Abstract
Objective
To evaluate the association between length of ICU stay and 1-year mortality for elderly patients who survived to hospital discharge in the United States.
Design and Setting
Retrospective cohort study of a random sample of Medicare beneficiaries who survived to hospital discharge, with 1 and 3-year follow-up, stratified by the number of days of intensive care and with additional stratification based on receipt of mechanical ventilation.
Interventions
None
Patients
The cohort included 34,696 Medicare beneficiaries older than 65 years who received intensive care and survived to hospital discharge in 2005.
Measurements and Main Results
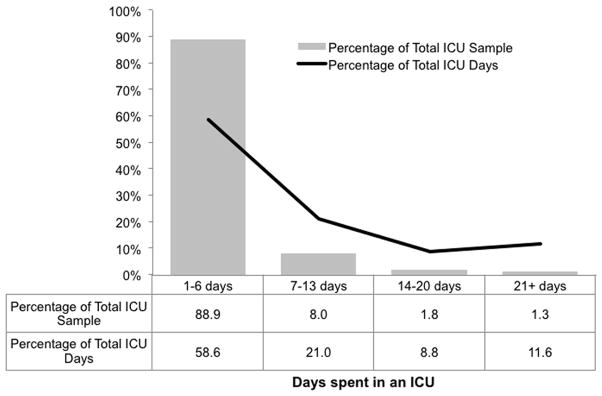
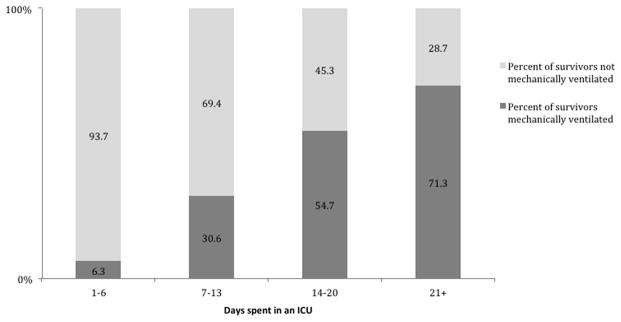
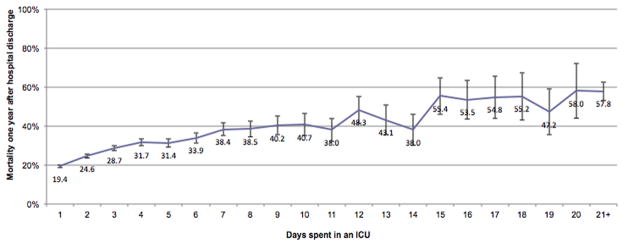
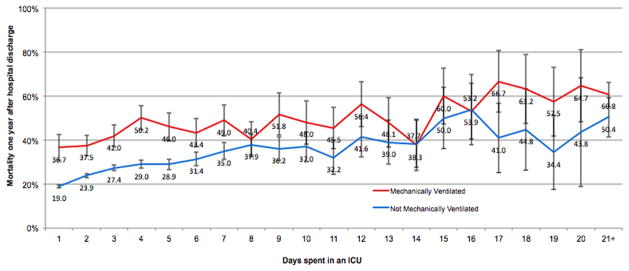
Among 34,696 patients who survived to hospital discharge, the mean ICU length of stay was 3.4 (±4.5) days. 88.9% of patients were in the ICU for 1–6 days, representing 58.6% of ICU bed-days. 1.3% of patients were in the ICU for 21+ days, but these patients used 11.6% of bed-days. The percentage of mechanically ventilated patients increased with increasing length of stay (6.3% for 1–6 days in the ICU and 71.3% for 21+ days). One-year mortality was 26.6%, ranging from 19.4% for patients in the ICU for one day, up to 57.8% for patients in the ICU for 21+ days. For each day beyond seven days in the ICU, there was an increased odds of death by 1-year of 1.04 (95% CI 1.03–1.05) irrespective of the need for mechanical ventilation.
Conclusions
Increasing ICU length of stay is associated with higher 1-year mortality for both mechanically ventilated and non-mechanically ventilated patients. No specific cut-off was associated with a clear plateau or sharp increase in long-term risk.
