Abstract
It is acknowledged that physicians do not seek the same expert aid for themselves as they would offer their patients. In their preclinical years, medical students appear to espouse comparable behavior. To many, medicine is described as a never-ending path that places the student under heavy stress and burnout from the beginning, leaving him/her vulnerable and with insufficient coping methods. Hence, the objective of this study is to 1) explore the prevalence of stress and burnout among preclinical medical students, and 2) propose solutions to decrease stress and burnout and improve medical education in the preclinical years. A detailed scholarly research strategy using Google Scholar, Scopus, Embase, MEDLINE and PubMed was implemented to highlight key themes that are relevant to preclinical medical students’ stress and burnout. Stress varied among different samples of medical students and ranged between 20.9% and 90%. Conversely, burnout ranged between 27% and 75%. Methods that help in reducing the incidence of stress and burnout by promoting strategies that focus on personal engagement, extracurricular activities, positive reinterpretation and expression of emotion, student-led mentorship programs, evaluation systems, career counseling and life coaching should be adopted.
Keywords: Burnout, medical education, medical school, medical student, preclinical years, stress
Introduction
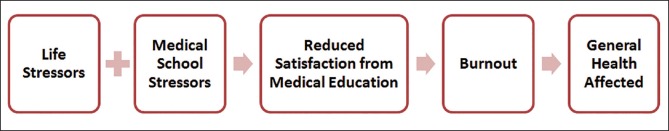
Medicine is a never-ending path and a highly demanding career that appears to leave many medical students at the risk of stress and burnout. A gap in the literature exists regarding the assessment of stress and burnout among preclinical medical students. Although medical schools strive to support students during the training process and aim to graduate knowledgeable, skillful and professional doctors, studies suggest that medical students experience high rates of personal distress,[1,2,3,4,5,6,7,8,9,10,11,12,13,14,15] with latent unfavorable consequences on academic performance,[16,17,18] aptitude,[19] professionalism[20,21,22,23,24,25,26,27] and health[12,28,29,30,31,32] [Figure 1]. There is proof that stress and anxiety during medical school foresee future predicaments in physicians,[13] which, in addition to individual torment, may unconstructively affect patient care.[13] Therefore, the objective of this article is to:
Figure 1.
A model illustrating the relations between contributing factors and health outcomes of burnout among medical students
Present the epidemiology and manifestations of stress and burnout among preclinical medical students, and
Propose solutions to decrease stress and burnout and improve medical education in the preclinical years.
To explore the central themes and epidemiology of preclinical medical students’ stress and burnout reported in the literature, sources were identified by searching Google Scholar, Scopus, Embase, MEDLINE and PubMed for English language articles published between 1953 and 2015. We used the following search terms: Medical student AND stress, burnout, distress, ethics, medical education, professionalism, emotional exhaustion, cynicism or academic performance. Additional studies were identified from the reference lists of these articles. Articles were reviewed critically by authors and included as appropriate to provide readers with a current overview of the research on medical student stress and burnout in the preclinical years.
Stress
Stress is a psychological and physical reaction to the ever-increasing demands of life. To a degree, it is a normal part of medical education and can be a motivator for certain individuals; however, not all students find stress constructive.[13] For many students, stress arouses feelings of fear, incompetence, uselessness, anger and guilt, and can be associated with both psychological and physical morbidities.[33,34,35] Among medical students, stress has been reported to be due to academic demands, exams, an inability to cope, helplessness, increased psychological pressure, mental tension, excessive workload,[36] curricular factors, personal life events and the learning environment.[37,38,39] These factors can result in decreased life satisfaction,[40] which in turn leads to unprofessional conduct, increased risk of suicidal ideation and serious thoughts of dropping out.[41,42] The literature reports varying rates of stress among samples of preclinical medical students. Fares et al.[43] rated stress among preclinical students from Lebanon at 62%. Sidik et al.,[44] Zaid et al.[45] and Fuad et al.[46] reported stress prevalence that ranges between 41.9% and 46.9% in Malaysian medical students. Moreover, Mosley et al.[8] and Ko et al.[47] reported a stress prevalence of 57% among preclinical medical students in the US and Singapore, respectively. In the UK, Guthrie revealed a 35.4% stress prevalence among preclinical medical students.[48] Similarly in India, Konjengbam et al.[49] reported a 37% stress prevalence among undergraduate medical students. Other studies report lower medical student stress ranging between 20.9% and 29.6%.[50,51,52]
Burnout
Burnout is another measure of physical exhaustion and mental distress, which is catalyzed primarily by occupational and professional demands. This syndrome of emotional exhaustion, depersonalization and low personal accomplishment culminates in decreased effectiveness at work.[42] A broad range of professions that heavily involve human interactions, such as physicians,[53,54] nurses[55,56] and educators,[57] experience burnout. Burnout is associated with decreased job performance[58] and reduced job commitment[56] and predicts stress-related health problems[59] and low career satisfaction.[60,61,62] It is well established in the literature that workload, lack of support and loss of control at times contribute to a sense of emotional exhaustion in those who endure medical education.[42,43] In addition, feelings of reduced personal accomplishment, overwork and emotional commitment to medicine can lead to depersonalization.[8] Hence, the development of burnout begins during the preclinical years, in which the setting is that of overwhelming work and facts to be learned with limited resources of time and memory, and continues throughout the clinical years.[33,43,52]
Burnout and stress are symptomatically similar, with burnout attributed specifically to occupational or academic stressors.[63] McManus et al.[64] proposed that there is a cyclic relation between stress and emotional exhaustion, which suggests that heightened levels of stress and poor coping strategies may be key contributors in the development of burnout.
