Abstract
Objective:
The purpose of this study was to evaluate compliance with guidelines in surgical prophylaxis (SP) procedures in Turkey.
Materials and Methods:
A point prevalence study involving 4 university, 5 education and research and 7 public hospitals was performed assessing compliance with guidelines for antibiotic use in SP. Compliance was based on the “Clinical Practice Guidelines for Antimicrobial Surgery (CPGAS) 2013” guideline.
Results:
Sixteen centers were included in the study, with 166 operations performed at these being evaluated. Parenteral antibiotic for SP was applied in 161 (96.9%) of these. Type of antibiotic was inappropriate in 66 (40.9%) cases and duration of use in 47 (29.1%). The main antibiotics used inappropriately in SP were ceftriaxone, glycopeptides and aminoglycosides. No significant difference was observed between secondary and tertiary hospitals in terms of inappropriate selection. Duration of prophylaxis was also incompatible with guideline recommendations in approximately half of surgical procedures performed in both secondary and tertiary hospitals, however statistical significance was observed between institutions in favor of tertiary hospitals.
Conclusion:
Antibiotics are to a considerable extent used in a manner incompatible with guidelines even in tertiary hospitals in Turkey. It must not be forgotten that several pre-, intra- and postoperative factors can be involved in the development of surgical site infections (SSI), and antibiotics are not the only option available for preventing these. A significant improvement can be achieved in prophylaxis with close observation, educational activities, collaboration with the surgical team and increasing compliance with guidelines. All health institutions must establish and apply their own SP consensus accompanied by the guidelines in order to achieve success in SP.
Keywords: Surgical prophylaxis, antibiotics, Turkey
Öz
Amaç:
Bu çalışmanın amacı, ülkemizdeki cerrahi proflaksi uygulamalarının rehberlere uygunluğunun değerlendirilmesidir.
Gereç ve Yöntem:
Bu amaçla, 4 üniversite, 5 eğitim-araştırma ve 7 devlet hastanesini içine alan bir nokta prevalans çalışması yapılmıştır. Cerrahi proflaksideki uygunluğunun değerlendirilmesinde “Clinical Practice Guidelines for Antimicrobial Surgery (CPGAS) 2013” rehberi baz alınmıştır.
Bulgular:
Toplam 16 merkez çalışmaya katılmış olup, bu merkezlerdeki 166 operasyon değerlendirilmiştir. Bunların 161’inde (%96,9) cerrahi proflaksi amacıyla parenteral antibiyotik uygulanmıştır. Olguların 66’sında (%40,9) kullanılan antibiyotiğin türü, 47’sinde (%29,1) ise süresi uygunsuz bulunmuştur. Cerrahi proflakside uygunsuz kullanılan antibiyotikler olarak en çok; seftriakson, glikopeptidler ve aminoglikozitler dikkati çekmektedir. İkinci ve 3.basamak sağlık kuruluşları arasında antibiyotik seçimindeki uygunsuzluk açısından anlamlı bir fark görülmemiştir. Cerrahi uygulamaların yaklaşık yarısında proflaktik antibiyotiklerin süresi rehber önerileriyle uyumlu bulunmamış olmakla birlikte; istatistiksel olarak 3.basamak hastanelerinin lehine bir durum olduğu görülmüştür.
Sonuç:
Cerrahi proflakside ülkemiz 3.basamak hastanelerinde bile büyük oranda antibiyotiklerin rehberlere uygunsuz kullanıldığı görülmektedir. Sonuç olarak bakıldığında; cerrahi alan enfeksiyonlarının gelişmesinde pre, intra ve post operatif birçok faktörün etkili olduğu unutulmamalı ve bunların önlenmesinde antibiyotikler tek seçenek olarak görülmemelidir. Yakın gözlem, eğitim faaliyetleri, cerrahi ekiple olan işbirliği ve kılavuzlara uyumun artırılması ile proflakside belirgin bir iyileşme sağlanabilmektedir. Cerrahi proflakside başarıya ulaşabilmek için her sağlık kurumunun kılavuzlar eşliğinde kendi cerrahi proflaksi konsensusunu oluşturması gerekli olup uygulamalar bu ortak konsensüs çerçevesinde yapılmalıdır.
