Abstract
Objective:
To determine gender differences and secular trends in total, low-density lipoprotein (LDL) and high DL (HDL) cholesterol and triglycerides using a large hospital database in India.
Methods:
All blood lipid tests evaluated from July 2007 to December 2014 were analyzed. Details of gender and age were available. Statin therapy was obtained at two separate periods. Trends were calculated using linear regression and Mantel-Haenszel X2.
Results:
Data of 67395 subjects (men 49,904, women 17,491) aged 51 ± 12 years were analyzed. Mean levels (mg/dl) were total cholesterol 174.7 ± 45, LDL cholesterol 110.7 ± 38, non-HDL cholesterol 132.1 ± 44.8, HDL cholesterol 44.1 ± 10, triglycerides 140.8 ± 99, and total: HDL cholesterol 4.44 ± 1.5. Various dyslipidemias in men/women were total cholesterol ≥200 mg/dl 25.4/36.4%, LDL cholesterol ≥130 mg/dl 28.1/35.0% and ≥100 mg/dl 54.4/66.4%, non-HDL cholesterol ≥160 mg/dl 25.5/29.6%, HDL cholesterol <40/50 mg/dl 54.4/64.4%, and triglycerides ≥150 mg/dl 34.0/26.8%. Cholesterol lipoproteins declined over 7 years with greater decline in men versus women for cholesterol (Blinearregression = −0.82 vs. −0.33, LDL cholesterol (−1.01 vs. −0.65), non-HDL cholesterol (−0.88 vs. −0.52), and total: HDL cholesterol (−0.02 vs. −0.01). In men versus women there was greater decline in prevalence of hypercholesterolemia (X2trend 74.5 vs. 1.60), LDL cholesterol ≥130 mg/dl (X2trend 415.5 vs. 25.0) and ≥100 mg/dl (X2trend 501.5 vs. 237.4), non-HDL cholesterol (X2trend 77.4 vs. 6.85), total: HDL cholesterol (X2trend 212.7 vs. 10.5) and high triglycerides (X2trend 10.8 vs. 6.15) (P < 0.01). Use of statins was in 2.6% (36/1405) in 2008 and 9.0% (228/2527) in 2014 (P < 0.01). Statin use was significantly lower in women (5.8%) than men (10.3%).
Conclusions:
In a large hospital - database we observed greater hypercholesterolemia and low HDL cholesterol in women. Mean levels and prevalence of high total, LDL, non-HDL and total: HDL cholesterol declined over 7 years. A lower decline was observed in women. This was associated with lower use of statins.
Keywords: Cardiovascular disease, cholesterol, dyslipidemias
INTRODUCTION
Global burden of metabolic risk factors study reported trends in total cholesterol levels in different countries and world regions from the years 1980 to 2008.[1] It was summarized that while total cholesterol levels increased in low-income and lower-middle income countries over this period, a decline was observed in high-income countries.[2] These trends, however, were derived using mathematical modeling from sparse epidemiological studies in a number of countries.[1] Good quality data were available from high-income countries due to periodic nationwide surveys (e.g., the USA, the UK, Germany, Japan, etc.).[1] On the other hand, in low and lower-middle countries such as India, where most of the cardiovascular and coronary heart disease mortality occurs, high-quality epidemiological data were not available.[2]
In India, only limited studies exist on the epidemiology of cholesterol and other lipoprotein lipids in large samples.[3] We reviewed all the population based epidemiological studies and found that there were only five multisite studies with sample size ranging from 2000 to 10,000.[4,5,6,7,8,9] None of these were prospective or nationally representative. Jaipur Heart Watch (JHW), a series of cross sectional studies in an Indian urban population, reported secular trends in cholesterol, and other lipoproteins over a 20 year period.[10,11] Increasing levels of total cholesterol, low-density lipoprotein (LDL) cholesterol, high DL (HDL) cholesterol, and triglycerides were reported.[11] However, this was a small study. Big data analytic science is set to influence medical research and clinical practice.[12] We used a large hospital based laboratory database of cholesterol lipoproteins and triglycerides at a tertiary care hospital from the year 2007 to 2014 to determine trends in lipid levels and prevalence of hypercholesterolemia in women compared to men. Studies have also reported gender related differences in trends of hypercholesterolemia in developed countries.[13,14,15,16,17,18,19,20,21,22,23] No such data exists in most developing countries, and therefore, we also determined gender related differences in time trends of lipid levels.
METHODS
We performed an audit of consecutively performed lipoprotein lipid levels (total cholesterol, LDL cholesterol, non-HDL cholesterol, HDL cholesterol, ratio of total: HDL cholesterol and triglycerides) available from the health evaluation program at a tertiary care hospital in India. The hospital management committee and research review board approved the protocol. The Institutional Ethics Committee approved the study protocol and permitted the use of anonymized data of the study participants. The Ethics Committee also waivered the need for individual consent and hence this was not obtained. The study was not financially supported by any organization. There are no more data available besides reported in this study. None of the authors have any conflicts of interest.
