Abstract
The lifetime prevalence of allergic diseases in adults in Germany [self-reported doctor diagnosed allergic diseases, Study on Adult Health in Germany (Studie zur Gesundheit Erwachsener in Deutschland, DEGS1, 2008–2011) of the Robert Koch Institute] is 8.6 % for asthma, 14.8 % for hay fever, 3.5 % for atopic dermatitis, 8.1 % for contact dermatitis, 4.7 % for food allergies, and 2.8 % for insect venom allergies. Almost 20 % of German adults are currently affected by at least one allergy.
In tests on 50 common single allergens and two mixtures comprising either inhalant allergens or grass pollen allergens, 48.6 % of participants exhibited at least one allergic sensitization (specific IgE antibody detection). Overall, 33.6 % of participants were sensitized to inhalant allergens, 25.5 % to at least one food allergens, and 22.6 % to at least one insect venom allergens. A comparison of data on adults from 1998 [Federal Health Survey 1998 (Bundes-Gesundheitssurvey 1998, BGS98) of the Robert Koch Institute] and 2008–2011 (DEGS1) shows an increase in prevalence over time of almost three percentage points, while the rate of sensitization to inhalant allergens has increased from 29.8 % to 33.6 %. The prevalence of doctor diagnosed hay fever, atopic dermatitis, and food allergies, on the other hand, has remained virtually unchanged over the last 15 years.
The Germany-wide lifetime prevalence of allergic diseases in children and adolescents [Study on the Health of Children and Adolescents in Germany (Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland, KiGGS initial survey, 2003–2006) of the Robert Koch Institute] was 4.7 % for asthma, 10.7 % for hay fever, and 13.2 % for atopic dermatitis. Altogether, 40.8 % of German children and adolescents were sensitized to at least one of the inhalant or food allergens measured, while 20.0 % were sensitized to at least one food allergen. A marked increase in hay fever prevalence among East German children in the 1990s has resulted in an alignment of prevalence rates in East and West Germany. In contrast to adults, there was no longer a discernible difference in the prevalence of asthma, hay fever, and allergic sensitization in children between the western and eastern German federal states.
In international comparisons with prevalence data from other studies, the participating German centers are in the lower third of the distribution of frequency for both children and adults.
Key words: inhalant allergies, prevalence, sensitization, type-I allergy, adults, children
Introduction
Allergic reactions are aberrant immune responses to exogenous, normally harmless substances (allergens from, e.g., pollen, house dust mites, animal dander, insect venom, food components). In type-I (immediate-type) allergies, specific immunoglobulin E (IgE) antibodies react with allergens and trigger allergic reactions. The presence of IgE antibodies (in blood and on some skin and mucosa cells, e.g., mast cells) is an absolute precondition for the clinical manifestation of allergy in this allergy type. The presence of specific IgE antibodies is referred to as allergic sensitization. Sensitization is the precondition for an allergy, i.e., the onset of allergic symptoms; however, it may also be present without leading to symptom onset upon contact with the allergen. The prevalence of sensitizations to certain allergens has increased in recent years.
Unfortunately, a straightforward answer to the question of the prevalence of allergic diseases in Germany is not possible, since:
There is, to an extent, no generally accepted definition of the various forms of allergic diseases (e.g., asthma is often classified as an allergy, although many cases involve non-allergic rather than allergic asthma).
It is virtually impossible to collect epidemiological data on these specific disease entities in large population-based studies.
Routine data are unavailable or insufficiently valid.
The availability of data deemed representative of the German population is poor.
Thus, most large epidemiological surveys are restricted to answering simple questions such as those relating to the doctor diagnosis of asthma, hay fever, and atopic dermatitis, or gathering data on key symptoms, such as wheezing respiratory sounds, eye redness and irritation in the absence of cold symptoms, pruritic skin rash, which appears for some weeks and then disappears for a certain period. An assessment of bronchial hyperreactivity of the airways to a nonspecific irritant with repeat pulmonary function tests and the determination of allergic sensitization by skin prick testing or specific serum IgE detection, as well as standardized skin examination according to SCORAD (scoring atopic dermatitis) to assess the severity of eczema, yield more objective data. An immune dysfunction is always present in the case of allergy; this can be determined with skin or blood tests. In contrast, food allergies or intolerances can only be detected by means of specific food challenge testing. Tests of this kind are complex and are rarely performed in the general population. Therefore, reliable data on the prevalence of these diseases are largely lacking. However, the risk (not the disease itself!) of food allergies can be determined in blood by detecting specific immunoglobulins (IgE) to food allergens.
