Abstract
Objective
To examine the association between family meals and disordered eating behaviors within a diverse sample of adolescents and further investigate whether family-level variables moderate this association.
Method
Data from adolescents (EAT 2010: Eating and Activity in Teens) and their parents (Project F-EAT: Families and Eating and Activity among Teens) were collected in 2009–2010. Surveys were completed by 2,382 middle and high school students (53.2% girls, mean age = 14.4 years) from Minneapolis/St. Paul, MN, public schools. Parents/guardians (n = 2,792) completed surveys by mail or phone.
Results
Greater frequency of family meals was associated with decreased odds of engaging in unhealthy weight control behaviors in boys, and dieting, unhealthy and extreme weight control behaviors in girls. Results indicate that the protective effects of family meals are, in general, robust to family-level variables; 64 interactions were examined and only seven were statistically significant. For example, among girls, the protective nature of family meals against dieting and unhealthy weight control behaviors was diminished if they also reported family weight-related teasing (both p < .01).
Discussion
The results confirmed previous research indicating that participation in family meals is protective against disordered eating for youth, particularly girls. However, results suggest that in some cases, the protection offered by family meals may be modified by family-level variables.
Introduction
Disordered eating behaviors, such as self-induced vomiting, laxative use, and binge eating, are highly prevalent in youth1–3 and predictive of adverse physical and psychosocial outcomes.4–6 Thus, there is a need to identify potentially modifiable factors that contribute to the development of disordered eating in adolescents. The protective role of family meals against disordered eating behaviors among youth has been suggested by population-based cross-sectional,7–10 retrospective11,12 and prospective longitudinal studies,13,14 and qualitative investigations.15,16 However, it remains unclear whether the protective effect of family meals is the same for families with different family-level characteristics. For example, in homes in which family members talk negatively about food and eating, or in homes where the atmosphere at the family meal is not positive, does the protection of family meals against disordered eating behaviors diminish?
Previous research examining the association between family meal frequency and disordered eating behaviors in adolescents have adjusted for family-level variables, including family connectedness and adolescent enjoyment of family meals.8,13,17 Results of these studies have shown that family meals continue to offer protection against endorsement of disordered eating behaviors above and beyond the protection provided by a positive family environment, suggesting that there is something uniquely protective about the family meal experience.8,13,17 However, to our knowledge, only one study to date has examined how this protection might be moderated by family-level variables.14 This study by Haines et al. found that the protection offered by family meals remained, even when adolescents perceived their thinness to be of importance to their parents, weight-based teasing was normative in the home environment, and maternal dieting behaviors were reported.
The goal of the current study is to expand upon the extant research on family meals, by exploring a range of family-level variables that might moderate the association between family meal frequency and disordered eating behaviors. Research has demonstrated that “negative mealtime experiences,” including controlling food-related parenting practices and a negative atmosphere at family meals, and “negative familial interactions,” such as poor family functioning, high levels of weight and body talk, poor communication, and frequent weight teasing, are associated with disordered eating behaviors among youth.18–25 Understanding the role that this broad range of variables might play in the association between family meal frequency and adolescent use of disordered eating behaviors has important implications for physicians and other healthcare providers working with families of adolescents. On one hand, if the protective nature of family meals is robust to differences in family-level variables, frequent family meals can be recommended to all families without hesitation. On the other hand, if the protective nature of family meals is diminished or reversed in the presence of negative family-level variables, healthcare providers should make recommendations to improve the family meal environment, or suggest families consider decreasing the frequency of family meals, at least until there are improvements in the harmful family-level variables.
The current study aims to answer the following research questions in a diverse population-based sample of adolescents: (a) Is family meal frequency associated with use of disordered eating behaviors? and (b) Do familial factors, including parent feeding practices, atmosphere at family meals, family functioning, parent-led conversations about weight, weight and body talk in the home, or family weight-related teasing, moderate the association between family meal frequency and use of disordered eating behaviors? (see Fig. 1 for graphic depiction of research questions.) Based on existing evidence from cross-sectional, retrospective, and prospective studies,7,12–14,26 it was hypothesized that greater frequency of family meals would be negatively associated with adolescent engagement in disordered eating behaviors, particularly in adolescent girls. Further, guided in part by prior work in this area,14 it was hypothesized that the presence of family factors noted in the literature to be associated with disordered eating, such as poor family functioning, frequent parent-led conversations about weight or body- and weight-related talk in the home, the occurrence of family weight-related teasing, high levels of controlling feeding practices, and a lack of adolescent enjoyment of family meals, would diminish, but not eliminate, the protection offered by family meals.
FIGURE 1.
Theoretical model depicting the potential effect modifiers explored in the relationship between family meal frequency and disordered eating behaviors.
Method
Study Design and Population
Data for this analysis were drawn from two coordinated, population-based studies: EAT 2010 (Eating and Activity in Teens), a study of 2,793 adolescents, and Project F-EAT (Families and Eating and Activity Among Teens), a study of the parents (n = 3,709) of adolescents in EAT 2010. Additional details on these studies can be found elsewhere.27,28 All study procedures were approved by the University of Minnesota’s Institutional Review Board Human Subjects Committee and participating school districts.