A study in Lebanon that measures burnout risk in preclinical medical students showed that 75% suffered from burnout.[43] Another study from Spain revealed that 14.8% experienced burnout.[65] The varying levels of stress and burnout in different countries can be attributed to the life stressors that vary from one region to another. In addition to academic and medical school stressors, socioeconomic, political, conflict-related and health-related factors contribute to the increased levels of stress and burnout. In Lebanon, a Middle Eastern country amid conflicts and regional instability,[66,67,68,69,70] stress and burnout levels are expected to be higher than in Spain, for example, where similar stressors are relatively non-existent.
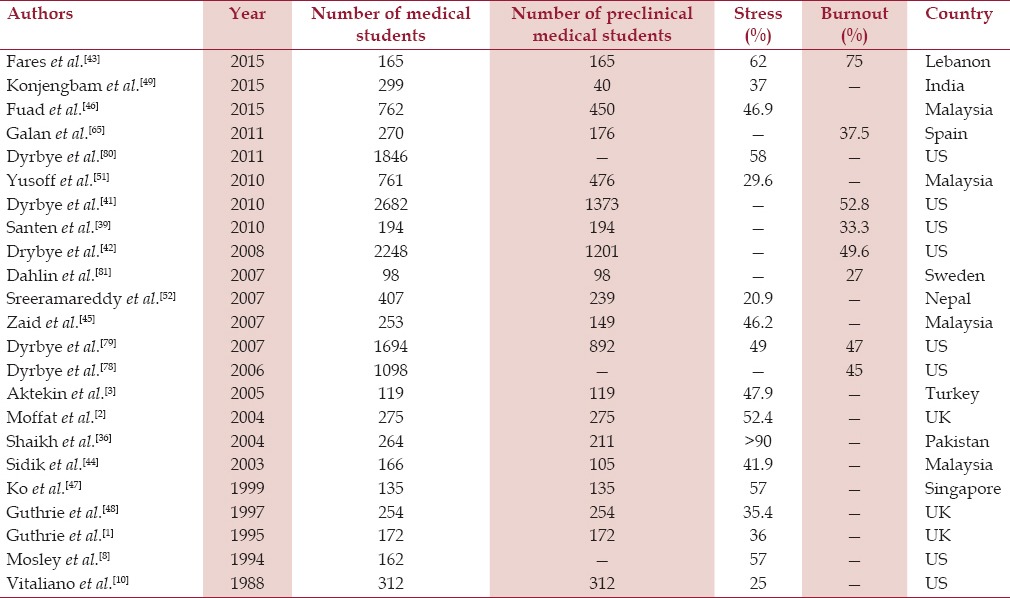
Numerous studies note rates of burnout between 25% and 60% in a wide spectrum of health-related specialties.[71,72,73,74,75,76] Nine US-based studies on burnout in medical students reported a prevalence ranging between 45% and 71%.[4,38,40,42,77,78,79,80,81] Table 1 shows the prevalence of stress and burnout in studies that include preclinical medical students from 1988 until 2015.
Table 1.
Stress and burnout levels in studies involving preclinical medical students between 1988 and 2015
Coping Mechanisms and Proposed Solutions
Students use various coping mechanisms to process stress [Figure 2]. Strategies that involve engagement such as problem solving, positive reinterpretation and expression of emotion, facilitate student adaptation,[2,8,33,43,82] which reduces anxiety and depression and their effects on mental wellbeing[59] and physical health.[82] Extracurricular activities involving music and physical exercise have been associated with decreased stress and burnout levels in preclinical medical students.[43] Unfortunately, few students seek help,[83] and distress often continues into residency and beyond[13] where it may have adverse effects on the quality of patient care delivered.[84,85] Therefore, it is critical for medical educators to understand the prevalence and severity of student stress and burnout, the potential adverse personal and professional consequences and the institutional factors that can affect student health from an early time.
