Abstract
Rifampicin (RIF) is a benchmark drug for treatment of tuberculosis, but poor bioavailability, prolonged treatment, and pill burden have been linked to therapeutic failure and the development of multidrug resistant strains. To overcome these limitations, this study investigated a method of rifampicin nanoencapsulation and aerosol delivery using a commercial, hand-held nebulizer modified with a nitrogen stream.
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis (MB) and is considered one of the main challenges in modern public health.1 According to the World Health Organization, TB remains one of the world's deadliest communicable diseases and an estimated 9.0 million people developed TB and 1.5 million died from the disease in 2013.2, 3 One of the drugs used as a first-line treatment for TB is rifampicin (RIF), an antibiotic that inhibits the synthesis of bacterial RNA by binding to the beta-subunit of RNA polymerase.4, 5 RIF is considered a model antibiotic with well defined chemical properties (MW = 823 g/mol, pI = 4.8) and optical response (absorption maxima at 255 nm, 336 nm, and 475 nm). RIF is soluble in a number of organic solvents (dimethylsulfoxide: ∼100 mg/mL; methanol: 16 mg/ml; chloroform: 349 mg/ml; ethyl acetate: 108 mg/ml; and acetone: 14 mg/ml) and is slightly soluble in water (2.5 mg/ml). Although RIF is one of the most effective anti-tuberculosis agents available, increased drug resistance, low cell permeability, difficulty in maintaining higher drug concentrations at the infected site, and degradation of the drug before reaching the target site6 limit drug efficacy. In addition, several reports have described limited bioavailability of RIF (especially when used in combination with other antituberculosis agents such as isoniazid, pyrazinamide and/or ethambutol).1, 5 Moreover, when administrated orally RIF may also cause adverse effects, attributed to the systemic exposure to the drug.7, 8 Because the pulmonary form of TB prevails, growing attention has been given to respiratory routes to administer RIF. However, the poor retention of the drugs in the lungs and the invasive nature of some of these procedures (e.g. intra-tracheal instillation) have hindered its use in clinical settings. Clearly, developing a more efficient RIF delivery route could significantly improve TB treatment and outcomes.
The use of nanomaterials9 and colloidal systems10 are promising avenues for decreasing side effects, enhancing the therapeutic efficacy, and improving bioavailability.11, 12 Because they exhibit unique physicochemical properties such as ultra-small and controllable size, large surface-to-volume ratio, and well-known surface chemistry,13 nanoparticles have been proposed for formulations administered via diverse delivery modalities including parenteral, oral, intraocular, transdermal, or pulmonary inhalation. As the latter route is non-invasive and can be used for both systemic and local applications,7, 14 it has received great attention in last few years. Moreover, the large alveolar surface area, extensive vascularization, limited proteolytic activity and absence of first-pass metabolism7, 14 have recently enabled the development of inhalable insulin.15 In general, formulations based on nanoaerosols can provide better drug solubility, reduce clearance by macrophages, and decrease the displacement of the drug to the airways10, 16-18.
Among the different types of commercial systems that have been used to produce aerosols for respiratory drug delivery,19 mesh nebulizers (vibrating a plate with micro orifices) enable the on-demand aerosol production with minimal volume requirements, low heat production, and narrow dispersion of particles produced.18, 20 Because the droplet size is typically in the 3 μm to 9 μm range, one of the main drawbacks of this technology is that only a small fraction of the material can reach the site of the infection. This is principally because larger aerosolized molecules impact at bifurcations in the upper airways. Ventilation-perfusion inequalities further impair the effective delivery of micrometer-sized drugs to the lower lung and extrapulmonary spaces. Aiming to address these shortcomings, the present manuscript describes the encapsulation of RIF in self-assembled nanoparticles (NP) produced as aerosols using a low-cost, hand-held nebulizer. This communication builds on a previous report12 focused on the development of the nanoparticles and their potential to encapsulate model drugs.
Materials and Methods
A detailed description of the instruments and procedures used in this project is included as Supplementary Information. NPs containing RIF were prepared according to a procedure recently described.12 Briefly, the lipid nanoparticle formulation was prepared by a combination acid responsive asparagine-derived amphiphile (ALA-11) and cholesterol (20:80). The N,N-acetal group of ALA-11 disassembles under acidic conditions results in the release of a hydrophobic encapsulates. ALA-11 was synthetized by cyclocondensation of an equimolar ratio of L-asparagine and n-dodecanal in a methanolic NaOH solution followed by evaporation. Cholesterol was added to a freshly prepared ALA-11 formulation and the mixture was dissolved in 50:50 chloroform/methanol (v/v). As a reference, the structure of the selected amphiphile (ALA-11) is shown in Figure 1.
