Abstract
Background
The aim of this study was to describe the experience of pediatric and young adult hemodialysis (HD) patients from a global cohort.
Methods
The Pediatric Investigation and Close Collaborative Consortium for Ongoing Life Outcomes for MONitoring Dialysis Outcomes (PICCOLO MONDO) study provided de-identified electronic information of 3244 patients, ages 0–30 years from 2000 to 2012 in four regions: Asia, Europe, North America and South America. The study sample was categorized into pediatric (≤18 years old) and young adult (19–30 years old) groups based on the age at dialysis initiation.
Results
For those with known end-stage renal disease etiology, glomerular disease was the most common diagnosis in children and young adults. Using Europe as a reference group, North America [odds ratio (OR) 2.69; CI 1.29, 5.63] and South America (OR 4.21; CI 2.32, 7.63) had the greatest mortality among young adults. North America also had higher rates of overweight, obesity, hypertension, cardiovascular disease, hospitalizations and secondary diabetes compared with all other regions. Initial catheter use was greater for North American (86.4% in pediatric patients and 75.2% in young adults) and South America (80.6% in pediatric patients and 75.9% in young adults). Catheter use at 1-year follow-up was most common in North American children (77.3%) and young adults (62.9%). Asia had the lowest rate of catheter use. For both age groups, dialysis adequacy (equilibrated Kt/V) ranged between 1.4 and 1.5. In Asia, patients in both age groups had significantly longer treatment times than in any other region.
Conclusions
The PICCOLO MONDO study has provided unique baseline and 1-year follow-up information on children and young adults receiving HD around the globe. This cohort has brought to light aspects of care in these age groups that warrant further investigation.
Keywords: adolescents, international, young adults
Introduction
Children, adolescents and young adults with end-stage renal disease (ESRD) constitute a group of patients with unique morbidities. Their disease etiology is heterogeneous and varies greatly by age, with congenital anomalies of the kidneys and urinary tract (CAKUT) affecting younger individuals and acquired conditions more prevalent in older patients [1, 2]. The incidence of ESRD in the pediatric age group differs by region of the world [1–4], and in some countries, an accurate estimate of the number of patients with this condition is not available.
Investigation of comorbidities of pediatric hemodialysis (HD) patients may underrepresent the 16- to 18-year-old patients, as a number of adolescents are dialyzed in adult-focused units [5]. In the USA, two-thirds of pediatric HD patients are treated at facilities with fewer than 5% of patients younger than 19 years of age. Furthermore, young adult patients on HD included in adult studies do not share the comorbidities affecting the majority of adult ESRD patients [6].
We describe the findings of the global Pediatric Investigation and Close Collaborative Consortium for Ongoing Life Outcomes for MONitoring Dialysis Outcomes (PICCOLO MONDO) study. The PICCOLO MONDO is a subset of the volunteer global MONDO consortium that reports data on patients maintained on HD [7, 8]. The PICCOLO MONDO study characterized the incident and 1-year longitudinal outcomes of 0- to 30-year-old patients on HD.
Materials and methods
The ‘MONDO Consortium’ consists of dialysis facilities from the Renal Research Institute in the USA; Fresenius Medical Care in Europe, Asia Pacific and Latin America; KfH in Germany; Imperial College in London, UK; Pontifical University of Parana in Curitiba, Brazil; and Maastricht University Medical Center in The Netherlands [7, 8]. The MONDO database includes information on all patients treated in their respective provider network with the data directly extracted from the electronic health record systems. Every individual provider has its own procedures for data cleaning before data end up in the respective provider system. The MONDO database contains only de-identified data. Research conducted by MONDO complies with the Declaration of Helsinki. MONDO partner organizations are responsible for the primary collection and safeguarding of patient data in accordance with all applicable local data protection laws and privacy protection regulations. They also ensure full compliance with laws and regulations regarding the secondary use of data in the context of MONDO. For data collection and analysis, local ethical, compliance and legal standards are followed [7, 8]. This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
The PICCOLO MONDO cohort is a subset of MONDO and includes patients from 0 to 30 years of age, from 510 units, and in-center HD treatment data from 2000 to 2012. The study sample was categorized into pediatric (≤18 years old) and young adult (19–30 years old) groups based on the age at dialysis initiation. We divided the regions of the world into Asia (Australia, Hong Kong, South Korea, Malaysia, Philippines, Singapore, Turkey, Taiwan, Thailand), Europe (Bosnia, Czech Republic, France, Hungary, Ireland, Italy, Poland, Portugal, Romania, Russia, Serbia, Slovakia, Slovenia, Spain, UK), North America (USA) and South America (Argentina, Brazil, Chile, Colombia, Venezuela). Incident patients and their 1-year outcomes were analyzed by age group and region.