Keywords: Respirator artificial, critical illness, chronic disease, outcomes research, respiratory care units, mechanical ventilation
INTRODUCTION
Due to advancements in medical technology and management of illnesses such as sepsis, an increasing number of intensive care unit (ICU) patients are stabilized during acute illness following prolonged resuscitation and treatment. These patients develop metabolic, neuroendocrine, immunological, and neuromuscular disturbances, become dependent on intensive care therapies, and may require prolonged organ support. These patients are often described as being “chronically critically ill”(1). The development of this new type of patient in the modern era poses novel challenges for care, prognosis, and health care utilization in the ICU and after discharge (2). Yet, studies are hampered by a lack of data identifying the appropriate at-risk groups, and associated long-term outcomes, and often focus on data from single centers (3–8). In particular, definitions of chronic critical illness vary and outcomes differ based on cohort definitions (9). Most studies use a minimum length of stay in the ICU such as 21 days (10), or 28 days to define this illness (3–5, 7, 8). Several studies have investigated patients who specifically received prolonged mechanical ventilation (ranging from 24 hours to 28 days) (5, 6, 9, 11–18), while others have used the need for tracheostomy (2, 13, 17, 19). However, patients who are mechanically ventilated represent a small subgroup of elderly patients who receive intensive care in the United States (20), and the broader population of hospital survivors who received intensive care remains unexplored.
We therefore sought to determine the relationship between ICU length of stay and long-term mortality for elderly Medicare beneficiaries admitted to the ICU and survived to hospital discharge in order to provide data relevant for both future research and prognostication.
METHODS
Design and Data Sources
We conducted a retrospective, cohort study using data from 2004 through 2008 from the 5% Medicare Standard Analytic Files from the Centers for Medicare and Medicaid Services. The data set contains all fee-for-service claims, including hospital inpatient, hospital outpatient, skilled nursing facility, and “carrier” claims (which includes all office visits), for a random, longitudinal 5% sample of beneficiaries.
Cohort
We created a cohort of all Medicare beneficiaries who were 66 years of age or older who received intensive care in 2005 using a random 5% sample. We categorized any person with intensive care room charges as having received intensive care. We excluded anyone who received intermediate intensive care or only coronary care or intermediate coronary care room charges because these patients have lower hospital mortality and constitute a distinct group of patients with cardiac disease. We then excluded anyone who died during the hospitalization, so that the cohort consisted of patients who survived to hospital discharge.
Data Analyses
The exposure of interest was days spent in the ICU. The primary outcome was one year mortality, and secondary outcome was three year mortality. We first calculated summary statistics for demographic and clinical characteristics, including age, sex, race, and comorbidities of patients by using percentages, means ± standard deviations (±sd), and medians with interquartile ranges (IQR) when appropriate. For the purposes of summary statistics, we grouped patients based on the number of days spent in the ICU (1–6 days, 7–13, 14–20, 21+). Due to the small sample size, we grouped all patients who were in the ICU for 21 or more days together. Using information from the index hospitalization, we identified patients who received any mechanical ventilation, defined as ICD-9 procedure code 31.1 (temporary tracheostomy) or 96.7x (mechanical ventilation) or the Diagnosis-Related Group 483 (tracheostomy with mechanical ventilation > 96 hours) (21). We also stratified patients who received mechanical ventilation as less than 96 hours (96.71) and 96 hours or more (96.72). Non-surgical and surgical patients were defined using DRGs, and we grouped patients by age at hospitalization (66 to 74, 75 to 84, and 85 years and above) for the whole cohort and for mechanically ventilated subgroups. We used data from all health care encounters from the 4 quarters prior to the index hospitalization and secondary diagnoses from the index hospitalization to calculate Elixhauser comorbidities by using ICD-9-CM codes (22). We present counts of the total number of Elixhauser comorbidities (see Appendix Table 1).
We then examined the relationship between total ICU length of stay and 1- and 3-year mortality, with 1-year mortality the primary outcome. We first assessed this visually, and then generated logistic regression models to determine whether there was an increased risk of 1-year mortality associated with each additional day spent in the ICU. Due to the fact that (1) the majority of patients spent 1–6 days in the ICU, and we were interested in determining the relative risk for patients with longer lengths of stay in the ICU, we created a model that excluded patients who spent 1–6 days in the ICU, and used patients who were in the ICU for seven days as the baseline group.
Variables included in the model for risk-adjustment included age, sex, race, Elixhauser comorbidities, whether the patients were medical or surgical, and whether or not the patient was mechanically ventilated. Due to an a priori hypothesis of different relationships between ICU length of stay and mortality for patients who did or did not require mechanical ventilation, we assessed for a possible interaction between mechanical ventilation and length of stay in the model using the Breslow-Day test and determined that there was no statistically significant interaction. Because of the concern for immortality bias associated with longer stays in ICU, we did not include factors that would accrue during a stay in ICU (such as dialysis). We did include mechanical ventilation because it typical occurs on day one in the ICU.
Database management and statistical analysis were performed with Excel (Microsoft, Redmond, WA), and SAS version 9.2 (SAS Institute Inc., Cary, NC) software. All hypothesis tests were two-sided and considered statistically significant if ≤ 0.05. We also assessed differences for clinical significance because of the large size of the data set. This research involved secondary analyses of de-identified data and was granted a waiver of consent by the Columbia University Medical Center Institutional Review Board.