Figure 1.
Structure of the amphiphile ALA-11, used to develop the aerosolized NPs.
The solvent was evaporated from these preparations to produce thin films, which were dissolved in a phosphate buffered solution (PBS, pH 7.4, 4°C) until use. Stock solutions of RIF (1.0 mg/mL) were prepared by dissolving an appropriate amount of solid RIF in methanol.
For the encapsulation, 300 μL of the solution containing NP (in PBS pH 7.4) were dispensed in a round bottom flask and lyophilized (-50°C). Next, 1 mL of methanol (containing 1 mg of RIF) was added, and the slurry was vortexed for 15 s, and evaporated under a N2 stream. This process was repeated with 1 mL of chloroform to prepare a homogeneous phase containing both lipid and RIF (other solvents should be considered if the protocol is to be adapted for animal studies). Finally, 3 mL of water were added and the contents were vortexed until complete homogenization (typically less than 5 min) and placed in the nebulizer's medicine chamber. For the characterization, the produced aerosol was first collected on grids (300 mesh carbon film) and analyzed using a transmission electron microscope (TEM). Preliminary experiments demonstrated that in addition to NPs, large amounts of water were nebulized and collected in the grid, impairing the analysis by microscopy. To remove the water droplets, a drying chamber composed of a glass tube (60 cm length, 2.5 cm ID) equipped with a nitrogen inlet was coupled to the outlet of the nebulizer. TEM samples were collected at four N2 flow rates (2, 3, 4 and 5 L/min) by exposing the microscopy grid to the outlet of the glass tube. To estimate the nebulization rate, the change in weight of the TEM grids was determined.
To measure the amount of RIF encapsulated in the NPs, 3 mL of an aqueous suspension of RIF/NP, were centrifuged (13400 rpm for 5 minutes) to produce a pellet (containing the RIF/NP) and a supernatant containing free RIF. After removing the supernatant, the precipitate was dissolved in 1.5 mL of isopropanol, sonicated (5 min), and centrifuged (13400 rpm for 15 min) to release RIF from the NPs. The RIF was quantified by spectrophotometry (absorbance at 336 nm) using a calibration curve performed under equivalent conditions.
One of the main advantages of using NPs for drug delivery is the possibility to sustain the delivery of the drug over a period of time. In order to stablish the half-life and determine the stability of the putative NPs, 7.5 mg of RIF/NP lyophilized were resuspended in 5 mL of PBS (8 g/L NaCl, 0.2 g/L KCl, 1.44 g/L Na2HPO4 and 0.24 g/L KH2PO4) and maintained in an orbital shaker (100 rpm) at room temperature (72 ± 2 F). An aliquot of the sample (500 μl) was obtained at different times (during 9 days), centrifuged (13.4 rpm for 5 min) and analyzed spectrophotometrically to determine the remaining amount of encapsulated RIF using the procedure above described.
Results
Aerosolization Process
Hand-held nebulizers are inexpensive, compatible with the delivery of a number of therapeutic agents, and afford dose control by temporal exposure. Because it has been reported that the nebulization rate can be influenced by a number of parameters (including the viscosity of the solution), the nebulization rate of a solution containing encapsulated RIF was measured. According to our experiments (data not shown), a constant rate of 0.088 ± 0.005 mL/min was maintained over 20 min. These results indicate that although the addition of the NP/RIF significantly decreased the nebulization rate with respect to the maximum specified value from the manufacturer (up to 0.25 mL/min), the selected device enable reasonable control of the dosage of the proposed formulation. The difference observed, with respect to the nominal value reported by the manufacturer, could be attributed to differences in the viscosity of the nebulized solution.
In order to analyze the number the NP released during the nebulization, 3 mL aliquots of a solution containing NP/RIF were dispensed in the “medication cup” of the nebulizer. Samples of nebulized NP were collected on carbon grids and analyzed by scanning TEM for each of the four previously examined N2 flow rates (2, 3, 4 and 5 L/min). Each grid was positioned at the outlet of the glass chamber and the NPs were collected during 15 seconds. At least five, separate, randomly-chosen fields per substrate and condition were processed in the TEM, manually counted and used to construct the histogram. According to our results (Figure 1), an increased N2 flow rate resulted in a substantial increase in the number of particles collected (200 NP/min at 2 mL/min vs 3200 NP/min at 5 mL/min) and decrease in the average size of such particles (780 nm at 2 mL/min vs 380 nm at 5 mL/min). Data in Figure 2 provide strong evidence that the majority of the aerosolized sample exists in the sub-800 nm range. While the numerical difference in the average can be attributed to the presence of larger particles in the sample collected using 2 mL/min N2, the mode (most frequently occurring value) of both populations was very similar (292 nm at 2 mL/min vs 278 nm at 5 mL/min). These results indicate that adding a stream of N2 to the outlet of the nebulizer can provide significant advantages in the delivery and control of the particle dimensions. It is important to note that if required, the carrier gas could be potentially replaced by compressed air (containing oxygen).