Introduction
The first approach that comes to mind in the context of surgical prophylaxis (SP) is the use of parenteral antibiotics. However, antibiotics are unable to prevent surgical site infections (SSI) alone, and a number of pre-, intra- and postoperative conditions need to be met [1–3]. Nonetheless, excessive reliance is placed on antibiotics in SP, and there is a tendency for antibiotics to be used inappropriately in clinical practice [4–9]. While previous studies have investigated the place of antibiotics in SP in Turkey, our study is the first multi-center study to evaluate SP administration simultaneously in university, research and training and public hospitals.
Materials and Methods
A point prevalence study involving 4 university, 5 education and research and 7 public hospitals and assessing compliance with guidelines for antibiotic use in SP was performed on 29.01.2015. The study was conducted according to the principles of Helsinki Declaration at the School of Medicine, Karadeniz Technical University, Trabzon, Turkey. The hospital ethical committee approved the study before commencement. Assessment of suitability of SP was based on “Clinical Practice Guidelines for Antimicrobial Surgery (CPGAS) 2013” prepared on the basis of the common opinions of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Surgical Infection Society, and the Society for Healthcare Epidemiology of America [10]. Appropriateness of type of antibiotics selected and length of use was investigated. During the statistical analysis, categorical data were compared using the Chi-square test (Epi Info 7; CDC, USA) and the results of the analysis were presented as P values. P<0.05 was regarded as statistically significant.
Results
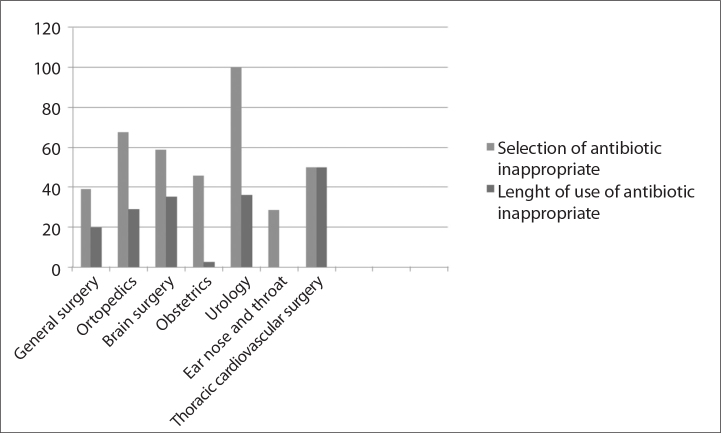
Sixteen centers participated in the study, with 166 operations performed at these being evaluated. Parenteral antibiotic for SP was applied in 161 (96.9%) of these. One-hundred (62.1%) of patients were male, 61 (37.9%) female. Avarage age of patients was 45±23 (22–78). Type of antibiotic was inappropriate in 66 (40.9%) cases and duration of use in 47 (29.1%). Urology, orthopedics and brain surgery were the branches where inappropriate SP was most common. The antibiotics most commonly used inappropriately in SP were ceftriaxone, glycopeptides and aminoglycosides. Assessment of antibiotics for SP by branch is shown in Figure 1.
Figure 1.
Inappropriate use of antibiotics in surgical prophylaxis by branches.
