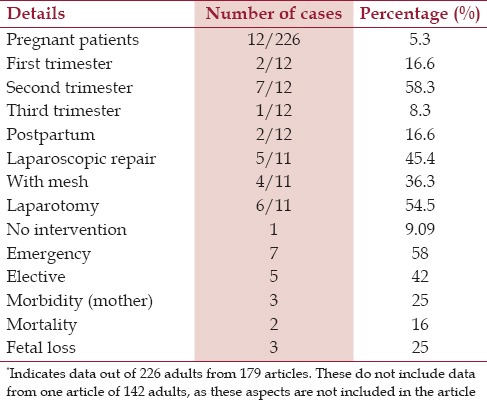
There was overall 2.7% mortality among all the operated cases; 4 deaths, 2 each in the laparotomy and thoracotomy groups. Among the pregnant patients, 58% were treated in the second trimester. The surgical approach for them included laparotomy and laparoscopy in 54.5% and 45.5%, respectively [Tables 3 and 4].
Table 3.
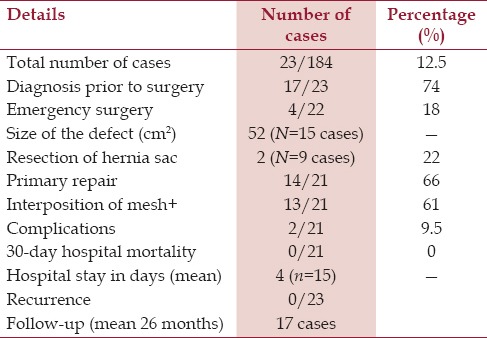
Table 4.
Embryological Cause
Embryologically, the development of diaphragm occurs during the fourth week of gestation, and by the sixth week the pleuroperitoneal folds on the lateral body wall grows medially to fuse with the septum transversum.[1,4,29] The fusions of these two muscle groups, which occur at the final stage of development, are regions anatomically vulnerable to developing hernia.[2,4] BH develops at around 8-10 weeks of gestation at this fibrous lumbocostal trigone, which is the junction of lumbar and costal muscle groups in the posterolateral diaphragm.[2,4,29,30]
CDH has been classified into the following different types: Eventeration of diaphragm, posterolateral hernia of Bochdalek (aka, BH), parasternal hernia of Morgagni-Larrey, pertioneopericardial hernia, and the central tendon hernias.[1,2,4,7,29] BH, which was first described by Bochdalek in 1867, is the commonest of CDH and accounts for 95% of them.[1,2] Unlike BH, Morgagni-Larrey hernia is usually asymptomatic in the neonatal period and may present in adulthood with incarceration.[1,7,30] The defect occurs between the attachment of the diaphragm to the xiphoid process and the seventh costal cartilage. The retroxiphoid space is termed “Larrey's gap” on the left and “Morgagni's gap” on the right side.[1,2,7] Central diaphragmatic hernias are even rarer and involve the central tendinous (amuscular) portion of the diaphragm, with rest of the diaphragmatic musculature being normal.[1,7,29,30]
Incidence and Prevalence
The prevalence of BH in one of the earlier reports (1985) was found to be 6% among the 940 adults studied.[30] However, the incidence of BH in the 13,138 abdominal computed tomographic (CT) scans performed for various chest and abdominal symptoms was reported to be 0.17%.[3] This is similar to other studies, which report an incidence of less than 1%.[13,31] The reasons for the difference between the earlier studies and the later ones are related to selection bias and the possible inclusion of diaphragmatic bosselation due to poor CT resolution in the 1980s.[3] There is a general belief, however, that the incidence of BH is much higher than they were reported earlier.[3,31] This view is supported by two recent reports, where on review of multidimensional computerized tomography (MDCT) images used for the diagnosis of other chest and abdominal pathologies, asymptomatic BH was noted in 10.5% and 12.5% of these patients, respectively.[13,32] The high incidence of BH in these studies has been attributed to the high clarity in the definition of structural abnormality and the present wide use of MDCT in routine practice.[13]
Congenital Anomalies
Congenital anomalies were observed in 11% of the patients studied in this review. These include situs inversus,[1] malrotation,[33,34,35,36] incomplete attachment of the cecum,[31] hepatic hypoplasia,[37,38,39,40] bifid liver,[41] pulmonary hypoplasia,[37] Chilaiditi's syndrome,[42] Marfan syndrome,[43] mitral/tricuspid valve prolapse,[44] patent ductus arteriosus,[45] pulmonary sequestration,[45] Down's syndrome,[46] accessory lung lobe,[47] congenital pulmonary blebs,[48] asplenia, deafness, accessory diaphragm,[49] aberrant systemic artery to right lobe, and anomalous pulmonary vein.[50] In neonates, the pulmonary hypoplasia and pulmonary hypertension that BH is invariably associated with, along with persistent fetal circulation leading to respiratory failure, causes management problems.[5,7] The repair of BH is generally carried out in the neonate period after there is a significant improvement in pulmonary function and reduction in pulmonary hypertension.[7] Laparoscopic repair, however, is not a viable option in neonates because of the risk of pneumperitoneum in an infant who already has compromised respiratory function.[7]
Clinical Details
BH is usually congenital, arising due to failed closure of pleuroperitoneal ducts.[7,29,30] About 5-25% of these are diagnosed beyond 8 weeks of life,[2,51] and about 5% are diagnosed in adults.[1,7,29,30,52] These hernias can thus be acquired in adulthood due to reopening of these ducts following the initial extension of intraabdominal or perirenal fat.[1] The demographics of BH are reported to differ between symptomatic and asymptomatic patients.[4] While some have reported that the right-side defects are larger,[14] others have found no difference in the size between the two sides, being 37 cm2 versus 39 cm2, respectively.[4] Symptomatic BHs are usually left-sided and are less likely on the right side, possibly due to the caudate lobe of the liver compressing the right pleuroperitoneal canal, thus preventing right-sided herniation.[1,4,7,30] Moreover, the right hemidiaphragm is fully formed embryologically before the left.[29,30] The hernial contents include the colon (63%), stomach (40%), omentum (39%), and small bowel (28%). Uncommon contents may include the spleen, tail of pancreas, and the kidney.[4] The right-sided contents are likely to be the liver, kidney, fat and occasionally colon.[1,4,7] The left-sided content includes the stomach, small gut, colon, spleen, tail of pancreas, and kidney.[1,4,7] However, in patients with asymptomatic BH, detected on reviewing the MDCT images performed for other conditions, omental fat as content was noted in 95.5% of the cases. This could possibly indicate the detection of the hernia at an earlier stage.[13] The clinical symptoms of BH are frequently vague and nonspecific and include chest and/or abdominal symptoms.[1,4,7] Moreover, they could be intermittent, as herniated viscera can spontaneously reduce, causing symptom regression.[1,7,8] The majority of these patients in our review (86%) were symptomatic, with abdominal pain (62%) and pulmonary symptoms (40%) being the most commonest.[4] Obstructive symptoms (abdominal distension/vomiting) were observed in 36% of the cases, with strangulation in 26% of them. The other symptoms (9%) with which these patients presented included fatigue, cardiac failure, hypertension, and jaundice. Dysphagia (3%), gastro-esophageal reflux disease (GERD) (4%) were other uncommon symptoms.[4,20] Nearly half of these patients presented acutely, with 43% presenting with symptoms for 1 month or less.[4] Gastric volvulus and obstruction and strangulation of the small or large gut are potential complications, with morbidity in some series being reported in 32% of these cases.[1,53] In addition, gastric reflux and pancreatitis have been noted.[20]