We analyzed all the lipid profile data from July 2007 to December 2014. Details of gender and age were available for all the subjects while details of disease status or treatment status were not available. Detail of methodology has been reported earlier.[24] To determine disease status or treatment status we performed two studies at various time points (2008 and 2013) over a 1-month period. Successive patients undergoing lipid profile were interviewed to determine disease status with a focus on cardiovascular disease (coronary heart disease, stroke, and peripheral arterial disease) and diabetes and use of lipid-lowering drugs (statins). Serum total cholesterol was estimated using the cholesterol oxidase-peroxidase method, LDL cholesterol was determined with Friedwald's equation from July 2007 to December 2008 and with direct estimation since then using automated LDL by the homogenous enzymatic method. HDL cholesterol was estimated with homogenous enzymatic method and triglycerides using the direct enzymatic method. Internal as well as external validation protocols are regularly performed and the coefficient of variation is <5%, as per the National Accreditation Board for Laboratories, India requirements.[24] The variations were for total cholesterol <2.6%, automated LDL cholesterol <3.8%, automated HDL cholesterol <4.6%, and for triglycerides <4.5%.
Statistical analysis
All the data are available in the computerized database of the hospital. No additional data are available. This database was converted to a user-friendly Microsoft Excel version for analyses. Statistical analyses were performed using SPSS version 13.0 (SPSS Inc. Chicago, IL, USA). Numerical variables are presented as means ± 1 standard deviation while categorical variables are reported as a percent. Triglyceride levels followed a skewed distribution and were also reported as a median and interquartile range (IQR). High cholesterol was defined as ≥200 mg/dl, high LDL cholesterol as ≥130 mg/dl as well as ≥100 mg/dl, high non-HDL cholesterol as ≥160 mg/dl and high total: HDL cholesterol ratio as ≥4.5. Low HDL cholesterol was defined when levels were <40 mg/dl in men and <50 mg/dl in women and high triglycerides by levels ≥150 mg/dl according to US National Cholesterol Education Program report.[25] Age and gender-specific analyses were performed. Secular trends in various mean levels of cholesterol lipoprotein lipids were determined with linear regression for continuous variables using SPSS and B values (95% confidence intervals, CI) are reported. Trends in categorical variables have been analyzed using Mantel-Haenszel X2 for trend. P < 0.05 was considered significant.
RESULTS
Details of fasting lipid profile were available in 67395 subjects (men 49,904, women 17,491). The mean age of study participants was 51 ± 12 years. Mean levels of cholesterol lipoproteins in the whole group were: Total cholesterol 174.7 ± 45.8 mg/dl, LDL cholesterol 110.7 ± 38.5 mg/dl, non-HDL cholesterol 132.1 ± 44.8 mg/dl, HDL cholesterol 44.1 ± 10.4 mg/dl, triglycerides 140.8 ± 99.2 mg/dl (median 118, IQR 85–166 mg/dl) and total: HDL cholesterol 4.44 ± 1.55. Mean levels in men versus women were total cholesterol 169.2 ± 46.5 versus 185.5 ± 43.9 mg/dl (P < 0.001), LDL cholesterol 106.2 ± 38.9 versus 116.1 ± 37.4 mg/dl (P < 0.001), non-HDL cholesterol 129.7 ± 45.2 versus 139.0 ± 42.8 mg/dl (P < 0.001), HDL cholesterol 39.4 ± 9.7 versus 46.4 ± 11.6 mg/dl (P < 0.001), triglycerides 144.5 ± 111.8 versus 128.3 ± 90.6 mg/dl (median, IQR 121, 87–171 vs. 111, 81–153 mg/dl) (P < 0.001), and total: HDL cholesterol 4.5 ± 1.6 versus 4.2 ± 1.5 (P < 0.001).
Age-specific levels in the overall participants is shown in Table 1. Data show that with age there is an increase in total cholesterol, LDL cholesterol, non-HDL cholesterol and triglyceride levels from age groups <20 years to 30–39 years followed by a decline. Highest levels of cholesterol related lipoproteins and triglycerides are at age 30–49 years [Table 1]. Levels of HDL increase with age while total: HDL cholesterol ratio shows a declining trend. Age-related trends are not different in men and women [Supplementary Tables 1 (316.5KB, tif) and 2 (316.5KB, tif) ]. However, levels of total, LDL and non-HDL cholesterol levels and triglycerides peak earlier in men as compared to women [Figure 1]. Levels of cholesterol and its lipoproteins are the highest at age 30–39 in men and 50–59 in women. HDL cholesterol levels are greater among women at all age-groups.
Table 1.