The cause of ESRD was identified based on the International Classification of Diseases (ICD)-9 (North America) and ICD-10 (Europe and Asia) codes. We converted ICD-10 categories to be compatible with the ICD-9 codes. The data provided by dialysis units in South America did not include cause of ESRD, whereas the Asian data were organized into several categories of ESRD etiology.
Given our large sample and for analysis purposes, we were able to expand the diagnosis groups published by the pediatric CKiD Study [9] into five groups as: glomerular, non-glomerular (including CAKUT, and cystic and hereditary conditions), diabetes mellitus (DM), ‘other’ (e.g. tubulo-interstitial nephritis, tubular necrosis) and ‘unknown’. Comorbidities examined such as congestive heart failure, hypertension, secondary diabetes and cardiovascular disease (CVD) excluding hypertension were identified by each facility report.
Blood pressure parameters included pre-dialysis systolic (preSBP) and pre-dialysis diastolic blood pressures (preDBP). For the pediatric group, we defined hypertension using the 97th percentile for children with an inputted height of the age-appropriate 50th percentile, using data generated in US children and adolescents [10]. This definition accounted for potential regional blood pressure differences related to height. For pediatric patients, we derived the standard cutoff definitions of overweight and obesity based on Cole et al. [11]. This group defined overweight as a body mass index (BMI) of 25–30 kg/m2 and obesity as a BMI >30 kg/m2. For quality assurance, we set height limits for patients less than 3 years of age at 100 cm and for those less than 12 years of age at 170 cm.
Nutritional information included serum albumin, serum creatinine and normalized protein catabolic rate (nPCR). Inflammatory markers analyzed were C-reactive protein (CRP), ferritin and neutrophil-to-lymphocyte ratio (NLR). Treatment and adequacy measures included post-dialysis weight, inter-dialytic weight gain (IDWG) as percent of post-dialysis weight, ultrafiltration rate, treatment time, equilibrated Kt/V (eKt/V) and urea reduction ratio (URR). For all clinical and laboratory parameters, the mean of the first year on dialysis was used.
Outcomes
We report odds ratio (OR) of death in the first year of dialysis in the pediatric and young adult patients separately. For hospital admissions, we constructed Poisson regression with number of hospitalizations as the outcome with an offset for exposure days. In both mortality and hospitalization analyses, Europe was used as a reference group. Dialysis catheter use was determined at onset, at 6 months, and at 1 year or date of censoring (whichever was earlier).
Data are presented as the mean with standard deviation for continuous variables, and percent (%) for categorical variables. One-way analysis of variance and χ2-tests were used to compare continuous and categorical variables, respectively. Linear regression was used to assess differences in patient treatment and laboratory parameters adjusted for regional differences, as well as age, gender and cause of ESRD. Univariate Kaplan–Meier analysis was used to assess catheter prevalence by region at 183 and 365 days, and log-rank test was used for group comparison. All P-values are two sided. The analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC, USA).
Results
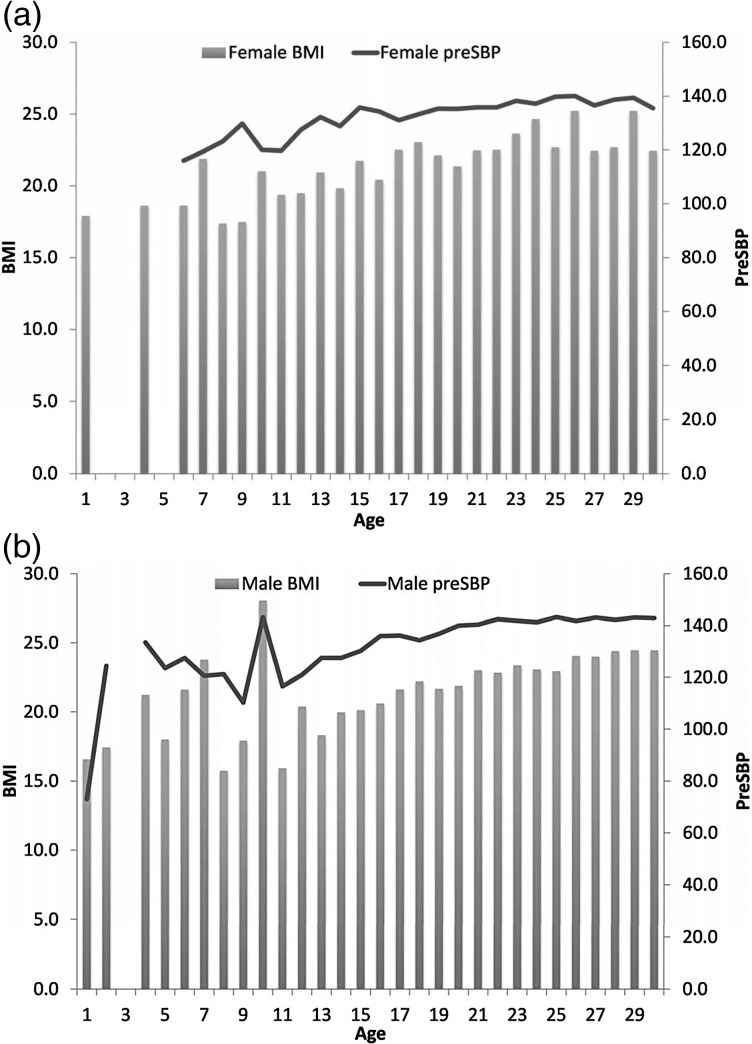
We included 3244 patients aged 0–30 years, with 418 (13%) in the pediatric group aged 0–18 years, and 2826 (87%) in the young adult group, aged 19–30 years. Sex, race and patient characteristics, including cause of ESRD and comorbidities, are reported by region in Table 1 (74% were white, 9% were black and 5% were of Asian race). The age distribution is depicted in Figure 1. In the pediatric group, the South America region has the greatest pediatric representation, whereas the European region has the greatest representation in the young adult group. Gender distribution was similar in both age groups with the exception that there were more males in the Asian pediatric group (62.8%). More than 90% of patients were treated in HD units managed by adult-focused providers.