Misdiagnosis
A significant number of these patients with BH are misdiagnosed due to a combination of the rarity of this condition in adults and the varied clinical presentation. The incidence of misdiagnosis has been reported to be 38%.[5] The misdiagnosis includes hydropneumothorax, hemothorax, empyema, pleural effusion, and pneumonia.[16,17,18,19] The consequence of misdiagnosis is a delay in appropriate management, leading to a potential risk of strangulation; some of these unfortunate patients, in whom an intercostal tube is inadvertently placed, could have serious consequences.[4,16,17,18,19] In view of the risk of misdiagnosis, some have suggested to look for additional clues in patients who present with respiratory symptoms and are suspected to have BH.[52] These include:
Abdominal or thoracic symptoms aggravated in the supine position;
Postprandial respiratory symptoms;
Gurgling sounds in the chest with bowel sounds heard on auscultation;
Radiographic abnormalities while supine; and
Abdominal symptoms aggravated by physical effort.
Precipitating Factors
Precipitating factors play a role in the manifestation of BH and have been reported in 25% of these patients.[4] The prime factor is the rise in intraabdominal pressure and may be due to several causes, including persistent coughing/chronic obstructive airway disease (COPD),[37,38] vigorous physical activity, sneezing, chronic constipation,[44] retching, large meals, diving, fits of laughter, pregnancy, and childbirth.[9,10,11,12,52,54,55,56,57,58,59]
Association with Pregnancy
Overall, 5.3% of the adult patients with BH in our review were pregnant.[9,10,11,12,54,55,56,57,58,59,60,61,62] Pregnancy has been found to be the most significant predisposing factor and is seen in 34% of cases where at least one precipitating factor is noted.[4] The management of these patients and the timing of surgical repair with regard to the stage of pregnancy is debatable. In patients who are asymptomatic and are discovered to have BH incidentally during pregnancy, elective hernia repair during the second trimester is advised.[9,33,62] In those patients who present with obstructive symptoms, surgical intervention is carried out irrespective of the stage of pregnancy because of the potential risk of strangulation and its deleterious consequence on both the fetus and the mother.[62] For those that are detected in the third trimester, there are some who would induce labor once fetal maturity is reached and carry out the repair in the postpartum phase.[11,62] There are others who discourage active labor to prevent further herniation of the contents and recommend cesarean section and hernia repair simultaneously.[61] In a review of 34 cases of diaphragmatic hernia in pregnancy (15 traumatic and 11 cases of BH), 66% underwent emergency surgeries, and of them 55% had strangulation.[62] A fetal mortality of 26% (9/34) and maternal death of 14% (5/34) was noted.[62] Only 2 of the maternal deaths were in BH patients and were in those who were treated before 1980. The risk of maternal and fetal mortality in patients with diaphragmatic hernia reflects the seriousness of this hernia in pregnancy and the need for its early identification and prompt treatment.
Recurrence Rate
This review notes recurrence in 3 out of 184 patients (1.6%) of the operated cases.[62,63,64] The initial repairs in these patients were by open thoracic and thoracoabdominal approaches. In addition, the primary repair was reenforced with mesh. No precipitating factors to contribute to their recurrence were observed. The recurrence was repaired by laparotomy with mesh reenforcement (dual and polypropelene each).[62,63,64] The difficulty encountered during the repair included dense adhesions to surrounding structures, including the pericardium. In addition, larger diaphragmatic defects were found. In 1 case there was a near absence of diaphragm, barring a rim of peripheral remnant, due to retraction of the diaphragm.[63,64]
Investigations
An adequate preoperative and intraoperative assessment of the location and the size of defect are critical to the success of BH repair,[3,4,7,8,32] The presence of air meniscus sign on chest x-ray should draw the attention of the clinician to this possible diagnosis. Further radiological investigations may be performed to confirm the diagnosis.[65] BH is often difficult to appreciate on chest x-ray and a previous normal chest x-ray may not exclude BH, as the herniation of content may be intermittent.[66,67] The role of CT as a diagnostic modality in establishing a preoperative diagnosis is well established[68] [Figure 1]. The typical findings on a CT include the presence of fat or soft tissue over the upper surface of the diaphragm, characteristically posterolateral, a mass adjacent to the diaphragmatic defect and a continuous density over and under the diaphragm's discontinuity.[30] However, a preoperative CT or magnetic resonance imaging (MRI) in the usual horizontal plane may not always enable the definitive diagnosis of BH, or reveal the details of the diaphragmatic defect. Hence a reconstructed three-dimensional section on CT or MRI images may be useful to detect the precise diaphragmatic defect and size.[69,70] Of late, MDCT has further enhanced the detection rate and clarity of diaphragmatic abnormality.[13,32] MRI, too, distinctly reveals the discontinuity of the soft tissue lines in the diaphragm on both the sagittal and coronal planes.[70]
Figure 1.