Age-specific levels of various cholesterol lipoproteins and triglycerides in the study population
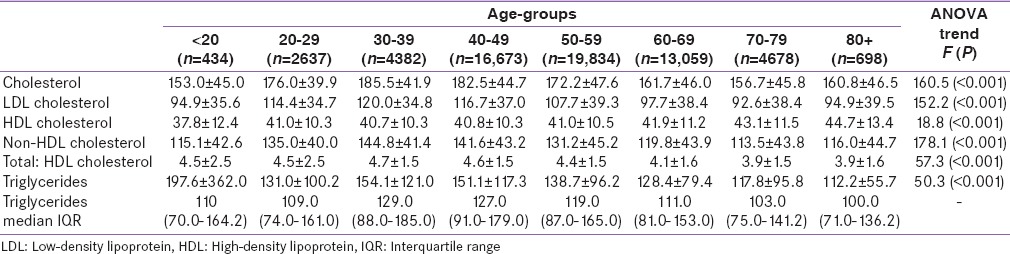
Figure 1.
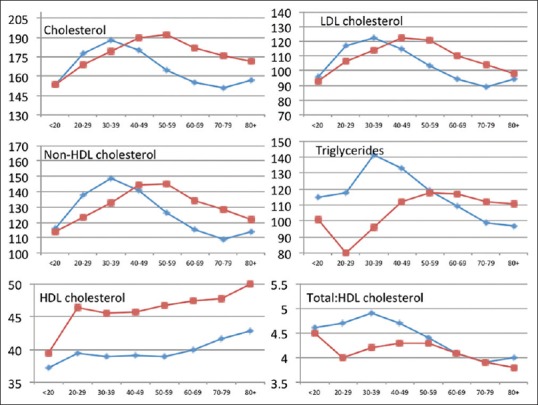
Age-related trends in mean levels of total cholesterol, low-density lipoprotein cholesterol, nonhigh-density lipoprotein cholesterol, high-density lipoprotein cholesterol and total: high-density lipoprotein cholesterol and median levels of triglycerides in the study population. Mean levels in cholesterol lipoproteins are significantly greater among women after age of 50 years. Mean total, low-density lipoprotein and non-high density lipoprotein cholesterol levels are the highest in men at age 30–39 years and in women at 40–59 years
Age-specific levels of various cholesterol lipoproteins and triglycerides in men
Age-specific levels of various cholesterol lipoproteins and triglycerides in women
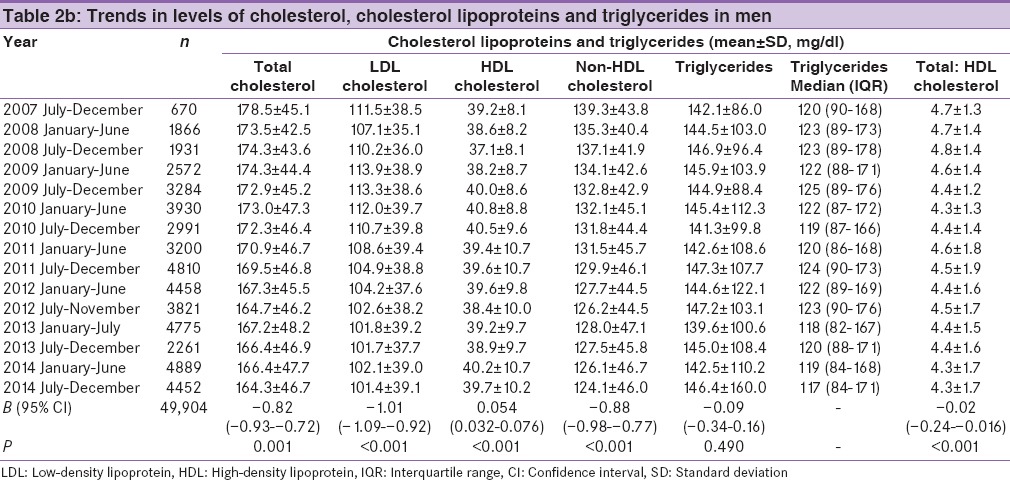
Mean levels of various cholesterol lipoproteins and triglycerides at half-yearly intervals form July 2007 to December 2014 in the overall population and in men and women shown in Tables 2a-c, respectively. In the overall population, significant decline is observed in total cholesterol (linear regression analysis, B = −0.73, P < 0.001), LDL cholesterol (B = 0.93, P < 0.001), non-HDL cholesterol (B = 0.80, P < 0.001) and total: HDL cholesterol (B= −0.02, P < 0.001). Levels of HDL cholesterol show an increase (B = 0.74, P < 0.001) while no significant change is observed in triglycerides (B= −0.06, P = 0.545). Gender specific regression analysis reveals that in men versus women there is a significantly greater decline in mean levels of total cholesterol (B = −0.82 vs. −0.33), LDL cholesterol (B = −1.01 vs. −0.65), non-HDL cholesterol (B = −0.88 vs. −0.52), and total: HDL cholesterol (B = −0.02 vs. −0.01) (P < 0.05) while no significant differences are observed in trends in HDL cholesterol (B = 0.05 vs. 0.18) and triglycerides (B = −0.09 vs. −0.12) [Table 2b and c].
Table 2a.