Figure 2.

Methods and strategies that help in reducing stress and burnout in preclinical medical students
Student-led support programs that are designed to promote the mentorship of junior students by senior students are recommended because they appear to lower student stress and ultimately burnout. Although the Association of American Medical Colleges urges medical schools to foster relationships between faculty members and students to promote a positive learning environment,[86] we agree with Wolf et al.[87] that student-guided programs may present a stronger source of support and promote positive strategies for coping with stress. Mouret[88] proposed that senior medical students can more easily relate to challenges encountered by junior students. Many studies have shown that such events help in easing anxiety and stress and preventing burnout.[14,89,90,91,92]
Linzer et al.[93] and Freedborn et al.[94] discussed the importance of autonomy as a central component of physician job satisfaction. Dyrbye et al.[95] believed that autonomy was likely to be important for medical students as well. Students bring unique perspectives to curriculum committees and provide them a sense of ownership in their educational experience.[95]
The evaluation system used to assess student performance can also have a massive effect on the learning environment. Robins et al.[96] evaluated the effect of changing from numerical and letter grading schemes to a pass-fail grading system on student performance and satisfaction; they reported that students’ satisfaction with the evaluation system and learning environment improved with the pass-fail approach. Although certain medical schools foster a pass-fail evaluation system for the preclinical years, we believe that the competitive mentality of the students that has developed during the premedical years continues throughout the preclinical years and can lead to anxiety and distress.
We agree with Stewart et al.[33] and Park and Adler[82] that early poor academic performance in medical school, mental health problems and avoidant coping mechanisms may place students at risk of distress both during and after medical school. We suggest that medical schools offer career counseling, life-coaching and confidential resources covered by the university's health insurance plan to help these students. We also believe that student-led support groups, discussed earlier, can help students in processing conflict, raising self-awareness and nurturing empathy. Maslach[97] added that peer discussion groups also provide opportunities for students to express, analyze and share feelings, which decreases the likelihood of burnout. Pololi and Frankel[98] asserted that shared reflections helped students in realizing that their struggles were common and provided an insight into how colleagues solved similar problems.
More work can also be done to improve the stress and burnout conditions of preclinical medical students. Parkerson et al.[14] emphasized the importance of encouraging students to promote personal health with regular physical activity and adequate sleep. In addition, Wolf[99] and Gaber and Martin[100] believed that students should be provided with appropriate periods of rest during holidays and between modules to allow them to dissociate from the rigors of education and training. The transformation of medical students into medical doctors who are care-giving, compassionate, knowledgeable, well-appearing, and healthy requires improving the living and learning conditions during their medical education.[62]
Conclusion
This article implemented a detailed scholarly research strategy to highlight key themes that are relevant to preclinical medical students’ stress and burnout by introducing their definitions and exploring their prevalence and causes. In addition, this article proposed expert strategies and theories to help in reducing the incidence of stress and burnout and in promoting well-being among medical schools. Stress varied among the different samples of preclinical medical students and ranged between 20.9% and >90%, whereas the burnout prevalence rates ranged between 27% and 75%. As a result of work overload, overwhelming academic pressures to learn much within a limited time span and a sense of emotional commitment to medicine as a future career, burnout was found to manifest early