Abstract
Objective:
The objective of this study was to determine the prevalence of obesity among students of medical colleges of Lahore and to study its correlation with high-caloric diet intake and physical inactivity.
Study Design:
A cross-sectional survey was conducted at four medical colleges of Lahore, Pakistan between March and June 2012.
Methods:
A total of 244 medical students (85 males, 159 females) of the median age of 20 years (range: 18–25) were randomly included in the study. Anthropometric measures were obtained. High-caloric diet intake and physical profile were assessed through a self-reported questionnaire. The relationships between obesity indices (body mass index [BMI], waist-to-hip ratio) were investigated and correlated with the studied dietary and physical activity factors.
Results:
Approximately, 30.5% males and 16% females had BMI ≥25.0 kg/m2 overall affecting 21% of total medical students. Central obesity was found in 46% of male and 31.4% of female students. Central obesity was associated with a higher total daily caloric intake, studying at private medical college and male gender. Overall, 197 of 244 (80.7%) students played no sports in college. Median time to watch television or work on the computer was 120 min a day (range: 30–420). Only 70 (28.7%) students had regular walk or jogging.
Conclusion:
A substantial proportion of Pakistani medical students were overweight or obese. Higher total daily caloric intake was associated with central obesity but not a BMI >25. Physical activity parameters favored an overall sedentary aptitude for medical students.
Keywords: High-caloric diet, medical students, obesity, Pakistan, physical activity
INTRODUCTION
The incidence of obesity is increasing dramatically worldwide. The estimated total numbers of overweight and obese adults in 2005 were 937 and 396 million, respectively. Overall 23% world adult population is overweight and 9.8% is obese. By 2030, the number of overweight and obese adults is projected to be 2.16 and 1.12 billion, (38% and 20%), respectively. Moreover, if recent trends continue, by 2030 up to 57.8% of the world's adult population (3.3 billion people) could be either overweight or obese.[1]
A variety of factors, including diet, genetic predisposition, physical activities, physiological, and behavioral factors, are implicated as contributing factors to obesity.[2] Health personnel are important promoters and role models for maintaining a healthy lifestyle for the general population; however, studies on medical students and health personnel in many countries suggest that obesity is a problem among these population groups.[3,4,5,6,7,8] Obesity is an important noncommunicable disease in Pakistan. A recent survey conducted on an adult population of Karachi showed that 46% of the participants were obese and 18% were overweight. The prevalence of obesity in medical students of Pakistan is unknown. Moreover, the dietary patterns and level of physical activity have not been studied in this particular population group.
The aim of this descriptive study was to assess the prevalence of preobesity and obesity among medical students of Lahore, Pakistan. We investigated the relationships between two different obesity indices (body mass index [BMI] and waist-to-hip [WHR] ratio) with high-caloric food intake and physical activity.
METHODS
A cross-sectional survey was conducted between March and June 2012 at following four medical colleges of Lahore, Pakistan:
Allama Iqbal Medical College
Services Institute of Medical Sciences
Fatima Memorial Hospital College of Medicine and Dentistry
Lahore Medical and Dental College.
Assuming a proportion of 20% in a population of 10,000 and 95% confidence interval, the calculated sample size was 240. A total of 244 students were randomly selected by using computer generated random numbers. Medical students of both genders and all professional years were eligible. Students were enrolled in the survey after obtaining written informed consent. A brief history was taken regarding any endocrine disorder, medication, or relevant subjective signs and symptoms before choosing the respondent. Medical students suffering from metabolic disorders such as hypothyroidism (untreated), type 2 diabetes mellitus, and metabolic syndrome were excluded. Medical students who are taking steroids and anti-obesity drugs, such as amphetamines and orlistat, were also excluded.
Data collection procedure
The detailed demographic information was collected from the respondents. The data related to dietary and physical activity were collected on a self-administered structured questionnaire. Caloric intake was assessed across 24 categories of common high-caloric food items. Frequency, number of servings, and serving sizes were recorded and monthly caloric intake from each dietary item was calculated. Average total daily caloric intake from high-calorie diets was calculated for each individual. Physical activity was assessed by documenting type and time spent on a number of physical activities and time spent on watching TV. Subjects were given instructions on how to fill out the questionnaire completely and truthfully. After filling out the questionnaire, anthropometric measurements such as weight, height, waist, and hip measurements were done according to the WHO standards.