Trends in mean levels of cholesterol, cholesterol lipoproteins and triglycerides in the study population
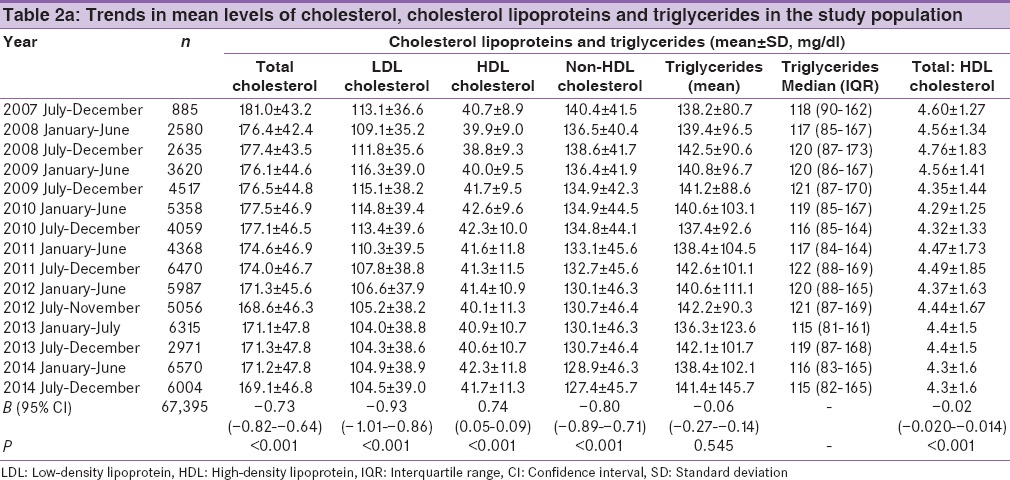
Table 2c.
Trends in levels of cholesterol, cholesterol lipoproteins and triglycerides in women
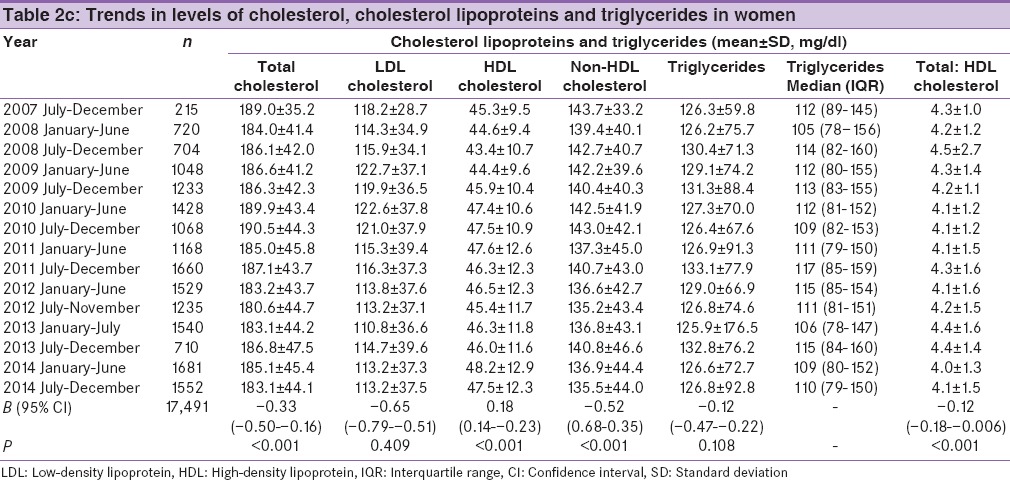
Table 2b.
Trends in levels of cholesterol, cholesterol lipoproteins and triglycerides in men
We also determined prevalence of various dyslipidemias in the study population [Figure 2]. Prevalence in men versus women, respectively, is total cholesterol ≥200 mg/dl in 25.4 versus 35.6%, LDL cholesterol ≥130 mg/dl in 28.1 versus 35.1%, LDL cholesterol ≥100 mg/dl in 54.4 versus 66.4%, non-HDL cholesterol ≥160 mg/dl in 25.5 vs. 29.6%, HDL cholesterol <40/50 mg/dl in 54.9 versus 64.4%, triglycerides ≥150 mg/dl in 33.9 versus 26.8% and high total: HDL cholesterol ≥4.5 in 45.1 versus 36.4% (P < 0.05). Prevalence of high total cholesterol, high LDL cholesterol, high non-HDL cholesterol, and low HDL cholesterol are significantly greater in women [Figure 2].
Figure 2.
