Abstract
Thyroid sarcoma is a very rare entity, accounting for less than 1% of all malignant thyroid tumours. Rhabdomyosarcoma (RMS) is a sarcoma subtype, which is more common in children and adolescents. In this case, a 68-year old man, presented with hoarseness and diagnosed with pleomorphic RMS, was explored. No study of primary thyroid pure RMS has been reported in the literature, with the exception of the case reports of differentiated RMS.
Keywords: Pleomorphic rhabdomyosarcoma, adult, thyroid cancer
Öz
Tiroid sarkomu, tüm tiroid malignitelerinin %1’inden azını oluşturan oldukça nadir bir klinik antitedir. Rabdomyosarkom (RMS) coçuk ve adölesanlarda daha yaygın görülen sarkom subtiptidir. Diferansiye RMS vaka sunumları hariç, primer saf tiroid RMS vakası rapor edilmemiştir. Biz ses kısıklığı ile şikayeti ile başvuran ve pleomorfik RMS tanısı konulan 68 yaşında erkek hastayı sunduk.
Introduction
The most common thyroid cancers are papillary and follicular thyroid carcinomas, accounting for 90% of all thyroid malignancies [1]. Thyroid sarcomas are uncommon tumours, accounting for less than 1% of all thyroid malignancies [2]. Rhabdomyosarcoma (RMS) is a tumour of skeletal muscle that originates from embryonic mesenchymal tissue. RMS is the most common connective tissue sarcoma and accounts for 4–6% of the malignancies among children and young adults. In the paediatric population, approximately 40% of the RMSs are seen in the head and neck region [3]. RMS frequency decreases with advancing age. Pleomorphic rhabdomyosarcoma is more common in men and the median age of onset corresponds to the sixth decade of life [4–7]. In this study, we present a case of pure RMS of the thyroid gland in an adult patient.
Case Report
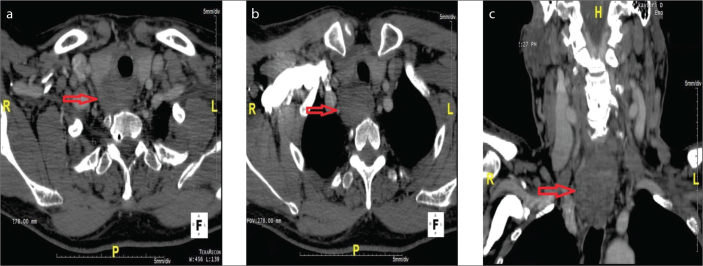
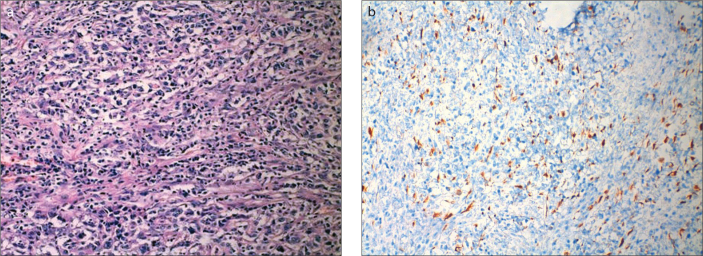
A 68-year old man, presented with hoarseness, referred to our clinic. There was no abnormal feature other than smoking in his history. On the physical examination, a nodule (5×4 cm in size) was detected in the right lobe of the thyroid gland of the patient, who was otherwise healthy. A hypoechoic, solid mass lesion (47×27 mm in size) with lobulated contours was detected on thyroid sonography. Computed Tomography (CT) scan showed a mass lesion (55×40×30 mm in size) with malignant appearance, which was originated from the infero-posterior region of the right thyroid lobe and spreading to mediastinum, and which had vague demarcation with the cervical esophagus and trachea, was detected (Figure 1); then he underwent bilateral total thyroidectomy. Surgery revealed a mass (5 cm in diameter), which was invading esophagus at the posterior region of right thyroid lobe and recurrent laryngeal nerve. The surgical specimen was reported as pleomorphic rhabdomyosarcoma after pathological evaluation. Immunohistochemical evaluations revealed positive staining for vimentin and desmin, whereas negative staining for CD38, CD34, Bcl-2, thyroglobulin, TTF-1, pan-keratin, pancreatin, LCA, SMA, S100 and CD117. The number of mitoses was 4–5 at 10X magnification and the Ki67 proliferation index was 40% (Figure 2). During surgery, the mass was removed totally and surgical margins were negative. Moreover, there was no regional lymph node involvement or distant metastasis, so that, it was decided to follow-up without any additional treatment.