Table 1.
Demographic information, cause of ESRD and comorbidities among 418 pediatric and 2826 young adult hemodialysis patients
| Age group (years) | Demographic characteristics |
ESRD causes |
Comorbidities |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Continent | N | Age (±SD) | Black (%) | White (%) | Asian (%) | Male (%) | Unknown (%) | DM (%) | GU (%) | Glomerular (%) | Other (%) | HTN (%) | CHF (%) | Any CVD (%) | 2o DM (%) | |
| ≤18 | Asia | 43 | 15.1 (2.8) | 0.0 | 72.1 | 25.6 | 62.8 | 55.8 | 2.3 | 11.6 | 25.6 | 4.6 | 6.3 | 0.0 | 7.3 | 2.3 |
| Europe | 47 | 15.7 (2.7) | 0.0 | 93.6 | 0 | 55.3 | 51.1 | 0.0 | 27.6 | 21.3 | 0.0 | 8.5 | 0.0 | 8.5 | 0.0 | |
| North America | 44 | 15.2 (2.1) | 40.9 | 56.8 | 0 | 45.5 | 20.5 | 2.3 | 20.4 | 38.6 | 18.2 | 52.3 | 2.3 | 52.3 | 6.8 | |
| South America | 284 | 14.4 (3.6) | 3.2 | 70.8 | 0 | 53.2 | N/A | N/A | N/A | N/A | N/A | 10.9 | 1.4 | 8.1 | 0.4 | |
| >18 | Asia | 371 | 25.3 (3.4) | 0.0 | 63.3 | 36.4 | 61.5 | 41.2 | 11.6 | 6.8 | 24.5 | 15.9 | 8.1 | 0 | 6.3 | 11.6 |
| Europe | 1039 | 25.3 (3.2) | 1.5 | 92.4 | 0.5 | 62.2 | 46.8 | 6.3 | 14.0 | 23.0 | 9.8 | 17.0 | 0.7 | 19.8 | 7.4 | |
| North America | 423 | 25.2 (3.4) | 45.6 | 48.9 | 3.3 | 51.8 | 16.5 | 13.0 | 12.0 | 24.1 | 34.3 | 50.6 | 8.3 | 53.9 | 20.3 | |
| South America | 993 | 25.2 (3.4) | 4.1 | 70.9 | 0.1 | 51.8 | N/A | N/A | N/A | N/A | N/A | 30.4 | 2.8 | 23.8 | 5.6 | |
All continuous variables are presented as mean (±SD).
ESRD, end-stage renal disease; DM, diabetes mellitus; GU, congenital anomalies of the kidneys and urinary tract, cystic and hereditary conditions, glomerular and ‘other’ (e.g. tubule-interstitial nephritis or tubular necrosis); HTN, hypertension; CHF, congestive heart failure; CVD, cardiovascular disease; 2o DM, secondary diabetes mellitus.
Fig. 1.
Age distribution (in years) of study patients.
Cause of ESRD
For those for whom an ICD code was provided, 16–55% had a diagnosis of ‘unknown’ cause of ESRD. Non-glomerular (GU) etiologies were most commonly reported in the European region in both age groups. In the pediatric group, glomerular disease was the most common cause of ESRD in the Asian and North American regions. In the young adult group, glomerular disease was the most common cause in Asia and Europe, whereas ‘unknown’ was most common in North America. Diabetes as the primary cause of ESRD was seen in Asia (2.3% of children and 11.6% of young adults) and North America (2.3% in children and 13.0% of young adults).