The prevalence of allergic disease in Germany
The prevalence data presented in this position paper pertain to the general German population. The literature search was restricted to only those national surveys that included the entire population of the Federal Republic of Germany, in order to exclude the possibility of specific regional data not related to the entire German population. The surveys included were those conducted in children and adults under the direction of the Robert Koch Institute in recent years.
Adults
Prevalence estimates representative for Germany were obtained from the Study on Adult Health in Germany (Studie zur Gesundheit Erwachsener in Deutschland, DEGS1) last conducted between 2008 to 2011 (Fig. 1). Data was collected from 7988 18- to 79-year-olds using computer-aided medical interviews at participation rates of 42 % and 62 % in the population initially invited and the follow-up population of the BGS98, respectively. According to these data, the lifetime prevalence of doctor diagnosed allergic disease is 8.6 % for asthma, 14.8 % for hay fever, 3.5 % for atopic dermatitis and for urticaria, 8.1 % for contact dermatitis, 4.7 % for food allergies, and 2.8 % for insect venom allergies [1].
Fig. 1.
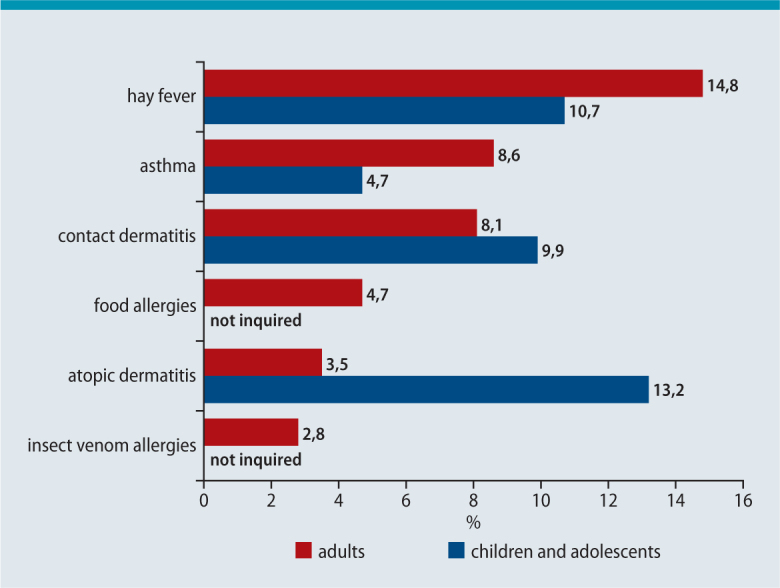
Lifetime prevalence of medically diagnosed allergic diseases (self-reported) in adults (18–79 years, RKI survey DEGS1, survey period 11/2008–11/2011, n=7988 [1]) and children/adolescents (0–17 years, RKI survey KiGGS, survey period 05/2003–05/2006, n=17,641 [5])
Altogether, at least one of the above-mentioned allergies has been diagnosed in almost a third of German adults at some point. Almost 20 % of German adults are currently affected by at least one allergy. In general, women are more frequently affected than men and younger women more frequently than older. In addition, allergies are more prevalent in the western federal states compared to the eastern. Higher socioeconomic status and living in large urban areas likewise increase disease prevalence.
Also as part of this study, specific IgE antibodies to 50 widespread single allergens were measured and two tests performed, each using a mixture of inhalant allergens (composition: timothy, rye, birch, mugwort, house dust mite, cat dander, dog dander, Cladosporium herbarum) and grass pollen allergens (composition: cocksfoot, meadow fescue, darnel, timothy, bluegrass) (Fig. 2, Fig. 3). Sensitization was detected in 48.6 % of participants. More men compared to women were sensitized to at least one allergen. In addition, more of the younger participants compared with the older, as well as more subjects with a higher social status, were affected by at least one sensitization. Altogether, 33.6 % of participants were sensitized to inhalant allergens, 25.5 % to at least one food allergen, and 22.6 % to at least one insect venom [2].
