Abstract
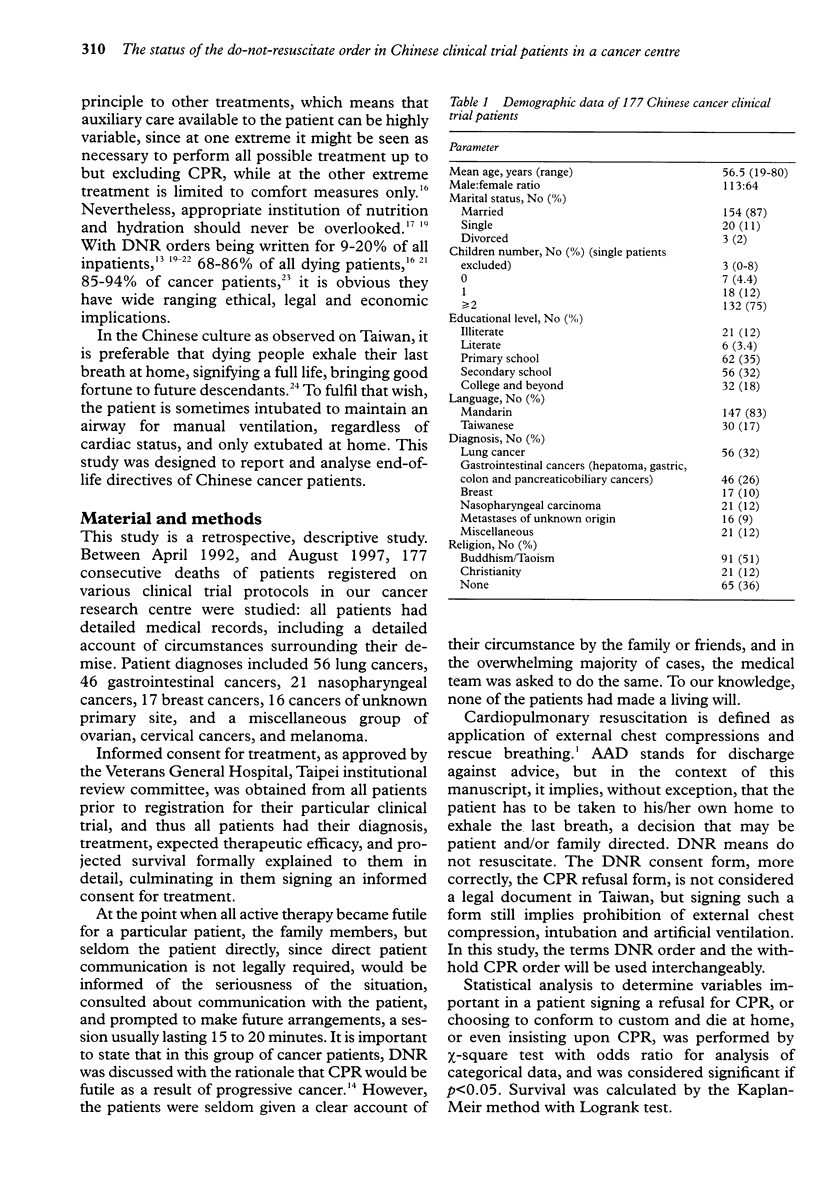
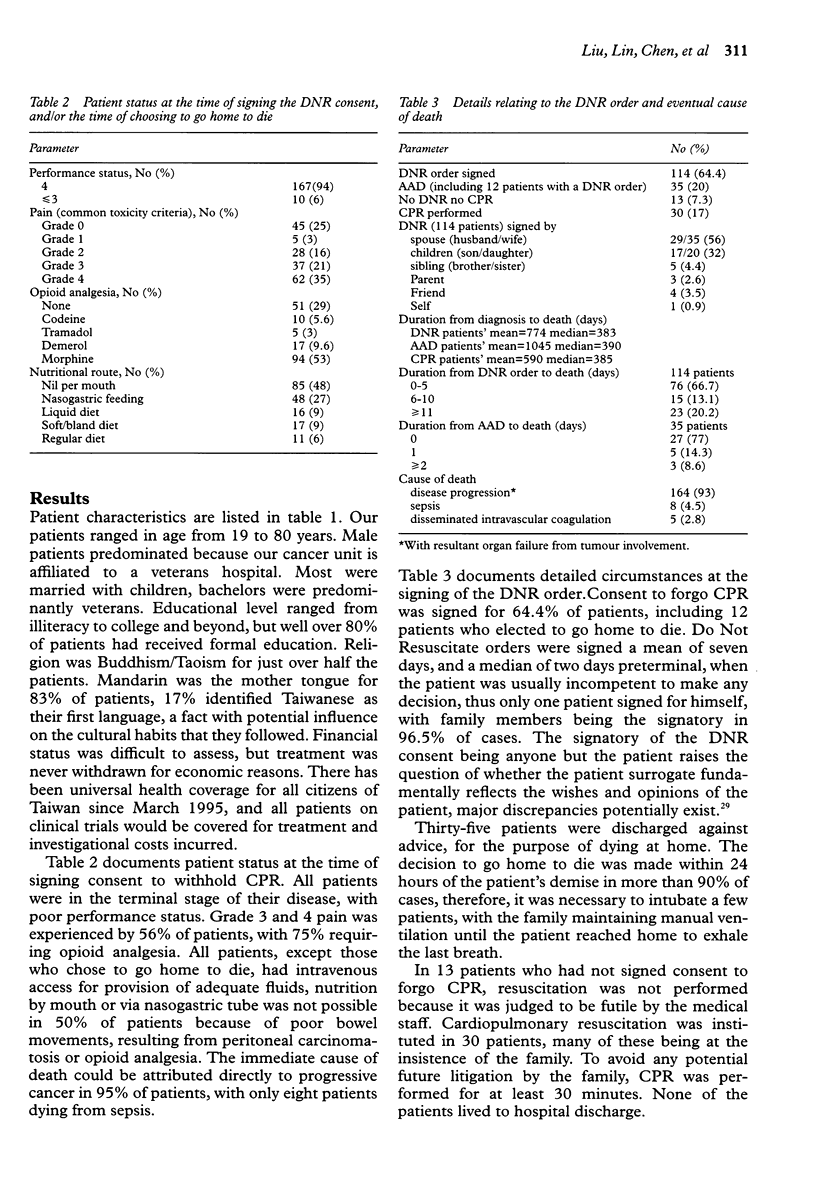
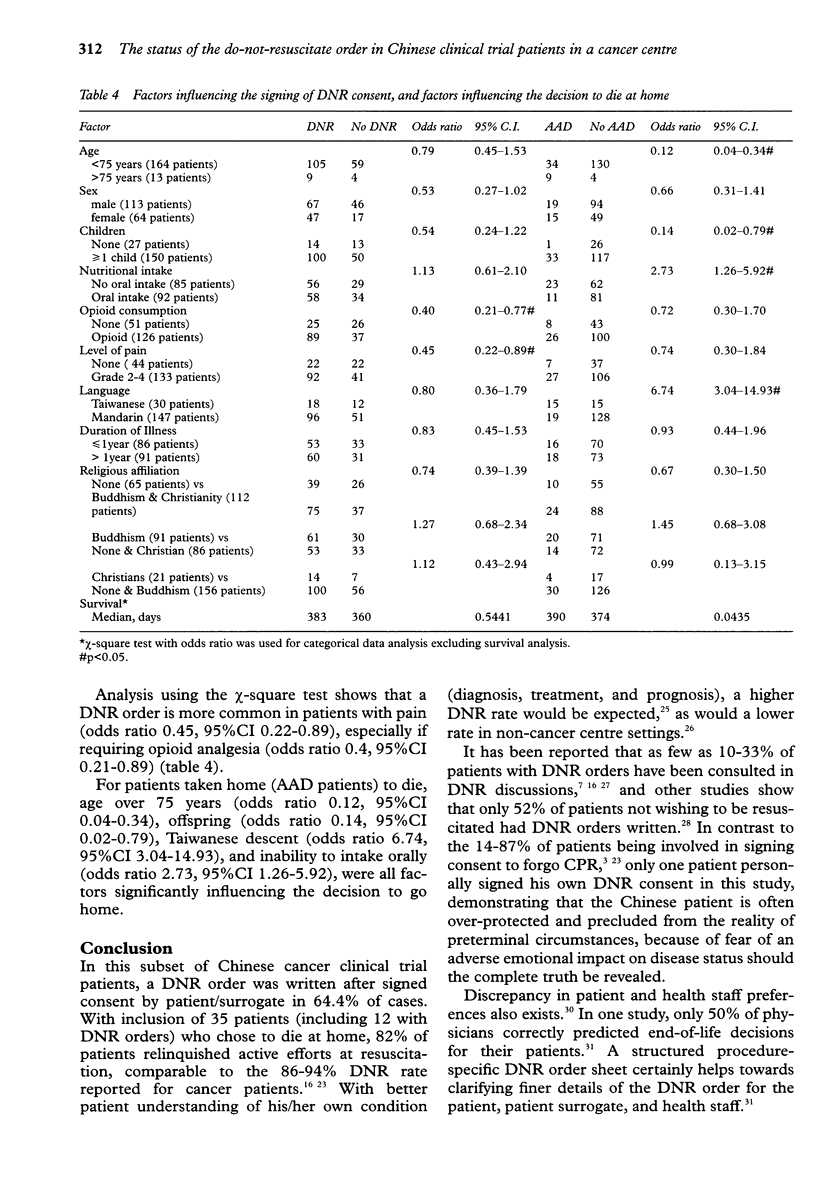
OBJECTIVE: To report and analyse the pattern of end-of-life decision making for terminal Chinese cancer patients. DESIGN: Retrospective descriptive study. SETTING: A cancer clinical trials unit in a large teaching hospital. PATIENTS: From April 1992 to August 1997, 177 consecutive deaths of cancer clinical trial patients were studied. MAIN MEASUREMENT: Basic demographic data, patient status at the time of signing a DNR consent, or at the moment of returning home to die are documented, and circumstances surrounding these events evaluated. RESULTS: DNR orders were written for 64.4% of patients. Patients in pain (odds ratio 0.45, 95% CI 0.22-0.89), especially if requiring opioid analgesia (odds ratio 0.40, 95% CI 0.21-0.77), were factors associated with a higher probability of such an order. Thirty-five patients were taken home to die, a more likely occurrence if the patient was over 75 years (odds ratio 0.12, 95% CI 0.04-0.34), had children (odds ratio 0.14, 95% CI 0.02-0.79), had Taiwanese as a first language (odds ratio 6.74, 95% CI 3.04-14.93), or was unable to intake orally (odds ratio 2.73, 95% CI 1.26-5.92). CPR was performed in 30 patients, none survived to discharge. CONCLUSIONS: DNR orders are instituted in a large proportion of dying Chinese cancer patients in a cancer centre, however, the order is seldom signed by the patient personally. This study also illustrates that as many as 20% of dying patients are taken home to die, in accordance with local custom.