RESULTS
After exclusions (Figure 1), the cohort included 34,696 Medicare beneficiaries older than 65 years who received intensive care and survived to hospital discharge in 2005.
Figure 1.
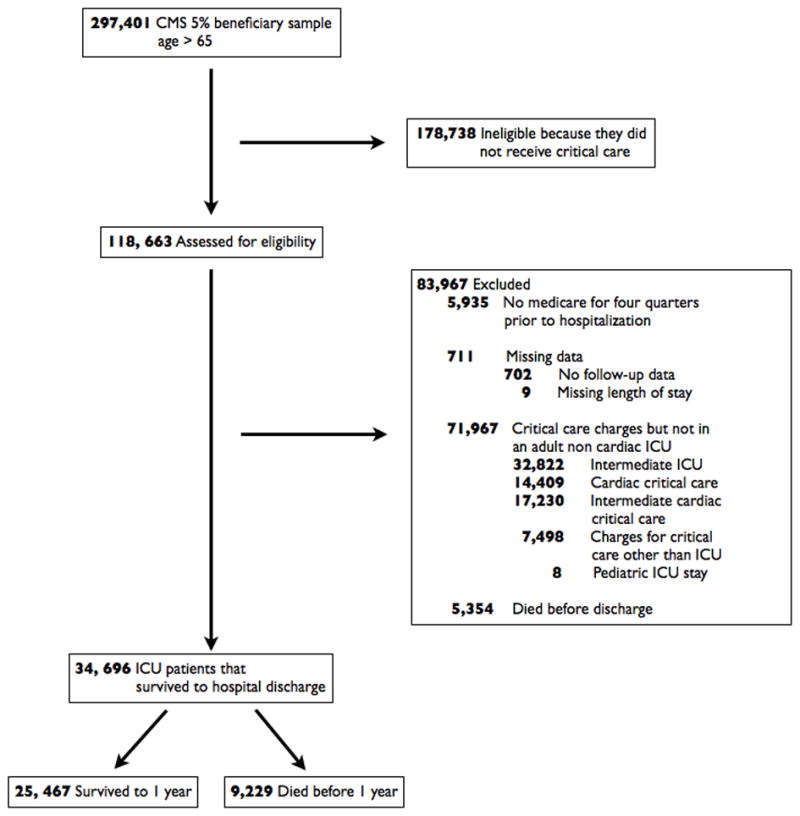
Patient flowchart of cohort of ICU survivors
ICU Length of Stay
The mean ICU length of stay was 3.4 (±4.5) days for intensive care patients who survived to hospital discharge, with a median of 2 day (IQR 1–4) (Table 1). A third of patients (35.9%) spent only 1 day in the ICU and 88.9% of patients were in the ICU for 1–6 days, representing 58.6% of the ICU bed-days in the cohort. Only 1.3% of patients were in the ICU for 21+ days, but these patients took up 11.6% of bed-days (Figure 2).
Table 1.
Characteristics of Medicare beneficiaries who received intensive care, stratified by days spent in an ICU
| Days spent in an ICU (days) | |||||
|---|---|---|---|---|---|
| Characteristics | Survived to hospital discharge | 1–6 | 7–13 | 14–20 | 21+ |
| (N=34,696) | (N=30,855) | (N=2,769) | (N=636) | (N=436) | |
| Male, n (%) | 16,460 (47.4) | 14586 (47.3) | 1348 (48.7) | 318 (50.0) | 208 (47.7) |
| Age, (yrs), median (IQR) | 77 (72–82) | 77 (72–82) | 77 (72–82) | 77 (72–81) | 75 (70–81) |
| Age, (yrs) mean (±sd) | 77.3 ± 7.1 | 77.3 ± 7.2 | 77.5 ± 7.0 | 76.9 ± 6.5 | 75.8 ± 6.7 |
| Age, (yrs), n (%) | |||||
| 66–69 | 5640 (16.3) | 5061 (16.4) | 409 (14.8) | 82 (12.9) | 88 (20.2) |
| 70–74 | 7875 (22.7) | 6979 (22.6) | 610 (22.0) | 173 (27.2) | 113 (25.9) |
| 75–79 | 8270 (23.8) | 7301 (23.7) | 699 (25.2) | 165 (25.9) | 105 (24.1) |
| 80–84 | 7080 (20.4) | 6280 (20.4) | 579 (20.9) | 135 (21.2) | 86 (19.7) |
| 85+ | 5831 (16.8) | 5234 (17.0) | 472 (17.1) | 81 (12.7) | 44 (10.1) |
| Race, n (%) | |||||
| White, non-Hispanic | 30375 (87.6) | 27124 (87.9) | 2362 (85.3) | 521 (81.9) | 368 (84.4) |
| Black, non-Hispanic | 2964 (8.5) | 2535 (8.2) | 296 (10.7) | 82 (12.9) | 51 (11.7) |
| Hispanic/Other Races | 1357 (3.9) | 1196 (3.9) | 111 (4.0) | 33 (5.2) | 17 (3.9) |
| Non-surgical, n (%) | 18839 (54.3) | 17175 (55.7) | 1376 (49.7) | 232 (36.5) | 56 (12.8) |
| Co-morbiditiesa, n (%) | |||||
| 0 | 8098 (23.3) | 7401 (24.0) | 513 (18.5) | 110 (17.3) | 74 (17.0) |
| 1 | 8292 (23.9) | 7502 (24.3) | 613 (22.1) | 99 (15.6) | 78 (17.9) |
| 2 | 6617 (19.1) | 5876 (19.0) | 509 (18.4) | 143 (22.5) | 89 (20.4) |
| 3+ | 11689 (33.7) | 10076 (32.7) | 1134 (41.0) | 284 (44.7) | 195 (44.7) |
| Mechanical Ventilation, n (%) | |||||
| None | 31235 (90.0) | 28899 (93.7) | 1923 (69.5) | 288 (45.3) | 125 (28.7) |
| < 96 hoursb | 2022 (5.8) | 1635 (5.3) | 321 (11.60) | 55 (8.7) | 11 (2.5) |
| ≥ 96 hours or moreb | 1439 (4.2) | 321 (1.0) | 525 (19.0) | 293 (46.1) | 300 (68.8) |