among preclinical medical students; it then continues through the clinical years. High stress and burnout levels are associated with decreased life satisfaction, serious thoughts of dropping out and suicidal ideations; these cyclically lead to poorer performance, reduced commitment and higher levels of stress. It is particularly important to propose and implement strategies to reduce the incidence of stress and burnout among preclinical medical students to strengthen their commitment to medicine as a profession and allow for better future patient care. Strategies that focus on personal engagement, positive reinterpretation and expression of emotion, support programs delivered by senior students and extracurricular activities (mainly musical and physical activities) are among the coping mechanisms that are needed to reduce anxiety and thus, stress and burnout. It is the duty of medical educators to facilitate the utilization of such coping mechanisms to allow for smoother preclinical years and eventually more fruitful clinical years with physicians dedicated to providing the best care and commitment to patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Guthrie EA, Black D, Shaw CM, Hamilton J, Creed FH, Tomenson B. Embarking upon a medical career: Psychological morbidity in first year medical students. Med Educ. 1995;29:337–41. doi: 10.1111/j.1365-2923.1995.tb00022.x. [DOI] [PubMed] [Google Scholar]
- 2.Moffat KJ, McConnachie A, Ross S, Morrison JM. First year medical student stress and coping in a problem-based learning medical curriculum. Med Educ. 2004;38:482–91. doi: 10.1046/j.1365-2929.2004.01814.x. [DOI] [PubMed] [Google Scholar]
- 3.Aktekin M, Karaman T, Senol YY, Erdem S, Erengin H, Akaydin M. Anxiety, depression and stressful life events among medical students: A prospective study in Antalya, Turkey. Med Educ. 2005;35:12–7. doi: 10.1046/j.1365-2923.2001.00726.x. [DOI] [PubMed] [Google Scholar]
- 4.Guthrie E, Black D, Bagalkote H, Shaw C, Campbell M, Creed F. Psychological stress and burnout in medical students: A five-year prospective longitudinal study. J R Soc Med. 1998;91:237–43. doi: 10.1177/014107689809100502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Givers JL, Tjia J. Depressed medical students’ use of mental health services and barriers to use. Acad Med. 2002;77:918–21. doi: 10.1097/00001888-200209000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Clark DC, Zeldow PB. Vicissitudes of depressed mood during four years of medical school. JAMA. 1988;260:2521–8. [PubMed] [Google Scholar]
- 7.Rosal MC, Ockene IS, Ockene JK, Barren SV, Ma Y, Hebert JR. A longitudinal study of students’ depression at one medical school. Acad Med. 1997;72:542–6. doi: 10.1097/00001888-199706000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Mosley TH, Jr, Perrin SG, Neral SM, Dubbert PM, Grothues CA, Pinto BM. Stress, coping, and well-being among third-year medical students. Acad Med. 1994;69:765–7. doi: 10.1097/00001888-199409000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Roberts LW, Warner TD, Lyketsos C, Frank E, Ganzini L, Carter D. Collaborative Research Group on Medical Student Health. Perceptions of academic vulnerability associated with personal illness: A study of 1,027 students at nine medical schools. Compr Psychiatry. 2004;42:1–15. doi: 10.1053/comp.2001.19747. [DOI] [PubMed] [Google Scholar]
- 10.Vitaliano PP, Maiuro RD, Russo J, Mitchell ES, Carr JE, Van Citters RL. A biopsychosocial model of medical student distress. J Behav Med. 1988;11:311–31. doi: 10.1007/BF00844933. [DOI] [PubMed] [Google Scholar]
- 11.Raj SR, Simpson CS, Hopman WM, Singer MA. Health-related quality of life among final-year medical students. CMAJ. 2000;162:509–10. [PMC free article] [PubMed] [Google Scholar]
- 12.Ball S, Bax A. Self-care in medical education: Effectiveness of health-habits interventions for first-year medical students. Acad Med. 2002;77:911–7. doi: 10.1097/00001888-200209000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Tyssen R, Vaglum P, Gronvold NT, Ekeberg O. Suicidal ideation among medical students and young physicians: A nationwide and prospective study of prevalence and predictors. J Affect Disord. 2001;64:69–79. doi: 10.1016/s0165-0327(00)00205-6. [DOI] [PubMed] [Google Scholar]