Full text
PDF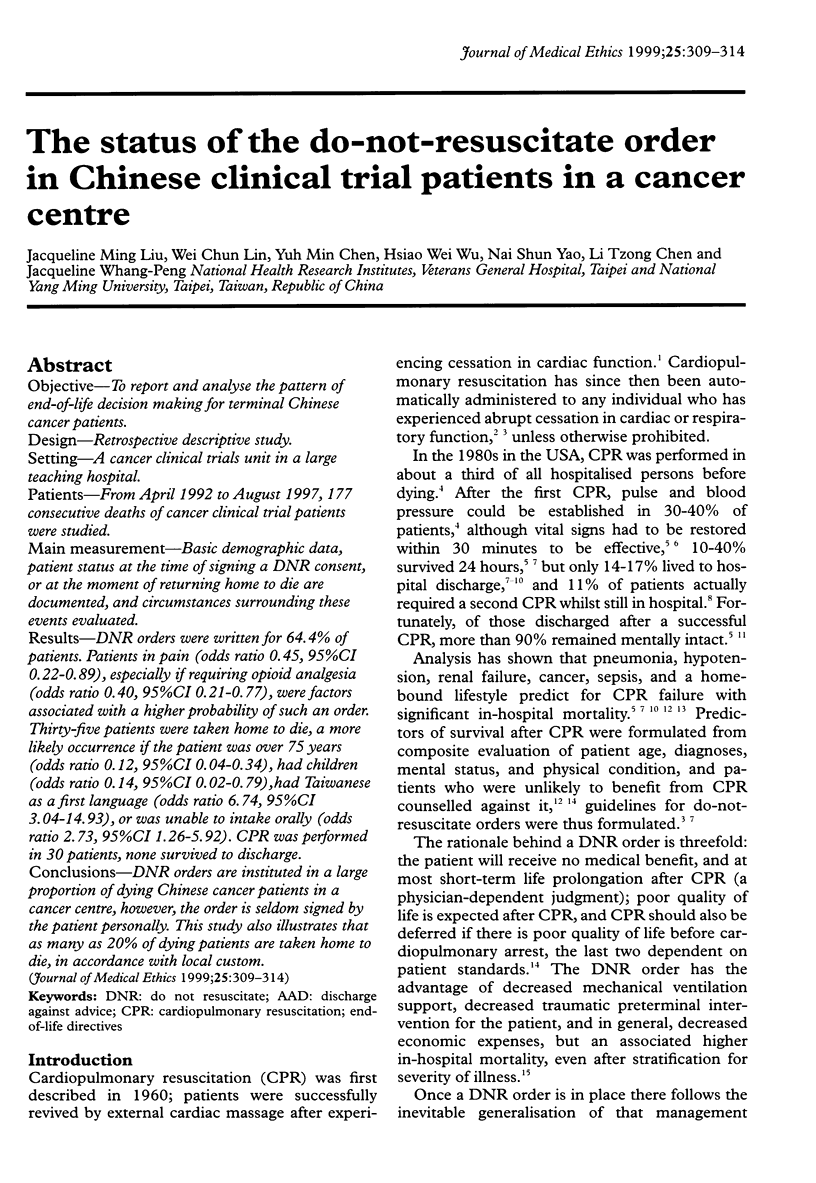
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ballew K. A., Philbrick J. T., Caven D. E., Schorling J. B. Predictors of survival following in-hospital cardiopulmonary resuscitation. A moving target. Arch Intern Med. 1994 Nov 14;154(21):2426–2432. [PubMed] [Google Scholar]
- Bedell S. E., Delbanco T. L. Choices about cardiopulmonary resuscitation in the hospital. When do physicians talk with patients? N Engl J Med. 1984 Apr 26;310(17):1089–1093. doi: 10.1056/NEJM198404263101706. [DOI] [PubMed] [Google Scholar]
- Bedell S. E., Delbanco T. L., Cook E. F., Epstein F. H. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med. 1983 Sep 8;309(10):569–576. doi: 10.1056/NEJM198309083091001. [DOI] [PubMed] [Google Scholar]
- Craig G. M. On withholding artificial hydration and nutrition from terminally ill sedated patients. The debate continues. J Med Ethics. 1996 Jun;22(3):147–153. doi: 10.1136/jme.22.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebell M. H. Practical guidelines for do-not-resuscitate orders. Am Fam Physician. 1994 Nov 1;50(6):1293-9, 1303-4. [PubMed] [Google Scholar]
- Ebell M. H., Preston P. S. The effect of the APACHE II score and selected clinical variables on survival following cardiopulmonary resuscitation. Fam Med. 1993 Mar;25(3):191–196. [PubMed] [Google Scholar]
- Evans A. L., Brody B. A. The do-not-resuscitate order in teaching hospitals. JAMA. 1985 Apr 19;253(15):2236–2239. [PubMed] [Google Scholar]
- Fukaura A., Tazawa H., Nakajima H., Adachi M. Do-not-resuscitate orders at a teaching hospital in Japan. N Engl J Med. 1995 Sep 21;333(12):805–808. doi: 10.1056/NEJM199509213331218. [DOI] [PubMed] [Google Scholar]
- Hakim R. B., Teno J. M., Harrell F. E., Jr, Knaus W. A., Wenger N., Phillips R. S., Layde P., Califf R., Connors A. F., Jr, Lynn J. Factors associated with do-not-resuscitate orders: patients' preferences, prognoses, and physicians' judgments. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1996 Aug 15;125(4):284–293. doi: 10.7326/0003-4819-125-4-199608150-00005. [DOI] [PubMed] [Google Scholar]
- Hare J., Pratt C., Nelson C. Agreement between patients and their self-selected surrogates on difficult medical decisions. Arch Intern Med. 1992 May;152(5):1049–1054. [PubMed] [Google Scholar]
- Heffner J. E., Barbieri C., Casey K. Procedure-specific do-not-resuscitate orders. Effect on communication of treatment limitations. Arch Intern Med. 1996 Apr 8;156(7):793–797. [PubMed] [Google Scholar]