| Tracheostomy | 486 (1.4) | 82 (0.3) | 84 (3.0) | 109 (17.1) | 211 (48.4) |
| Organ failurec | |||||
| None | 25675 (74.0) | 23995 (77.8) | 1370 (49.5) | 200 (31.5) | 110 (25.2) |
| 1 | 7110 (20.5) | 5699 (18.5) | 948 (34.2) | 271 (42.6) | 192 (44.0) |
| 2+ | 1911 (5.5) | 1161 (3.8) | 451 (16.3) | 165 (25.9) | 134 (30.7) |
| ICU length of stay, mean (±sd) | 3.4 ± 4.5 | 2.3 ± 1.4 | 9.0 ± 8.0 | 16.4 ± 2.0 | 31.4 ± 12.0 |
| ICU length of stay, median (IQR) | 2 (1–4) | 2 (1–3) | 8 (7–10) | 16 (15–18) | 28 (23–36) |
| Non-ICU Hospital length of stay, mean (±sd) | 4.6 ± 6.1 | 4.3 ± 5.4 | 6.4 ± 7.6 | 7.8 ± 10.4 | 9.1 ± 16.3 |
| Total Hospital length of stayd, mean (±sd) | 8.0 ± 8.2 | 6.6 ± 5.8 | 15.4 ± 7.9 | 24.2 ± 10.5 | 40.5 ± 21.3 |
| Discharge location | |||||
| Home | 15776 (45.5) | 15118 (48.9) | 561 (20.3) | 68 (10.7) | 29 (6.7) |
| Skilled care/rehab | 12866 (37.1) | 10455 (33.9) | 1595 (57.6) | 454 (71.4) | 362 (83.0) |
| Other acute hospital | 5101 (14.7) | 4530 (14.7) | 476 (17.2) | 70 (11.0) | 25 (5.7) |
| Hospice | 867 (2.5) | 670 (2.2) | 134 (4.8) | 43 (6.8) | 20 (4.6) |
| Other | 86 (0.2) | 82 (0.3) | NA | NA | NA |
Notes:
Abbreviations: ICU, intensive care unit; IQR, interquartile range; sd, standard deviation; NA = not available due to small numbers
Includes only distinct Elixhauser comorbidities that negatively impact mortality; having diabetes with or without complications, and having a tumor with or without metastasis counts as 1 comorbidity each.
Includes patients with tracheostomies
Organ failures defined using the severe sepsis definition from Angus et al. (23)
Hospital length of stay includes both intensive care and hospital days.
Figure 2.
Distribution of Medicare beneficiaries who survived to hospital discharge, and proportion of total bed days, stratified by length of stay in ICU
Cohort Characteristics
Of the cohort, 47.4% were male and 87.6% were non-Hispanic white (Table 1). The mean age of the cohort was 77.3 ±7.1. Most patients (76.7%) had at least one Elixhauser comorbidity (see Appendix Table 1 for full list of comorbidities), and 33.7% had three or more comorbidities. Among survivors to hospital discharge, almost one quarter of patients had organ failure. For patients in the ICU between 7 and 13 days, over 50% of patients had at least one organ that had failed and for patients in the ICU more than 21 days (three weeks), 75% of patients had one or more organs fail. (Table 1) (23). Stratified by ICU length of stay, gender and age distributions were similar. The percentage of patients who were non-surgical decreased as the ICU length of stay increased, such that only 12.8% of patients who stayed 21+ days were non-surgical.