Fig. 2.

Prevalence of sensitization to specific allergens in adults (18–79 years, RKI survey DEGS1, survey period 11/2008–11/2011, n=7025 [2]) and children/adolescents (3–17 years, RKI survey KiGGS, survey period 05/2003–05/2006, n=12,988 [4, 12]). The panels tested are not identical: In the adult group, blood samples were analyzed for specific IgE antibodies to 50 widespread single allergens, and two tests performed, each using a mixture of inhalant allergens (SX1) and grass pollen (GX1). In the child/adolescent group, blood samples were analyzed for specific IgE antibodies to 20 single allergens and tests performed with a mixture of inhalant allergens (SX1).
Fig. 3.

Prevalence of sensitization to selected food allergens in adults (18–79 years, RKI survey DEGS1, survey period 11/2008–11/2011, n=7025 [2]) and children/adolescents (3–17 years, RKI survey KiGGS, survey period 05/2003–05/2006, n=12988 [12])
Children
Allergy prevalence data representative for the whole of Germany were collected between 2003 and 2006 in the German „Children and Adolescent Health Survey“ (Kinder- und Jugend-Gesundheitssurvey, KiGGS) (Fig. 1). At a participation rate of 66.6 %, 17,641 children and adolescents aged between 0 and 17 years were investigated. Interviews and questionnaires relating to doctor diagnosed diseases yielded a lifetime prevalence of 4.7 % for asthma, 10.7 % for hay fever, and 13.2 % for atopic dermatitis [3, 4]. Of the study participants, 40.8 % were sensitized to at least one of the 20 inhalant or food allergens measured (Fig. 2). With the exception of eczema, a marked increase in atopic disease was seen with age, indicating that age-specific prevalence data are more meaningful. Boys were more frequently affected by asthma, hay fever, and specific sensitizations compared to girls. There is no longer a discernible difference between western and eastern German federal states. Children from families of lower socioeconomic status or with a background of migration are significantly less frequently affected by allergic disease [4]. The follow-up study of 12,368 children and adolescents in the KiGGS Wave-1 survey conducted between 2009 and 2012 as a combined cross-sectional and longitudinal survey largely confirmed these figures (the lifetime prevalence of doctor diagnosed diseases was 6.3 % for asthma, 12.6 % for hay fever, and 14.3 % for atopic dermatitis) [5].
As in other large epidemiological studies, the estimates on the prevalence of allergic disease in both the KiGGS and DEGS are essentially based on surveying doctor diagnoses and not on the standardized collection of data on key symptoms or even objective clinical tests; the real burden of disease, therefore, may be underestimated.
In international comparison with prevalence data from the ISAAC study (The International Study of Asthma and Allergies in Childhood) in children and the ECRHS (European Community Respiratory Health Survey) in adults in numerous other countries, prevalence estimates for asthma, hay fever, and eczema at the participating German centers are in the lower third of the distribution of prevalence for both children and adults [6, 7].
A marked increase in the prevalence of hay fever and allergic sensitization was seen in adults (particularly young adults) during the 1990s. The increase in asthma was less pronounced [8, 9]. In a comparison between the German Federal Health Survey of 1998 (BGS98) and the first wave of the DEGS survey (2008–2011), the prevalence of asthma has risen by just under a further three percentage points, while allergic sensitization to inhalant allergens has risen from 29.8 % to 33.6 % [2]. In contrast, the frequency of medically diagnosed hay fever, atopic dermatitis, and food allergies has remained virtually unaltered over the last 15 years.
A marked rise in the prevalence of hay fever, allergic sensitization, and asthma was seen in particular in East German children in the 1990s. This marked rise resulted in an alignment of prevalence rates in children in East and West Germany. In contrast to adults, there is no longer a discernible difference in the prevalence rates of asthma, hay fever, and allergic sensitization in children between the old and new German federal states.