- Hunt R., Bonett A., Roder D. Trends in the terminal care of cancer patients: South Australia, 1981-1990. Aust N Z J Med. 1993 Jun;23(3):245–251. doi: 10.1111/j.1445-5994.1993.tb01725.x. [DOI] [PubMed] [Google Scholar]
- Johnston S. C., Pfeifer M. P., McNutt R. The discussion about advance directives. Patient and physician opinions regarding when and how it should be conducted. End of Life Study Group. Arch Intern Med. 1995 May 22;155(10):1025–1030. doi: 10.1001/archinte.155.10.1025. [DOI] [PubMed] [Google Scholar]
- Jonsson P. V., McNamee M., Campion E. W. The 'Do not resuscitate' order. A profile of its changing use. Arch Intern Med. 1988 Nov;148(11):2373–2375. [PubMed] [Google Scholar]
- Kai I., Ohi G., Yano E., Kobayashi Y., Miyama T., Niino N., Naka K. Communication between patients and physicians about terminal care: a survey in Japan. Soc Sci Med. 1993 May;36(9):1151–1159. doi: 10.1016/0277-9536(93)90235-v. [DOI] [PubMed] [Google Scholar]
- Layson R. T., McConnell T. Must consent always be obtained for a do-not-resuscitate order? Arch Intern Med. 1996 Dec 9;156(22):2617–2620. [PubMed] [Google Scholar]
- Löfmark R., Nilstun T. Do-not-resuscitate orders--should the patient be informed? J Intern Med. 1997 May;241(5):421–425. doi: 10.1046/j.1365-2796.1997.138144000.x. [DOI] [PubMed] [Google Scholar]
- McCann R. M., Hall W. J., Groth-Juncker A. Comfort care for terminally ill patients. The appropriate use of nutrition and hydration. JAMA. 1994 Oct 26;272(16):1263–1266. doi: 10.1001/jama.272.16.1263. [DOI] [PubMed] [Google Scholar]
- McGrath R. B. In-house cardiopulmonary resuscitation--after a quarter of a century. Ann Emerg Med. 1987 Dec;16(12):1365–1368. doi: 10.1016/s0196-0644(87)80420-1. [DOI] [PubMed] [Google Scholar]
- Misbin R. I., O'Hare D., Lederberg M. S., Holland J. C. Compliance with New York State's do-not-resuscitate law at Memorial Sloan-Kettering Cancer Center. A review of patient deaths. N Y State J Med. 1993 Mar;93(3):165–168. [PubMed] [Google Scholar]
- Murphy D. J., Burrows D., Santilli S., Kemp A. W., Tenner S., Kreling B., Teno J. The influence of the probability of survival on patients' preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994 Feb 24;330(8):545–549. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- Owen C., Tennant C., Levi J., Jones M. Resuscitation in cancer. Comparison of patient and health staff preferences. Gen Hosp Psychiatry. 1994 Jul;16(4):277–285. doi: 10.1016/0163-8343(94)90007-8. [DOI] [PubMed] [Google Scholar]
- Owen C., Tennant C., Levi J., Jones M. Resuscitation. Patient and staff attitudes in the context of cancer. Gen Hosp Psychiatry. 1992 Sep;14(5):327–333. doi: 10.1016/0163-8343(92)90067-k. [DOI] [PubMed] [Google Scholar]