The majority of patients (90.0%) who were admitted to ICU and survived to hospital discharge were not mechanically ventilated. Among patients who stayed only 1–6 days in the ICU, only 6.3% received mechanical ventilation (Figure 3). This increased to 71.3% of patients who were in the ICU for 21+ days.
Figure 3.
Percentage of Medicare beneficiaries who survived to hospital discharge who received mechanical ventilation, stratified by length of stay in the ICU
Discharge Destination
Among all ICU patients who survived to hospital discharge, 45.5% were discharged to home (Table 1). Very few patients who stayed in the ICU for more than 14 days were discharged home (10.7% for patients 14–20 days; 6.7% for 21+ days). As length of stay in the ICU increased, the percentage discharged to skilled care facilities or rehabilitation increased (83.0% for patients in the ICU 21+ days).
1- and 3-year mortality
The 1-year mortality ranged from 19.4% for patients who stayed one day in the ICU, up to 57.8% for patients staying 21+ days (Figure 4), and 3-year mortality ranged from 35.1% to 70.4% (data not shown). Characteristics of ICU patients stratified by 1-year survival are reported in Appendix Table 2. Overall mortality for patients who were not mechanically ventilated was lower than for mechanically ventilated patients (Figure 5), with a 1-year mortality of 50.4% for non-mechanically ventilated patients (versus 60.8% for those mechanically ventilated) who received intensive care for 21+ days.
Figure 4.
1-year mortality for Medicare beneficiaries who received intensive care and survived to hospital discharge, by days in the ICU
Figure 5.
1-year mortality for Medicare beneficiaries who received intensive care and survived to hospital discharge, stratified by days in the ICU and whether or not patients received invasive mechanical ventilation
After multivariable modeling, for each day beyond seven days in the ICU, there was an increased odds of death by 1-year of 1.04 (95% CI 1.03–1.05), irrespective of the need for mechanical ventilation (Table 2). This estimate was similar for the model using 3-year mortality adjusted OR 1.04 (95% CI 1.02–1.05) (data not shown).
Table 2.
Multivariable Logistic Regression Analysis of Association between Days Spent in and ICU and Mortality 1 Year after Discharge
| Variable | Adjusted OR | (95% CI) | P Value |
|---|---|---|---|
| Spent 7 days in an ICU | ref | ||
| Each additional day spent in an ICU | 1.04 | (1.03–1.05) | <0.0001 |
| White, non-Hispanic | ref | ||
| Hispanic/Other Races | 0.89 | (0.63–1.25) | 0.50 |
| Black, non-Hispanic | 1.26 | (1.01–1.57) | 0.04 |
| Female | ref | ||
| Male | 1.12 | (0.98–1.29) | 0.10 |
| Age (centered at mean=77 years) | ref | ||
| Age (each 1 year increase) | 1.06 | (1.05–1.07) | <0.0001 |
| Surgical patient | ref | ||
| Medical patient | 1.55 | (1.34–1.79) | <0.0001 |
| Not Mechanically ventilated | ref | ||
| Mechanically ventilated | 1.67 | (1.44–1.93) | <0.0001 |
| Prior medical history (ref=no history of condition) | ref | ||
| Congestive heart failure | 1.25 | (1.07–1.46) | <0.01 |
| Neurological disorders | 1.34 | (1.10–1.62) | <0.01 |
| Chronic pulmonary disease | 1.22 | (1.05–1.41) | 0.01 |
| Renal Failure | 1.36 | (1.05–1.76) | 0.02 |
| Metastatic Cancer | 3.14 | (1.93–5.10) | <0.01 |
| Solid tumor w/out metastasis | 1.41 | (1.13–1.77) | <0.01 |
| Weight loss | 1.49 | (1.18–1.87) | <0.001 |
| Fluid and electrolyte disorders | 1.37 | (1.15–1.62) | <0.001 |
| Deficiency Anemias | 1.26 | (1.08–1.47) | <0.01 |
Notes:
Abbreviations: OR = odds ratio, CI = confidence intervals, ICU = intensive care unit.
Sample consists of everyone with at least 7 days spent in an ICU n=3,841. Prior medical history is based on Elixhauser conditions defined using ICD-9-CM diagnoses codes from the previous year. Hosmer-Lemeshow goodness -of-fit test, p=0.543
DISCUSSION
Approximately 1.4 million elderly Medicare beneficiaries survive to hospital discharge after receiving intensive care. Elderly patients who are discharged alive and required prolonged critical care services represent a small portion of all ICU patients, yet this population consumes a disproportionate percentage of health care resources (24). In this cohort of elderly US ICU survivors who were discharged from the hospital, 40% of ICU days were used by the 11% of patients who were in the ICU for one week or more. After experiencing one week of intensive care and surviving to hospital discharge, more than a third of patients died within one year of discharge regardless of whether or not they received mechanical ventilation. We found that overall mortality rates continued to increase with increased length of stay, independent of mechanical ventilation.