For EAT 2010, surveys and anthropometric measures were completed by adolescents from the Minneapolis/St Paul metropolitan area of Minnesota during the 2009–2010 academic year. For Project F-EAT, data were collected by surveying up to two parents or caregivers of the adolescents in EAT 2010; approximately 30% of adolescents provided contact information for one parent or guardian and 70% provided information for two parents or guardians. Parent surveys were collected by mail and telephone interviews. Additional details on adolescent and parent participants can be found in Table 1.
TABLE 1.
Characteristics of the EAT 2010 and Project F-EAT samples
| Adolescents (EAT 2010)
|
Parent/Caregiver (Project F-EAT)
|
|||
|---|---|---|---|---|
| Total (N) | 2793 | 2382 | ||
| Age (Mean, SD) | 14.45 | 1.98 | 41.45 | 7.94 |
| Gender (N, %) | ||||
| Male | 1307 | 46.8 | 208 | 8.74 |
| Female | 1486 | 53.3 | 2173 | 91.3 |
| Race (N, %) | ||||
| White | 525 | 18.8 | 687 | 28.8 |
| African American | 808 | 28.9 | 662 | 27.8 |
| Hispanic | 472 | 16.9 | 394 | 16.5 |
| Asian American | 555 | 19.9 | 464 | 19.5 |
| Native American | 102 | 3.7 | 9 | 0.38 |
| Mixed race/other/Missing | 331 | 11.9 | 166 | 6.97 |
| Socioeconomic statusa (N, %) | ||||
| Low | 1072 | 38.9 | 536 | 22.8 |
| Mid-low | 595 | 22.1 | 517 | 21.9 |
| Middle | 471 | 17.5 | 668 | 28.4 |
| Mid-high | 347 | 12.9 | 415 | 17.6 |
| High | 203 | 7.6 | 220 | 9.34 |
| Weight statusb (N,%) | ||||
| Normal | 1079 | 38.6 | 697 | 31.1 |
| Overweight | 1101 | 39.5 | 785 | 35.1 |
| Obese | 613 | 21.9 | 735 | 32.8 |
Socioeconomic status (SES): Separate measures of SES were included in both the EAT 2010 and the Project F-EAT surveys. Details on how SES was assessed within each survey can be found in the measures section. Furthermore, details on how SES was included in each of the models presented can be found in the Statistical Analysis section.
Normal weight = 5th percentile to less than the 85th percentile; Overweight= 85th to less than the 95th percentile; Obese = equal to or greater than 95th percentile.
The sample includes EAT 2010 participants who had at least one parent with whom they lived at least 50% of the time respond to the Project F-EAT questionnaire. Although data from up to two parents were collected in Project F-EAT, only data from one parent were included in the current study to ensure independence of data. In selecting one parent for inclusion, preference was given to parents who reported living with the adolescent most of the time; when youth lived equally with both parents, mothers were selected for inclusion because research indicates that women are more often in charge of the family meal environment.29 The analytic sample consisted of 2,793 adolescents, 2,382 of whom had parental data available.
Survey Development and Measures
Both the EAT 2010 student survey and the Project FEAT parent survey underwent extensive pilot and test–retest reliability testing to ensure questions were appropriate for the intended audience. An initial draft of the EAT 2010 survey was pilot tested within a sample of 56 adolescents from diverse backgrounds to examine their understandability and relevance. This draft survey was additionally reviewed by a team of experts in the domains of nutrition, physical activity, adolescent development, body image, family relations, and urban design. After revisions based on initial pretesting and feedback from the expert reviewers, the survey was further pilot tested with a different sample of 129 middle school and high school students to examine the test–retest reliability of measures over a 1-week period and the internal consistency of scales. An initial draft of the Project F-EAT parent survey was first reviewed by content area experts to ensure that key constructs relevant to adolescent weight-related behaviors and outcomes were included. Furthermore, survey appropriateness for the major cultural groups participating in the study (i.e., Native American, Hmong, Latino, Somali, and African American groups) was addressed by having bi-cultural staff from the Wilder Research Foundation review the survey and provide feedback on the appropriateness and relevance of the survey items. Next, three focus groups were conducted to pretest an initial draft of the Project F-EAT survey. Feedback from 28 socioeconomically and ethnically/racially diverse parent participants was used to reword or eliminate problematic survey items and expand on topic areas of perceived importance (e.g., family meals, conversations about weight at home). An additional sample of 102 parents completed the Project F-EAT survey twice in a 2-week time period to examine test–retest reliability of survey questions. Finally, scale psychometric properties were examined within the full Project F-EAT sample. Data for the outcome variables (i.e., disordered eating behaviors) and the predictor variable (family meal frequency) were drawn from the EAT 2010 surveys completed by adolescent participants. Moderating variables were drawn from both the adolescent survey and Project F-EAT parent survey in an attempt to assess the broadest range of potential effect modifiers available within the datasets.