Based on the revised guidelines for Asian population, the respondents were classified as overweight and obese if their BMI was 23–24.9 and ≥25, respectively. Central/abdominal obesity was defined as a WHR ≥0.90 for males and 0.85 for females.[9]
Data analysis procedure
Data were analyzed using SPSS Statistics software version 17 (SPSS Inc., Chicago, IL, USA). Frequencies of different categorical variables were calculated. Median and range were calculated for continuous variables. Patient characteristics were compared with the use of the Chi-square or Fisher's exact test for categorical variables. Mann–Whitney test was used for continuous variables. A one-sided P < 0.05 was considered to be statistically significant at a 95% confidence interval. A multivariate logistic regression analysis was performed to determine predictors of overweight and obesity.
RESULTS
A total of 244 medical students were included in the study. The median age was 20 years (range: 18–25) and 159 (65.2%) were females. Out of 244 subjects, 143 (58.6%) were from the public sector. Median height of the subjects was 165 cm (range: 146–193), median weight was 58 kg (range: 38– 105), and median BMI was 21.35 kg/m2 (range: 15.6–36.1). Out of 244 subjects, 26 (10.7%) were underweight, 142 (58.2%) had normal BMI, 25 (10.2%) were overweight/preobese, and 51 (20.9%) were obese. Significantly greater number of males were obese (BMI ≥25) as compared to females (31% [26 of 85] vs. 16% [25 of 159]; P = 0.007). The median WHR was 0.88 (range: 0.74–1.04) in males and 0.80 (range: 0.56–1.04) in females. Central obesity was seen in 46% (39 of 85) of males (WHR ≥0.90) and 31% (49 of 159) of female (WHR ≥0.85); the difference was statistically significant (P = 0.02). Day scholars were more likely to have central obesity as compared to boarders (44% [48 of 109] vs. 29.6% [40 of 135]; P = 0.02). Students from private medical colleges were significantly more likely to have central obesity than students from public sector medical colleges (56% [57 of 101] vs. 22% [31 of 143]; P < 0.001). BMI ≥25 was also more common in students from private medical colleges than the private sector colleges; however, the difference was not statistically significant (26.7% [27 of 101] vs. 16.8% [24 of 143]; P = 0.06).
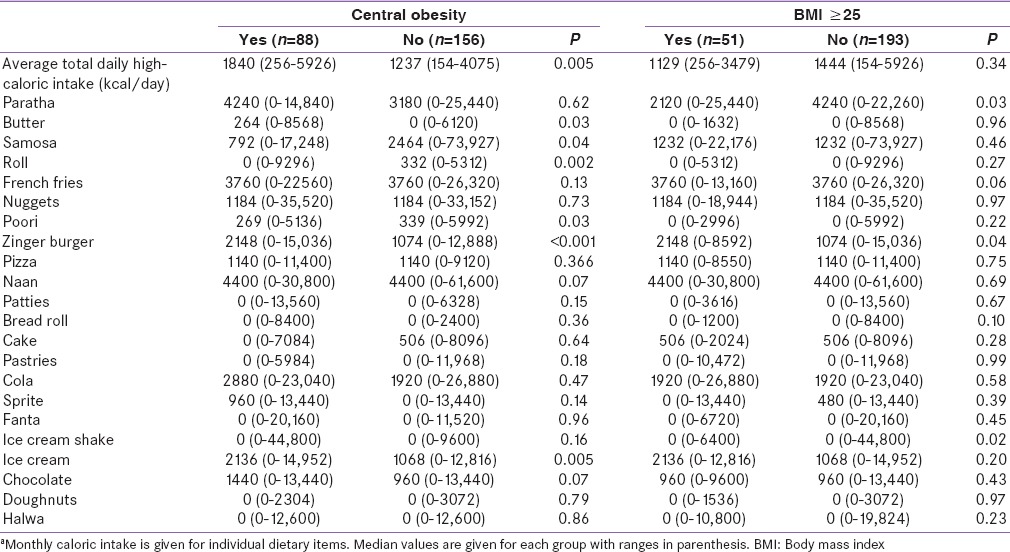
Average total daily caloric intake was significantly higher in students who had central obesity but not in patients who had a BMI ≥25 [Table 1]. Similarly, the average total daily caloric intake was significantly higher in students from private medical colleges (median 1818 kcal [range: 385–5926] vs. 1235 [range: 154–4075]; P = 0.001). Day scholars also had a higher average daily caloric intake as compared to boarders; however, the difference was not statistically significant (median 1488 [range: 256–5926] vs. median 1356 [range: 154–4075]; P = 0.08). The average monthly caloric intake from a variety of food items is shown [Table 1]. Students with central obesity had a significantly higher caloric intake from fried continental and/or fast food (butter, zinger burger) and ice cream. Students with a BMI ≥25 had a higher caloric intake from zinger burger and lesser intake from paratha. These students also were less likely to take daily breakfast as compared to those with a BMI <25 (35.2% [18 of 51] vs. 53.4% [103 of 193]; P = 0.02).