- 14.Parkerson GR, Jr, Broadhead WE, Tse CK. The health status and life satisfaction of first-year medical students. Acad Med. 1990;65:586–8. doi: 10.1097/00001888-199009000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Carson AJ, Dias S, Johnston A, McLoughlin MA, O’Connor M, Robinson BL, et al. Mental health in medical students: A case control study using the 60 item General Health Questionnaire. Scott Med J. 2000;45:115–6. doi: 10.1177/003693300004500406. [DOI] [PubMed] [Google Scholar]
- 16.Spiegel DA, Smolen RC, Jonas CK. An examination of the relationships among interpersonal stress, morale and academic performance in male and female medical students. Soc Sci Med. 1986;23:1157–61. doi: 10.1016/0277-9536(86)90334-5. [DOI] [PubMed] [Google Scholar]
- 17.Spiegel DA, Smolen RC, Hopfensperger KA. Medical student stress and clerkship performance. J Med Educ. 1986;61:929–31. doi: 10.1097/00001888-198611000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Hojat M, Robeson M, Damjanov I, Veloski JJ, Glaser K, Gonnella JS. Students’ psychosocial characteristics as predictors of academic performance in medical school. Acad Med. 1993;68:635–7. doi: 10.1097/00001888-199308000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–7. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- 20.Woloschuk W, Harasym PH, Temple W. Attitude change during medical school: A cohort study. Med Educ. 2004;38:522–34. doi: 10.1046/j.1365-2929.2004.01820.x. [DOI] [PubMed] [Google Scholar]
- 21.Hojat M, Mangione S, Nasca T, Rattner S, Erdmann JB, Gonnella JS, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–41. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 22.Crandall SJ, VoIk RJ, Loemker V. Medical students’ attitudes toward providing care for the underserved: Are we training socially responsible physicians? JAMA. 1993;269:2519–23. [PubMed] [Google Scholar]
- 23.Rezler AG, Ten Haken JT. Affect and research in medical education. Med Educ. 1984;18:331–8. doi: 10.1111/j.1365-2923.1984.tb01278.x. [DOI] [PubMed] [Google Scholar]
- 24.Eron LD. D. The effect of medical education on attitudes: A follow-up study. J Med Educ. 1958;33:25–33. [PubMed] [Google Scholar]
- 25.Wolf TM, Balson PM, Faucett JM, Randall HM. A retrospective study of attitude change during medical education. Med Educ. 1989;23:19–23. doi: 10.1111/j.1365-2923.1989.tb00807.x. [DOI] [PubMed] [Google Scholar]
- 26.Eron LD. Effect of medical education on medical students’ attitudes. J Med Educ. 1955;30:559–66. [PubMed] [Google Scholar]
- 27.Rezler AG, Flaherty JA. New York, NY: Springer; 1985. The Interpersonal Dimension in Medical Education. [Google Scholar]
- 28.Gutgesell M, Reeve R, Parsons B, Morse RM. Exercise and alcohol consumption among medical students. Acad Med. 1999;74:750–1. doi: 10.1097/00001888-199907000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Croen LG, Woesner M, Herman M, Reichgott M. A longitudinal study of substance use and abuse in a single class of medical students. Acad Med. 1997;72:376–81. doi: 10.1097/00001888-199705000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Clark D, Eckenfels EJ, Daugherty SR, Fawcett J. Alcohol-use patterns through medical school: A longitudinal study of one class. JAMA. 1987;257:2921–6. [PubMed] [Google Scholar]
- 31.Mangus RS, Hawkins CE, Miller MJ. Tobacco and alcohol use among 1996 medical school graduates. JAMA. 1998;280:1192–3, 1195. [PubMed] [Google Scholar]
- 32.Newbury-Birch D, Walshaw D, Kamali F. Drink and drugs: From medical students to doctors. Drug Alcohol Depend. 2001;64:265–70. doi: 10.1016/s0376-8716(01)00128-4. [DOI] [PubMed] [Google Scholar]
- 33.Stewart SM, Betson C, Lam TH, Marshall IB, Lee PW, Wong CM. Predicting stress in first year medical students: A longitudinal study. Med Educ. 1997;31:163–8. doi: 10.1111/j.1365-2923.1997.tb02560.x. [DOI] [PubMed] [Google Scholar]
- 34.Bramness JG, Fixdal TC, Vaglum P. Effect of medical school stress on the mental health of medical students in early and late clinical curriculum. Acta Psychiatr Scand. 1991;84:340–5. doi: 10.1111/j.1600-0447.1991.tb03157.x. [DOI] [PubMed] [Google Scholar]
- 35.Tyssen R, Vaglum P, Grønvold NT, Ekeberg O. Factors in medical school that predict postgraduate mental health problems in need of treatment: A nationwide and longitudinal study. Med Educ. 2001;35:110–20. doi: 10.1046/j.1365-2923.2001.00770.x. [DOI] [PubMed] [Google Scholar]