CT scan revealing herniated stomach through a left BH (arrows)
Ultrasound has been reported as a useful initial tool in the work-up of suspected cases of BH.[71] The features that would support the diagnosis include a fragmented diaphragm, inability to view the spleen and kidney within the same plane, and accordion-like spleen.[71] In view of the association of congenital anomalies of the gut with the possibility of volvulus of herniated stomach, some recommend a barium series prior to surgical intervention.[4] This is of particular importance if one were to consider thoracoscopic approach for repair.[72] The presence of malrotation or volvulus would warrant an abdominal approach.[4,7,68,73] Several other investigations may play a role in preoperative preparation of these patients, particularly in those with respiratory symptoms. These may include fluoroscopy, bronchogram, and pulmonary angiography.[49]
Repair
The first successful surgical repair of BH was performed in 1901.[61] Historically these patients were managed either by an open transabdominal or by a transthoracic approach. However, with the expansion of laparoscopic[4,7,8,9,10,12,24,25,26,27,28] and thoracoscopic[74,75,76,77,78,79,80,81,82,83,84,85] expertise and advances in instruments, the minimally invasive approach has emerged as an attractive option. There are, however, several areas of debate and these include the following:
Should all patients with BH be operated irrespective of whether they are symptomatic or asymptomatic (detected incidentally on investigations);
Should it be an open or laparoscopic/thoracoscopic approach;
Should the sac be excised;
Should a mesh be used to reenforce the repair, and if so, when; and
The method of fixation of mesh.
Most agree that all fit patients who are symptomatic and even those who are asymptomatic and detected incidentally should undergo surgical repair.[1,5,8,10,12,27,60] The argument in favor of such an approach is that a significant number of these patients present acutely with serious complications such as strangulation of the gut, leading to severe morbidity and mortality.[4,12,27,61]
The approach to repair of BH depends on the presentation (emergency or elective), size and side of the defect, and the presence of complications.[4,5,8,10,76,77,78,79,80] For emergent cases, laparotomy is the favored approach, using either a midline or subcostal, or in difficult cases a thoracoabdominal, incision.[4,7,8,41,79] This achieves better visualization of diaphragm on the left side and on the right side; the same is achieved following the mobilization of the right lobe of the liver.[1,81,82] Laparotomy has the advantage of identifying the position of the viscera after the “pull back” of hernia content and repairing the malrotation, if any.[1,50] Dissection of the sac is associated with a high risk of pleural injury and hence most of the surgeons prefer to leave the hernia sac in place.[23,27] The development of a seroma in the remnant sac is a potential risk; however, it has been reported that the remnant sac completely disappears 30 days following surgery.[83]
The superiority of thoracotomy, however, lies in separating the herniated organs from the thoracomediastinal viscera under direct vision before “push back” of contents is performed.[21,22,62] A combined thoracoabdominal approach is undertaken in difficult cases, where a large volume of hernia contents is noted and when dense adhesions are expected, as in recurrent hernias.[6,18,62,84] Small defects are easier to repair, whereas larger defects may involve the reduction of a large amount of intraabdominal contents.[1,4,7,8,10] The defect is usually repaired along a “transverse axis” and may require the use of mesh in the absence of contamination.[4,82] There are no data favoring interrupted over running sutures, permanent over absorbable, or two-layer over single-layer closure.[6] Generally, nonabsorbable braided sutures in either interrupted or continuous fashion is advocated, based on the size and location of the defect.[6] Suturing the defect is important for the restoration of the anatomy between the thoracic and abdominal cavities.[4,23,24,82]
The mesh reenforcement of the repair depends on the defect size. While there are some who recommend the use of mesh for a defect larger than 20-30 cm,[28] there are others who use it in defects of 8 cm size[5,27] or when the defect is more than 25 cm2.[86] Many surgeons prefer to repair most hernias with prosthetic graft reenforcement because of the continuing stress on the diaphragm that results from respiratory movements and cardiac motions.[23] The use of mesh to a certain extent may achieve a tensionless repair of the defect.[23] A primary closure may not be possible in 53% of the cases and hence those cases will obviously require repair with mesh.[87] Many types of mesh are available for use in these types of repair. Polypropylene mesh has the benefit of providing indefinite support and excellent tissue growth. However, the concern of erosion of the mesh into the gastrointestinal organs represents a theoretical risk.[23] The decreased tendency for adhesion formation between polytetrafluroethylene and other types of dual mesh make them more desirable.[23,26,27] Fixation of prosthesis can be achieved by intracorporeal suture or mechanical fixation devices such the endostaplers.[27] Surgeons should take great care during the fixation of mesh with laparoscopic tacker where the diaphragm is relatively thin and in close proximity to the pericardium.[23] Following surgery, while some would place an intercostal drainage tube to drain the chest,[61,85,88,89,90,91,92,93] others would manage with transabdominal suction catheter to evacuate the thorax, just before deflation of the abdomen following the repair.[4]
Laparoscopic Repair
Usually, a minimally invasive technique is used in an elective setting, though rarely for emergency cases. A laparoscopic approach was used in 82% of elective cases in our review. Laparoscopic repair is carried out by some, by placing the patient in lateral decubitus, reverse Trendelenburg position,[4,93,94] while others would perform the procedure with the patient in the supine position.[23,26,27] The lateral decubitus position has been reported to be particularly beneficial in pregnant patient undergoing BH repair.[62] A 30-degree or 45-degree scope is desirable for adequate visualization of the diaphragm and the defect.[6] While the laparoscopic approach is avoided in the presence of strangulation, there are reports of such surgeries being carried out in patients with incarcerated hernias, following the opening up of the diaphragm defect radially to reduce the viscera.[23,25] Patients with gangrenous gut would require extensive resection of hernia contents and reconstruction.[25,95] Minimally invasive techniques have been reported to result in reduced morbidity and might also improve the ease of hernia reduction, hemostasis, and adhesiolysis[5,7,8,23,24,25,67] [Figure 2]. The distinct advantages of laparoscopy noted in this review are low morbidity (9%), no mortality, and short hospital stay (of 4 days). There has been a constant increase in cases where the laparoscopic approach was opted for in the management of BH in recent years.[4]
Figure 2.