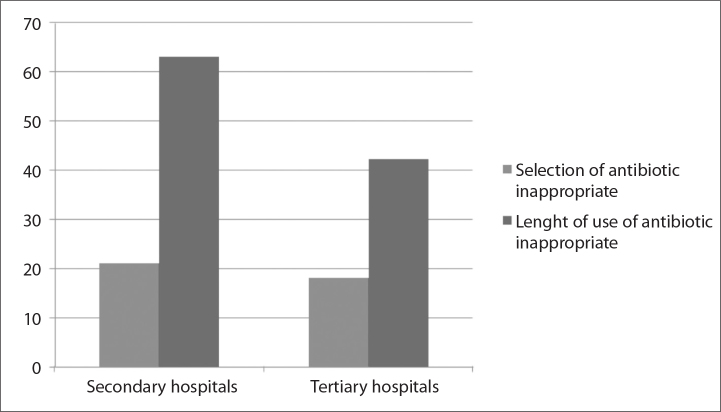
Comparing secondary and tertiary hospitals, antibiotic selection was in appropriate in 8 (21%) out of 38 cases and length of use was inappropriate in 24 (63.2%) of cases in secondary hospitals. In tertiary hospitals, choice of antibiotic was inappropriate in 26 (18.1%) of 123 cases and length of use was inappropriate in 52 (42.4%) of cases (p 0.829 and 0.024, respectively) (Figure 2).
Figure 2.
Levels of inappropriate use in surgical prophylaxis in secondary and tertiary health institutions.
Discussion
Use of parental antibiotics in patients hospitalized in Turkey has been legally subject to supervision by infectious disease specialists since 2003 [11]. In addition, various factors such as physical conditions, and health team numbers and training levels affect the development of infections, and it is a known fact that ideal conditions are not being achieved even in many university or education-research hospitals in Turkey [12–15]. These deficiencies increase surgical team concerns over SSIs, resulting in the infectious diseases specialist receiving intense demands for antibiotics. These demands may sometimes involve practices that are incompatible with SP guidelines.
Incorrect procedures in SP may be associated with a number of factors, such as choice of antibiotic, time and length of administration, and dosage [4–9]. One of the most frequently encountered of these is incorrect choice of antibiotic [7, 8]. The ideal agent to be used in SP must be as broad-spectrum as possible, have minimal side-effects, be highly concentrated in the surgical wound tissue and be inexpensive. Since it meets all these criteria, cefazolin is the most commonly recommended agent in SP in several contemporary guidelines [9]. One study from Turkey reported that antibiotics are used inappropriately to a large extent in SP, and that penicillin combinations including beta-lactamase inhibitors, cephalosporins, quinolones and even carbapenems are the most commonly prescribed drugs for this purpose [5]. Cefazolin was the most widely used antibiotic in SP in this study. Other antibiotics used for the purpose of SP include 2nd and 3rd generation cephalosporins, aminoglycosides, quinolones, ampicillin-sulbactam, clindamycin and teicoplanin, of which ceftriaxone, aminoglycosides and teicoplanin were the most frequently inappropriately used antibiotics. Approximately 1/3–1/4 of antibiotics used in SP consist of those not recommended by the CPGAS. Inappropriate use is more evident in major branches such as general surgery and orthopedics.
In terms of general guideline recommendations regarding the length of antibiotic administration in SP, a single dose of the prophylactic agent concerned following induction of anesthesia is usually sufficient. A single additional dose is recommended for some operations, and total length of SP should not exceed 24 h [8–10, 16]. One error that is frequently made in Turkey is unnecessarily prolonged use of antibiotics in prophylaxis [4, 17]. Since long-term antibiotic use creates a false sense of security in the surgical team it is a phenomenon frequently encountered in clinical practice. Infectious diseases specialists sometimes approve incorrect procedures, and erroneous practices incompatible with guideline recommendations may therefore be seen in several institutions. In a retrospective study investigating CP, Özkurt et al. [7] reported that the duration of 82.8% of antibiotics used in SP was inappropriate and selection antibiotic in 66.4%. In a point prevalence study involving two different days in 2011 and 2012, Bozkurt et al. [5] showed that 88.5% and 43.7%, respectively of antibiotics in SP were used inappropriately. In a multicenter study from Turkey, Hoşoğlu et al. [8] showed that 32% of antibiotics in SP were not selected appropriately and that 80% were used for more than 24 h. The most common error in our study was inappropriate duration of prophylaxis. Duration of prophylaxis was incompatible with guideline recommendations in approximately half of surgical procedures performed in both secondary and tertiary hospitals, however statistical significance was observed between institutions in favor of tertiary hospitals. In conclusion, antibiotics are to a large extent used inappropriately even in teaching institutions.
