Abstract
Background:
Molar incisor hypomineralization (MIH) is a developmental defect. The prevalence of MIH ranges widely from 2.4% to 40.2%.
Aim:
This study was under taken to determine the prevalence of MIH in 7–9-year-old children of Bengaluru City, India.
Materials and Methods:
A cross-sectional epidemiological study was conducted in a representative sample of 2500 school children aged 7–9 years of Bengaluru, India. Oral examination was carried out by a single trained calibrated examiner under natural daylight.
Results:
Twelve children (0.48%) were diagnosed with MIH. A total of 68 teeth were observed with MIH. All four first permanent molars were affected in 50% of children. In the molar group, mandibular molars (29.41%) were more frequently affected than maxillary molars (27.94%).
Conclusion:
The prevalence of MIH in 7–9-year-old children of Bengaluru was 0.48%, with no gender predilection.
Keywords: Childhood illness, molar incisor hypomineralization, prevalence
Introduction
Molar incisor hypomineralization (MIH) is the result of a variety of environmental factors affecting the developing enamel, with an underlying genetic predisposition.[1] Occurrence of disturbed ameloblast function in the later mineralization phase of amelogenesis results in defective enamel with a significantly increased protein content.[2] Due to the varied pattern exhibited by affected molars and incisors, the causative disturbances could take place between the end of the second gestational trimester and up to the age of 4 years.[3]
Various terms have been used to refer to hypomineralized molars, such as nonfluoride enamel opacities, internal enamel hypoplasia, nonendemic mottling of enamel, opaque spots, idiopathic enamel opacities, enamel opacities, and cheese molars. It was in 2001 that Weerheijm et al. coined the term MIH.[4]
Clinically hypomineralization can be seen as an abnormality in the translucency of enamel. The enamel of MIH molars looks soft and porous and has the appearance of discolored chalk or old Dutch cheese. Demarcated opacities of a different color, that is, opacities with a clear and distinct border can be seen adjacent to enamel.[5] MIH is related to unexpected rapid caries development in the erupting first permanent molars. During brushing, children experience pain and hypersensitivity even when the enamel is intact.[5]
Many risk factors have been related to MIH including problems during gestation, preterm delivery, cyanosis, diseases of early childhood such as chickenpox, otitis media, urinary tract infections, tonsillitis, high fever, gastrointestinal disorders and frequent use of antibiotics.[6,7,8,9,10] These conditions probably cause an alteration in the calcium-phosphate balance or insufficient oxygen supply to ameloblasts leading to enamel defects.[6]
Worldwide prevalence of MIH shows a wide variation ranging from 2.4% to 40%.[6,7,8,9,10] This is because of differences in the criteria used to diagnose MIH in earlier studies.[6,7,11] Many prevalence studies on MIH have been carried out in European countries.[4,5,6,7] There is not much published data on MIH in India.[9,10,12] In national epidemiological surveys on the prevalence of dental caries in India, children are not routinely examined for the presence of MIH. This study was under taken to determine the prevalence of MIH in 7–9-year-old children of Bengaluru City and to evaluate its association with childhood illness and usage of drugs.
Materials and Methods
A cross-sectional epidemiological study was conducted on a random sample of 2500 normal -healthy school children aged between 7 and 9 years, in Bengaluru, India. The sample size was calculated according to the WHO guidelines at 95% of confidence level with a relative precision (α) of 5%.[13]
Ethical clearance to conduct the study was obtained from the institutional review board. Prior to the commencement of the study, a list of all schools in Bengaluru (urban) was obtained from the deputy director of public instruction office. The city was divided geographically into five different zones: North, South, East, West and Central. Random selections of six schools, both private and public, from each of these five zones of Bengaluru were selected. Permission was taken from the school authorities to carry out an oral examination of the children. The nature of the study was explained to parents, and their written consent was taken for participation in the study. Children wearing fixed appliances, which interfere with evaluation of index teeth, were excluded.