- 36.Shaikh BT, Kahloon A, Kazmi M, Khalid H, Nawaz K, Khan N, et al. Students, stress and coping strategies: A case of Pakistani medical school. Educ Health (Abingdon) 2001;17:346–53. doi: 10.1080/13576280400002585. [DOI] [PubMed] [Google Scholar]
- 37.Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. Personal life events and medical student burnout: A multicenter study. Acad Med. 2006;81:374–84. doi: 10.1097/00001888-200604000-00010. [DOI] [PubMed] [Google Scholar]
- 38.Dyrbye LN, Thomas MR, Harper W, Massie FS, Jr, Power DV, Eacker A, et al. The learning environment and medical student burnout: A multicentre study. Med Educ. 2009;43:274–82. doi: 10.1111/j.1365-2923.2008.03282.x. [DOI] [PubMed] [Google Scholar]
- 39.Santen SA, Holt DB, Kemp JD, Hemphill RR. Burnout in medical students: Examining the prevalence and associated factors. South Med J. 2010;103:758–63. doi: 10.1097/SMJ.0b013e3181e6d6d4. [DOI] [PubMed] [Google Scholar]
- 40.Kjeldstadli K, Tyssen R, Finset A, Hem E, Gude T, Gronvold NT, et al. Life satisfaction and resilience in medical school – A six-year longitudinal, nationwide and comparative study. BMC Med Educ. 2006;6:48. doi: 10.1186/1472-6920-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dyrbye LN, Massie FS, Jr, Eacker A, Harper W, Power D, Durning SJ, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304:1173–80. doi: 10.1001/jama.2010.1318. [DOI] [PubMed] [Google Scholar]
- 42.Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149:334–41. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 43.Fares J, Saadeddin Z, Al Tabosh H, Aridi H, El-Mouhayyar C, Koleilat MK, et al. Extracurricular activities associated with stress and burnout in preclinical medical students. J Epidemiol Glob Health. 2015 doi: 10.1016/j.jegh.2015.10.003. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sidik SM, Rampal L, Kaneson N. Prevalence of emotional disorders among medical students in a Malaysian university. Asia Pac Fam Med. 2003;2:213–7. [Google Scholar]
- 45.Zaid ZA, Chan SC, Ho JJ. Emotional disorders among medical students in a Malaysian private medical school. Singapore Med J. 2007;48:895–9. [PubMed] [Google Scholar]
- 46.Fuad MD, Al-Zurfi BM, Qader MA, Abu Bakar MF, Elnajeh M, Abdullah MR. Prevalence and risk factors of stress, anxiety and depression among medical students of a private medical university in Malaysia. Education in Medicine Journal. 2015;7:e52–9. [Google Scholar]
- 47.Ko SM, Kua EH, Fones CS. Stress and the undergraduates. Singapore Med J. 1999;40:627–30. [PubMed] [Google Scholar]
- 48.Guthrie EA, Black D, Shaw CM, Hamilton J, Creed FH, Tomenson B. Psychological stress in medical students: A comparison of two very different university courses. Stress Med. 1997;13:179–84. [Google Scholar]
- 49.Konjengbam S, Laishram J, Singh BA, Elangbam V. Psychological morbidity among undergraduate medical students. Indian J Public Health. 2015;59:65–6. doi: 10.4103/0019-557X.152872. [DOI] [PubMed] [Google Scholar]
- 50.Sarikaya O, Civaner M, Kalaca S. The anxieties of medical students related to clinical training. Int J Clin Pract. 2006;60:1414–8. doi: 10.1111/j.1742-1241.2006.00869.x. [DOI] [PubMed] [Google Scholar]
- 51.Yusoff MS, Abdul Rahim AF, Yaacob MJ. Prevalence and sources of stress among Universiti Sains Malaysia medical students. Malays J Med Sci. 2010;17:30–7. [PMC free article] [PubMed] [Google Scholar]
- 52.Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7:26. doi: 10.1186/1472-6920-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gundersen L. Physician burnout. Ann Intern Med. 2001;135:145–8. doi: 10.7326/0003-4819-135-2-200107170-00023. [DOI] [PubMed] [Google Scholar]
- 54.Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM, Leaning MS, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–9. doi: 10.1038/bjc.1995.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kilfedder CJ, Power KG, Wells TJ. Burnout in psychiatric nursing. J Adv Nurs. 2001;34:383–96. doi: 10.1046/j.1365-2648.2001.01769.x. [DOI] [PubMed] [Google Scholar]
- 56.Leiter MP, Harvie P, Frizzell C. The correspondence of patient satisfaction and nurse burnout. Soc Sci Med. 1998;47:1611–7. doi: 10.1016/s0277-9536(98)00207-x. [DOI] [PubMed] [Google Scholar]
- 57.Cherniss C. New York, NY: Psychology Press; 1995. Beyond Burnout: Helping Teachers, Nurses, Therapists, and Lawyers Recover from Stress and Disillusionment. [Google Scholar]