Outcome Variable: Disordered Eating
Adolescents reported their dieting frequency by responding to the question, “How often have you gone on a diet during the last year? By ‘diet’ we mean changing the way you eat so you can lose weight.” Response options included: never, 1–4 times, 5–10 times, more than 10 times, and I am always dieting. As in previous analyses, responses were dichotomized into nondieters (responded never) and dieters (other responses) (Test–retest agreement [nondieter versus dieter] = 82%).30
Adolescents were asked about their use of unhealthy and extreme weight control behaviors with the question: “Have you done any of the following things in order to lose weight or keep from gaining weight during the past year?” (Yes/No for each method). Behaviors categorized as unhealthy weight control behaviors included fasted, ate very little food, used a food substitute (powder or a special drink), skipped meals, and smoked cigarettes. Behaviors categorized as extreme weight control behaviors included took diet pills, made myself vomit, used laxatives, and used diuretics. Responses were used to create two dichotomous indicators of having done any one or more of the unhealthy weight control behaviors (test–retest agreement = 85%) and any one or more of the extreme weight control behaviors (test–retest agreement = 96%).9
To assess binge eating, adolescents responded to two questions31: “In the past year, have you ever eaten so much food in a short period of time that you would be embarrassed if others saw you (binge eating)?” (Yes/No). If yes, they were asked: “During the times when you ate this way, did you feel you couldn’t stop eating or control what or how much you were eating?” (Yes/No) (test–retest agreement = 90% [first question] and 75% [second question]). Participants needed to respond affirmatively to both questions to be coded as binge eating.
Predictor Variable: Family Meal Frequency
To assess family meal frequency, adolescents were asked, “During the past week, how many times did all, or most, of your family living in your household eat a meal together?”32 Response options included: never, 1–2 times, 3–4 times, 5–6 times, 7 times, and more than 7 times (Test–retest r = .63). For the current analysis, family meal frequency was treated as a continuous variable.
Moderating Variables
Adolescent Reported Variables
To assess family functioning, adolescents were asked to indicate agreement with the following statements: “Family members are accepted for who they are”; “Making decisions is a problem for the family”; “We don’t get along well together”; “We can express feelings to each other”; and “Planning family activities is difficult because we misunderstand each other”.33,34 Response options included strongly disagree, somewhat disagree, somewhat agree, and strongly agree. Responses were assigned values from 1 to 4, with reverse coding used for statements worded in the negative form, before values were added. Higher scores represent higher family functioning (Cronbach’s α = 0.70).
Weight talk in the home was assessed by asking adolescents to indicate agreement with two statements about each of their parents: “My mother/father talks about her/his weight” and “My mother/father makes comments about other people’s weight.” Response options ranged on a 4-point scale from not at all to very much. Responses to these four questions were averaged to create a weight talk in the home variable (Cronbach’s α = 0.75).
Family weight-related teasing was assessed by asking adolescents the question: “How often do family members make comments to you about your weight or your eating that make you feel bad?” Response options included: never, less than once a year, a few times a year, a few times a month, and a few times a week (test–retest r =.67).
Adolescent enjoyment of family meals was assessed with one item, “I enjoy eating meals with my family”. Response options ranged on a 4-point scale from strongly disagree to strongly agree (test–retest r =.68).
Parent Reported Variables
Parent-led conversations about weight were assessed using four items modified from the Parental Energy Index.25 Mothers and fathers were asked, “How often in the past year. . .”: (1) Have you had a conversation with your child about his/her weight or size?; (2) Have you mentioned to your child that he/she weighs too much?; (3) Have you mentioned to your child that he/she should eat differently to lose weight or keep from gaining weight?; and (4) Have you mentioned to your child that he/she should exercise to lose weight or keep from gaining weight? Participants responded to each item using a 5-point scale ranging from 1 (never or rarely) to 5 (almost every day) (test–retest r = .73, Cronbach’s α = 0.89).
Food restriction was measured using six items (of eight) from the Child Feeding Questionnaire (CFQ) Restriction Subscale, which was designed to measure a parent’s attempt to control a child’s eating by restricting access to palatable foods.35 Pressure-to-eat was assessed using the full CFQ Pressure-to-Eat Subscale, which was designed to measure the degree to which the parent encourages their child to eat more food. Overall scores for each scale were created by averaging responses to items from that scale. [Scale Range: 1 (low control) to 4 (high control); Restriction: r = .72, α = 0.86; Pressure-to-eat: r =.73, α = 0.70].
Covariates
Several demographic and personal characteristics of adolescents were considered for statistical analysis. Age, race/ethnicity, and socioeconomic status (SES) were based on adolescent self-report. SES was based primarily on parental education level (as reported by adolescent), defined as the higher level of educational attainment of either parent (test–retest r = .90). An algorithm was developed that also took into account family eligibility for public assistance, eligibility for free or reduced-cost school meals, and parent employment status.36,37 Body mass index (BMI) was calculated using anthropometric data assessed by trained staff following standardized procedures.38
Statistical Analysis
To examine associations between family meal frequency and disordered eating behaviors (dieting, unhealthy and extreme weight control behaviors, and binge eating), separate logistic regressions for each disordered eating behavior outcome were estimated with family meal frequency as the primary predictor controlling for adolescent age, race, SES, and BMI. The odds ratio (OR) and 95% confidence interval (CI) for family meal frequency represent the multiplicative change in odds (i.e., ORs less than 1 indicate protective effects) of exhibiting the disordered eating behavior for every one meal increase in family meals per week.