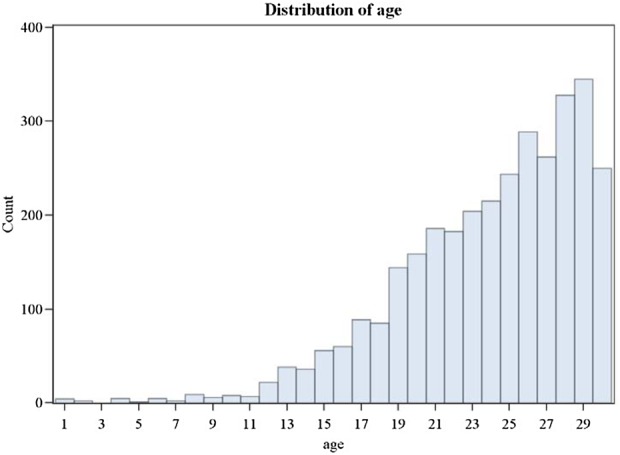
Cardiovascular disease
Compared with other regions, North America had the highest mean BMI and the highest rates of hypertension and CVD in both age groups (Table 2). Adjusted linear regression analysis demonstrated that mean preSBP was significantly higher among pediatric and young adult patients in North America compared with all other regions (all P < 0.02) (results not shown). PreSBP and preDBP were positively correlated with age in both groups. Males had significantly higher average preSBP readings, by 1.6 mmHg in the pediatric group and 6.0 mmHg in the young adult group (P < 0.001 for both). No significant differences in preSBP and preDBP were observed in pediatric patients by ESRD etiology. Using the patients with unknown diagnosis as a reference group, preSBP was significantly higher in young adults with diabetes (by 10.5 mmHg, P < 0.001) or glomerular conditions (by 2.7 mmHg, P = 0.013) as ESRD cause. When adjusting for race, preSBP was still higher in North America, although white patients had lower preSBP by 6.2 mmHg compared with non-black and non-Asian patients (Asian and black patients' preSBP was not significantly different from non-black and non-Asian patients).
Table 2.
Catheter use, hospitalization, deaths, obesity and blood pressure
| Age group (years) | Continent | Initial catheter (%) | Catheter at 1 year (%) | Hospital admissionsa | OR of deathb | BMI (kg/m2) | Overweightc (%) | Obesed (%) | PreSBP (mmHg) | Pre-systolic HTNe (%) | PreDBP (mmHg) | Pre-diastolic HTNf (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤18 | Asia | 45 | 30 | −0.30 (−0.79, 0.18) | N/A | 18.9 (4.6) | 8 | 6 | 125.9 (15.2) | 24.2 | 76.9 (9.8) | 9.1 |
| Europe | 61.7 | 42.6 | 0.0 (ref) | N/A | 20.1 (4.5) | 12 | 4 | 133.3 (14.5) | 35.9 | 76.8 (11.7) | 7.7 | |
| North America | 86.4 | 77.3 | 0.59 (0.20, 0.97) | N/A | 25.1 (6.8) | 39 | 22 | 143.7 (17.1) | 57.6 | 82.8 (11.6) | 18.2 | |
| South America | 80.6 | −1.38 (−1.77, −0.98) | N/A | 20.3 (19.9) | 11 | 5 | 124.9 (17.1) | 26.8 | 72.9 (11.4) | 10.8 | ||
| >18 | Asia | 42 | 21.3 | −0.52 (−0.72, −0.32) | 1.20 (0.46, 3.16) | 21.3 (4.8) | 9 | 5 | 135.2 (17.5) | 80 (8.9) | ||
| Europe | 51 | 25.7 | 0.0 (ref) | 1.0 (ref) | 22.7 (5.7) | 15 | 6 | 139.9 (16.5) | 80.8 (11.2) | |||
| North America | 75.2 | 62.9 | 0.82 (0.70, 0.93) | 2.69 (1.29, 5.63) | 28.1 (10.2) | 19 | 31 | 148.8 (18.7) | 86.7 (12.4) | |||
| South America | 75.9 | −0.97 (−1.12, −0.82) | 4.21 (2.32, 7.63) | 22.4 (7.7) | 11 | 5 | 134.6 (18.4) | 77.7 (11.5) |
All continuous variables are presented as mean (±SD).
aPoisson regression with Europe as a reference group.
bLogistic regression with Europe as a reference group.
cOverweight and dobese are based on international pediatric age-specific definitions.
eHypertension (HTN) with preSBP >97th percentile for age.
fHypertensive with preDBP >97th percentile for age.
Mortality and hospitalizations
Death was uncommon in the pediatric sample (<1%) across all regions. In the young adult group and using Europe as the reference group, North America (OR 2.69; CI 1.29, 5.63) and South America (OR 4.21; CI 2.32, 7.63) reported the highest OR of death and Asia appeared to have a similar death rate compared with Europe (Table 2). In both age groups, the number of hospitalizations occurred most frequently in North America (Table 2).