Figure 1. a–c.
Tomography Scanning of the case: Axial contrast enhanced CT images (a, b) at the level of cervical trachea show a heterogeneous hypoattenuating mass in the right posterior thyroid gland. Coronal reformatted contrast enhanced CT image (c) it is demonstrated that mass extends the retrosternal space.
Figure 2. a, b.
Histopathological and immunohistochemical imaging of the case: a) Most of the tumour cells are spindled and arranged in interlacing fascicles. The nuclei are large and pleomorphic, and mitotic figures are easily found (10×). A minor component of the tumour displays “rhabdoid” tumour cells with distinct cytoplasmic borders, voluminous pink to red cytoplasm, eccentric nuclei and prominent nucleoli (100×). b) Immunohistochemical positive staining for desmin.
Discussion
RMSs constitute 3% of all soft-tissue sarcomas [8]. Traditionally, RMS has been classified as alveolar, embryonal and pleomorphic. Alveolar and embryonal variants are more commonly seen in paediatric and adolescent populations, while the pleomorphic variant is more common in adults and in the lower limbs [5]. There is a male predominance for RMSs [6]. The identification of subtype is essential, as there is a significant difference between subtypes regarding prognosis. RMSs localized in the head and neck region are classified into 3 subtypes including orbital, parameningeal and nonparameningeal. Among them, the best prognosis is seen in orbital subtype [9].
Pleomorphic RMSs are seen commonly in middle-aged men with a median age of 54–56 years and most commonly involve the lower limbs. However, they may also involve the abdomen, retroperitoneum, chest wall, spermatic cord/testes, upper limbs, mouth and orbit more rarely. Because of the aggressive behaviour of tumour, prognosis is generally poor in RMSs [5, 6].
Up to date, the reported cases of thyroid sarcomas in the literature are as follows: Kaposi sarcoma, leiomyosarcoma, radiation-induced sarcoma, fibro sarcoma, angio sarcoma, Ewing sarcoma and synovial sarcoma [10–16]. However, they were not large series but only case reports. Primary RMS of the thyroid gland is a truly rare malignancy. Up to now, only 4 cases have been reported, these include 2 cases with anaplastic thyroid carcinoma exhibiting RMS differentiation [17] and 2 cases who were child, in whom thyroid gland tissue was detected within anterior cervical tissue and diagnosed as RMS [18, 19] (Table 1). These tumours also exhibited the characteristics of aggressive tumour by invading the surrounding tissue as in our case. RMS generally presents with bulky mass and compression of the surrounding tissues. In a study, it was reported that RMS was detected in one of 77 children, in whom the etiology of thyroid nodules was evaluated [20]. In addition, Hafez MT et al. have reported a metastasis to the thyroid gland from RMS originated from lower limb as a case [21]. To the best of our knowledge, there is no previous report about primary pleomorphic RMS in an adult patient.
Table 1.
Cases of primary thyroid sarcomas in the literature
| Cases | Age | Gender | Type of tumour |
|---|---|---|---|
| Griem et al. [12], 1989 | 23 years | Male | Radiation-induced sarcoma |
| Poniecka et al. [10], 2007 | 45 years | Female | Kaposi sarcoma |
| Yeo [13], 2009 (9 cases in literature) | 6th–7th decades | Male (generally) | Fibro sarcoma |
| Petronella et al. [14] 2012 | 71 years | Male | Angio sarcoma |
| Chirila et al. [15] 2013 | 48 years | Male | Ewing sarcoma |
| Boudin et al. [16] 2014 | 55 years | Male | Synovial sarcoma |
| Conza et al. [11], 2014 (12 cases in literature) | 6th–7th decades | Female (generally) | Leiomyosarcoma |
| Alexis et al. [18], 2005 | 7 months | Male | Rhabdomyosarcoma |
| Dutta et al. [19], 2013 | 7 years | Male | Rhabdomyosarcoma |
| Our case | 68 years | Male | Rhabdomyosarcoma |
Rhabdomyosarcomas generally have a very high mitotic rate, explaining the aggressive nature and poor prognosis of these tumours. Histologically, small blue cells are seen in pleomorphic RMSs and positive expression of desmin, myogen and myoD1 are most frequently seen [22]. Differential diagnosis includes anaplastic thyroid carcinoma with rhabdoid variant due to the presence in each variant of spindle cell elements. The majority of anaplastic (undifferentiated) thyroid tumours show ‘sarcoma-like’ features, with spindle-shaped neoplastic cells arranged in a fascicular or whorled pattern of growth. Immunohistochemical positive staining for keratins, confirm the epithelial nature of the tumour [17]. Immunohistochemical evaluations revealed positive staining for vimentin and desmin, whereas negative staining for pankeratin thus, rhabdoid variant of anaplastic thyroid carcinoma was excluded as in our case.