Studies of SP performed outside Turkey reveal serious problems in other countries, as well. Gagliotti et al. [18] reported that the most common error, at a level of 41%, concerned length of antibiotic use. A study in which theAPACHE study group assessed 765 surgical operations reported that correct decisions regarding antibiotic selection, duration and timing were made in only 8% of cases [15]. Another study reported inappropriate length of antibiotic use in more than half of 250 surgical cases [1]. A prospective study involving assessing application of SP in general, orthopedic and gynecological surgeryreported appropriate antibiotic selection in only 18.5% of cases and appropriate length of use in 31.8% [19].
Inappropriate antibiotic use in SP can lead to various adverse outcomes, such as selection of resistant micro-organisms and increased costs [8, 15, 20]. Prevention of inappropriate use must represent a priority in Turkey, as in other countries. In particular, it must be remembered at antibiotics are not the only option in protection from SSI. A significant improvement can be achieved in prophylaxis with close observation, educational activities, and increasing compliance with guidelines [4, 20]. Improvements from 35% to 100%% in terms of dose and duration have been reported with the development and application of common SP protocols in collaboration with the surgical team [4, 5]. All health institutions must establish and apply their own SP consensus accompanied by the guidelines in order to achieve success in SP.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Karadeniz Technical University, Farabi Hospital.
Informed Consent: Written informed consent was not obtained from patients due to the nature of this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - S.K., I.K., S.A.; Design - S.K., I.K., S.A.; Supervision - S.K.; Resources - S.K., S.A., S.S., R.T., N.O., F.A., P.F., S.Y., A.O., A.G., S.S., A.K., S.E.C., D.Ç., H.Y., I.B., T.E., A.S.T., A.A., N.F.K., I.K.; Materials - S.K., S.A., I.K. Data Collection and/or Processing - S.K.; Analysis and/or Interpretation - S.K, İ.K.; Literature Search - S.K.; Writing Manuscript - S.K.; Critical Review - S.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.El Hassan M, Elnour AA, Farah FH, et al. Clinical pharmacists’ review of surgical antimicrobial prophylaxis in a tertiary hospital in Abu Dhabi. Int J Clin Pharm. 2015;37:18–22. doi: 10.1007/s11096-014-0045-4. http://dx.doi.org/10.1007/s11096-014-0045-4. [DOI] [PubMed] [Google Scholar]
- 2.Young PY, Khadaroo RG. Surgical site infections. Surg Clin North Am. 2014;94:1245–64. doi: 10.1016/j.suc.2014.08.008. http://dx.doi.org/10.1016/j.suc.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 3.Cooper RA. Surgical site infections: epidemiology and microbiological aspects in trauma and orthopaedic surgery. Int Wound J. 2013;10(Suppl 1):3–8. doi: 10.1111/iwj.12179. http://dx.doi.org/10.1111/iwj.12179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bozkurt F, Kaya S, Gülsün R, et al. Assessment of perioperative antimicrobial prophylaxis using ATC/DDD methodology. Int J Infect Dis. 2013;17:e1212–7. doi: 10.1016/j.ijid.2013.08.003. http://dx.doi.org/10.1016/j.ijid.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Bozkurt F, Kaya S, Gülsün R, et al. Analysis of antimicrobial consumption and cost in a teaching hospital. J Infect Public Health. 2014;7:161–9. doi: 10.1016/j.jiph.2013.09.007. http://dx.doi.org/10.1016/j.jiph.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Tuna N, Öğütlü A, Sandıkcı Ö, et al. Bir araştırma hastanesinde cerrahi proflaksi uygulamalarının gözden geçirilmesi. Ankem Derg. 2010;24:92–5. [Google Scholar]