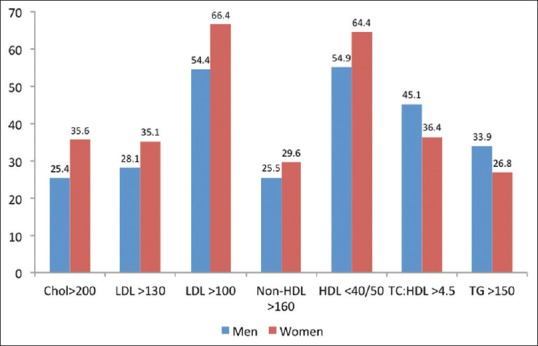
Prevalence of various dyslipidemias in the study population. Prevalence of high total cholesterol >200 mg/dl, high low-density lipoprotein cholesterol >130 mg/dl and >100 mg/dl, high non-high density lipoprotein cholesterol >160 mg/dl, and low high-density lipoprotein cholesterol in greater in women while high total: high-density lipoprotein cholesterol >4.5 and high triglycerides >150 mg/dl is significantly greater in women
Time trends in the prevalence of various dyslipidemias are shown in Table 3. Significant secular decline in prevalence of high total cholesterol (≥200 mg/dl), high LDL cholesterol (≥100 mg/dl or ≥130 mg/dl), and high non-HDL cholesterol (≥160 mg/dl) was observed. Trends in prevalence of dyslipidemias in men and women are reported in Supplementary Tables 3 (589.2KB, tif) and 4 (585.3KB, tif) . In men versus women [Figure 3], greater decline is observed in prevalence of high cholesterol (X2trend 74.5 vs. 1.60), LDL cholesterol ≥130 mg/dl (X2trend 415.5 vs. 25.0), LDL cholesterol ≥100 mg/dl (X2trend 501.5 vs. 237.4), high non-HDL cholesterol (X2trend 77.4 vs. 6.85), high total: HDL cholesterol (X2trend 212.7 vs. 10.5) and high triglycerides (X2trend 10.8 vs. 6.15) (P < 0.01).
Table 3.
Trends in prevalence of various dyslipidemias in the study cohort
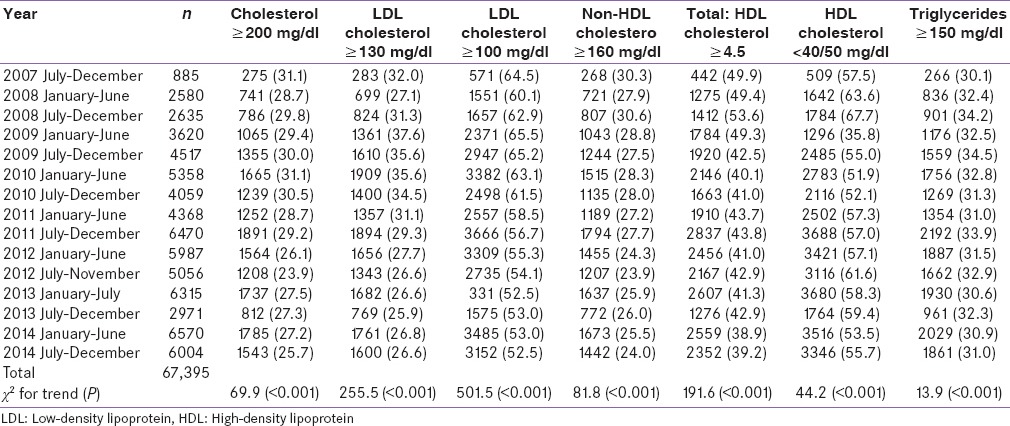
Figure 3.
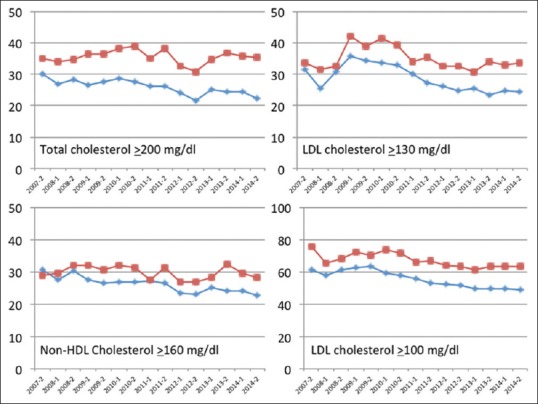
Secular trends in the prevalence of various dyslipidemias in men and women from 2007 to 2014. Among men, there is a greater decline in high total cholesterol, high low-density lipoprotein cholesterol 100 mg/dl, high non-high density lipoprotein cholesterol and high total: high-density lipoprotein cholesterol as compared to women
Trends in prevalence of various dyslipidemias in men
Trends in prevalence of various dyslipidemias in women
To determine the influence of cholesterol-lowering drug therapy (statins) on lipid levels we performed two sub-studies among a sub-sample of study participants in March 2008 (n = 1405) and August 2013 (n = 2527). In the first study, use of statins was in 36 (2.6%) and was in 228 (9.0%) in the second (P < 0.01). Statin use was significantly lower in women (5.8%) as compared to men (10.3%) (P < 0.01).
DISCUSSION
This study shows that in a large hospital - based database at a tertiary care hospital in India women, as compared to men, had higher levels of total cholesterol, LDL cholesterol and non-HDL cholesterol and greater prevalence of these dyslipidemias. Over a 7 year period, declining trends in mean levels and prevalence of high total cholesterol, LDL cholesterol, and non-HDL cholesterol were observed. The decline was significantly less in women as compared to men. There was a significant increase in the use of statins over this period but was significantly lower in women as compared to men.