The imaging has no specific feature in RMS. On CT scan, it is similar to skeletal muscle and there is increased attenuation. However, imaging is usually helpful in staging as 44% of RMS cases have metastasis at the time of diagnosis. On MRI, it appears as homogenous mass, which has increased the signal intensity, when compared to muscle and fat, on T1-weighted images while isointensity or minimal hyperintensity could be detected, when compared to muscle, on T2-weighted images [4].
In conclusion, the thyroid gland can now be added to the list of infrequent involvement sites of pleomorphic RMS such as the upper limb, mouth, orbit, spermatic cord/testes, abdomen, retroperitoneum and chest wall. This could be translated as novel sites of involvement by pleomorphic RMS that will appear in the future.
Footnotes
Informed Consent: Written informed consent was obtained from the who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - E.O.; Design - V.B.; Supervision - E.O.; Resources - S.B.; Materials - S.S., G.C.; Data Collection and/ or Processing - A.O.D.; Analysis and/or Interpretation - O.B., B.E. Literature Search - E.O.; Writing Manuscript - E.O., V.B.; Critical Review - H.K., M.O.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Carling T, Udelsman R. Cancer of the Endocrine System. In: DeVita VT, Lawrence TS, Rosenberg SA, DePinho RA, Weinberg RA, editors. DeVita, Hellman And Rosenberg’s Cancer Principles Practice of Oncology. 8th edition. Lippincott Williams Wilkins; 2008. pp. 1669–70. [Google Scholar]
- 2.Melmed S. Nontoxic diffuse and nodular goiter and thyroid neoplasia. In: Schlumberger JM, Filetti S, Hay DL, editors. Williams textbook of endocrinology. 12th edition. Saunders Elsevier; Philadelphia: 2011. pp. 440–75. [Google Scholar]
- 3.Kraus DH, Saenz NC, Gollamudi S, et al. Pediatric rhabdomyosarcoma of the head and neck. Am J Surg. 1997;174:556–60. doi: 10.1016/s0002-9610(97)00171-2. http://dx.doi.org/10.1016/S0002-9610(97)00171-2. [DOI] [PubMed] [Google Scholar]
- 4.Davies CE, Davies AM, Kindblom LG, James SL. Soft tissue tumors with muscle differentiation. Semin Musculoskelet Radiol. 2010;14:245–56. doi: 10.1055/s-0030-1253165. http://dx.doi.org/10.1055/s-0030-1253165. [DOI] [PubMed] [Google Scholar]
- 5.Furlong MA, Mentzel T, Fanburg-Smith JC. Pleomorphic rhabdomyosarcoma in adults: a clinicopathologic study of 38 cases with emphasis on morphologic variants and recent skeletal muscle-specific markers. Mod Pathol. 2001;14:595–603. doi: 10.1038/modpathol.3880357. http://dx.doi.org/10.1038/modpathol.3880357. [DOI] [PubMed] [Google Scholar]
- 6.Gaffney EF, Dervan PA, Fletcher CD. Pleomorphic rhabdomyosarcoma in adulthood. Analysis of 11 cases with definition of diagnostic criteria. Am J Surg Pathol. 1993;17:601–9. http://dx.doi.org/10.1097/00000478-199306000-00008. [PubMed] [Google Scholar]
- 7.Hollowood K, Fletcher CD. Rhabdomyosarcoma in adults. Semin Diagn Pathol. 1994;11:47–57. [PubMed] [Google Scholar]
- 8.Weiss S, Goldblum JR. Rhabdomyosarcoma. In: Weiss S, Goldblum JR, editors. Enzinger and Weiss’s soft tissue tumors. 6th edition. St. Louis, MO: Mosby; 2014. pp. 601–2. [Google Scholar]
- 9.Nasri S, Mark RJ, Sercarz JA, Tran LM, Sadeghi S. Pediatric sarcomas of the head and neck other than rhabdomyosarcoma. Am J Otolaryngol. 1995;16:165–71. doi: 10.1016/0196-0709(95)90096-9. http://dx.doi.org/10.1016/0196-0709(95)90096-9. [DOI] [PubMed] [Google Scholar]