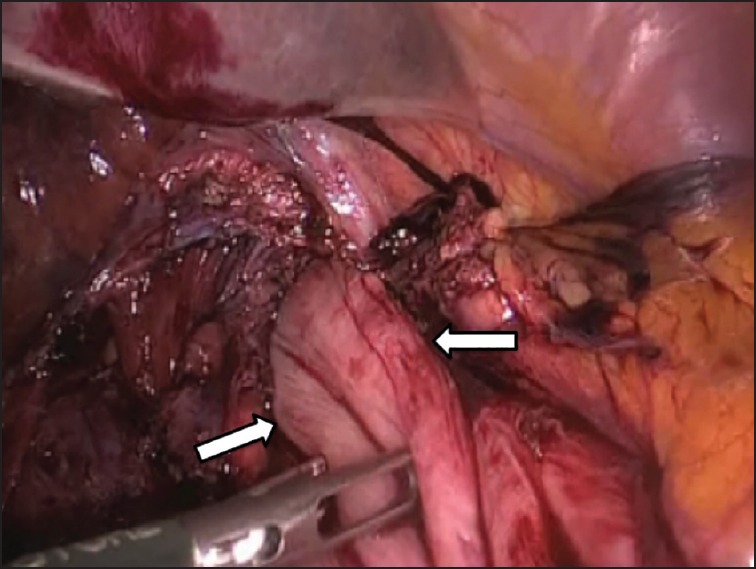
Laparoscopic view of reducing the herniated stomach from the chest in a patient with left BH (arrows)
The thoracoscopic approach for the repair of BH has been advocated by some.[74,75,76] The distinct advantages of this approach are that it is minimally invasive and allows for the release of adhesions between the herniated viscera and thoracomediastinal structures under direct vision, before reducing them into the abdominal cavity.[74,75,76] The thoracic cavity and the herniated organ can be examined in detail for ischemic changes, necrosis, or perforation before reduction. Moreover, repair of the hernia on the right side will be relatively easier, as the liver would not be obscuring the view.[74] The concern, however, is that it may be difficult to manipulate the herniated organs into the abdomen, and in case of the spleen there may be a potential risk of bleeding while doing so.[73,74] The reduction is facilitated by the reverse Trendelenburg position and CO2 insufflation into the thoracic cavity.[74] The abdominal cavity is inspected through the defect by thoracoscope to ensure safe placement of the herniated organ without malrotation.[79] Some patients undergo minithoracotomy for placement of mesh.[74,75,76]
Due to the absence of randomized controlled studies comparing the thoracic and abdominal approaches and the open and minimally invasive approaches, the choice of repair is left entirely to the indvidual surgeon's discretion. This choice is influenced by his/her past experience with minimal access surgery and the circumstances under which the surgery is performed (elective or emergency),[23] and by the presence of complications. Preferably, surgical repair is performed in an elective setting and is the treatment of choice. This is reflected in the results, e.g., in one series, while the mortality of elective surgery was 5%, that following emergency surgery was significantly higher at 32%.[83]
Intraoperative and Postoperative Complications
Pneumothorax has been recognized as a potential complication during laparoscopic diaphragm defect repair.[6] Laparoscopic repair of traumatic diaphragmatic injury presents the greatest risk, with a reported risk of tension pneumothorax in 0.8% of the cases.[94] Usually when present, the symptoms of pneumothorax are minimal and can be deal with by lowering the insufflation pressure and adding positive end-expiratory pressure.[6] Patients with persistent pneumothorax would need intercostal tube insertion in the postoperative period.[6] The risk of pneumothorax, however, is minimal in patients with chronic diaphragmatic hernia, possibly due to the presence of intrathoracic adhesions and the presence of sac.
Potential complications also include injury to gut including perforation and bleeding while reducing and handling an oedematous gut.[95,96] Moreover disruption of the spleen with bleeding or injury to the tail of pancreas during manipulation could also result.[74]
If large hernias are reduced, it is crucial to monitor postoperatively for abdominal compartment syndrome (ACS).[21] A firm tense abdomen, increased peak inspiratory pressure, and oliguria in the immediate postoperative period should raise concerns.[21] In one such patient who underwent BH repair for incarcerated hernia, ACS in the postoperative period was complicated with empyema, gastropleural fistula, and sepsis, requiring multiple surgeries and a hospital stay of 11 months.[21] Among the long-term complications, gastroesophageal reflux has been reported to be a potential complication after CDH repair.[97,98] The role of antireflux procedure during the repair of hernia in these patients, however, is debatable.[26,97,98]
The overall 30-day mortality was 2.7% (2% among the patients who underwent laparotomy[4] and 5% of the patients who underwent thoracotomy), and there was no reported mortality among the patients who underwent thoracoscopic or laparoscopic repair.[4] This may reflect selection bias, as the more complicated cases would have undergone an open approach.
Conclusion
BH is an uncommon form of diaphragmatic hernia. The recent literature, however, indicates a slightly increased prevalence of BH, with most being asymptomatic. It is pertinent for clinicians to be aware of this entity, particularly in patients who present with combined abdominal and thoracic symptoms. CT and MRI are useful diagnostic tools. Pregnancy is a significant predisposing factor and when BH is found incidentally in pregnant cases, it may warrant an elective repair, preferably in the second trimester. A significant number of these patients present acutely with complications. While in the past an open approach with primary repair and mesh reenforcement was the norm, there is a constant increase in the reports of these being performed laparoscopically, with the associated well-established benefits.
Financial support and sponsorship
Nil.
Conflicts of interest
There is no conflict of interest in publishing this article.