Figure 2.
Relative abundance as a function of the RIF/NP diameter (in log scale) collected using a flow of N2 of 2 L/min (
 ) or 5 L/min (
) or 5 L/min (
 ). Inserts: Micrograph of NP analyzed by high resolution scanning electron microscope (STEM) FE Hitachi S-5500 (0.4 nm at 5kV) with a BF/DF Duo-STEM detector.
). Inserts: Micrograph of NP analyzed by high resolution scanning electron microscope (STEM) FE Hitachi S-5500 (0.4 nm at 5kV) with a BF/DF Duo-STEM detector.
Electron microscopy images were used to provide evidence that RIF was contained within the structure of the aerosolized particles. As it can be observed in Figure 3A, and in agreement with previous results,12 spherical particles with rather uniform optical density were observed when only the NP was placed in the nebulizer. On the other hand, much smaller particles (solids) were obtained when a solution of RIF (no NP) was nebulized (Figure 3B). On the contrary, when the composite of NP/RIF was aerosolized, the expected core/shell arrangement was obtained (Figure 3C). In this case, the dimensions of neither the RIF core nor the lipidic shell were significantly affected (when compared to the originally described NP12). It was observed however, that the RIF core visualized inside the NP were morphologically cubic. These polymorphic forms of RIF (form I and form II), have been previously reported and could impact the pharmacokinetics of RIF.21, 22 Further experiments are required to identify the structure of RIF in the core of the NP.
Figure 3.

Images isolated of an empty nanoparticle (A), pure rifampicin (B) and rifampicin/nanoparticle (C)
To evaluate the encapsulation efficiency into the NPs, mixtures of the lipid NP (2.5 mg) were mixed with increasing amounts of RIF (in the 0.75 – 2.0 mg range). The RIF-encapsulated NPs were prepared following the previously described procedure, free RIF was removed from the bulk solution by centrifugation/washing cycles, and the encapsulation was measured by spectrophotometry at 336 nm after releasing the RIF from the NPs using isopropanol. As it can be observed in Figure 4, the higher the concentration of RIF added to the mixture, the higher the amount of RIF encapsulated. As the size and area of the NP is relatively constant, these results are compatible with the inclusion of the antibiotic inside the NP.
Figure 4.
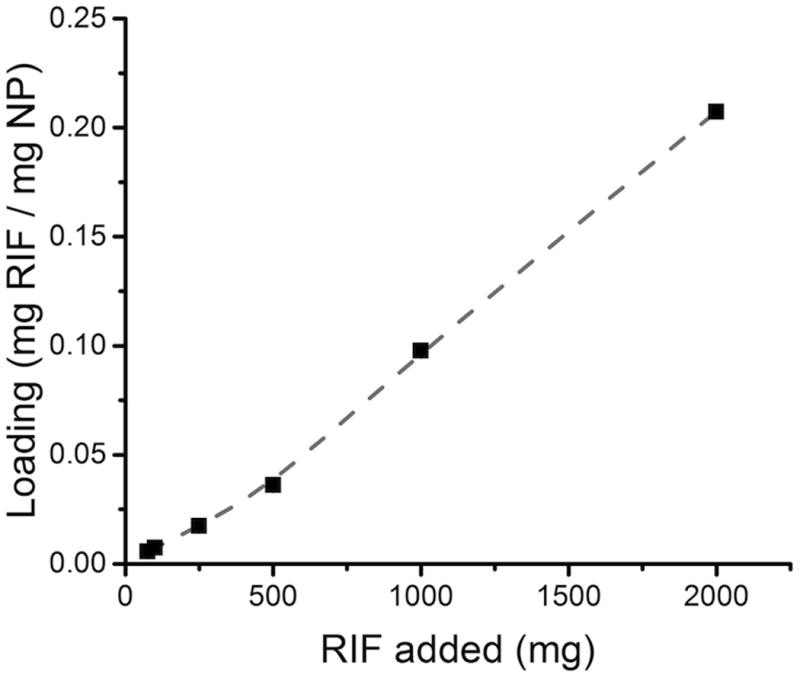
Dependence of the amount of RIF encapsulated in the NP as a function of the amount of RIF used to prepare the NP/RIF composite. Line included to guide the eye.