Table 1.
Comparison of dietary intake patternsa
Overall, 197 of 244 (80.7%) students played no sports in college. Median time to watch television or work on the computer was 120 min a day (range: 30–420). Only 70 (28.7%) students had regular walk or jogging. Work out in the gym was reported in 28 (11.5%) students. No significant difference was found across these groups (obese vs. nonobese) in terms of these indicators of physical activity.
On multivariate binary logistic regression analysis, the predictors of central obesity included higher total average daily caloric intake, studying at private medical college, higher caloric intake from ice cream, and higher training year.
DISCUSSION
In this study, we found that approximately 30.5% males and 16% females had BMI ≥25.0 kg/m2 overall affecting 21% of total medical students. It was observed that preobesity and obesity were 14.5% more prevalent in males as compared to females. Our findings are similar to other studies in terms of high prevalence of preobesity and obesity among male medical students. A study in Greece showed that 40% of male and 23% of female students had BMI ≥25.0 kg/m2.[5] A study in Slovakia showed that 16% of male but only 2% of female medical students had a BMI >25.0 kg/m2.[10] In a study of male medical students in the US, nearly one-fifth of the subjects had a BMI >24.7 kg/m2 and a further 30% were classified as overweight with BMI 22.8–24.7 kg/m2.[11]
In our survey, the prevalence of central obesity was alarmingly high (46% of male and 31.4% of female students); higher than that reported in Greece (33.4% male and 21.7% female medical students).[5]
Students with central obesity had a significantly greater total daily caloric intake. However, no correlation was found between total daily caloric intake from high-calorie diets and BMI. Students from private medical colleges were more likely to have central obesity and had a higher median daily high-caloric intake. Day scholars were also more likely to have central obesity; however, the average total daily caloric intake was not significantly different from that of boarders.
Overall, the physical activity was very low in medical students. Most of the students neither played sports in college nor did do regular walk or jogging. Several studies have illustrated the importance of decreased energy expenditure in the pathogenesis of weight gain. Estimates of energy intake and energy expenditure in Great Britain suggest that reduced energy expenditure is more important than increased food intake in causing obesity.[12] Similarly, a study of middle-aged men in the Netherlands found that the decline in energy expenditure accounted for almost all of the weight gain.[13] According to the Surgeon General's Report of Physical Activity, the percent of adult Americans participating in physical activity decreases steadily with age, and reduced energy expenditure in adults and children is predictive of weight gain.[14]
In our study, the median time to watch TV or work on the computer was also high (median 2 h a day). Of all sedentary behaviors, prolonged television watching appears to be the most predictive of obesity and diabetes risk. In the Nurses’ Health Study, after adjustment for age, smoking, exercise level, and dietary factors, every 2 h increment spent watching TV was associated with a 23% (95% CI 17–30%) increase in obesity and a 14% (95% CI 5–23%) increase in the risk of diabetes.[15] We did not find any statistically significant difference in physical activity between obese and nonobese individuals. As overall physical activity was very low across these groups, the risk of ß error is high, and a larger sample size would be required to address this problem.
Students with central obesity had a higher caloric intake from butter and zinger burger. Frequent fast-food consumption may also be associated with weight gain and risk of type 2 diabetes. This was illustrated in a secondary analysis of the CARDIA study, a population-based prospective study of cardiovascular disease risk factor development in young adults followed for the subsequent 15 years.[16] When compared to subjects who ate fast food infrequently (less than once per week), and after adjustment for other lifestyle factors, subjects who consumed fast food frequently (greater than twice per week) at baseline and follow-up gained an extra 4.5 kg of weight and had a two-fold increase in insulin resistance as measured by the homeostasis model (HOMA). The study is limited by the lack of information on portion size and caloric density of the foods consumed.