Access
In both age groups, the Asian cohort had the lowest rates of HD catheters at the first HD treatment (45% in children and 42% in young adults). South America and North America reported the highest rates of catheter use among young adults (76 and 75%, respectively) at dialysis initiation. In both age groups, catheter dependence at 1 year was high in North America (77.3% in children and 62.9% in young adults; Table 2). Access data at the specified follow up time points were not available for South America. Kaplan–Meier curves demonstrated that these differences in catheter use and dependence are statistically significant at 183 and 365 days of treatments (see Figure 2).
Fig. 2.
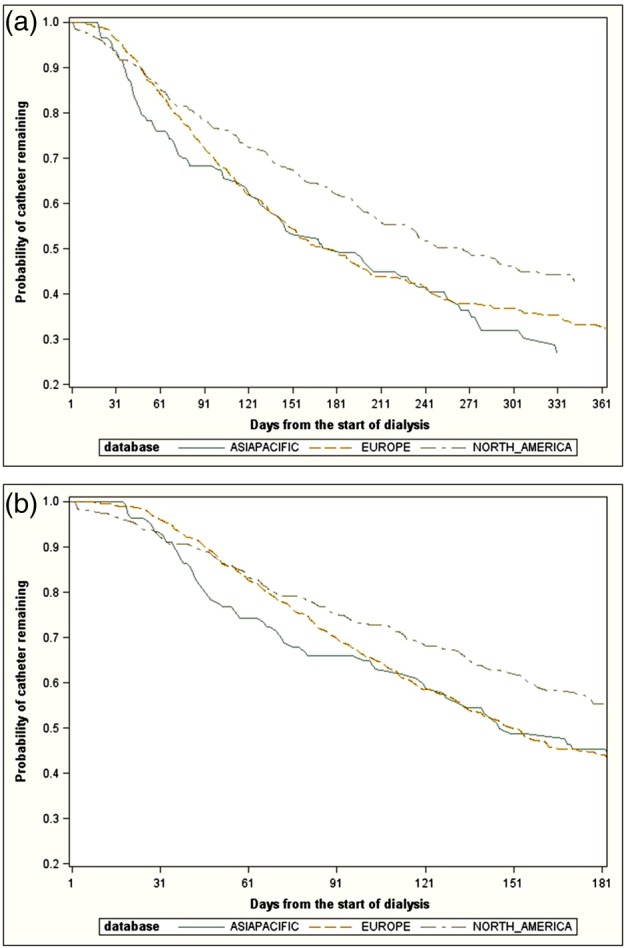
(a) Kaplan–Meier analysis of catheter prevalence over 183 days (log-rank test; P = 0.03). (b) Kaplan–Meier analysis of catheter prevalence over 365 days (log-rank test; P < 0.001).
Treatment times and adequacy
The Asian pediatric and young adult patients had the longest treatment times at 237 and 246 min, respectively, compared with the North American cohorts with the lowest mean treatment times reported, at 196 and 215 min, respectively (P < 0.001; Table 3). The mean URR ranged from 69.8% in North America to 76.2% in Asia and eKt/V ranged from 1.4 to 1.5 (Table 3). Using Europe as a reference group, males had significantly lower eKt/V in both age groups. Among young adults, eKt/V was significantly higher in the Asian and North American regions (P < 0.03 for both) when adjusted for age, gender and cause of ESRD (data not shown). We had no information on residual renal function.
Table 3.
Nutritional data, dialysis adequacy and inflammatory markers
| Age (years) | Continent | Serum albumin (g/dL) | Creatinine (mg/dL) | nPCR (g/kg/day) | IDWG (%) | Treatment time (min) | URR (%) | eKt/V | CRP (mg/L) | Ferritin (ng/mL) | NLR |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤18 | Asia | 4.1 (0.4) | 8.8 (3) | 1.1 (0.1) | 4.3 (2.2) | 237 (16.8)* | 76.2 (5.8) | 1.5 (0.3) | 7.9 (10.6) | 443.3 (250.6) | 2.3 (1.4) |
| Europe | 3.9 (0.6) | 7.8 (2.4) | 1 (0.1) | 3.7 (1.6) | 229 (24.7) | 73 (7.9) | 1.4 (0.3) | 12.1 (18) | 317.9 (288) | 3.6 (5) | |
| North America | 3.8 (0.6) | 8.6 (3.3) | 0.8 (0.2) | 3.1 (1.5) | 196 (15.9) | 69.8 (10.9) | 1.5 (0.4) | 516.7 (1281.9) | 6.7 (11) | ||
| South America | 3.7 (0.6) | 7.4 (3.4) | 1 (0.1) | 3.8 (1.9) | 228 (25.9) | 74 (7.6) | 1.4 (0.4) | 9.4 (18.8) | 383.2 (315) | 3.2 (3.7) | |
| >18 | Asia | 4 (0.5) | 9.5 (3) | 1.1 (0.1) | 3.9 (2) | 246 (24.4)* | 73.1 (7.2) | 1.4 (0.3) | 10.3 (18) | 456.9 (274.4) | 3 (2.3) |
| Europe | 3.9 (0.5) | 9.3 (2.6) | 1 (0.1) | 3 (1.4) | 235 (22.7) | 73.1 (7.5) | 1.4 (0.3) | 9.2 (15.9) | 340.3 (243.5) | 3.2 (3.3) | |
| North America | 3.9 (0.5) | 9.5 (3.4) | 0.8 (0.2) | 3.3 (1.4) | 215 (25.1) | 71.3 (7.5) | 1.4 (0.3) | 503.9 (523.2) | 4.1 (3.9) | ||
| South America | 3.9 (0.5) | 9 (3.5) | 1 (0.1) | 3.8 (1.8) | 239 (9.8) | 72.8 (8.1) | 1.4 (0.3) | 7.2 (13.2) | 395.1 (313.1) | 3.1 (2.6) |
Data are presented as mean (±SD).