To determine whether there were differential effects of family meals on disordered eating behavior depending on the quality of familial interactions and mealtime atmosphere, a series of interaction models were performed. In total, we considered eight potential effect modifiers, including family functioning; parent-led conversation about weight; parent dieting behaviors; family weight-related teasing; weight and body talk in the home; food restriction; pressure-to-eat; and adolescent enjoyment of family meals. (see Fig. 1 for visual depiction of the research question and list of eight effect modifiers examined). For each of these eight moderators, a separate logistic regression model was fit with family meal frequency, the moderator, and the cross-product between the two controlling for adolescent age, race, SES, and BMI. BMI was first explored as a potential effect measure modifier; however, it was not found to modify any of the relationships, therefore BMI was only included as a covariate. ORs and CIs are presented by using Paneled Forest Plots for each of the models run. For each model, we present the OR of the family meal frequency at the minimum and the maximum value of the moderator. For example, low pressure-to-eat corresponds to a value of 1 and high pressure-to-eat corresponds to a value of 4. Note, each of the moderators was measured on a continuous scale and was included in the regression as a continuous predictor, but for illustration of the interaction effect, ORs are presented at fixed high (maximum) vs. low (minimum) values of the moderator (see Appendix 1). CIs for the ORs appropriately account for the value at which the moderator is fixed. Reported p values were not adjusted for multiple testing. Appendix 1 includes information on the frequency of participants reporting the minimum and maximum levels of each potential effect measure modifier explored.
Appendix 1.
Frequency of participants reporting the minimum and maximum levels of potential effect measure modifiers
| Frequency at Minimum Level “Low” N (%) | Frequency at Maximum Level “High” N (%) | |
|---|---|---|
| Enjoyment of family meals [Range = 1–4] | 214 (8.0) | 1002 (36.0) |
| Family functioning [Range = 1–4] | 36 (1.0) | 483 (17.0) |
| Weight talk in the home [Range = 1–4] | 813 (30.0) | 19 (1.0) |
| Family weight-related teasing [Range = 1–5) | 1608 (59.0) | 147 (5.0) |
| Parent-led conversations about weight [Range = 1–5] | 708 (30.0) | 50 (2.0) |
| Parental food restriction [Range = 1–4] | 372 (16.0) | 69 (3.0) |
| Parental pressure-to-eat [Range = 1–4] | 259 (11.0) | 151 (6.0) |
| Parental dieting behaviors [Range = 1–5] | 1091 (46.0) | 176 (7.0) |
For the first research question (associations between family meal frequency and adolescent disordered eating behaviors), the analytic sample included all 2,793 adolescents who responded to the questions on the EAT 2010 survey. For the second research question (exploration of potential moderators in the relationship between family meal frequency and adolescent disordered eating behaviors), the analytic sample included either all 2,793 adolescents, if the moderating variable of interest was an item reported by the adolescent, or included only the 2,382 adolescents with available parent data if the moderating variable of interest was reported by the parents. Adolescents who had parents participate (n = 2,382) did not differ by weight status or age from those who did not have parents participate (n = 411); however, adolescents who had parents participate were more likely to be white and of mid-high to high SES, as compared with those who did not. All analyses were stratified by gender of the adolescent and performed in SAS 9.2 (SAS, Chicago, IL).
Results
Prevalence of Disordered Eating Behaviors Among Adolescents
Among boys, 31% (n = 406) reported dieting, 38% (n = 495) reported engaging in unhealthy weight control behaviors, 4% (n = 51) reported engaging in extreme weight control behaviors, and 6% (n = 81) reported engaging in binge eating with loss of control. Among girls, 46% (n = 680) reported dieting, 50% (n = 743) reported engaging in unhealthy weight control behaviors, 7% (n = 100) reported engaging in extreme weight control behaviors, and 10% (n = 141) reported engaging in binge eating with loss of control.
Family Meals and Disordered Eating Behaviors
Greater frequency of family meals was associated with significantly lower levels of dieting (OR = 0.94, CI = 0.90–0.98), unhealthy weight control behaviors (OR = 0.93, CI = 0.89–0.97), and extreme weight control behaviors in adolescent girls (OR = 0.88, CI = 0.80–0.95), but only with unhealthy weight control behaviors in adolescent boys (OR = 0.94, CI = 0.90–0.98) (Table 2). Statistically significant associations were not found between family meals and binge eating.
TABLE 2.
Odds ratios of adolescents engaging in disordered eating behaviors associated with a one meal increase in family meals per weeka
| Boys (n = 1307)
|
Girls (n = 1,486)
|
|||
|---|---|---|---|---|
| Outcome | OR | 95% CI | OR | 95% CI |
| Any dieting | 1.00 | (0.95–1.06) | 0.94 | (0.90–0.98) |
| Unhealthy weight control behaviors | 0.94 | (0.89–0.98) | 0.93 | (0.89–0.97) |
| Extreme weight control behaviors | 0.94 | (0.84–1.06) | 0.88 | (0.80–0.95) |
| Binge eating | 0.92 | (0.83–1.01) | 0.94 | (0.87–1.01) |
OR – Odds ratio, CI – Confidence interval. Bold indicates OR significant at p < .05.
Models adjusted for adolescent age, race, socioeconomic status, and BMI.