It's important to point that although the loading obtained with 2 mg of RIF is relatively low (20%), these composites can participate in the aerosolization and efficiently encapsulate significant amounts of RIF. Additional studies are currently underway (and will be reported separately) to evaluate the efficiency of sonication in the encapsulation process. The results obtained with RIF (modestly soluble in water) are in agreement with our previous studies, where we showed that ALA-11/cholesterol NPs encapsulated two highly hydrophobic molecules (but not hydrophilic molecules) and suggest that the interior of the produced NPs does not contain solvent.
One of the most important aspects of the use of NPs for drug delivery is the ability to release the drug in a timespam that is clinically relevant. In this regard, Aboutaleb et al23 showed a release of 75% of encapsulated RIF during 3 days. Singh, et al 24 showed 70% RIF release RIF from NP after 9 days. To evaluate the stability of NP/RIF under near physiological conditions, NP/RIF were placed in an isotonic solution (pH 7.4) and kept under constant agitation (orbital shaker, 100 rpm) for 8 days. Aliquots were collected daily to measure the amount of remaining NP/RIF. As it can be observed in Figure 5, samples collected during the 8 days showed an exponential decrease in the amount of RIF released (as NP/RIF loose integrity), reaching a release of RIF of 65% of RIF within 8 days. While additional studies are required to investigate the stability of the NP/RIF in the long-term, these results demostrate that the proposed NP can significantly delay the delivery of the RIF and could provide a sustained delivery mechanism for the antibiotic.
Figure 5.
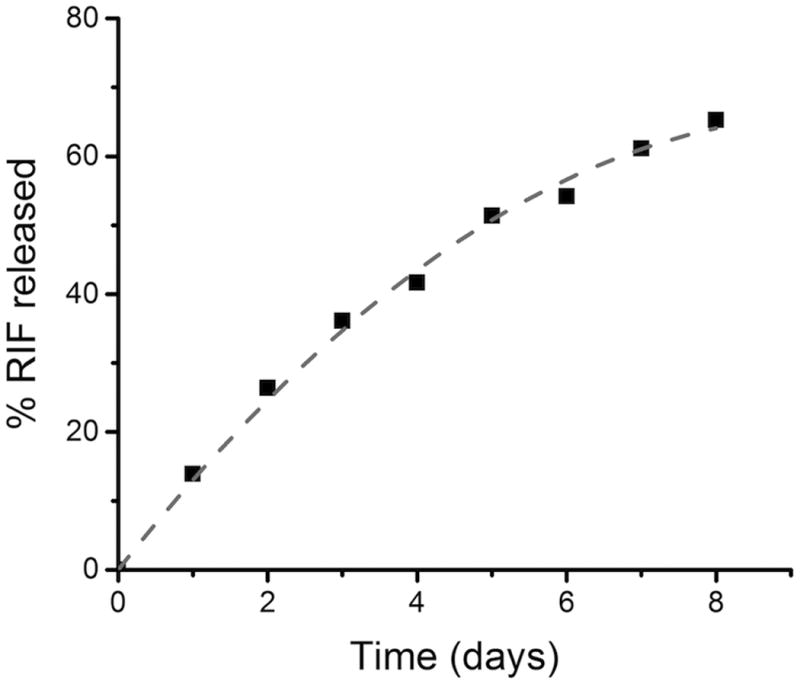
Stability of NP evaluated thought absorbance of RIF measured day by day. Line included to guide the eye.
Conclusions
Low-cost nebulizers can be used to produce aerosols containing 400 nm NP loaded with RIF. The NPs are approximately 20% w/w of RIF, a core/shell configuration was obtained, where the RIF crystal was encapsulated by the lipidic NPs. Although the kinetics of RIF encapsulation and release may be affected by the specific dimensions of the particle, the presented NP/RIF showed a rather slow release of the RIF. In addition, previous results from our group have demonstrated that slight increases in the acidity of the environment can aid in the disaggregation of the NP and deliver their contents. Overall, we believe this low-cost methodology could provide alternative ways to administer RIF, reduce of overall therapeutic dose, prevent unwanted side effects, and improve adherence of patients to the therapy.
Supplementary Material
Acknowledgments
This work was supported in part by the National Institute of Health through grant numbers G12MD007591 and ES015022. AAI also thanks the scholarship provided by CAPES (BEX 7469/14-4).
Contributor Information
George R. Negrete, Email: george.negrete@utsa.edu.