Definitions of chronic critical illness used in studies do vary, including mechanical ventilation for more than 24 hours (14, 25), 2 days (26), 4 days (12), 14 days (11, 27), 21 days (6, 9, 16, 18), and 28 days (5); tracheostomy (2, 13, 17, 19); or ICU length of stay of more than 7 days (28, 29), 10 days (30, 31), 14 days (32–35), 21 days (10), and 28 days (3–5, 7, 8). After studying the impact of a categorical continuum of ICU length of stay on mortality, we found that although mortality rates increased with increasing length of stay, there does not appear to be a clear length of stay cutoff at which a patient’s prognosis significantly changes. Our data suggest that chronic critically ill patients have a mixed trajectory, likely influenced by specific physiological changes and reserve.
Patients with prolonged mechanical ventilation have been identified as a group with a high mortality who consume a significant proportion of health care resources (6, 9, 36). In our cohort of elderly patients, 60% of patients who were in the ICU for more than a week did not receive mechanical ventilation, and the majority were surgical patients (based on DRG). Limiting economic investigations of the chronically critically ill to patients whose lungs are mechanically ventilated for a prolonged period may underestimate the financial impact of this unique group of patients (24). Poor outcomes, independent of the need for mechanical ventilation, may be attributable to the observed complications of prolonged critical care: nosocomial infections, immunosuppression, protein-wasting malnutrition, suppression of anterior pituitary hormone secretion, myopathy, posttraumatic stress disorder, and brain dysfunction (1).
Inadequate communication between health care providers and patients and their families is problematic (17, 35). The burden on caregivers and the ability to return home may be important when discussing quality of life after hospitalization. Only a small number of patients who were in the ICU for more than two weeks were discharged to home. Surrogate decision makers consider hospital and 1-year mortality “important to know.” A published survey reported that 94% of respondents did not receive information on 1-year survival (37). As patients stay longer and longer in the ICU, significant changes accrue in short- and long-term morbidity and mortality, which may be important to consider in medical decision-making. While we found that only 7% of patients in our cohort who were in the ICU for over 21 days were discharged to home, a little over 40% of those patients survived to 1 year. Although the overall prognosis of chronic critical illness is poor, these data also suggest that a significant number of patients actually survive chronic critical illness. While extended time in the ICU may often feel to caregivers like it must be associated with futile care, this simple marker does not provide any satisfactory cut-point.
The use of an administrative data set and the retrospective nature of this study are limitations. In particular, the use of Medicare data means that the analysis includes only those patients who are older than 65 years. However, the majority of US citizens older than 65 years participate in Medicare (19). Another limitation is that we do not have information about delayed or premature discharge from the ICU, both of which may have an impact on ultimate outcomes for patients and could influence our findings regarding the association between ICU length of stay and outcomes. It is also notable that the majority of long-stay ICU patients who survived to hospital discharge were classified as “surgical” based on their DRG. It is impossible to determine whether this is due to the fact that high-risk surgical patients represent a large proportion of this long-stay group, or whether increased length of stay in the ICU is associated with ultimately requiring a surgical procedure that may determine the DRG. This issue warrants further investigation. We do not have detailed data regarding the length of mechanical ventilation in these patients, which has often been used as a marker of chronic critical illness in other studies. We, therefore, cannot correlate the overall ICU length of stay with the exact length of mechanical ventilation for some patients. Finally, our database does not include physiological measurements that may impact management decisions.
CONCLUSIONS
These data provide important epidemiologic and prognostic information regarding the association between ICU length of stay and outcomes in elderly hospital survivors. After systematically, studying the impact of ICU length of stay on mortality in elderly hospital survivors, we found that long-term mortality rates increase with ICU length of stay regardless of whether or not patients experienced surgery or mechanical ventilation. Outcome studies of the chronically critically ill that limit inclusion criteria to patients who experience prolonged mechanical ventilation, and are only “medical” will exclude a significant number of at-risk patients. We also found that there is no clear ICU length of stay cut-off that identifies a chronically critically ill population at risk for poor long-term outcome.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by a Foundation for Anesthesia Education and Research (FAER) Fellowship Grant to Hannah Wunsch in 2008–2009, and also Award Number K08AG038477 from the National Institute On Aging
Footnotes
Copyright form disclosures:
Dr. Moitra served as a malpractice expert for several cases which are unrelated to this topic and received support for article research from the National Institutes of Health (NIH). His institution received funding from the Foundation for Anesthesia Education and Research (FAER) (Fellowship Grant to Hannah Wunsch in 2008–2009) and from the National Institute On Aging (Award Number K08AG038477). The remaining authors have disclosed that they do not have any potential conflicts of interest.