- 58.Parker PA, Kulik JA. Burnout, self-and supervisor-rated job performance, and absenteeism among nurses. J Behav Med. 1995;18:581–99. doi: 10.1007/BF01857897. [DOI] [PubMed] [Google Scholar]
- 59.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 60.Goldberg R, Boss RW, Chan L, Goldberg J, Mallon WK, Moradzadeh D, et al. Burnout and its correlates in emergency physicians: Four years’ experience with a wellness booth. Acad Emerg Med. 1996;3:1156–64. doi: 10.1111/j.1553-2712.1996.tb03379.x. [DOI] [PubMed] [Google Scholar]
- 61.Lemkau JP, Rafferty JP, Gordon R., Jr Burnout and career-choice regret among family practice physicians in early practice. Fam Pract Res J. 1994;14:213–22. [PubMed] [Google Scholar]
- 62.Ayoub F, Fares Y, Fares J. The psychological attitude of patients toward health practitioners in Lebanon. N Am J Med Sci. 2015;7:452–8. doi: 10.4103/1947-2714.168663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maslach C, Jackson SE, Leiter MP. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. The Maslach Burnout Inventory. [Google Scholar]
- 64.McManus IC, Keeling A, Paice E. Stress, burnout and doctors’ attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Med. 2004;2:29. doi: 10.1186/1741-7015-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Galán F, Sanmartín A, Polo J, Giner L. Burnout risk in medical students in Spain using the Maslach Burnout Inventory-Student Survey. Int Arch Occup Environ Health. 2011;84:453–9. doi: 10.1007/s00420-011-0623-x. [DOI] [PubMed] [Google Scholar]
- 66.Fares Y, Fares J. Anatomical and neuropsychological effects of cluster munitions. Neurol Sci. 2013;34:2095–100. doi: 10.1007/s10072-013-1343-7. [DOI] [PubMed] [Google Scholar]
- 67.Fares Y, El-Zaatari M, Fares J, Bedrosian N, Yared N. Trauma-related infections due to cluster munitions. J Infect Public Health. 2013;6:482–6. doi: 10.1016/j.jiph.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 68.Fares Y, Ayoub F, Fares J, Khazim R, Khazim M, Gebeily S. Pain and neurological sequelae of cluster munitions on children and adolescents in South Lebanon. Neurol Sci. 2013;34:1971–6. doi: 10.1007/s10072-013-1427-4. [DOI] [PubMed] [Google Scholar]
- 69.Fares Y, Fares J, Gebeily S. Head and facial injuries due to cluster munitions. Neurol Sci. 2014;35:905–10. doi: 10.1007/s10072-013-1623-2. [DOI] [PubMed] [Google Scholar]
- 70.Hoteit A, Fares J. Psycho-environmental tribulations arising from cluster munitions in South Lebanon. Sci-Afric Journal of Scientific Issues, Research and Essays. 2014;2:469–73. [Google Scholar]
- 71.Robinson GE. Stresses on women physicians: Consequences and coping techniques. Depress Anxiety. 2003;17:180–9. doi: 10.1002/da.10069. [DOI] [PubMed] [Google Scholar]
- 72.Doyle C, Hind P. Occupational stress, burnout and job status in female academics. Gend Work Organ. 1998;5:67–82. [Google Scholar]
- 73.Firth-Cozens J. Source of stress in women junior house officers. BMJ. 1990;301:89–91. doi: 10.1136/bmj.301.6743.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McMurray JE, Linzer M, Konrad TR, Douglas J, Shugerman R, Nelson K. The work lives of women physicians results from the physician work life study. The SGIM Career Satisfaction Study Group. J Gen Intern Med. 2000;15:372–80. doi: 10.1111/j.1525-1497.2000.im9908009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gadzella BM, Ginther DW, Tomcala M, Bryant GW. Stress as perceived by professionals. Psychol Rep. 1990;67:979–83. doi: 10.2466/pr0.1990.67.3.979. [DOI] [PubMed] [Google Scholar]
- 76.Whitley TW, Allison EJ, Jr, Gallery ME, Cockington RA, Gaudry P, Heyworth J, et al. Work-related stress and depression among practicing emergency physicians: An international study. Ann Emerg Med. 1994;23:1068–71. doi: 10.1016/s0196-0644(94)70105-9. [DOI] [PubMed] [Google Scholar]
- 77.Peisah C, Latif E, Wilhelm K, Williams B. Secrets to psychological success: Why older doctors might have lower psychological distress and burnout than younger doctors. Aging Ment Health. 2009;13:300–7. doi: 10.1080/13607860802459831. [DOI] [PubMed] [Google Scholar]
- 78.Dyrbye LN, Thomas MR, Huschka MM, Lawson KL, Novotny PJ, Sloan JA, et al. A multicenter study of burnout, depression, and quality of life in minority and nonminority US medical students. Mayo Clin Proc. 2006;81:1435–42. doi: 10.4065/81.11.1435. [DOI] [PubMed] [Google Scholar]