Effect Modification by Family Environment Variables
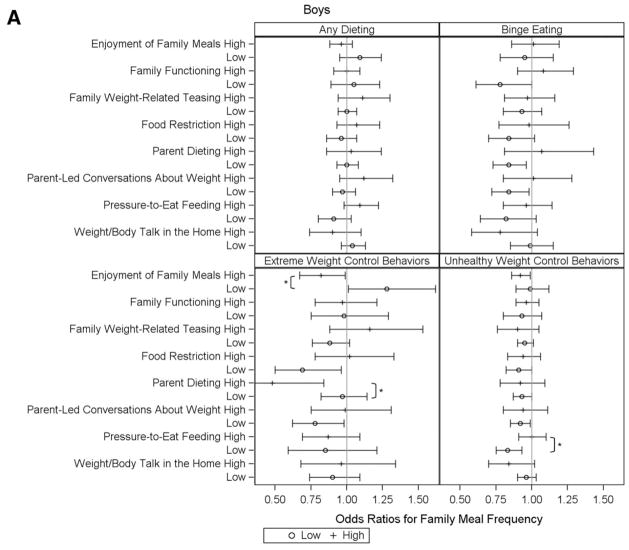
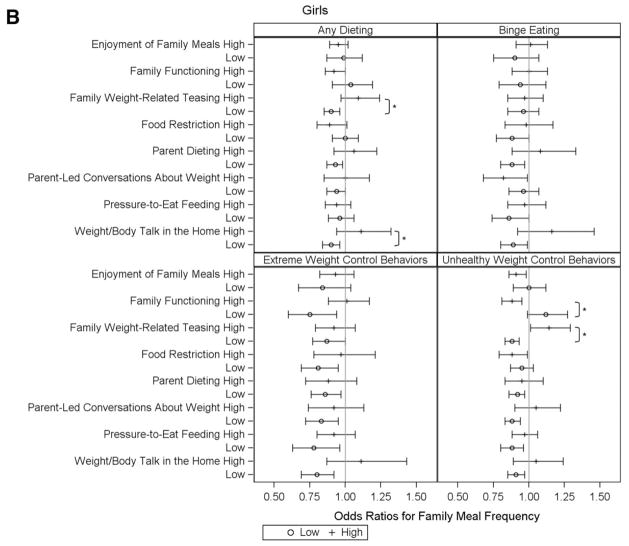
Of the 64 interactions examined (8 family level effect modifiers × 4 outcome variables for boys and girls), only seven were found to be statistically significant at p ≤ .05. This finding suggests that the protective effects of adolescents engaging in family meals against use of disordered eating behaviors were generally robust to the bulk of familial interaction and mealtime atmosphere variables examined in the current study. ORs and 95% CIs for each of the eight potential effect modifiers explored are displayed in Figures 2a and 2b at the low (minimum) and high (maximum) values of each modifier. ORs greater than 1 indicate an increased risk for adolescent engagement in the disordered eating behavior of interest, whereas ORs less than 1 indicate that the effect modifier was protective against the use of the disordered eating behavior of interest. Statistically significant effect modifiers (p ≤ .05) are noted in the figure with an asterisk (*). Food restriction, parent-led conversations about weight, and pressure-to-eat were reported by parents, and thus analyses were limited to adolescents with parent data (n = 2,382); all other analyses were conducted with the full adolescent sample (n = 2,793).
FIGURE 2.
Effect modifiers (high versus low) of the relationship between family meal frequency and adolescent disordered eating behaviors, odds ratios and 95% confidence intervals.
Notes: Odds Ratios and 95% confidence intervals for each of the 8 potential moderators of family meal frequency are displayed at the low (minimum) and high (maximum) values of each moderator. ORs greater than 1 indicate an increased risk for adolescent engagement in disordered eating behaviors. Statistically significant effect modifiers (p≤0.05) are noted with an asterisk (*). Food restriction, parent-led conversations about weight, and pressure-to-eat were reported by parents, and thus analyses were limited to adolescents with parent data (n=2382), all other analyses were conducted with the full adolescent sample (n=2,793).
Among boys (Fig. 2a), there was evidence of effect modification by three variables of 32 models examined: parental pressure-to-eat, atmosphere at family meals, and parental dieting. Parental use of pressure-to-eat feeding practices modified the association between family meals and use of unhealthy weight control behaviors (p = .05). The odds of engaging in unhealthy weight control behaviors decreased with greater family meal frequency among boys whose parents reported a low level of pressure-to-eat feeding practices; specifically, the odds of engaging in unhealthy weight control behaviors decreased by 0.83 with each additional meal eaten together with family in the past week (p < .01). In contrast, family meals offered no protection against unhealthy weight control behaviors among boys whose parents report using a high level of pressure-to-eat feeding practices (OR: 1.00, CI = 0.91–1.10). In addition, extreme weight control behaviors decreased with greater frequency of family meals among boys who reported enjoying their family meal experience; the odds of using extreme weight control behaviors decreased by 0.82 with each additional family meal eaten together in the past week (CI: 0.67–0.99). On the other hand, when boys reported a low level of enjoyment of family meals, boys who have frequent family meals are more likely to report engaging in extreme weight control behaviors (OR = 1.28, CI = 1.01–1.62). Finally, family meals were found to offer greater protection against the use of extreme weight control behaviors among boys whose parents engaged in frequent dieting (p < .01).
Among girls (Fig. 2b), evidence of statistically significant effect modification was found within four models (of 3 models examined). Family weight-related teasing modified associations between family meals and both dieting (p = .01) and unhealthy weight control behaviors (p < .01).For example, among girls, the odds of dieting decreased with greater family meal frequency in homes with low levels of family weight-related teasing (OR = 0.90, CI = 0.85–0.96). In contrast, the odds of dieting increased with greater frequency of family meals among girls who reported high levels of family weight-related teasing (OR = 1.09, CI = 0.97–1.24). In other words, family meals were protective against dieting for girls whose families engaged in no or low level weight-related teasing, but when weight teasing was present, exposure to family meals became a risk factor for engaging in dieting. There was also evidence of significant effect modification by overall family functioning among girls for the association between family meals and unhealthy weight control behaviors (p < .01); for girls whose families had poor overall functioning, frequent family meals were associated with greater odds of engaging in unhealthy weight control behaviors. Finally, frequent family meals were found to be a risk factor for engaging in dieting among girls exposed to high levels of weight talk in the home (p = .05).