The comparison of 12-month prevalence rates of atopic diseases between KiGGS survey period 1 and KiGGS baseline survey 6 years earlier (cross-sectional comparison) indicates that the frequency of asthma is increased in children and adolescents with no significant increase of hay fever either; the 12-month prevalence rates of atopic dermatitis show a statistically significant reduction [5].
The sensitizing potential of mold is estimated as far lower compared with other environmental allergens, such as grass or tree pollen and mites [10]. Current — population- as well as patient-based [11] — studies show comparatively low sensitization rates of 3 %–10 % throughout Europe [2].
Conclusion
Given that almost every third person in Germany is affected by allergic disease in the course of their life and that allergic sensitization was detected in 50 % of the German population, one is compelled to classify this phenomenon as an important, frequent, and widespread disease that impairs the quality of life of many. Any trivialization of the problem is wholly misplaced in view of the well-documented situation. No primary allergy prevention is in sight. Therefore, particularly in terms of our responsibility to the young generation, it is essential to increase efforts on all levels (research, treatment, and administration) to ensure that the „allergy problem in Germany“ is recognized and addressed as a genuine problem in the health sector.
Footnotes
Conflict of interest
The authors declare that there are no conflicts of interest.
Cite this as
Bergmann KC, Heinrich J, Niemann H. Current status of allergy prevalence in Germany. Position paper of the Environmental Mediine Commission of the Robert Koch Institute. Allergo J Int 2016;25:6–10 DOI: 10.1007/s40629-016-0089-1
Comment
Adopted by the Environmental Medicine Commission of the Robert Koch Institute at their meeting of 17th June 2015
Commission members
Prof. Dr. K.-C. Bergmann (Allergy-Center Charité, Charité University Hospital, Berlin, Germany), Prof. Dr. W. Dott (Aachen University Hospital, Institute for Hygiene and Environmental Medicine, Aachen, Germany), Prof. Dr. T. Eikmann (Gießen University, Institute for Hygiene and Environmental Medicine, Gießen, Germany), Dr. J. H. (Helmholtz Center Munich, Epidemiology I, Munich, Germany), Prof. Dr. C. Herr (Bavarian Health and Food Safety Authority, Germany), PD Dr. A. Heutelbeck (Göttingen University Hospital, Institute for Occupational, Social, and Environmental Medicine, Göttingen, Germany), Prof. Dr. B. Hoffmann (Heinrich-Heine University Düsseldorf, Institute for Environmental Medical Research, Düsseldorf, Germany), Prof. Dr. C. Hornberg (Bielefeld University, Faculty of Health Sciences, Bielefeld, Germany), Dr. K. Leitner (former WHO Deputy Director General, Geneva, Switzerland), Prof. Dr. V. Mersch-Sundermann (Freiburg University, Institute of Hospital Hygiene and Environmental Medicine), Prof. Dr. D. Nowak (Ludwig-Maximilian University, City Center Clinic, Institute and Polyclinic for Occupational and Environmental Medicine, Munich, Germany), Dr. M. Otto (non-profit Kinderumwelt GmbH), Prof. Dr. A. Peters (Helmholtz Center, Epidemiology II, Munich, Germany), Dr. M. Schümann (formerly of the Authorities for Health and Consumer Protection of the Free and Hanseatic City of Hamburg, Germany), Prof. Dr. G. A. Wiesmüller (Cologne Health Authority, Germany)
Permanent guests of the commission