The oral examination was carried out by a single trained calibrated examiner under natural daylight with sterilized disposable mouth mirror and blunt probe. An average of fifty children was examined per day. MIH was diagnosed using criteria given by Weerheijm et al.[8] Every surface of the incisors and permanent first molar were examined and the relevant diagnostic code was recorded on the odontogram. A questionnaire was given only to parents of children with MIH in order to record medical history of the mother during the pregnancy, childbirth, and infancy.
Ten percent of children were re-examined after 1 month by the same investigator. The resulting weighted Cohen's Kappa coefficient was 0.95, indicating a very high level of agreement. Data obtained were subjected to statistical analysis using Statistical Package for the Social Sciences (SPSS 20.0 version, Delaware, Chicago, IL, USA). Means were compared using Student's t-test and ANOVA, and the Chi-square test was used for proportion comparison. The significance level was considered as P ≤ 0.05.
Results
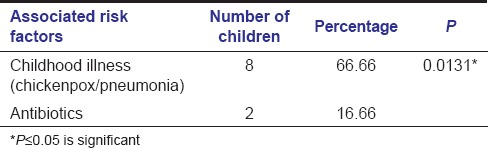
The distribution of children is given in Table 1. Twelve children (0.48%) presented with MIH. In total, 29 incisors and 39 molars were affected. A higher number of maxillary incisors (16) were involved [Table 2]. A higher number (40) of children presented only with molar hypomineralization (MH). Six children had all 4first permanent molars affected with hypomaturation [Table 3]. There were more number of molars affected in the mandibular arch (55%) [Table 4]. A significant association was observed between childhood illness and MIH (P ≤ 0.05) [Table 5].
Table 1.
Percentage of children with molar incisor hypomineralization and molar hypomineralization
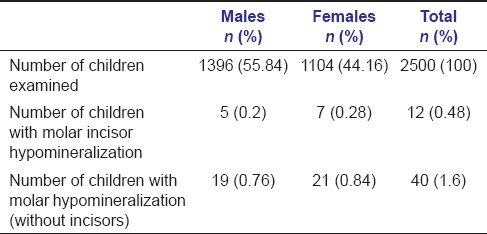
Table 2.
Distribution of molars and incisors affected with molar incisor hypomineralization
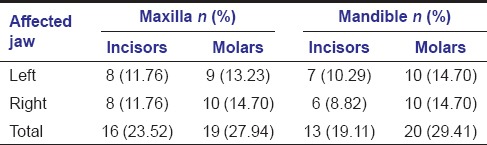
Table 3.
Percentage distribution of children according to frequency of hypomineralization
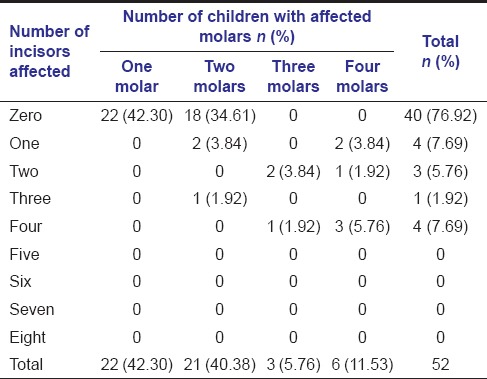
Table 4.
Distribution of first permanent molars affected with hypomineralization
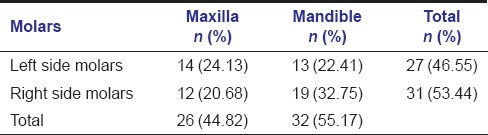
Table 5.
Association of childhood illness and use of drugs with molar incisor hypomineralization
Discussion
Enamel defects are alterations that can affect a single tooth or group of similar teeth [Figures 1-3]. This anomaly can involve only the primary or permanent teeth, or even both dentitions. Any systemic, local, or genetic factor that can cause an imbalance during the maturation phase of amelogenesis results in hypomineralization.[14] Hypomineralization is a qualitative defect visually identified as an anomaly of enamel translucency, also called enamel opacity [Figures 1 and 2].[15]
Figure 1.

Molar incisor hypomineralization-demarcated opacity in relation to incisors
Figure 3.

Molar incisor hypomineralization-posteruptive enamel breakdown in relation to incisors
Figure 2.