Discussion
The current study explored the association between family meal frequency and use of disordered eating behaviors among adolescents and sought to understand how variables in the family environment, including family functioning, parent-led conversations about weight, weight and body talk in the home, family weight-related teasing, parent feeding practices, and atmosphere at family meals, might moderate this association. Overall, greater frequency of family meals was associated with lower prevalence of dieting, unhealthy weight control behaviors, and extreme weight control behaviors in adolescent girls, but only with lower levels of unhealthy weight control behaviors in adolescent boys. The protective nature of family meals was found to be, in general, robust to differences in family level variables, suggesting that engagement in regular family meals should be recommended for the majority of families with adolescents.
Although some of the overall effect sizes were small, the findings from our first research question are in agreement with those from previous cross-sectional7 and longitudinal13,14 studies that also found a significant inverse association between family meal frequency and disordered eating among adolescents, particularly adolescent girls. The authors have previously suggested several possible mechanisms by which family meals may decrease the risk for endorsement of disordered eating behaviors, including parental modeling of healthy eating patterns, increased opportunities for connecting with teens via conversations, and regular monitoring of a child’s eating behaviors and emotional health, allowing for early identification of problems.15,17,39
Only a limited number of familial interaction and mealtime atmosphere variables were found to significantly moderate the association between frequency of family meals and adolescent engagement in disordered eating behaviors. The general trend of null findings found in the current manuscript aligns with the work of Haines et al.14 who found that the protection offered by family meals remained, even when adolescents in their study perceived thinness to be of importance to their parents, weight-based teasing was normative in their home environment and maternal dieting behaviors were reported. Overall, results of this current study, in conjunction with the previous work by Haines et al., suggest that for the most part, family meals are protective against the endorsement of disordered eating behaviors among adolescents. Furthermore, given the large number of interactions examined within the current study, it is important to consider that even the few significant results found may be, in fact, spurious associations.
However, it is worthwhile to reflect on the potential importance of each of the significant effect modifiers, particularly with regard to how these findings might impact clinical recommendations for families. For example, the associations between family meals and unhealthy and extreme weight control behaviors among boys were modified by both adolescent enjoyment of family meals and parental report of pressure-to-eat. These findings suggest that boys may be influenced by mealtime atmosphere; when young men enjoy eating meals with their family and when parental control at meals is low, exposure to frequent family meals protects against the use of disordered eating behaviors. However, in circumstances when young men perceive the atmosphere at meals to be less enjoyable or they are exposed to more controlling (high pressure-to-eat) parenting practices, the protective nature of family meals against disordered eating behaviors diminishes. Given that research has shown boys are more likely than girls to be exposed to pressure-to-eat,40 the moderating effect of this variable among boys might provide some explanation for why the strength of the association between family meal frequency and disordered eating behaviors has often been weaker among boys.
Among girls, the association between family meals and disordered eating behaviors was found to be moderated by family level weight and body talk, weight-based teasing, and overall family functioning. This suggests that for girls, the broader family environment may play a role in the level of protection that family meals can offer. For example, it might be that for girls who have experienced poor family functioning or have been exposed to family weight teasing or high levels of weight talk, sharing a meal with the family does not offer the same safety or protection against the use of disordered eating, as compared with girls living in a family environment that is characterized by positive family functioning and free of weight-based conversations. Future research should aim to understand how often weight-based teasing or weight/body talk is occurring at family meals versus other times and how the timing of this negative weight-based talk might impact the association between family meal frequency and disordered eating behaviors.
Strengths and limitations should be considered in interpreting these study findings. The large, diverse, population-based sample used in the current study allows for generalizability of the study findings to nonclinical samples. Furthermore, inclusion of both boys and girls in the sample allowed for exploration of how adolescent gender might influence the impact of certain family-level effect modifiers. Finally, the large number of measures assessing the family and mealtime environment allowed for the exploration of how these variables might moderate associations between family meals and disordered eating in adolescents. However, the cross-sectional study design is a limitation of the current study as the temporal ordering of changes over time in family meal frequency and disordered eating behaviors remains unclear. For example, as previously supported by longitudinal research, it could be that eating regular meals with family members protects adolescents from engaging in disordered eating behaviors.7,13,17,41,42 On the other hand, it could be that adolescents who eat family meals less frequently may have more eating problems and, therefore, avoid engaging in meals with their family. Another study limitation is that our survey did not distinguish whether certain family-level variables (weight-based teasing, pressure-to-eat) occurred during family meal time. Finally, the use of primarily unvalidated survey instruments, for both adolescents and parents, should be taken into account when interpreting study results.