Institution where work was performed: Columbia University, College of Physicians & Surgeons
Financial Disclosures: The authors have no conflicts of interest to declare.
References
- 1.Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med. 182:446–454. doi: 10.1164/rccm.201002-0210CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Estenssoro E, Reina R, Canales HS, Saenz MG, Gonzalez FE, Aprea MM, Laffaire E, Gola V, Dubin A. The distinct clinical profile of chronically critically ill patients: A cohort study. Crit Care. 2006;10:R89. doi: 10.1186/cc4941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hartl WH, Wolf H, Schneider CP, Kuchenhoff H, Jauch KW. Acute and long-term survival in chronically critically ill surgical patients: A retrospective observational study. Crit Care. 2007;11:R55. doi: 10.1186/cc5915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goins WA, Reynolds HN, Nyanjom D, Dunham CM. Outcome following prolonged intensive care unit stay in multiple trauma patients. Crit Care Med. 1991;19:339–345. doi: 10.1097/00003246-199103000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Gracey DR, Naessens JM, Krishan I, Marsh HM. Hospital and posthospital survival in patients mechanically ventilated for more than 29 days. Chest. 1992;101:211–214. doi: 10.1378/chest.101.1.211. [DOI] [PubMed] [Google Scholar]
- 6.MacIntyre NR, Epstein SK, Carson S, Scheinhorn D, Christopher K, Muldoon S. Management of patients requiring prolonged mechanical ventilation: Report of a namdrc consensus conference. Chest. 2005;128:3937–3954. doi: 10.1378/chest.128.6.3937. [DOI] [PubMed] [Google Scholar]
- 7.Montuclard L, Garrouste-Orgeas M, Timsit JF, Misset B, De Jonghe B, Carlet J. Outcome, functional autonomy, and quality of life of elderly patients with a long-term intensive care unit stay. Crit Care Med. 2000;28:3389–3395. doi: 10.1097/00003246-200010000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Friedrich JO, Wilson G, Chant C. Long-term outcomes and clinical predictors of hospital mortality in very long stay intensive care unit patients: A cohort study. Crit Care. 2006;10:R59. doi: 10.1186/cc4888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cox CE, Carson SS, Lindquist JH, Olsen MK, Govert JA, Chelluri L. Differences in one-year health outcomes and resource utilization by definition of prolonged mechanical ventilation: A prospective cohort study. Crit Care. 2007;11:R9. doi: 10.1186/cc5667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller RS, Patton M, Graham RM, Hollins D. Outcomes of trauma patients who survive prolonged lengths of stay in the intensive care unit. J Trauma. 2000;48:229–234. doi: 10.1097/00005373-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Combes A, Costa MA, Trouillet JL, Baudot J, Mokhtari M, Gibert C, Chastre J. Morbidity, mortality, and quality-of-life outcomes of patients requiring >or=14 days of mechanical ventilation. Crit Care Med. 2003;31:1373–1381. doi: 10.1097/01.CCM.0000065188.87029.C3. [DOI] [PubMed] [Google Scholar]
- 12.Douglas SL, Daly BJ, Gordon N, Brennan PF. Survival and quality of life: Short-term versus long-term ventilator patients. Crit Care Med. 2002;30:2655–2662. doi: 10.1097/00003246-200212000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Engoren M, Arslanian-Engoren C, Fenn-Buderer N. Hospital and long-term outcome after tracheostomy for respiratory failure. Chest. 2004;125:220–227. doi: 10.1378/chest.125.1.220. [DOI] [PubMed] [Google Scholar]
- 14.Spicher JE, White DP. Outcome and function following prolonged mechanical ventilation. Arch Intern Med. 1987;147:421–425. [PubMed] [Google Scholar]
- 15.Carson SS, Cox CE, Holmes GM, Howard A, Carey TS. The changing epidemiology of mechanical ventilation: A population-based study. J Intensive Care Med. 2006;21:173–182. doi: 10.1177/0885066605282784. [DOI] [PubMed] [Google Scholar]