Our results underscore the need to implement health promotion programs, especially to promote the need for adopting a healthy and active lifestyle in the adult population.
CONCLUSION
There is a high prevalence of obesity and preobesity in medical students of Lahore, Pakistan. Males, students from private medical colleges and students having higher average daily high-caloric diet intake were more likely to have central obesity. The level of physical activity was alarmingly low in the students.
Acknowledgment
We thank Mrs. Shehla Javed Akram for her help in developing the questionnaire.
Financial support and sponsorship
The study was funded by Research Society, Allama Iqbal Medical College, Lahore.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32:1431–7. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 2.Wilborn C, Beckham J, Campbell B, Harvey T, Galbreath M, La Bounty P, et al. Obesity: Prevalence, theories, medical consequences, management, and research directions. J Int Soc Sports Nutr. 2005;2:4–31. doi: 10.1186/1550-2783-2-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar A, Ramiah S. Anthropometric studies on students of the Nepal medical college: Elbow breadth. Kathmandu Univ Med J (KUMJ) 2005;3:345–8. [PubMed] [Google Scholar]
- 4.Ohe K, Hachiya Y, Takahashi Y, Oda S, Takahara K. The significance of obesity in UOEH medical students – Multiple regression analysis of the annual physical checkup data in 1991. J UOEH. 1992;14:279–88. doi: 10.7888/juoeh.14.279. [DOI] [PubMed] [Google Scholar]
- 5.Bertsias G, Mammas I, Linardakis M, Kafatos A. Overweight and obesity in relation to cardiovascular disease risk factors among medical students in Crete, Greece. BMC Public Health. 2003;3:3. doi: 10.1186/1471-2458-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neser WB, Thomas J, Semenya K, Thomas DJ, Gillum RF. Obesity and hypertension in a longitudinal study of black physicians: The Meharry Cohort study. J Chronic Dis. 1986;39:105–13. doi: 10.1016/0021-9681(86)90066-4. [DOI] [PubMed] [Google Scholar]
- 7.Abbate C, Giorgianni C, Munaò F, Beninato G, D’Arrigo G, D’Arrigo P, et al. Evaluation of obesity in healthcare workers. Med Lav. 2006;97:13–9. [PubMed] [Google Scholar]
- 8.Rampal L, Rampal S, Khor GL, Zain AM, Ooyub SB, Rahmat RB, et al. A national study on the prevalence of obesity among 16,127 Malaysians. Asia Pac J Clin Nutr. 2007;16:561–6. [PubMed] [Google Scholar]
- 9.Sydney: Health Communications; 2000. [Last accessed on 2016 Jan 11]. WHO/IASO/ITO: The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Available from: http://www.wpro.who.int/nutrition/documents/docs/Redefiningobesity.pdf?ua=1 . [Google Scholar]
- 10.Baska T, Straka S, Madar R. Smoking and some life-style changes in medical students – Slovakia, 1995-1999. Cent Eur J Public Health. 2001;9:147–9. [PubMed] [Google Scholar]
- 11.Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Body mass index in young men and the risk of subsequent knee and hip osteoarthritis. Am J Med. 1999;107:542–8. doi: 10.1016/s0002-9343(99)00292-2. [DOI] [PubMed] [Google Scholar]
- 12.Prentice AM, Jebb SA. Obesity in Britain: Gluttony or sloth? BMJ. 1995;311:437–9. doi: 10.1136/bmj.311.7002.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kromhout D. Changes in energy and macronutrients in 871 middle-aged men during 10 years of follow-up (the Zutphen study) Am J Clin Nutr. 1983;37:287–94. doi: 10.1093/ajcn/37.2.287. [DOI] [PubMed] [Google Scholar]
- 14.Atlanta, GA: US Department of Health and Human Services; 1996. US Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. [Google Scholar]
- 15.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289:1785–91. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 16.Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, Jacobs DR, Jr, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet. 2005;365:36–42. doi: 10.1016/S0140-6736(04)17663-0. [DOI] [PubMed] [Google Scholar]