Mean levels of various cholesterol lipoprotein lipids in the present study are not very dissimilar to previous studies in urban populations in India.[4,6,7,8,9] Prevalence of various dyslipidemias, especially LDL cholesterol ≥100 mg/dl and hypertriglyceridemia is greater than previous studies while the prevalence of low HDL cholesterol is lower. We have earlier reported that prevalence of various dyslipidemias in the hospital based data are not similar to population-based studies[24] and this study shows similar findings. However, the prevalence of dyslipidemias, especially high total, LDL and non-HDL cholesterol is much lower than studies from the USA[25,26] and other developed countries.[1,27]
Declining trends in lipid levels observed in the present analysis is similar to data from high-income countries in the global burden of metabolic risk factors study.[1] Although no uniform data were obtained on use of statins in this large study, sub-sample analysis at time-periods at the beginning and end of the study shows an almost trebling in use of lipid lowering drugs (statins) from 2.6 to 9.0%. It is hypothesized that declining trends in cholesterol levels in the present study is due to greater use of statins along with changing lifestyles with healthier diets in this largely middle class cohort.[1,2] Although we performed sub-sample analysis, in absence of regularly collected data we cannot be emphatic of this finding and this is a major study limitation. However, these are limitation of big data analyses performed in this study. Mayer–Schonberger and Cukier have commented that although correlations can be reported mathematically using big data we cannot easily explain the reason/s behind correlations.[28] Causality will not be discarded, but it is being knocked off its pedestal as the primary fountain of meaning.[28] Studies from India have reported a low use of statins for primary and secondary prevention at secondary and primary care as well in community based samples.[29,30] On the other hand, secular trends in statin use report an increasing consumption of these drugs in India.[31] The declining trend in cholesterol and its lipoproteins in the present study are also different from the JHW studies.[10,11] In these cross sectional studies, marginally increasing trend was observed in the total cholesterol, LDL cholesterol and total: HDL cholesterol ratio and a significant increase was observed in triglycerides.[10] The populations studies are different in the present study where in lipid profiles were evaluated at a tertiary care hospital based primary and secondary prevention program while the JHW studies were population-based in the Jaipur population[10] or in the middle class.[11] Increase in cholesterol has also been reported in a series of two cross sectional studies in Delhi.[32]
Greater prevalence of dyslipidemias in women, especially after the middle-age as observed in this study is similar to previous international data.[26,33] It has been reported that from ages 20–55 years men tend to have higher cholesterol levels but after this age the cholesterol levels increase rapidly in women and exceed those in men. However, in our study, this changeover occur 10 years earlier [Figure 1]. This may be related to earlier age of menopause in Indian women compared to the US counterparts, this may also be due to premature development of greater cardiovascular risk in Indian women due to a lower age at menopause.[34] Women lifelong have higher levels of HDL cholesterol which is similar to this study. Gender-related difference in decline of cholesterol lipoproteins in the present study is an important finding. Similar differences in trends in cholesterol lipoproteins have been reported in observational studies in the US and other developed countries.[13,15,16,22,23] Lesser focus on prevention in women and lower use of statins may also be important.[14,17,20] Gender disparities in use of statins has also been reported in coronary secondary prevention studies[18,21] including from India.[35]
This study has strength as well as multiple limitations. We used a large hospital based database and simple statistical analyses have provided useful results. However, this is a hospital based study and the results cannot be extrapolated and generalized to all populations. Moreover, the mean cholesterol levels as well as prevalence of various dyslipidemias are greater than general populations in Jaipur[10] and elsewhere in India.[3,6] We do not have data on other risk factors (body mass index, abdominal obesity, hypertension, etc.) disease status (diabetes, previous coronary disease or interventions) or treatment status and this is an important limitation. However, sub-study has shown increasing use of statins in this populations and points to either increased awareness of cholesterol as risk factor or higher levels of treatment. However, despite this limitation this study shows a gender-related difference in secular trends in cholesterol related lipoproteins. This highlights gender disparities and possible lower intensity cholesterol management among women. Greater mortality in women following an acute coronary event has been reported in India[36] and this study points to disparities in cholesterol management as an important reason.