IDWG, inter-dialytic weight gain; URR, urea reduction rate; CRP, C-reactive protein; NLR, neutrophil-to-lymphocyte ratio.
*P < 0.001.
Weight and inter-dialytic weight gain
The largest proportion of overweight and obese pediatric patients was observed in North America (39 and 22%, respectively), whereas the smallest was observed in Asia (8 and 6%, respectively). In an adjusted linear regression using Europe as the reference group, North American patients had significantly greater BMI among young adults (by 5.5 kg/m2, P < 0.001).The Asian young adult group had lower BMIs (by 1.4 kg/m2, P = 0.002). Refer to Figure 3 for the relationship between BMI and hypertension by age and sex.
Fig. 3.
(a) Mean BMI (in kg/m2) and preSBP (mmHg) in female patients. (b) Mean BMI (in kg/m2) and preSBP (mmHg) in male patients.
Serum albumin was higher in Asian pediatric and young adult patients. In both age groups, the mean nPCR ranged from 0.8 g/kg/day in North American patients to 1.1 g/kg/day in patients from Asia. Serum creatinine levels were also highest in patients from Asia in both age groups (Table 3).
The mean IDWG ranged from 3.0% body weight to 4.3% in both pediatric and young adult patients (Table 3). In an adjusted linear regression model, compared with Europe, the mean IDWG was significantly lower for North America in the pediatric group (P = 0.04). In the pediatric group, patients with diabetes had greater mean IDWG than those with other causes of ESRD.
Markers of inflammation
Ferritin levels were highest among North American pediatric and young adult patients compared with other regions. NLRs ranged from 2.3 (pediatric Asia group) to 6.7 (pediatric North America group). Highest NLR was observed in North America, while the lowest were seen in the Asian region in both young adults and pediatric patients (Table 3). CRP levels were not reported for North American patients of either age group.
Discussion
The PICCOLO MONDO is a unique longitudinal cohort that offers a view of baseline and 1-year outcomes in 0- to 30-year-old patients receiving HD through a single dialysis provider in several regions of the world. This unique opportunity was possible due to the good will of all volunteer MONDO Consortium participants [7, 8]. The sample size allowed us to characterize pediatric and young adult HD patients with conditions such as diabetes, expanding the CKiD Study diagnosis criteria [9].
For those with known cause of ESRD, CAKUT had the highest prevalence in Europe in both age groups. Glomerular conditions had the greatest number of cases reported in both age groups in North America and in Asia. We observed that patients in North America and Asia had similarly elevated rates of diabetes as a cause of ESRD in both age groups. The significance of this finding is unclear, but a possible explanation may be related to the prevalence of autoimmune conditions in these populations. In our cohort, we did not have granular information regarding the type of diabetes as the primary cause of ESRD. In a population-based study in Singapore, higher rice and noodle consumption was associated with greater markers of insulin resistance and hyperglycemia [12]. Furthermore, in an international registry of the USA and Europe, with nearly 33 000 pediatric patients with Type 1 DM, it was reported that 12% (n = 3977) of children in both registries combined were considered obese, 24% (n = 7825) or overweight, 64% (n = 20 942), based on the World Health Organization classification of BMI [13].
The PICCOLO MONDO cohort highlights the greater prevalence of cardiovascular risk factors (overweight, obesity and hypertension) in both age groups of North American patients compared with other regions, reflective of similar findings in the general worldwide population [14]. Figure 3 depicts the direct relationship between BMI and preSBP. As in older adults with ESRD, cardiovascular comorbidities are highly prevalent in both pediatric and young adult patients in all regions, although to varying degrees. In the USA, young adult ESRD patients have a 100-fold higher cardiovascular mortality rate than the general population [15]. Our study would support the same findings, but the magnitude may differ in other countries.
In an adult-based international study of HD patients, the USA has the highest rates of catheter use, followed by Europe and Japan [16]. Our study also showed high rates of HD catheter use (at baseline and 1-year follow-up) in North America, possibly associated with higher markers of inflammation. The lower IDWG, expressed as a percentage, in the North American and the European regions may be related to the higher BMI in these regions. The lower prevalence of hypertension in European patients may reflect the greater number of patients with GU anomalies as the cause of ESRD, who typically have a high urinary output and less hypertension.