Molar incisor hypomineralization- showing incisors with demarcated opacities
Enamel of the MIH affected molars is intact at the stage of tooth eruption but structurally it is soft and porous. Often it breaks down immediately after eruption, leaving unprotected dentin exposed to the oral environment and leading to rapid caries development [Figures 4-5]. MIH leads to a number of problems like poor esthetics, food retention in the defective enamel area, and higher sensitivity of the exposed dentine. Therefore, the presence of MIH requires dentists to identify this problem at the earliest.[1]
Figure 4.

Molar incisor hypomineralization-demarcated opacity involving first permanent molar
Figure 5.

MIH-showing breakdown of dentin
Epidemiological studies from the late 1970s until date have been largely conducted in countries in Europe. Very few studies have been published on the prevalence of MIH in Asia, with the prevalence of 2.8% in Hong Kong Chinese children[16] and 12.7% in Iranian children.[17] India, with a population of 1.21 billion people, has more than 35% of the population below the age of 15 years.[18] However, there have been no reports on the prevalence of MIH in Indian children in the last two decades.
Children of 7–9 years were selected because all four first permanent molars and incisors would have erupted into the oral cavity. At an older age, there would be a risk of posteruptive enamel breakdown and caries initiation.
There has been a great variation in the worldwide prevalence of MIH.[5,7,16,19,20,21] Two Indian studies have reported the prevalence of MIH to be 9.3% in Gujarat[12] and 6.31% in Chandigarh.[9] The prevalence of MIH in our study was found to be lower probably due to strict adherence to the criteria given by the European Archives of Paediatric Dentistry[8] while recording MIH. The inclusion of older children in the study group could result in higher prevalence figures.[16,21,22]
As with earlier reports[16,23] on MIH, gender predilection was evident in this study. In accordance with certain studies,[10,19,24] a higher prevalence of MH (1.6%) over MIH (0.48%) was observed. Other studies have shown contradictory findings.[9,12,22] In the present study, mandibular molars were more affected than maxillary molars. It could be due to earlier eruption of mandibular molars.[25]
MIH is the result of a variety of environmental factors acting systemically during prenatal, perinatal periods and during childhood.[1] Though several risk factors have been associated with the cause of MIH, the etiology has not been understood fully yet. Factors that cause an alteration in the calcium-phosphate balance or insufficient oxygen supply to ameloblasts can lead to enamel defects.[6]
Acute health illness such as pneumonia, upper respiratory tract infection, otitis media, chickenpox, tonsillitis, and episodes of high fever have been considered as important risk factors in the occurrence of MIH.[11,22,26,27,28] In our study, MIH was significantly associated with early childhood illness (chickenpox/pneumonia) and drug intake.
Chickenpox is caused by the herpes family of viruses. It is possible that the epithelial-derived ameloblasts at the maturation phase are also affected. Since enamel is not capable of remodeling, scarring may occur and clinically present as opacities. The patchy distribution of chickenpox skin lesions could be akin to the asymmetric distribution of MIH defects.[26]
In the present study, almost 17% of children with MIH were given antibiotics during their early childhood, at around 2 years of age. Since antibiotics are in most cases related to the occurrences of a disease, it is difficult to distinguish MIH was caused by antibiotic use or by the disease per se,[8] or a combination of both factors. Animal studies done on ameloblasts exposed to amoxicillin suggested that higher concentration of the drug altered the pattern of ameloblasts and thus interfered with mineralization of the tooth.[29,30]
The present study was cross-sectional in nature and information obtained relied on retrospective data in the form of a questionnaire given to the parents. The association of risk factors was recorded based on the ability of parents to recall the occurrence of early childhood illness and history of drug intake. It is difficult to obtain detailed information regarding minor complaints of short duration and medications used without medical consultation. There is definitely a need to determine the prevalence of MIH throughout India.