- 7.Özkurt Z, Kadanalı A, Ertek M, Erol S, Parlak M. Cerrahi proflakside antibiyotik kullanımı. Ankem Derg. 2005;19:111–4. [Google Scholar]
- 8.Hosoglu S, Sunbul M, Erol S, et al. Surgical antibiotic prophylaxis in Turkey: a survey study. Infect Control Hosp Epidemiol. 2003;24:758–61. doi: 10.1086/502127. http://dx.doi.org/10.1086/502127. [DOI] [PubMed] [Google Scholar]
- 9.Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195–283. doi: 10.2146/ajhp120568. http://dx.doi.org/10.2146/ajhp120568. [DOI] [PubMed] [Google Scholar]
- 10.Sipahi OR. Economics of antibiotic resistance. Expert Rev Anti Infect Ther. 2008;6:523–39. doi: 10.1586/14787210.6.4.523. http://dx.doi.org/10.1586/14787210.6.4.523. [DOI] [PubMed] [Google Scholar]
- 11.Lamagni T, Elgohari S, Harrington P. Trends in surgical site infections following orthopaedic surgery. Curr Opin Infect Dis. 2015;28:125–32. doi: 10.1097/QCO.0000000000000143. http://dx.doi.org/10.1097/QCO.0000000000000143. [DOI] [PubMed] [Google Scholar]
- 12.Lejus C, Dumont R, Gall CL, et al. A preoperative stay in an intensive care unit is associated with an increased risk of surgical site infection in neonates. J Pediatr Surg. 2013;48:1503–8. doi: 10.1016/j.jpedsurg.2013.01.055. http://dx.doi.org/10.1016/j.jpedsurg.2013.01.055. [DOI] [PubMed] [Google Scholar]
- 13.Sinha B, van Assen S, Friedrich AW. Important issues for perioperative systemic antimicrobial prophylaxis in surgery. Curr Opin Anaesthesiol. 2014;27:377–81. doi: 10.1097/ACO.0000000000000097. http://dx.doi.org/10.1097/ACO.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 14.Yalcın AN, Erbay RH, Serin S, Atalay H, Oner O, Yalcın AD. Perioperative antibiotic prophylaxis and cost in a Turkish University Hospital. Infez Med. 2007;15:99–104. [PubMed] [Google Scholar]
- 15.Ciofi Degli Atti M, Spila Alegiani S, Raschetti R, et al. Surgical antibiotic prophylaxis in children: adherence to indication, choice of agent, timing, and duration. Eur J Clin Pharmacol. 2015;71:483–8. doi: 10.1007/s00228-015-1816-0. http://dx.doi.org/10.1007/s00228-015-1816-0. [DOI] [PubMed] [Google Scholar]
- 16.Yalcın AN, Serin S, Gurses E, Zencir M. Surgical antibiotic prophylaxis in a Turkish University Hospital. J Chemother. 2002;14:373–7. doi: 10.1179/joc.2002.14.4.373. http://dx.doi.org/10.1179/joc.2002.14.4.373. [DOI] [PubMed] [Google Scholar]
- 17.Gagliotti C, Ravaglia F, Resi D, Moro ML. Quality of local guidelines for surgical antimicrobial prophylaxis. J Hosp Infect. 2004;56:67–70. doi: 10.1016/j.jhin.2003.09.007. http://dx.doi.org/10.1016/j.jhin.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 18.Graham HE, Vasireddy A, Nehra D. A national audit of antibiotic prophylaxis in elective laparoscopic cholecystectomy. Ann R Coll Surg Engl. 2014;96:377–80. doi: 10.1308/003588414X13946184900688. http://dx.doi.org/10.1308/003588414X13946184900688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Musmar SM, Baba H, Owais A. Adherence to guidelines of antibiotic prophylactic use in surgery: a prospective cohort study in North West Bank, Palestine. BMC Surg. 2014;14:69. doi: 10.1186/1471-2482-14-69. http://dx.doi.org/10.1186/1471-2482-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ozgun H, Ertugrul BM, Soyder A, Ozturk B, Aydemir M. Perioperative antibiotic prophylaxis: adherence to guidelines and effects of educational intervention. Int J Surg. 2010;8:159–63. doi: 10.1016/j.ijsu.2009.12.005. http://dx.doi.org/10.1016/j.ijsu.2009.12.005. [DOI] [PubMed] [Google Scholar]