References
- 1.Gedik E, Tuncer MC, Onat S, Avci A, Tacyildiz I, Bac B. A review of Morgagni and Bochdalek hernias in adults. Folia Morphol (Warsz) 2011;70:5–12. [PubMed] [Google Scholar]
- 2.Newman BM, Afshani E, Karp MP, Jewett TC, Jr, Cooney DR. Presentation of congenital diaphragmatic hernia past the neonatal period. Arch Surg. 1986;121:813–6. doi: 10.1001/archsurg.1986.01400070079017. [DOI] [PubMed] [Google Scholar]
- 3.Brown SR, Horton JD, Trivette E, Hofmann LJ, Johnson JM. Bochdalek hernia in the adult: Demographics, presentation, and surgical management. Hernia. 2011;15:23–30. doi: 10.1007/s10029-010-0699-3. [DOI] [PubMed] [Google Scholar]
- 4.Thomas S, Kapur B. Adult Bochdalek hernia-clinical features, management and results of treatment. Jpn J Surg. 1991;21:114–9. doi: 10.1007/BF02470876. [DOI] [PubMed] [Google Scholar]
- 5.Slesser AA, Ribbans H, Blunt D, Stanbridge R, Buchanan GN. A spontaneous adult right-sided Bochdlaek hernia containing perforated colon. JRSM Short Rep. 2011;2:54. doi: 10.1258/shorts.2011.011056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thoman DS, Hui T, Phillips EH. Laparoscopic diaphragmatic hernia repair. Surg Endosc. 2002;16:1345–49. doi: 10.1007/s00464-001-8162-2. [DOI] [PubMed] [Google Scholar]
- 7.Wadhwa A, Surendra JB, Sharma A, Khullar R, Soni V, Baijal M, et al. Laparoscopic repair of diaphragmatic hernias: Experience of six cases. Asian J Surg. 2005;28:145–50. doi: 10.1016/S1015-9584(09)60281-5. [DOI] [PubMed] [Google Scholar]
- 8.Palanivelu C, Rangarajan M, Senthilkumaran S, Parthasarathi R. Safety and efficacy of laparoscopic surgery in pregnancy: Experience of a single institution. J Laparoendosc Adv Surg Tech A. 2007;17:186–90. doi: 10.1089/lap.2006.0037. [DOI] [PubMed] [Google Scholar]
- 9.Debergh I, Fierens K. Laparoscopic repair of a Bochdalek hernia with incarcerated bowel during pregnancy: Report of a case. Surg Today. 2014;44:753–6. doi: 10.1007/s00595-012-0441-0. [DOI] [PubMed] [Google Scholar]
- 10.Islah MA, Jiffre D. A rare case of incarcerated bochdlaek hernia in a pregnant lady. Med J Malaysia. 2010;65:75–6. [PubMed] [Google Scholar]
- 11.Kocakusak A, Arikan S, Senturk O, Yucel AF. Bochdalek's hernia in an adult with colon necrosis. Hernia. 2005;9:284–7. doi: 10.1007/s10029-004-0302-x. [DOI] [PubMed] [Google Scholar]
- 12.Owen ME, Rowley GC, Tighe MJ, Wake PN. Delayed diagnosis of infarcted small bowel due to right-sided Bochdalek hernia. Ann R Coll Surg Engl. 2007;89:W1–2. doi: 10.1308/147870807X160407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Temizöz O, Gençhellaç H, Yekeler E, Umit H, Unlü E, Ozdemir H, et al. Prevalence and MDCT characteristics of asymptomatic Bochdalek hernia in adult population. Diagn Interv Radiol. 2010;16:52–5. doi: 10.4261/1305-3825.DIR.2750-09.1. [DOI] [PubMed] [Google Scholar]
- 14.Somani SK, Gupta P, Tandon S, Sonkar D, Bhatnagar S, Saxena M. Bochdalek diaphragmatic hernia masquerading as tension hydropneumothorax in an adult. J Thorac Cardiovasc Surg. 2010;141:300–1. doi: 10.1016/j.jtcvs.2009.11.062. [DOI] [PubMed] [Google Scholar]
- 15.Dhaka ES, Hasan MI, Mutatkar KK, Sapra ML. Strangulated diaphragmatic hernia simulating hydropneumothorax (case report) J Assoc Physicians India. 1979;27:777–9. [PubMed] [Google Scholar]
- 16.Dalton AM, Hodgson RS, Crossley C. Bochdalek hernia masquerading as a tension pneumothorax. Emerg Med J. 2004;21:393–4. doi: 10.1136/emj.2002.004697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Novakov IP, Paskalev G. Adult bochdalek hernia simulating left pleural effusion: A review and case report. Folia Med (Plovdiv) 2010;52:62–6. doi: 10.2478/v10153-010-0019-9. [DOI] [PubMed] [Google Scholar]
- 18.Soylu E, Junnarkar S, Kocher HM. Recurrent indigestion in a young adult. Case Rep Gastroenterol. 2010;4:518–23. doi: 10.1159/000322871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones HG, Kadhim A, Nutt M. Congenital diaphragmatic hernia: An unusual cause of obstructive jaundice. Ann R Coll Surg Engl. 2012;94:e8–9. doi: 10.1308/003588412X13171221499180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suzuki T, Okamoto T, Hanyu K, Suwa K, Ashizuka S, Yanaga K. Repair of Bochdalek hernia in an adult complicated by abdominal compartment syndrome, gastropleural fistula and pleural empyema: Report of a case. Int J Surg Case Rep. 2014;5:82–5. doi: 10.1016/j.ijscr.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou Y, Du H, Che G. Giant congenital diaphragmatic hernia in an adult. J Cardiothorac Surg. 2014;9:31–3. doi: 10.1186/1749-8090-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Toydemir T, Akinci H, Tekinel M, Suleyman E, Acunas B, Yerdel MA. Laparoscopic repair of an incarcerated bochdalek hernia in an elderly man. Clinics (Sao Paulo) 2012;67:199–201. doi: 10.6061/clinics/2012(02)20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamid KS, Rai SS, Rodriguez JA. Symptomatic Bochdalek hernia in an adult. JSLS. 2010;14:279–81. doi: 10.4293/108680810X12785289144719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vega MT, Maldonado RH, Vega GT, Vega AT, Liévano EA, Velázquez PM. Late-onset congenital diaphragmatic hernia: A case report. Int J Surg Case Rep. 2013;4:952–4. doi: 10.1016/j.ijscr.2013.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ayiomamitis GD, Stathakis PCh, Kouroumpas E, Avraamidou A, Georgiades P. Laparoscopic repair of congenital hernia complicated with sliding hiatal hernia with reflux in adult. Int J Surg Case Rep. 2012;3:597–600. doi: 10.1016/j.ijscr.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dente M, Bagarani M. Laparoscopic dual mesh repair of a diaphragmatic hernia of Bochdalek in a symptomatic elderly patient. Updates Surg. 2010;62:125–8. doi: 10.1007/s13304-010-0022-y. [DOI] [PubMed] [Google Scholar]