Conclusion
The prevalence of MIH in 7–9-year-old children of Bengaluru City, India was 0.48%, with no gender predilection. MIH was significantly associated with early childhood illness like chickenpox/pneumonia and intake of antibiotics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Willmott NS, Bryan RA, Duggal MS. Molar-incisor-hypomineralisation: A literature review. Eur Arch Paediatr Dent. 2008;9:172–9. doi: 10.1007/BF03262633. [DOI] [PubMed] [Google Scholar]
- 2.Mangum JE, Crombie FA, Kilpatrick N, Manton DJ, Hubbard MJ. Surface integrity governs the proteome of hypomineralized enamel. J Dent Res. 2010;89:1160–5. doi: 10.1177/0022034510375824. [DOI] [PubMed] [Google Scholar]
- 3.Suckling GW, Herbison GP, Brown RH. Etiological factors influencing the prevalence of developmental defects of dental enamel in nine-year-old New Zealand children participating in a health and development study. J Dent Res. 1987;66:1466–9. doi: 10.1177/00220345870660091101. [DOI] [PubMed] [Google Scholar]
- 4.Weerheijm KL, Jälevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35:390–1. doi: 10.1159/000047479. [DOI] [PubMed] [Google Scholar]
- 5.Weerheijm KL. Molar incisor hypomineralisation (MIH) Eur J Paediatr Dent. 2003;4:114–20. [PubMed] [Google Scholar]
- 6.Dietrich G, Sperling S, Hetzer G. Molar incisor hypomineralisation in a group of children and adolescents living in Dresden (Germany) Eur J Paediatr Dent. 2003;4:133–7. [PubMed] [Google Scholar]
- 7.Jälevik B. Prevalence and diagnosis of molar-incisor-hypomineralisation (MIH): A systematic review. Eur Arch Paediatr Dent. 2010;11:59–64. doi: 10.1007/BF03262714. [DOI] [PubMed] [Google Scholar]
- 8.Weerheijm KL, Duggal M, Mejàre I, Papagiannoulis L, Koch G, Martens LC, et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: A summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110–3. [PubMed] [Google Scholar]
- 9.Mittal NP, Goyal A, Gauba K, Kapur A. Molar incisor hypomineralisation: Prevalence and clinical presentation in school children of the northern region of India. Eur Arch Paediatr Dent. 2014;15:11–8. doi: 10.1007/s40368-013-0045-4. [DOI] [PubMed] [Google Scholar]
- 10.Chawla N, Messer LB, Silva M. Clinical studies on molar-incisor-hypomineralisation part 1: Distribution and putative associations. Eur Arch Paediatr Dent. 2008;9:180–90. doi: 10.1007/BF03262634. [DOI] [PubMed] [Google Scholar]
- 11.Jälevik B, Klingberg G, Barregård L, Norén JG. The prevalence of demarcated opacities in permanent first molars in a group of Swedish children. Acta Odontol Scand. 2001;59:255–60. doi: 10.1080/000163501750541093. [DOI] [PubMed] [Google Scholar]
- 12.Parikh DR, Ganesh M, Bhaskar V. Prevalence and characteristics of molar incisor hypomineralisation (MIH) in the child population residing in Gandhinagar, Gujarat, India. Eur Arch Paediatr Dent. 2012;13:21–6. doi: 10.1007/BF03262836. [DOI] [PubMed] [Google Scholar]
- 13.Lwanga SK, Lemeshow S. Geneva, Switzerland: World Health Organization; 1991. Sample Size Determination in Health Studies, A Practical Manual; pp. 1–3. [Google Scholar]
- 14.Mahoney EK. The treatment of localised hypoplastic and hypomineralised defects in first permanent molars. N Z Dent J. 2001;97:101–5. [PubMed] [Google Scholar]
- 15.Jälevik B, Norén JG. Enamel hypomineralization of permanent first molars: A morphological study and survey of possible aetiological factors. Int J Paediatr Dent. 2000;10:278–89. doi: 10.1046/j.1365-263x.2000.00210.x. [DOI] [PubMed] [Google Scholar]
- 16.Ogden AR, Pinhasi R, White WJ. Nothing new under the heavens: MIH in the past? Eur Arch Paediatr Dent. 2008;9:166–71. doi: 10.1007/BF03262632. [DOI] [PubMed] [Google Scholar]
- 17.Ahmadi R, Ramazani N, Nourinasab R. Molar incisor hypomineralization: A study of prevalence and etiology in a group of Iranian children. Iran J Pediatr. 2012;22:245–51. [PMC free article] [PubMed] [Google Scholar]
- 18.Census of India. 2011. [Last accessed on 2013 Sep 05]. Available from: http://www.censusindia.gov.in/PopulationFinder .