Conclusion
Findings from this study in a racially/ethnically and socioeconomically diverse, population-based sample suggest that adolescents, particularly girls, who eat more frequent family meals are less likely to engage in disordered eating behaviors. Future research efforts in this area should focus on building a better understanding of the underlying mechanisms by which eating meals with one’s family protects against the use of disordered eating behaviors. In addition, researchers should continue to explore the possibility that the protective nature of family meals may be modified by familial interactions and mealtime atmosphere. Based on the results of this study, in conjunction with findings from other previously conducted research, dietetic practitioners, physicians, and other healthcare providers working with families of adolescents should continue to engage parents in discussions about the importance of making frequent family meals a priority. Parents should be made aware that participating in regular family meals offers some protection for their teen against engaging in disordered eating behaviors. Finally, in addition to asking parents of teens about the frequency of family meals during well-child visits, healthcare providers should consider providing anticipatory guidance for parents on how to create familial interactions and a mealtime atmosphere conducive to the development of healthy weight-related behaviors in adolescents.
Acknowledgments
Supported by R01HL084064 and RO1HL093247-02 (PI: Neumark-Sztainer) from the National Heart, Lung, and Blood Institute. Katie Loth’s time was funded by Grant T32 MH082761-01 from the National Institute of Mental Health.
References
- 1.Graber JA, Brooks-Gunn J, Paikoff RL, Warren MP. Prediction of eating problems: An 8-year study of adolescent girls. Dev Psychol. 1994;30:823. [Google Scholar]
- 2.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Youth risk behavior surveillance—United States, 2011. MMWR Surveill Summ. 2012;61:1–162. [PubMed] [Google Scholar]
- 3.Stein D, Meged S, Bar-Hanin T, Blank S, Elizur A, Weizman A. Partial eating disorders in a community sample of female adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36:1116–1123. doi: 10.1097/00004583-199708000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Field AE, Aneja P, Austin SB, Shrier LA, de Moor C, Gordon-Larsen P. Race and gender differences in the association of dieting and gains in BMI among young adults. Obesity. 2007;15:456–464. doi: 10.1038/oby.2007.560. [DOI] [PubMed] [Google Scholar]
- 5.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, et al. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics. 2006;117:1203. doi: 10.1542/peds.2005-1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol. 1999;67:967. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- 7.Fulkerson JA, Story M, Mellin A, Leffert N, Neumark-Sztainer D, French SA. Family dinner meal frequency and adolescent development: Relationships with developmental assets and high-risk behaviors. J Adolesc Health. 2006;39:337–345. doi: 10.1016/j.jadohealth.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 8.Neumark-Sztainer D, Wall M, Story M, Fulkerson JA. Are family meal patterns associated with disordered eating behaviors among adolescents? J Adolesc Health. 2004;35:350–359. doi: 10.1016/j.jadohealth.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Neumark-Sztainer D, Patterson J, Mellin A, Ackard DM, Utter J, Story M, et al. Weight control practices and disordered eating behaviors among adolescent females and males with type 1 diabetes. Diabetes Care. 2002;25:1289–1296. doi: 10.2337/diacare.25.8.1289. [DOI] [PubMed] [Google Scholar]
- 10.Worobey J. Early family mealtime experiences and eating attitudes in normal weight, underweight and overweight females. Eating Weight Disorders: EWD. 2002;7:39–44. doi: 10.1007/BF03354428. [DOI] [PubMed] [Google Scholar]
- 11.Ackard DM, Neumark-Sztainer D, Story M, Perry C. Overeating among adolescents: Prevalence and associations with weight-related characteristics and psychological health. Pediatrics. 2003;111:67–74. doi: 10.1542/peds.111.1.67. [DOI] [PubMed] [Google Scholar]
- 12.Miller DAF, McCluskey-Fawcett K, Irving LM. Correlates of bulimia nervosa: Early family mealtime experiences. Adolescence. 1993;28:621–635. [PubMed] [Google Scholar]
- 13.Neumark-Sztainer D, Eisenberg ME, Fulkerson JA, Story M, Larson NI. Family meals and disordered eating in adolescents: Longitudinal findings from project EAT. Arch Pediatr Adolesc Med. 2008;162:17–22. doi: 10.1001/archpediatrics.2007.9. [DOI] [PubMed] [Google Scholar]
- 14.Haines J, Gillman MW, Rifas-Shiman S, Field AE, Austin SB. Family dinner and disordered eating behaviors in a large cohort of adolescents. Eat Disord. 2010;18:10–24. doi: 10.1080/10640260903439516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loth KA, Neumark-Sztainer D, Croll JK. Informing family approaches to eating disorder prevention: Perspectives of those who have been there. Int J Eat Disord. 2009;42:146–152. doi: 10.1002/eat.20586. [DOI] [PubMed] [Google Scholar]
- 16.Mellin AE, Neumark-Sztainer D, Patterson JM. Parenting adolescent girls with type 1 diabetes: Parents’ perspectives. J Pediatr Psychol. 2004;29:221–230. doi: 10.1093/jpepsy/jsh023. [DOI] [PubMed] [Google Scholar]
- 17.Neumark-Sztainer D, Larson NI, Fulkerson JA, Eisenberg ME, Story M. Family meals and adolescents: What have we learned from Project EAT (Eating Among Teens)? Public Health Nutr. 2010;13:1113–1121. doi: 10.1017/S1368980010000169. [DOI] [PubMed] [Google Scholar]