- 27.Schumpelick V, Steinau G, Schluper I, Prescher A. Surgical embryology and anatomy of the diaphragm with surgical applications. Surg Clin North Am. 2000;80:213–39, xi. doi: 10.1016/s0039-6109(05)70403-5. [DOI] [PubMed] [Google Scholar]
- 28.Skandalakis JE, Gray SW, Rowe JS, Jr, Skandalakis LJ. Surgical anatomy of the diaphragm. In: Nyhus LM, Baker RJ, editors. Mastery of Surgery. second ed. Boston: Little Brown and co; 1992. pp. 649–70. [Google Scholar]
- 29.Gale ME. Bochdalek hernia: Prevalence and CT characteristics. Radiology. 1985;156:449–52. doi: 10.1148/radiology.156.2.4011909. [DOI] [PubMed] [Google Scholar]
- 30.Fine R, Borrero E, Stone A. Bochdalek hernia in adulthood. N Y State J Med. 1987;87:516–8. [PubMed] [Google Scholar]
- 31.Salacin S, Alper B, Cekin N, Gulmen MK. Bochdalek hernia in adulthood: A review and an autopsy case report. J Forensic Sci. 1994;39:1112–6. [PubMed] [Google Scholar]
- 32.Kinoshita F, Ishiyama M, Honda S, Matsuzako M, Oikado K, Kinoshita T, et al. Late-presenting posterior transdiaphragmatic (Bochdalek) hernia in adults: Prevalence and MDCT characteristics. J Thorac Imaging. 2009;24:17–22. doi: 10.1097/RTI.0b013e31818c6bc8. [DOI] [PubMed] [Google Scholar]
- 33.Abdullah M. Congenital diaphragmatic hernia in a post-partum woman. Med J Malaysia. 2003;58:99–101. [PubMed] [Google Scholar]
- 34.Fisichella PM, Perretta S, Di Stefano A, Di Carlo I, La Greca G, Russello D, et al. Chronic liver herniation through a right Bochdalek hernia with acute onset in adulthood. Ann Ital Chir. 2001;72:703–5. [PubMed] [Google Scholar]
- 35.Pearson S. Strangulated diaphragmatic hernia; report of four cases. AMA Arch Surg. 1953;66:155–66. doi: 10.1001/archsurg.1953.01260030168004. [DOI] [PubMed] [Google Scholar]
- 36.Court FG, Wemyss-Holden SA, Maddern GJ. Postoperative colonic perforation in a right-sided congenital diaphragmatic hernia in an adult. Int Surg. 2003;88:9–11. [PubMed] [Google Scholar]
- 37.Alam A, Chander BN. Adult Bochdalek hernia. Med J Armed Forces India. 2005;61:284–6. doi: 10.1016/S0377-1237(05)80177-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rimpilainen J, Kariniemi J, Wiik H, Biancari F, Juvonen T. Post-traumatic herniation of the liver, gallbladder, right colon, ileum, and right ovary through a Bochdalek hernia. Eur J Surg. 2002;168:646–7. doi: 10.1080/11024150201680014. [DOI] [PubMed] [Google Scholar]
- 39.Zenda T, Kaizaki C, Mori Y, Miyamoto S, Horichi Y, Nakashima A. Adult right-sided Bochdalek hernia facilitated by coexistent hepatic hypoplasia. Abdom Imaging. 2000;25:394–6. doi: 10.1007/s002610000021. [DOI] [PubMed] [Google Scholar]
- 40.Daver GB, Bakhshi GD, Patil A, Ellur S, Jain M, Daver NG. Bifid liver in a patient with diaphragmatic hernia. Indian J Gastroenterol. 2005;24:27–8. [PubMed] [Google Scholar]
- 41.Kanazawa A, Yoshioka Y, Inoi O, Murase J, Kinoshita H. Acute respiratory failure caused by an incarcerated right-sided adult Bochdalek hernia: Report of a case. Surg Today. 2002;32:812–5. doi: 10.1007/s005950200156. [DOI] [PubMed] [Google Scholar]
- 42.Barakat MJ, Vickers JH. Necrotic gangrenous intrathoracic appendix in a marfanoid adult patient: A case report. BMC Surg. 2005;5:4. doi: 10.1186/1471-2482-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bujanda L, Larrucea I, Ramos F, Muñoz C, Sánchez A, Fernández I. Bochdalek's hernia in adults. J Clin Gastroenterol. 2001;32:155–7. doi: 10.1097/00004836-200102000-00013. [DOI] [PubMed] [Google Scholar]
- 44.Ketonen P, Mattila SP, Harjola PT, Jarvinen A, Mattila T. Congenital posterolateral diaphragmatic hernia in the adult. Acta Chir Scand. 1975;141:628–32. [PubMed] [Google Scholar]
- 45.Shimizu T, Hira S, Hirooka S, Yonekura T, Tamai H. Late onset of right Bochdalek's hernia with strangulation of the omentum. Acta Paediatr. 2002;91:483–5. doi: 10.1080/080352502317371760. [DOI] [PubMed] [Google Scholar]
- 46.Abu-Zikry A, Fahmy AR. Diaphragmatic hernia. J Egypt Med Assoc. 1970;53:617–48. [PubMed] [Google Scholar]
- 47.Michelson E. Congenital diaphragmatic hernia in the adult. A new technique in the closure of the Bochdalek Hernia. J Thorac Cardiovasc Surg. 1960;39:238–45. [Google Scholar]
- 48.Harrington DK, Curran FT, Morgan I, Yiu P. Congenital Bochdalek hernia presenting with acute pancreatitis in an adult. J Thorac Cardiovasc Surg. 2008;135:1396–7. doi: 10.1016/j.jtcvs.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 49.Ikeda T, Ishihara T, Yoshimatsu H, Kikuchi K, Yamazaki S, Hatakeyama T, et al. Accessory diaphragm associated with congenital posterolateral diaphragmatic hernia, aberrant systemic artery to the right lower lobe, and anomalous pulmonary vein. Review and report of a case. J Thorac Cardiovasc Surg. 1972;64:18–25. [PubMed] [Google Scholar]