- 16.Carson SS, Garrett J, Hanson LC, Lanier J, Govert J, Brake MC, Landucci DL, Cox CE, Carey TS. A prognostic model for one-year mortality in patients requiring prolonged mechanical ventilation. Crit Care Med. 2008;36:2061–2069. doi: 10.1097/CCM.0b013e31817b8925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, Olsen MK, Govert JA, Carson SS, Tulsky JA. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–2894. doi: 10.1097/CCM.0b013e3181ab86ed. quiz 2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, Clay AS, Chia J, Gray A, Tulsky JA, Cox CE. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: A cohort study. Ann Intern Med. 153:167–175. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Carson SS, Bach PB. The epidemiology and costs of chronic critical illness. Crit Care Clin. 2002;18:461–476. doi: 10.1016/s0749-0704(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 20.Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-year outcomes for medicare beneficiaries who survive intensive care. JAMA. 303:849–856. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- 21.Kahn JMCS, Angus DC, Linde-Zwirble WT, Iwashyna TJ. Development and validation of an algorithm for identifying prolonged mechanical ventilation in administrative data. Heatlh Serv Outcomes Res Method. 2009;9:117–132. [Google Scholar]
- 22.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the united states: Analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Cox CE, Carson SS, Govert JA, Chelluri L, Sanders GD. An economic evaluation of prolonged mechanical ventilation. Crit Care Med. 2007;35:1918–1927. doi: 10.1097/01.CCM.0000275391.35834.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gillespie DJ, Marsh HM, Divertie MB, Meadows JA., 3rd Clinical outcome of respiratory failure in patients requiring prolonged (greater than 24 hours) mechanical ventilation. Chest. 1986;90:364–369. doi: 10.1378/chest.90.3.364. [DOI] [PubMed] [Google Scholar]
- 26.Chelluri L, Im KA, Belle SH, Schulz R, Rotondi AJ, Donahoe MP, Sirio CA, Mendelsohn AB, Pinsky MR. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32:61–69. doi: 10.1097/01.CCM.0000098029.65347.F9. [DOI] [PubMed] [Google Scholar]
- 27.Vitacca M, Vianello A, Colombo D, Clini E, Porta R, Bianchi L, Arcaro G, Vitale G, Guffanti E, Lo Coco A, Ambrosino N. Comparison of two methods for weaning patients with chronic obstructive pulmonary disease requiring mechanical ventilation for more than 15 days. Am J Respir Crit Care Med. 2001;164:225–230. doi: 10.1164/ajrccm.164.2.2008160. [DOI] [PubMed] [Google Scholar]
- 28.Lipsett PA, Swoboda SM, Dickerson J, Ylitalo M, Gordon T, Breslow M, Campbell K, Dorman T, Pronovost P, Rosenfeld B. Survival and functional outcome after prolonged intensive care unit stay. Ann Surg. 2000;231:262–268. doi: 10.1097/00000658-200002000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stricker K, Rothen HU, Takala J. Resource use in the icu: Short- vs. Long-term patients. Acta Anaesthesiol Scand. 2003;47:508–515. doi: 10.1034/j.1399-6576.2003.00083.x. [DOI] [PubMed] [Google Scholar]
- 30.Bashour CA, Yared JP, Ryan TA, Rady MY, Mascha E, Leventhal MJ, Starr NJ. Long-term survival and functional capacity in cardiac surgery patients after prolonged intensive care. Crit Care Med. 2000;28:3847–3853. doi: 10.1097/00003246-200012000-00018. [DOI] [PubMed] [Google Scholar]
- 31.Weissman C. Analyzing the impact of long-term patients on icu bed utilization. Intensive Care Med. 2000;26:1319–1325. doi: 10.1007/s001340000612. [DOI] [PubMed] [Google Scholar]
- 32.Ryan TA, Rady MY, Bashour CA, Leventhal M, Lytle B, Starr NJ. Predictors of outcome in cardiac surgical patients with prolonged intensive care stay. Chest. 1997;112:1035–1042. doi: 10.1378/chest.112.4.1035. [DOI] [PubMed] [Google Scholar]
- 33.Heyland DK, Konopad E, Noseworthy TW, Johnston R, Gafni A. Is it ‘worthwhile’ to continue treating patients with a prolonged stay (>14 days) in the icu? An economic evaluation. Chest. 1998;114:192–198. doi: 10.1378/chest.114.1.192. [DOI] [PubMed] [Google Scholar]
- 34.Wong DT, Gomez M, McGuire GP, Kavanagh B. Utilization of intensive care unit days in a canadian medical-surgical intensive care unit. Crit Care Med. 1999;27:1319–1324. doi: 10.1097/00003246-199907000-00020. [DOI] [PubMed] [Google Scholar]
- 35.Teno JM, Fisher E, Hamel MB, Wu AW, Murphy DJ, Wenger NS, Lynn J, Harrell FE., Jr Decision-making and outcomes of prolonged icu stays in seriously ill patients. J Am Geriatr Soc. 2000;48:S70–74. doi: 10.1111/j.1532-5415.2000.tb03144.x. [DOI] [PubMed] [Google Scholar]
- 36.Nelson JE, Cox CE, Hope AA, Carson SS. Concise clinical review: Chronic critical illness. Am J Respir Crit Care Med. doi: 10.1164/rccm.201002-0210CI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nelson JE, Mercado AF, Camhi SL, Tandon N, Wallenstein S, August GI, Morrison RS. Communication about chronic critical illness. Arch Intern Med. 2007;167:2509–2515. doi: 10.1001/archinte.167.22.2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.