- 18.Dare C, Grange DL, Eisler I, Rutherford J. Redefining the psychosomatic family: Family process of 26 eating disorder families. Int J Eat Disord. 1994;16:211–226. doi: 10.1002/1098-108x(199411)16:3<211::aid-eat2260160302>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 19.Kog E, Vandereycken W. Family interaction in eating disorder patients and normal controls. Int J Eat Disord. 1989;8:11–23. [Google Scholar]
- 20.Leon GR, Fulkerson JA, Perry CL, Dube A. Family influences, school behaviors, and risk for the later development of an eating disorder. J Youth Adolesc. 1994;23:499–515. [Google Scholar]
- 21.Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: Correlations with weight status and disordered eating behaviors. Int J Obes Relat Metab Disord. 2002;26:123–131. doi: 10.1038/sj.ijo.0801853. [DOI] [PubMed] [Google Scholar]
- 22.Ordman AM, Kirschenbaum DS. Bulimia: Assessment of eating, psychological adjustment, and familial characteristics. Int J Eat Disord. 1986;5:865–878. [Google Scholar]
- 23.Strober M, Humphrey LL. Familial contributions to the etiology and course of anorexia nervosa and bulimia. J Consult Clin Psychol. 1987;55:654. doi: 10.1037//0022-006x.55.5.654. [DOI] [PubMed] [Google Scholar]
- 24.Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM. Family weight talk and dieting: How much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health. 2010;47:270–276. doi: 10.1016/j.jadohealth.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berge JM, MacLehose R, Loth KA, Eisenberg M, Bucchianeri MM, Neumark-Sztainer D. Parent Conversations About Healthful Eating and Weight. JAMA Pediatr. 2013;167:746–753. doi: 10.1001/jamapediatrics.2013.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ackard DM, Neumark-Sztainer D. Family mealtime while growing up: Associations with symptoms of bulimia nervosa. Eat Disord. 2001;9:239–249. doi: 10.1080/10640260127551. [DOI] [PubMed] [Google Scholar]
- 27.Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Eat this, not that! Parental demographic correlates of food-related parenting practices. Appetite. 2013;60:140–147. doi: 10.1016/j.appet.2012.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Neumark-Sztainer D, MacLehose R, Loth K, Fulkerson JA, Eisenberg ME, Berge J. What’s for dinner? Types of food served at family dinner differ across parent and family characteristics. Public Health Nutr. 2012;17:145–155. doi: 10.1017/S1368980012004594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McIntosh WA, Kubena KS, Tolle G, Dean WR, Jan J, Anding J. Mothers and meals. The effects of mothers’ meal planning and shopping motivations on children’s participation in family meals. Appetite. 2010;55:623–628. doi: 10.1016/j.appet.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 30.Neumark-Sztainer D, Wall MM, Story M, Perry CL. Correlates of unhealthy weight-control behaviors among adolescents: Implications for prevention programs. Health Psychol. 2003;22:88. doi: 10.1037//0278-6133.22.1.88. [DOI] [PubMed] [Google Scholar]
- 31.Yanovski SZ. Binge eating disorder: Current knowledge and future directions. Obes Res. 1993;1:306. doi: 10.1002/j.1550-8528.1993.tb00626.x. [DOI] [PubMed] [Google Scholar]
- 32.Berge JM, MacLehose RF, Loth KA, Eisenberg ME, Fulkerson JA, Neumark-Sztainer D. Family meals. Associations with weight and eating behaviors among mothers and fathers. Appetite. 2012;58:1128–1135. doi: 10.1016/j.appet.2012.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device*. J Marital Fam Ther. 1983;9:171–180. [Google Scholar]
- 34.Miller IW. The McMaster Family Assessment Device: Reliabilty and validity. J Marital Fam Ther. 1985;11:345–356. [Google Scholar]
- 35.Kaur H, Li C, Nazir N, Choi WS, Resnicow K, Birch LL, et al. Confirmatory factor analysis of the child-feeding questionnaire among parents of adolescents. Appetite. 2006;47:36–45. doi: 10.1016/j.appet.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 36.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and Regression Trees Belmont. CA: Wadsworth International Group; 1984. [Google Scholar]
- 37.Neumark-Sztainer D, Hannan PJ, Story M, Croll J, Perry C. Family meal patterns: Associations with sociodemographic characteristics and improved dietary intake among adolescents. J Am Diet Assoc. 2003;103:317–322. doi: 10.1053/jada.2003.50048. [DOI] [PubMed] [Google Scholar]
- 38.Gibson RS. Principles of Nutritional Assessment. Oxford University Press; US: 2005. p. 930. [Google Scholar]
- 39.Neumark-Sztainer D. Preventing obesity and eating disorders in adolescents: What can health care providers do? J Adolesc Health. 2009;44:206–213. doi: 10.1016/j.jadohealth.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 40.Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Food-related parenting practices and adolescent weight status: A population-based study. Pediatrics. 2013;131:e1443–e1450. doi: 10.1542/peds.2012-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Videon TM, Manning CK. Influences on adolescent eating patterns: The importance of family meals. J Adolesc Health. 2003;32:365–373. doi: 10.1016/s1054-139x(02)00711-5. [DOI] [PubMed] [Google Scholar]
- 42.Rollins BY, Belue RZ, Francis LA. The beneficial effect of family meals on obesity differs by race, sex, and household education: The national survey of children’s health, 2003–2004. J Am Diet Assoc. 2010;110:1335–1339. doi: 10.1016/j.jada.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]