- 19.Zawaideh FI, Al-Jundi SH, Al-Jaljoli MH. Molar incisor hypomineralisation: Prevalence in Jordanian children and clinical characteristics. Eur Arch Paediatr Dent. 2011;12:31–6. doi: 10.1007/BF03262776. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Margarit M, Catalá-Pizarro M, Montiel-Company JM, Almerich-Silla JM. Epidemiologic study of molar-incisor hypomineralization in 8-year-old Spanish children. Int J Paediatr Dent. 2014;24:14–22. doi: 10.1111/ipd.12020. [DOI] [PubMed] [Google Scholar]
- 21.da Costa-Silva CM, Jeremias F, de Souza JF, Cordeiro Rde C, Santos-Pinto L, Zuanon AC. Molar incisor hypomineralization: Prevalence, severity and clinical consequences in Brazilian children. Int J Paediatr Dent. 2010;20:426–34. doi: 10.1111/j.1365-263X.2010.01097.x. [DOI] [PubMed] [Google Scholar]
- 22.Lygidakis NA, Dimou G, Briseniou E. Molar-incisor-hypomineralisation (MIH). Retrospective clinical study in Greek children. I. Prevalence and defect characteristics. Eur Arch Paediatr Dent. 2008;9:200–6. doi: 10.1007/BF03262636. [DOI] [PubMed] [Google Scholar]
- 23.Tapias-Ledesma MA, Jiménez R, Lamas F, González A, Carrasco P, Gíl de Miguel A. Factors associated with first molar dental enamel defects: A multivariate epidemiological approach. J Dent Child (Chic) 2003;70:215–20. [PubMed] [Google Scholar]
- 24.Jasulaityte L, Veerkamp JS, Weerheijm KL. Molar incisor hypomineralization: Review and prevalence data from the study of primary school children in Kaunas/Lithuania. Eur Arch Paediatr Dent. 2007;8:87–94. doi: 10.1007/BF03262575. [DOI] [PubMed] [Google Scholar]
- 25.Nanda RS. Eruption of human teeth. Am J Orthod. 1960;46:363–78. [Google Scholar]
- 26.Whatling R, Fearne JM. Molar incisor hypomineralization: A study of aetiological factors in a group of UK children. Int J Paediatr Dent. 2008;18:155–62. doi: 10.1111/j.1365-263X.2007.00901.x. [DOI] [PubMed] [Google Scholar]
- 27.Kuscu OO, Caglar E, Aslan S, Durmusoglu E, Karademir A, Sandalli N. The prevalence of molar incisor hypomineralization (MIH) in a group of children in a highly polluted urban region and a windfarm-green energy Island. Int J Paediatr Dent. 2009;19:176–85. doi: 10.1111/j.1365-263X.2008.00945.x. [DOI] [PubMed] [Google Scholar]
- 28.Beentjes VE, Weerheijm KL, Groen HJ. Factors involved in the aetiology of molar-incisor hypomineralisation (MIH) Eur J Paediatr Dent. 2002;3:9–13. [PubMed] [Google Scholar]
- 29.Laisi S, Ess A, Sahlberg C, Arvio P, Lukinmaa PL, Alaluusua S. Amoxicillin may cause molar incisor hypomineralization. J Dent Res. 2009;88:132–6. doi: 10.1177/0022034508328334. [DOI] [PubMed] [Google Scholar]
- 30.Kuscu OO, Sandalli N, Dikmen S, Ersoy O, Tatar I, Turkmen I, et al. Association of amoxicillin use and molar incisor hypomineralization in piglets: Visual and mineral density evaluation. Arch Oral Biol. 2013;58:1422–33. doi: 10.1016/j.archoralbio.2013.04.012. [DOI] [PubMed] [Google Scholar]