- 50.Robb BW, Reed MF. Congenital diaphragmatic hernia presenting as splenic rupture in an adult. Ann Thorac Surg. 2006;81:e9–10. doi: 10.1016/j.athoracsur.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 51.Mullins ME, Stein J, Saini SS, Mueller PR. Prevalence of incidental Bochdalek's hernia in a large adult population. AJR Am J Roentgenol. 2001;177:363–6. doi: 10.2214/ajr.177.2.1770363. [DOI] [PubMed] [Google Scholar]
- 52.Fingerhut A, Baillet P, Oberlin PH, Ronat R. More on congenital diaphragmatic hernia in the adult. Int Surg. 1984;69:182–3. [PubMed] [Google Scholar]
- 53.Perhoniemi V, Helminen J, Luosto R. Posterolateral diaphragmatic hernia in adults – Acute symptoms, diagnosis and treatment. Case report. Scand J Thorac Cardiovasc Surg. 1992;26:225–7. doi: 10.3109/14017439209099082. [DOI] [PubMed] [Google Scholar]
- 54.Kurzel RB, Naunheim KS, Schwartz RA. Repair of symptomatic diaphragmatic hernia during pregnancy. Obstet Gynecol. 1988;71:869–71. [PubMed] [Google Scholar]
- 55.Senkyrik M, Lata J, Husová L, Díte P, Husa P, Horálek F, et al. Unusual Bochdalek hernia in puerperium. Hepatogastroenterology. 2003;50:1449–51. [PubMed] [Google Scholar]
- 56.Genc MR, Clancy TE, Ferzoco SJ, Norwitz E. Maternal congenital diaphragmatic hernia complicating pregnancy. Obstet Gynecol. 2003;102:1194–6. doi: 10.1016/s0029-7844(03)00680-x. [DOI] [PubMed] [Google Scholar]
- 57.Flood JL. Foramen of Bochdalek hernia in pregnancy. J Indiana State Med Assoc. 1963;56:32–4. [PubMed] [Google Scholar]
- 58.Hamoudi D, Bouderka MA, Benissa N, Harti A. Diaphragmatic rupture during labor. Int J Obstet Anesth. 2004;13:284–6. doi: 10.1016/j.ijoa.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 59.Rajasingam D, Kakarla A, Jones A, Ash A. Strangulated congenital diaphragmatic hernia with partial gastric necrosis: A rare cause of abdominal pain in pregnancy. Int J Clin Pract. 2007;61:1587–9. doi: 10.1111/j.1742-1241.2005.00763.x. [DOI] [PubMed] [Google Scholar]
- 60.Barbetakis N, Efstathiou A, Vassiliadis M, Fessatidis I. Congenital diaphragmatic hernia as a cause of cardiorespiratory failure and visceral obstruction in late pregnancy. J Gastrointestin Liver Dis. 2006;15:185–8. [PubMed] [Google Scholar]
- 61.Palanivelu C, Rangarajan M, Maheshkumaar GS, Parthasarathi R. Laparoscopic mesh repair of a Bochdalek diaphragmatic hernia with acute gastric volvulus in a pregnant patient. Singapore Med J. 2008;49:e26–8. [PubMed] [Google Scholar]
- 62.Julien F, Drolet S, Levesque I, Bouchard A. The right lateral position for laparoscopic diaphragmatic hernia repair in pregnancy: Technique and review of the literature. J Laproendosc Adv Surg Tech A. 2011;21:67–70. doi: 10.1089/lap.2010.0461. [DOI] [PubMed] [Google Scholar]
- 63.Stephenson BM, Stamatakis JD. Late recurrence of a congenital diaphragmatic hernia. Case report. Br J Obstet Gynaecol. 1991;98:110–1. doi: 10.1111/j.1471-0528.1991.tb10324.x. [DOI] [PubMed] [Google Scholar]
- 64.Sathyanarayana N, Rao RM, Rai SB. An adult recurrent diaphragmatic hernia with near complete defect: A rare scenario. J Clin Diagn Res. 2012;6:1574–6. doi: 10.7860/JCDR/2012/4314.2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Moldovan B, Biris P, Pocreata D, Vasile S, Cimpeanu L, Jeder O, et al. Recurrent left Bockdalek hernia in adult, a rare cause of subocclusive syndrome. Chirurgia (Bucur) 2013;108:116–9. [PubMed] [Google Scholar]
- 66.Katz AS, Naidech HJ, Malhotra P. The air meniscus as a radiographic finding: A review of the literature and presentation of nine unusual cases. CRC Crit Rev Diagn Imaging. 1978;11:167–83. [PubMed] [Google Scholar]
- 67.Kubota K, Yamaguchi H, Kawahara M, Kaminishi M. Bochodalek hernia in a young adult: Report of a case. Surg Today. 2001;31:322–4. doi: 10.1007/s005950170152. [DOI] [PubMed] [Google Scholar]
- 68.Heaton ND, Adam G, Howard ER. The late presentation of postero-lateral congenital diaphragmatic hernias. Postgrad Med J. 1992;68:445–8. doi: 10.1136/pgmj.68.800.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shin MS, Mulligan SA, Baxley WA, Ho KJ. Bochdalek hernia of diaphragm in the adult. Diagnosis by computed tomography. Chest. 1987;92:1098–101. doi: 10.1378/chest.92.6.1098. [DOI] [PubMed] [Google Scholar]
- 70.Yamana D, Ohba S. Three-dimensional image of Bochdalek diaphragmatic hernia; a case report. Radiat Med. 1994;12:39–41. [PubMed] [Google Scholar]
- 71.Sugimura A, Kikuchi J, Satoh M, Ogata M, Inoue H, Takishima T. Bilateral Bochdalek hernias in an elderly patient diagnosed by magnetic resonance imaging. Intern Med. 1992;31:281–3. doi: 10.2169/internalmedicine.31.281. [DOI] [PubMed] [Google Scholar]
- 72.Megremis SD, Segkos NI, Gavridakis GP, Mattheakis MG, Kehayas EG, Triantafyllou LB, et al. Sonographic appearance of a late-diagnosed left Bochdalek hernia in a middle-aged woman: Case report and review of the literature. J Clin Ultrasound. 2005;33:412–7. doi: 10.1002/jcu.20158. [DOI] [PubMed] [Google Scholar]
- 73.Silen ML, Canvasser DA, Kurkchubasche AG, Andrus CH, Naunheim KS. Video-assisted thoracic surgical repair of a foramen of Bochdalek hernia. Ann Thorac Surg. 1995;60:448–50. doi: 10.1016/0003-4975(95)00100-y. [DOI] [PubMed] [Google Scholar]
- 74.Nakashima S, Watanabe A, Hashimoto M, Mishina T, Obama T, Higami T. Advantages of video-assisted thorocoscopic surgery for adult congenital hernia with severe adhesions: Report of two cases. Ann Thorac Cardiovasc Surg. 2011;17:185–9. doi: 10.5761/atcs.cr.09.01528. [DOI] [PubMed] [Google Scholar]