This study also shows the important of big data analytics in medicine. It has been forecasted that such analyses shall change the future course of medical science, which is poised to become predictive and preventive rather than reactive.[12] Cardiovascular diseases are the most important cause of mortality and morbidity among women in India,[37] lipid abnormalities are the most important risk factor,[38] and gender-based differences in trends in lipids levels at a tertiary care primary and secondary prevention clinics highlights the importance of equitable lipid management among women in India.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Farzadfar F, Finucane MM, Danaei G, Pelizzari PM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in serum total cholesterol since 1980: Systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet. 2011;377:578–86. doi: 10.1016/S0140-6736(10)62038-7. [DOI] [PubMed] [Google Scholar]
- 2.Anand SS, Yusuf S. A global tsunami of cardiovascular risk. Lancet. 2011;377:502–5. doi: 10.1016/S0140-6736(10)62346-X. [DOI] [PubMed] [Google Scholar]
- 3.Gupta R, Guptha S, Sharma KK, Gupta A, Deedwania P. Regional variations in cardiovascular risk factors in India: India heart watch. World J Cardiol. 2012;4:112–20. doi: 10.4330/wjc.v4.i4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reddy KS, Prabhakaran D, Chaturvedi V, Jeemon P, Thankappan KR, Ramakrishnan L, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. 2006;84:461–9. doi: 10.2471/blt.05.027037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kinra S, Bowen LJ, Lyngdoh T, Prabhakaran D, Reddy KS, Ramakrishnan L, et al. Sociodemographic patterning of non-communicable disease risk factors in rural India: A cross sectional study. BMJ. 2010;341:c4974. doi: 10.1136/bmj.c4974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah B, Mathur P. Surveillance of cardiovascular disease risk factors in India: The need and scope. Indian J Med Res. 2010;132:634–42. doi: 10.4103/0971-5916.73420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pandey RM, Gupta R, Misra A, Misra P, Singh V, Agrawal A, et al. Determinants of urban-rural differences in cardiovascular risk factors in middle-aged women in India: A cross-sectional study. Int J Cardiol. 2013;163:157–62. doi: 10.1016/j.ijcard.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Guptha S, Gupta R, Deedwania P, Bhansali A, Maheshwari A, Gupta A, et al. Cholesterol lipoproteins and prevalence of dyslipidemias in urban Asian Indians: A cross sectional study. Indian Heart J. 2014;66:280–8. doi: 10.1016/j.ihj.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Joshi SR, Anjana RM, Deepa M, Pradeepa R, Bhansali A, Dhandania VK, et al. Prevalence of dyslipidemia in urban and rural India: The ICMR-INDIAB study. PLoS One. 2014;9:e96808. doi: 10.1371/journal.pone.0096808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta R, Guptha S, Agrawal A, Kaul V, Gaur K, Gupta VP. Secular trends in cholesterol lipoproteins and triglycerides and prevalence of dyslipidemias in an urban Indian population. Lipids Health Dis. 2008;7:40. doi: 10.1186/1476-511X-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta R, Guptha S, Gupta VP, Agrawal A, Gaur K, Deedwania PC. Twenty-year trends in cardiovascular risk factors in India and influence of educational status. Eur J Prev Cardiol. 2012;19:1258–71. doi: 10.1177/1741826711424567. [DOI] [PubMed] [Google Scholar]
- 12.Canton J, editor. Future Smart: Managing the Game Changing Trends that Will Transform your World. Philadelphia, USA: De Capo Press; 2015. The future of medicine: From prevention to regeneration; pp. 218–39. [Google Scholar]
- 13.Green MS, Heiss G, Rifkind BM, Cooper GR, Williams OD, Tyroler HA. The ratio of plasma high-density lipoprotein cholesterol to total and low-density lipoprotein cholesterol: Age-related changes and race and sex differences in selected North American populations. The Lipid Research Clinics Program Prevalence Study. Circulation. 1985;72:93–104. doi: 10.1161/01.cir.72.1.93. [DOI] [PubMed] [Google Scholar]
- 14.Winkleby MA, Feldman HA, Murray DM. Joint analysis of three U.S. community intervention trials for reduction of cardiovascular disease risk. J Clin Epidemiol. 1997;50:645–58. doi: 10.1016/s0895-4356(97)00020-6. [DOI] [PubMed] [Google Scholar]
- 15.Szklo M, Chambless LE, Folsom AR, Gotto A, Jr, Nieto FJ, Patsch W, et al. Trends in plasma cholesterol levels in the atherosclerosis risk in communities (ARIC) study. Prev Med. 2000;30:252–9. doi: 10.1006/pmed.1999.0612. [DOI] [PubMed] [Google Scholar]
- 16.Ferrario M, Sega R, Chatenoud L, Mancia G, Mocarelli P, Crespi C, et al. Time trends of major coronary risk factors in a northern Italian population (1986-1994). How remarkable are socioeconomic differences in an industrialized low CHD incidence country? Int J Epidemiol. 2001;30:285–97. doi: 10.1093/ije/30.2.285. [DOI] [PubMed] [Google Scholar]
- 17.Reibis RK, Bestehorn K, Pittrow D, Jannowitz C, Wegscheider K, Völler H. Elevated risk profile of women in secondary prevention of coronary artery disease: A 6-year survey of 117,913 patients. J Womens Health (Larchmt) 2009;18:1123–31. doi: 10.1089/jwh.2008.1082. [DOI] [PubMed] [Google Scholar]