Dr. U. Winkler, K. Höppner M. Sc. (German Federal Ministry of Health), J. Küllmer (German Federal Ministry for the Environment, Nature Conservation, Building and Nuclear Safety), Dr. A. Gies, Dr. W. Straff, Dr. A. Neumann, Dr. D. Plaß (German Federal Environment Agency), Dr. H. Desel (German Federal Institute for Risk Assessment, Berlin), Dr. Th. Jung (German Federal Office for Radiation Protection), Dr. H. Niemann (Head Office of the Environmental Medicine Commission of the Robert Koch Institute, Berlin, Germany), Dr. Th. Ziese, Dr. M. Faber, Prof. Dr. K. Stark (Robert Koch Institute, Berlin, Germany), Dr. F. Benkwitz (Chairman of the Federal States’ Working Group on Environment-Related Health Protection, LAUG)
References
- 1.Langen U, Schmitz R, Steppuhn H. Prevalence of allergic diseases in Germany. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2013;56:698–706. doi: 10.1007/s00103-012-1652-7. [DOI] [PubMed] [Google Scholar]
- 2.Haftenberger M, Lausmann D, Ellert U, Kalklosch M, Langen U, Schlaud M, et al. Prevalence of sensitisation to aeraoallergens and food allergens: results of the German Health Interview and Examination Survey for Adults (DEGS1) Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2013;56:687–97. doi: 10.1007/s00103-012-1658-1. [DOI] [PubMed] [Google Scholar]
- 3.Schmitz R, Atzpodien K, Schlaud M. Prevalence and risk factors of atopic diseases in German children and adolescents. Pediatr Allergy Immunol. 2012;23:716–23. doi: 10.1111/j.1399-3038.2012.01342.x. [DOI] [PubMed] [Google Scholar]
- 4.Schlaud M, Atzpodien K, Thierfelder W. Allergic diseases. Results from the German Health Interview and Examination Survey for Children and Adolescents (KiGGS) Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2007;50:701–10. doi: 10.1007/s00103-007-0231-9. [DOI] [PubMed] [Google Scholar]
- 5.Schmitz R, Thamm M, Ellert U, Kalcklosch M, Schlaud M; KiGGS Study Group. Verbreitung haufiger Allergien bei Kindern und Jugendlichen in Deutschland. Ergebnisse der KiGGS-Studie Erste Folgebefragung (KiGGS Welle 1). Bundesgesundheitsbl 2014;57:771–8 [DOI] [PubMed]
- 6.Asher MI, Montefort S, Bjorksten B, Lai CK, Strachan DP, Weiland SK, Williams H. ISAAC Phase Three Study Group. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006;3689537:733–43. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 7.Heinrich J, Richter K, Frye C, Meyer I, Wolke G, Wjst M, et al. European Community Respiratory Health Survey in Adults (ECRHS) Pneumologie. 2002;56:297–303. doi: 10.1055/s-2002-30699. [DOI] [PubMed] [Google Scholar]
- 8.Hermann-Kunz E, Thierfelder W. Allergische Rhinitis und Sensibilisierungsraten. Nimmt die Pravalenz wirklich zu? Wie sicher sind unsere Informationen? Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2001;44:643–53. doi: 10.1007/s001030100212. [DOI] [Google Scholar]
- 9.Hermann-Kunz E. Haufigkeit allergischer Krankheiten in Ost- und Westdeutschland. Gesundheitswesen. 1999;61(S2):100–5. [PubMed] [Google Scholar]
- 10.Taskinen T, Meklin T, Nousiainen M, Husman T, Nevalainen A, Korppi M. Moisture and mould problems in schools and respiratory manifestations in schoolchildren: clinical and skin test findings. Acta Paediatr. 1997;86:1181–7. doi: 10.1111/j.1651-2227.1997.tb14841.x. [DOI] [PubMed] [Google Scholar]
- 11.Heinzerling LM, Burbach GJ, Edenharter G, Bachert C, Bindslev-Jensen C, Bonini S, et al. GA(2)LEN skin test study I: GA(2)LEN harmonization of skin prick testing: novel sensitization patterns for inhalant allergens in Europe. Allergy. 2009;64:1498–506. doi: 10.1111/j.1398-9995.2009.02093.x. [DOI] [PubMed] [Google Scholar]
- 12.Haftenberger M, Lausmann D, Scheidt-Nave C, Thamm M. Abschlussbericht. Allergie- und Sensibilisierungsmonitoring im Rahmen der nationalen Gesundheitssurveys des Robert Koch-Instituts (RKI) zur Einschatzung der Allergiegefahrdung der erwachsenen Bevolkerung. Forderkennzeichen: 2808HS015 BLE. http://download.ble.de/08HS015/08HS015.pdf. Zugegriffen 07.09.2015