Carlos D. Garcia, Email: cdgarci@clemson.edu.
References
- 1.Moretton MA, Glisoni RJ, Chiappetta DA, Sosnik A. Colloids Surf B. 2010;79:467–479. doi: 10.1016/j.colsurfb.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 2.WHO. Global Tuberculosis report 2014. 2015 Agust; http://apps.who.int/iris/bitstream/10665/137094/1/9789241564809_eng.pdf?ua=1.
- 3.Burman WJ, Gallicano K, Peloquin C. Clin Pharmacokinet. 2001;40:327–341. doi: 10.2165/00003088-200140050-00002. [DOI] [PubMed] [Google Scholar]
- 4.Gürsoy A, Kut E, Özkırımlı S. Int J Pharm. 2004;271:115–123. doi: 10.1016/j.ijpharm.2003.10.033. [DOI] [PubMed] [Google Scholar]
- 5.Parmar R, Misra R, Mohanty S. Colloids Surf B Biointerfaces. 2015;129:198–205. doi: 10.1016/j.colsurfb.2015.03.051. [DOI] [PubMed] [Google Scholar]
- 6.Coban AY, Deveci A, Sunter AT, Palomino JC, Martin A. Int J Mycobacteriol. 2014;3:230–241. doi: 10.1016/j.ijmyco.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 7.Sung JC, Pulliam BL, Edwards DA. Trends Biotechnol. 2007;25:563–570. doi: 10.1016/j.tibtech.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Singh C, Koduri LVSK, Singh A, Suresh S. Asian J Pharm Sci. 2015;10:549–562. [Google Scholar]
- 9.Kaur M, Garg T, Rath G, Goyal AK. Critical Reviews™ in Therapeutic Drug Carrier Systems. 2014;31:49–88. doi: 10.1615/critrevtherdrugcarriersyst.2014008285. [DOI] [PubMed] [Google Scholar]
- 10.Sham JOH, Zhang Y, Finlay WH, Roa WH, Löbenberg R. Int J Pharm. 2004;269:457–467. doi: 10.1016/j.ijpharm.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 11.Drulis-Kawa Z, Dorotkiewicz-Jach A. Int J Pharm. 2010;387:187–198. doi: 10.1016/j.ijpharm.2009.11.033. [DOI] [PubMed] [Google Scholar]
- 12.Mfuh AM, Mahindaratne MPD, Ynigez-Gutierrez AE, Ramos Dominguez JR, Bedell Ii JT, Garcia CD, Negrete GR. RSC Adv. 2015;5:8585–8590. doi: 10.1039/C4RA11884G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L, Pornpattananangkul D, Hu CMJ, Huang CM. Curr Med Chem. 2010;17:585–594. doi: 10.2174/092986710790416290. [DOI] [PubMed] [Google Scholar]
- 14.Azarmi S, Roa WH, Löbenberg R. Adv Drug Deliv Rev. 2008;60:863–875. doi: 10.1016/j.addr.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 15.JAMA. 2015;313:2176–2177. doi: 10.1001/jama.2015.5634. [DOI] [PubMed] [Google Scholar]
- 16.Ely L, Roa W, Finlay WH, Lobenberg R. Eur J Pharm Biopharm. 2007;65:346–353. doi: 10.1016/j.ejpb.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 17.Smitha KT, Nisha N, Maya S, Biswas R, Jayakumar R. Int J Biol Macromol. 2015;74:36–43. doi: 10.1016/j.ijbiomac.2014.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Worth Longest P, Spence BM, Holbrook LT, Mossi KM, Son YJ, Hindle M. J Aerosol Sci. 2012;51:66–80. doi: 10.1016/j.jaerosci.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Callaghan C, Barry PW. Thorax. 1997;52:31–44. [Google Scholar]
- 20.Vecellio L. Breathe. 2006;2:253–260. [Google Scholar]
- 21.Agrawal S, Ashokraj Y, Bharatam PV, Pillai O, Panchagnula R. Eur J Pharm Sci. 2004;22:127–144. doi: 10.1016/j.ejps.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Freire FD, Aragão CFS, Moura TFAdL, Raffin FN. J Therm Anal Calorim. 2009;97:333–336. [Google Scholar]
- 23.Aboutaleb E, Noori M, Gandomi N, Atyabi F, Fazeli MR, Jamalifar H, Dinarvand R. Int Nano Lett. 2012;2:33. [Google Scholar]
- 24.Singh H, Bhandari R, Kaur IP. Int J Pharm. 2013;446:106–111. doi: 10.1016/j.ijpharm.2013.02.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.