- 75.Tokumoto N, Tanabe K, Yamamoto H, Suzuki T, Miyata Y, Ohdan H. Thorocoscopic-assisted repair of a bochdlaek hernia in an adult: A case report. J Med Case Rep. 2010;4:366. doi: 10.1186/1752-1947-4-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Frisoni R, Germain A, Ayav A, Brunaud L, Bresler L. Thorocoscopic treatment of a right Bochdalek hernia in an adult (with video) J Visc Surg. 2014;151:239. doi: 10.1016/j.jviscsurg.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 77.Salústio R, Nabais C, Paredes B, Sousa FV, Porto E, Fradique C. Association of intestinal malrotation and Bochdalek hernia in an adult: A case report. BMC Res Notes. 2014;7:296. doi: 10.1186/1756-0500-7-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Karamustafaoglu YA, Yoruk Y, Kuzucuoglu M, Yanik F. Massive Bochdalek diaphragmatic hernia in adult with hypoplastic lung. Asian Cardiovasc Thorac Ann. 2015;23:461–3. doi: 10.1177/0218492314532107. [DOI] [PubMed] [Google Scholar]
- 79.Jubber I, Madani Y, Yousaf S, Jubber A. Bochdalek hernia causing type II respiratory failure in an elderly patient. BMJ Case Rep 2014. 2014 doi: 10.1136/bcr-2014-203915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Losanoff JE, Sauter ER. Congenital posterolateral diaphragmatic hernia in an adult. Hernia. 2004;8:83–5. doi: 10.1007/s10029-003-0166-5. [DOI] [PubMed] [Google Scholar]
- 81.Rout S, Foo FJ, Hayden JD, Guthrie A, Smith AM. Right-sided Bochdalek hernia obstructing in an adult: Case report and review of the literature. Hernia. 2007;11:359–62. doi: 10.1007/s10029-007-0188-5. [DOI] [PubMed] [Google Scholar]
- 82.Costa Almeida CE, Reis LS, Almeida CM. Adult right-sided Bochdalek hernia with ileo-cecal appendix: Almieda-Reis hernia. Int J Surg Case Rep. 2013;4:778–81. doi: 10.1016/j.ijscr.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kumar A, Maheshwari V, Ramakrishnan TS, Sahu S. Caecal perforation with faecal peritonitis- unusual presentation of Bochdalek hernia in an adult: A case report and review of literature. World J Emerg Surg. 2009;4:16. doi: 10.1186/1749-7922-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mullins ME, Saini S. Imaging of incidental Bochdalek hernia. Semin Ultrasound CT MR. 2005;26:28–36. doi: 10.1053/j.sult.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 85.Choi YK, Ahn JH, Kim KC, Won TH. An adult right-sided Bochdalek hernia accompanied with hepatic hypoplasia and inguinal hernia. Korean J Thorac Cardiovasc Surg. 2012;45:348–50. doi: 10.5090/kjtcs.2012.45.5.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lucas CE, Ledgerwood AM. Diaphragmatic injury. I. In: Cameron JL, editor. Current Surgical Therapy. St. Louis: Mosby; 1998. pp. 944–47. [Google Scholar]
- 87.Ninos A, Felekouras E, Douridas G, Ajazi E, Manataki A, Pierrakakis S, et al. Congenital diaphragmatic hernia complicated by tension gastrothorax during gastroscopy: Report of a case. Surg Today. 2005;35:149–52. doi: 10.1007/s00595-004-2875-5. [DOI] [PubMed] [Google Scholar]
- 88.Harinath G, Senapati PS, Pollitt MJ, Ammori BJ. Laparoscopic reduction of an acute gastric volvulus and repair of a hernia of Bochdalek. Surg Laparosc Endosc Percutan Tech. 2002;12:180–3. doi: 10.1097/00129689-200206000-00009. [DOI] [PubMed] [Google Scholar]
- 89.Joyce M, Moran C, Khan M, Lowe D, McAnena O. Laparoscopic mesh repair of a diaphragmatic hernia of Bochdalek. Surg Laparosc Endosc Percutan Tech. 2006;16:267–9. doi: 10.1097/00129689-200608000-00016. [DOI] [PubMed] [Google Scholar]
- 90.Vagefi PA, Morse CR. Bochdalek hernia in an adult. J Am Coll Surg. 2009;209:540. doi: 10.1016/j.jamcollsurg.2009.01.052. [DOI] [PubMed] [Google Scholar]
- 91.Jastaniah S, el-Tahir MI, Grillo IA, Batouk A, al-Shehry MY, Softah A, et al. Bochdalek hernia in adulthood: A case report and review of recent literature. Indian J Chest Dis Allied Sci. 1998;40:281–5. [PubMed] [Google Scholar]
- 92.Richardson WS, Bolton JS. Laparoscopic repair of congenital diaphragmatic hernias. J Laparoendosc Adv Surg Tech A. 2002;12:277–80. doi: 10.1089/109264202760268078. [DOI] [PubMed] [Google Scholar]
- 93.Rice GD, O’Boyle CJ, Watson DI, Devitt PG. Laparoscopic repair of Bochdalek hernia in an adult. ANZ J Surg. 2001;71:443–5. doi: 10.1046/j.1440-1622.2001.02151.x. [DOI] [PubMed] [Google Scholar]
- 94.Swain JM, Klaus A, Achem SR, Hinder RA. Congenital diaphragmatic hernia in adults. Semin Laparosc Surg. 2001;8:246–55. [PubMed] [Google Scholar]
- 95.Ghanem AN, Chankun TS, Brooks PL. Total gastric gangrene complicating adult Bochdalek hernia. Br J Surg. 1987;74:779. doi: 10.1002/bjs.1800740908. [DOI] [PubMed] [Google Scholar]
- 96.Zantut LF, Ivatury RR, Smith RS, Kawahara NT, Porter JM, Fry WR, et al. Diagnostic and therapeutic laparoscopy for penetrating abdominal trauma: A multicenter experience. J Trauma. 1997;42:825–31. doi: 10.1097/00005373-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 97.Kieffer J, Sapin E, Berg A, Beaudoin S, Bargy F, Helardot PG. Gastroesophageal reflux after repair of congenital diaphragmatic hernia. J Pediatr Surg. 1995;30:1330–3. doi: 10.1016/0022-3468(95)90497-2. [DOI] [PubMed] [Google Scholar]
- 98.Nagaya M, Akatsuka H, Kato J. Gastroesophageal reflux occurring after repair of congenital diaphragmatic hernia. J Pediatr Surg. 1994;29:1447–51. doi: 10.1016/0022-3468(94)90141-4. [DOI] [PubMed] [Google Scholar]