- Perkins H. S., Bauer R. L., Hazuda H. P., Schoolfield J. D. Impact of legal liability, family wishes, and other "external factors" on physicians' life-support decisions. Am J Med. 1990 Aug;89(2):185–194. doi: 10.1016/0002-9343(90)90298-r. [DOI] [PubMed] [Google Scholar]
- Pijnenborg L., van Delden J. J., Kardaun J. W., Glerum J. J., van der Maas P. J. Nationwide study of decisions concerning the end of life in general practice in The Netherlands. BMJ. 1994 Nov 5;309(6963):1209–1212. doi: 10.1136/bmj.309.6963.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly B. M., Magnussen C. R., Ross J., Ash J., Papa L., Wagner M. Can we talk? Inpatient discussions about advance directives in a community hospital. Attending physicians' attitudes, their inpatients' wishes, and reported experience. Arch Intern Med. 1994 Oct 24;154(20):2299–2308. [PubMed] [Google Scholar]
- Schiedermayer D. L. The decision to forgo CPR in the elderly patient. JAMA. 1988 Oct 14;260(14):2096–2097. [PubMed] [Google Scholar]
- Skerritt U., Pitt B. 'Do not resuscitate': How? why? and when? Int J Geriatr Psychiatry. 1997 Jun;12(6):667–670. [PubMed] [Google Scholar]
- Taylor E. M., Parker S., Ramsay M. P., Peart N. S. The introduction and auditing of a formal do not resuscitate policy. N Z Med J. 1996 Nov 8;109(1033):424–428. [PubMed] [Google Scholar]
- Thorpe G. Enabling more dying people to remain at home. BMJ. 1993 Oct 9;307(6909):915–918. doi: 10.1136/bmj.307.6909.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlinson T., Brody H. Ethics and communication in do-not-resuscitate orders. N Engl J Med. 1988 Jan 7;318(1):43–46. doi: 10.1056/NEJM198801073180109. [DOI] [PubMed] [Google Scholar]
- Tulsky J. A., Chesney M. A., Lo B. See one, do one, teach one? House staff experience discussing do-not-resuscitate orders. Arch Intern Med. 1996 Jun 24;156(12):1285–1289. doi: 10.1001/archinte.156.12.1285. [DOI] [PubMed] [Google Scholar]
- Wenger N. S., Pearson M. L., Desmond K. A., Brook R. H., Kahn K. L. Outcomes of patients with do-not-resuscitate orders. Toward an understanding of what do-not-resuscitate orders mean and how they affect patients. Arch Intern Med. 1995 Oct 23;155(19):2063–2068. [PubMed] [Google Scholar]
- Wenger N. S., Pearson M. L., Desmond K. A., Harrison E. R., Rubenstein L. V., Rogers W. H., Kahn K. L. Epidemiology of do-not-resuscitate orders. Disparity by age, diagnosis, gender, race, and functional impairment. Arch Intern Med. 1995 Oct 23;155(19):2056–2062. [PubMed] [Google Scholar]