While payer incentives and best practices vary by region, campaigns such as the ‘fistula first’ started in the USA during our study period. In North America, the catheter dependence in the pediatric cohort was greater than in the young adults of this region. This latter group had similar catheter use to the Medicare population in 2006 [17]. North America also had the highest odds of hospitalization when compared with the other regions in both age groups, whereas these outcomes are multi-factorial, the significantly greater catheter use in North America may in fact contribute to this outcome.
Although dialysis adequacy as measured by eKt/V was similar in all regions, North America had the shortest overall treatment times, whereas Asia had the longest overall treatment times. North America also had lower nPCR when compared with other countries, as well as higher inflammatory markers. Our findings related to the nPCR and CVD among Asians warrant discussion. In the general population, protein intake varies by region, but even within countries, cultural differences are noted in soy-based protein intake. In a community-based study in Canada for example, Asians consume more soy products compared with others [18]. Diet changes have been observed in the cohort followed by the Mediators of Atherosclerosis in South Asians Living in America Study, where the intake of nutrients such as protein and fiber were inversely associated with the length of residence in the USA (P trend <0.05) [19]. Greater soy food consumption has been associated with less lipid abnormalities, hyperuricemia and cardiometabolic disturbances, particularly in women from a community-based study in China [20]. CRP level, a marker of inflammation, has been associated with dietary patterns in a population-based study of Koreans, where men with hypertension in the ‘vegetable’ pattern group had lower CRP levels [21]. In an Asian population of patients with CKD, 24-h urinary protein excretion exceeded the recommended guidelines [22].
The PICCOLO MONDO cohort is quite different from national samples represented in databases such as the USRDS [1]. The advantage of this study is that it provides a unique opportunity to explore the segment of the child and young adult ESRD population managed in adult-oriented dialysis units. Most children and younger adolescents are treated by pediatric sub-specialists in developed countries, whereas adolescents >16 years of age are commonly treated by adult-focused specialists. The focus of the nephrologist as adult- or child-oriented may influence how pediatric dialysis patients are viewed and treated within dialysis facilities [6]. The results of our analysis of children, adolescents and young adults in this cohort are consistent with the findings of treatment characteristics and behaviors described in cohorts of adult ESRD patients. For example, the Dialysis Outcomes and Practice Patterns (DOPPS) study showed that patients in the USA have consistently shorter treatment times than those in Europe or Japan [23]. Practices in South America were not analyzed by this DOPPS study.
Compared with the pediatric USRDS populations [1], this sample includes young adults, who are more likely to have glomerular disease. An important analysis that we were unable to address would be the comparison of outcomes by dialysis environment (adult versus pediatric oriented) with age and region matching. Such a study in the future may highlight opportunities to improve practice and outcomes in both types of dialysis practices.
Among our limitations, PICCOLO MONDO consists of dialysis providers interested in participating in this research initiative and who are not representative of all patients in the countries included. Pediatric and young adults in the North America region represent 5 and 12%, respectively, of the 2011 USRDS population [1]. To overcome different disease classification systems, we developed an equivalency algorithm. North America had the highest number of patients with a known cause of ESRD in both age groups. South America had the largest number of pediatric patients, but we were unable to determine their ESRD cause and 1-year dialysis access due to lack of documentation [7]. Overall, data were limited from South America, which made some comparisons and analyses difficult; however, important information was gleaned about this region with regard to demographics, comorbidities and clinical and laboratory characteristics. We had no information on residual renal function and the type of diabetes as the primary cause of ESRD. Also, in the European and Asia Pacific datasets, race information is not recorded, so we made assumptions on the race of the patients; in South America, a number of patients had missing race information. We defined overweight and obesity based on one of the international definitions for children by Cole et al. [11], although we acknowledge that other methods exist for obesity classification around the world. Further, adjusted analysis may be necessary to account for the differences in hospital admission rates and inflammatory markers. Finally, because this is a de-identified registry, we cannot confidently say which patients came from pediatric only units versus units with a mix of adult and pediatric patients. On the basis of a survey of the participating partners, we found that most clinics are not pediatric-specific. Because of this, pediatric data discussed in this manuscript may not be representative of the pediatric ESRD population.
Conclusions
The PICCOLO MONDO cohort describes and compares longitudinal data from pediatric and young adult HD patients within a single international dialysis provider system, and it was only possible by the good will and collaboration from all participating sites. Catheters for HD access are commonly used at initiation in both age groups and persist at 1 year across all regions. However, North American facilities rely on catheters more than other regions. Similarly, obesity and hypertension are most common in the Americas and represent a potential intervention target to reduce the long-term risk of cardiovascular comorbidities. Despite differences in treatment times, adequacy was similar in all regions. While these differences were observed in pediatric and adolescent patients, they may not be specific to these patients and point out a general ESRD patient care issue in those respective regions. This study highlights areas where further investigation is needed.