- 79.Dyrbye LN, Thomas MR, Eaker A, Harper W, Massie FS, Jr, Power DV, et al. Race, ethnicity, and medical student well-being in the United States. Arch Intern Med. 2007;167:2103–9. doi: 10.1001/archinte.167.19.2103. [DOI] [PubMed] [Google Scholar]
- 80.Dyrbye LN, Harper W, Durning SJ, Moutier C, Thomas MR, Massie FS, Jr, et al. Patterns of Distress in US Medical Students. Med Teach. 2011;33:834–9. doi: 10.3109/0142159X.2010.531158. [DOI] [PubMed] [Google Scholar]
- 81.Dahlin ME, Runeson B. Burnout and psychiatric morbidity among medical students entering clinical training: A three year prospective questionnaire and interview-based study. BMC Med Educ. 2007;7:6. doi: 10.1186/1472-6920-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Park CL, Adler NE. Coping style as a predictor of health and well-being across the first year of medical school. Health Psychol. 2003;22:627–31. doi: 10.1037/0278-6133.22.6.627. [DOI] [PubMed] [Google Scholar]
- 83.Tjia J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J Am Coll Health. 2005;53:219–24. doi: 10.3200/JACH.53.5.219-224. [DOI] [PubMed] [Google Scholar]
- 84.Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 85.West CP, Huschka MM, Novotny PJ, Sloan JA, Kolars JC, Habermann TM, et al. Association of perceived medical errors with resident distress and empathy: A prospective longitudinal study. JAMA. 2006;296:1071–8. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 86.Washington, DC: Association of American Medical Colleges; 1984. Association of American Medical Colleges. Physicians for the Twenty-First Century: The GPEP Report: Report of the Panel on the General Professional Education of the Physician and College Preparation for Medicine. [PubMed] [Google Scholar]
- 87.Wolf TM, Randall HM, Faucett JM. A survey of health promotion programs in U.S. and Canadian medical schools. Am J Health Promot. 1988;3:33–6. doi: 10.4278/0890-1171-3.1.33. [DOI] [PubMed] [Google Scholar]
- 88.Mouret GM. Stress in a graduate medical degree. Med J Aust. 2002;177(Suppl):S10–1. doi: 10.5694/j.1326-5377.2002.tb04615.x. [DOI] [PubMed] [Google Scholar]
- 89.Lemkau JP, Purdy RR, Rafferty JP, Rudisill JR. Correlates of burnout among family practice residents. J Med Educ. 1988;63:682–91. doi: 10.1097/00001888-198809000-00003. [DOI] [PubMed] [Google Scholar]
- 90.Myers DG. The funds, friends, and faith of happy people. Am Psychol. 2000;55:56–67. doi: 10.1037//0003-066x.55.1.56. [DOI] [PubMed] [Google Scholar]
- 91.Lee J, Graham AV. Students’ perception of medical school stress and their evaluation of a wellness elective. Med Educ. 2001;35:652–9. doi: 10.1046/j.1365-2923.2001.00956.x. [DOI] [PubMed] [Google Scholar]
- 92.Rathbun J. Helping medical students develop lifelong strategies to cope with stress. Acad Med. 1995;70:955–6. doi: 10.1097/00001888-199511000-00007. [DOI] [PubMed] [Google Scholar]
- 93.Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC. Society of General Internal Medicine (SGIM) Career Satisfaction Study Group (CSSG). Predicting and preventing physician burnout: Results from the United States and the Netherlands. Am J Med. 2001;111:170–5. doi: 10.1016/s0002-9343(01)00814-2. [DOI] [PubMed] [Google Scholar]
- 94.Freedborn DK. Satisfaction, commitment, and psychological well-being among HMO physicians. Permanente J. 2000;2:22–30. doi: 10.1136/ewjm.174.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80:1613–22. doi: 10.4065/80.12.1613. [DOI] [PubMed] [Google Scholar]
- 96.Robins LS, Fantone JC, Oh MS, Alexander GL, Shlafer M, Davis WK. The effect of pass/fail grading and weekly quizzes on first-year students’ performances and satisfaction. Acad Med. 1995;70:327–9. doi: 10.1097/00001888-199504000-00019. [DOI] [PubMed] [Google Scholar]
- 97.Maslach C. Burned out. Hum Behav. 1976;5:16–22. [Google Scholar]
- 98.Pololi L, Frankel RM. Small-group teaching emphasizing reflection can positively influence medical students’ values. Acad Med. 2001;76:1172–3. doi: 10.1097/00001888-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 99.Wolf TM. Stress, coping and health: Enhancing well-being during medical school. Med Educ. 1994;28:8. doi: 10.1111/j.1365-2923.1994.tb02679.x. [DOI] [PubMed] [Google Scholar]
- 100.Gaber RR, Martin DM. Still-Well osteopathic medical student wellness program. J Am Osteopath Assoc. 2002;102:289–92. [PubMed] [Google Scholar]