- 18.Dallongevillle J, De Bacquer D, Heidrich J, De Backer G, Prugger C, Kotseva K, et al. Gender differences in the implementation of cardiovascular prevention measures after an acute coronary event. Heart. 2010;96:1744–9. doi: 10.1136/hrt.2010.196170. [DOI] [PubMed] [Google Scholar]
- 19.Johansson I, Nilsson LM, Stegmayr B, Boman K, Hallmans G, Winkvist A. Associations among 25-year trends in diet, cholesterol and BMI from 140,000 observations in men and women in Northern Sweden. Nutr J. 2012;11:40. doi: 10.1186/1475-2891-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vimalananda VG, Miller DR, Hofer TP, Holleman RG, Klamerus ML, Kerr EA. Accounting for clinical action reduces estimates of gender disparities in lipid management for diabetic veterans. J Gen Intern Med. 2013;28(Suppl 2):S529–35. doi: 10.1007/s11606-013-2340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh M, Chin SH, Crothers D, Giles P, Al-Allaf K, Khan JM. Time trends of gender-based differences in lipid goal attainments during secondary prevention of coronary artery disease: Results of a 5-year survey. Am J Ther. 2013;20:613–7. doi: 10.1097/MJT.0b013e31824c3e8c. [DOI] [PubMed] [Google Scholar]
- 22.Eggen AE, Mathiesen EB, Wilsgaard T, Jacobsen BK, Njølstad I. Trends in cardiovascular risk factors across levels of education in a general population: Is the educational gap increasing?. The Tromsø study 1994-2008. J Epidemiol Community Health. 2014;68:712–9. doi: 10.1136/jech-2013-203428. [DOI] [PubMed] [Google Scholar]
- 23.Hulmán A, Tabák AG, Nyári TA, Vistisen D, Kivimäki M, Brunner EJ, et al. Effect of secular trends on age-related trajectories of cardiovascular risk factors: The Whitehall II longitudinal study 1985-2009. Int J Epidemiol. 2014;43:866–77. doi: 10.1093/ije/dyt279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maheshwari P, Sharma M, Sharma KK, Roy M, Goyal NK, Mishra BS, et al. Equivalence of cholesterol levels at hospital based health-check program with population based studies: A comparative study. J Clin Prev Cardiol. 2013;2:1–7. [Google Scholar]
- 25.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 26.Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988-2010. JAMA. 2012;308:1545–54. doi: 10.1001/jama.2012.13260. [DOI] [PubMed] [Google Scholar]
- 27.Geneva: World Health Organization; 2014. World Health Organization. Global Status Report of Non-Communicable Diseases 2014. [Google Scholar]
- 28.Mayer-Schonberger V, Cukier K, editors. Big Data: A Revolution that Will Transform How We Live, Work and Think. London: John Murray Publishers; 2013. Correlation; pp. 50–72. [Google Scholar]
- 29.Sharma KK, Gupta R, Agrawal A, Roy S, Kasliwal A, Bana A, et al. Low use of statins and other coronary secondary prevention therapies in primary and secondary care in India. Vasc Health Risk Manag. 2009;5:1007–14. doi: 10.2147/vhrm.s8017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yusuf S, Islam S, Chow CK, Rangarajan S, Dagenais G, Diaz R, et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): A prospective epidemiological survey. Lancet. 2011;378:1231–43. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 31.Choudhry NK, Dugani S, Shrank WH, Polinski JM, Stark CE, Gupta R, et al. Despite increased use and sales of statins in India, per capita prescription rates remain far below high-income countries. Health Aff (Millwood) 2014;33:273–82. doi: 10.1377/hlthaff.2013.0388. [DOI] [PubMed] [Google Scholar]
- 32.Roy A, Praveen PA, Gupta R, Lakshmy R, Krishnan A, Prabhakaran D. Twenty year trends in cardiovascular risk factors in urban Delhi, India. J Am Coll Cardiol. 2013;61:E1351. Abstract. [Google Scholar]
- 33.Watson KE. Women. In: Wong ND, Black HR, Gardin JM, editors. Preventive Cardiology: A Practical Approach. 2nd ed. New York: McGraw Hill; 2005. pp. 384–98. [Google Scholar]
- 34.Mozumdar A, Agrawal PK. Prevalence, trends, and determinants of menopause in India: NFHS 1992-93 to NFHS 2005-06. Am J Hum Biol. 2015;27:421–5. doi: 10.1002/ajhb.22648. [DOI] [PubMed] [Google Scholar]
- 35.Sharma KK, Gupta R, Basniwal PK, Guptha S, Gupta R. Age and gender disparities in evidence-based treatment for coronary artery disease in the community: A cross-sectional study. Indian J Community Med. 2011;36:159–60. doi: 10.4103/0970-0218.84138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pais P, Xavier D, Gupta R, Sigamani A, George N, Thomas S, et al. Gender differences in presentation, treatments and outcomes of over 20,000 acute coronary syndrome patients in India: The CREATE registry. Circulation. 2012;125:E780. Abstract. [Google Scholar]
- 37.Gupta R, Joshi P, Mohan V, Reddy KS, Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 38.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–94. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Age-specific levels of various cholesterol lipoproteins and triglycerides in men
Age-specific levels of various cholesterol lipoproteins and triglycerides in women
Trends in prevalence of various dyslipidemias in men
Trends in prevalence of various dyslipidemias in women