Funding
The members of the MONDO Consortium.
Conflict of interest statement
None declared. The results presented in this paper have not been published previously in whole or part, except in abstract form.
References
- 1.US Renal Data System. USRDS. 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2010 [Google Scholar]
- 2.ERA-EDTA Registry Annual Report 2008. Amsterdam, The Netherlands: Academic Medical Center, Department of Medical Informatics, 2010 [Google Scholar]
- 3.Harambat J, van Stralen KJ, Kim JJ, et al. Epidemiology of chronic kidney disease in children. Pediatr Nephrol 2012; 27: 363–373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orr NI, McDonald SP, McTaggart S, et al. Frequency, etiology and treatment of childhood end-stage kidney disease in Australia and New Zealand. Pediatr Nephrol 2009; 24: 1719–1726 [DOI] [PubMed] [Google Scholar]
- 5.Furth SL, Powe NR, Hwaung W, et al. Does greater pediatric experience influence treatment choices in chronic disease management? Dialysis modality choice for children with end-stage renal disease. Arch Pediatr Adolesc Med 1997; 151: 545–550 [DOI] [PubMed] [Google Scholar]
- 6.Furth SL, Hwang W, Yang C, et al. Relation between pediatric experience and treatment recommendations for children and adolescents with kidney failure. JAMA 2001; 285: 1027–1033 [DOI] [PubMed] [Google Scholar]
- 7.Usvyat LA, Haviv YS, Etter M, et al. 2013 The MONitoring Dialysis Outcomes (MONDO) initiative. Blood Purif 2013; 35: 37–48 [DOI] [PubMed] [Google Scholar]
- 8.von Gersdorff GD, Usvyat LA, Marcelli D, et al. 2013 Monitoring dialysis outcomes across the world—the MONDO Global Database Consortium. Blood Purif 2013; 36: 165–172 [DOI] [PubMed] [Google Scholar]
- 9.Wong CJ, Moxey-Mims M, Jerry-Fluker J, et al. KiD (CKD in Children) Prospective Cohort Study: a review of current findings. Am J Kidney Dis 2012; 60: 1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics 2004; 114: 555–576 [PubMed] [Google Scholar]
- 11.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320: 1240–1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zuñiga YL, Rebello SA, Oi PL, et al. Rice and noodle consumption is associated with insulin resistance and hyperglycaemia in an Asian population. Br J Nutr 2014; 111: 1118–1128 [DOI] [PubMed] [Google Scholar]
- 13.DuBose SN, Hermann JM, Tamborlane WV, et al. Obesity in youth with type 1 diabetes in Germany, Austria, and the United States. J Pediatr 2015; pii: S0022-3476(15)00554-5 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry 2012; 24: 176–188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parekh RS, Carroll CE, Wolfe RA, et al. Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 2002; 141: 191–197 [DOI] [PubMed] [Google Scholar]
- 16.Ethier J, Mendelssohn D, Elder SJ, et al. Vascular access use and outcomes: an international perspective from the Dialysis Outcomes and Practice Pattern study. Nephrol Dial Transplant 2008; 23: 3219–3226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Medicare & Medicaid Services: Press release dated 31 March 2006. INTER REF. http://www.cms.hhs.gov/apps/media/press/release.asp?Counter=1818 .
- 18.Mudryj AN, Aukema HM, Yu N. Intake patterns and dietary associations of soya protein consumption in adults and children in the Canadian Community Health Survey, Cycle 2.2. Br J Nutr 2015; 6: 1–11 [DOI] [PubMed] [Google Scholar]
- 19.Talegawkar SA, Kandula NR, Gadgil MD, et al. Dietary intakes among south Asian adults differ by length of residence in the USA. Public Health Nutr 2015; 20: 1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu J, Sun LL, He LP, et al. Soy food consumption, cardiometabolic alterations and carotid intima-media thickness in Chinese adults. Nutr Metab Cardiovasc Dis 2014; 24: 1097–1104 [DOI] [PubMed] [Google Scholar]
- 21.Lee Y, Kang D, Lee SA. Effect of dietary patterns on serum C-reactive protein level. Nutr Metab Cardiovasc Dis 2014; 24: 1004–1011 [DOI] [PubMed] [Google Scholar]
- 22.Teo BW, Toh QC, Xu H, et al. Dietary protein intake in a multi-ethnic Asian population of healthy participants and chronic kidney disease patients. Ann Acad Med Singapore 2015; 44: 145–149 [PubMed] [Google Scholar]
- 23.Tentori F, Zhang J, Li Y, et al. Longer dialysis session length is associated with better intermediate outcomes and survival among patients on in-center three times per week hemodialysis: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant 2012; 27: 4180–4188 [DOI] [PMC free article] [PubMed] [Google Scholar]