- 10.Poniecka A, Ghorab Z, Arnold D, Khaled A, Ganjei-Azar P. Kaposi’s sarcoma of the thyroid gland in an HIV-negative woman: a case report. Acta Cytol. 2007;51:421–3. doi: 10.1159/000325758. http://dx.doi.org/10.1159/000325758. [DOI] [PubMed] [Google Scholar]
- 11.Conzo G, Candela G, Tartaglia E, et al. Leiomyosarcoma of the thyroid gland: A case report and literature review. Oncol Lett. 2014;7:1011–4. doi: 10.3892/ol.2014.1853. http://dx.doi.org/10.3892/ol.2014.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griem KL, Robb PK, Caldarelli DD, Templeton AC. Radiation-induced sarcoma of the thyroid. Arch Otolaryngol Head Neck Surg. 1989;115:991–3. doi: 10.1001/archotol.1989.01860320101028. http://dx.doi.org/10.1001/archotol.1989.01860320101028. [DOI] [PubMed] [Google Scholar]
- 13.Yeo CK. Fibrosarcoma of the thyroid gland. J Otolaryngol Head Neck Surg. 2009;38:39–41. [PubMed] [Google Scholar]
- 14.Petronella P, Scorzelli M, Luise R, et al. Primary thyroid angiosarcoma: an unusual localization. World J Surg Oncol. 2012;10:73. doi: 10.1186/1477-7819-10-73. http://dx.doi.org/10.1186/1477-7819-10-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chirila M, Muresan M, Ciuleanu E, Cosgarea M. Extraosseous Ewing sarcoma and peripheral primitive neuroectodermal tumor of the thyroid gland: Case report and review. Ear Nose Throat J. 2013;92:E3–6. doi: 10.1177/014556131309200419. [DOI] [PubMed] [Google Scholar]
- 16.Boudin L, Fakhry N, Chetaille B, et al. Primary synovial sarcoma of the thyroid gland: case report and review of the literature. Case Rep Oncol. 2014;7:6–13. doi: 10.1159/000357913. http://dx.doi.org/10.1159/000357913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carda C, Ferrer J, Vilanova M, Peydró A, Llombart-Bosch A. Anaplastic carcinoma of the thyroid with rhabdomyosarcomatous differentiation: a report of two cases. Virchows Arch. 446:46–51. doi: 10.1007/s00428-004-1123-0. http://dx.doi.org/10.1007/s00428-004-1123-0. [DOI] [PubMed] [Google Scholar]
- 18.Alexis DF, David AL, Soham R. Rhabdomyosarcoma presenting as an anterior neck mass and possible thyroid malignancy in a seven-month-old. Int J Pediatr Otorhinolaryngol. 2005;69:267–70. doi: 10.1016/j.ijporl.2004.09.006. http://dx.doi.org/10.1016/j.ijporl.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Dutta M, Chatterjee I, Roy S, Gure PK. Primary embryonal rhabdomyosarcoma of the anterior neck and thyroid: report of a new case with review of the literature. Laryngoscope. 2013;123:2072–6. doi: 10.1002/lary.23794. http://dx.doi.org/10.1002/lary.23794. [DOI] [PubMed] [Google Scholar]
- 20.Kaur J, Srinivasan R, Arora SK, et al. Fine-needle aspiration in the evaluation of thyroid lesions in children. Diagn Cytopathol. 2012;40:33–7. doi: 10.1002/dc.21568. http://dx.doi.org/10.1002/dc.21568. [DOI] [PubMed] [Google Scholar]
- 21.Hafez MT, Hegazy MA, Abd Elwahab K, Arafa M, Abdou I, Refky B. Metastatic rhabdomyosarcoma of the thyroid gland, a case report. Head Neck Oncol. 2012;29:27. doi: 10.1186/1758-3284-4-27. http://dx.doi.org/10.1186/1758-3284-4-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allen SD, Moskovic EC, Fisher C, Thomas JM. Adult rhabdomyosarcoma: cross-sectional imaging findings including histopathologic correlation. AJR Am J Roentgenol. 2007;189:371–7. doi: 10.2214/AJR.07.2065. http://dx.doi.org/10.2214/AJR.07.2065. [DOI] [PubMed] [Google Scholar]