Abstract
This systematic review examines the characteristics and psychometric properties of the instruments used to assess self-care behaviors among persons with type 2 diabetes. Electronic databases were searched for relevant studies published in English within the past 20 years. Thirty different instruments were identified in 75 articles: 18 original instruments on type 2 diabetes mellitus self-care, 8 translated or revised version, and 4 not specific but relevant to diabetes. Twenty-one instruments were multidimensional and addressed multiple dimensions of self-care behavior. Nine were unidimensional: three focusing exclusively on medication taking, three on diet, one on physical activity, one on self-monitoring of blood glucose, and one on oral care. Most instruments (22 of 30) were developed during the last decade. Only 10 were repeated more than once. Nineteen of the 30 instruments reported both reliability and validity information but with varying degrees of rigor. In conclusion, most instruments used to measure self-care were relatively new and had been applied to only a limited number of studies with incomplete psychometric profiles. Rigorous psychometric testing, operational definition of self-care, and sufficient explanation of scoring need to be considered for further instrument development.
Keywords: type 2 diabetes mellitus, self-care, self-report, instrument
Introduction
With population growth, aging, and urbanization, diabetes has become a rising global hazard. According to the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group’s survey, the number of people with diabetes increased from 153 million in 1980 to 347 million in 2008 (Danaei et al., 2011). It is estimated that diabetes will affect 592 million worldwide by 2035 (Guariguata et al., 2014). As one of the top 10 leading causes of death in the world, type 2 diabetes mellitus (T2DM) represents 85–95% of all diabetes cases in developed countries and accounts for an even higher percentage in developing countries (Roglic et al., 2005). Multiple complications and premature mortality from uncontrolled T2DM often create a significant burden on the individual, family, and society.
Individuals with T2DM need to perform lifelong self-care to prevent or delay its short- and long-term complications and to improve quality of life. Self-care is defined as actions taken by individuals to care for themselves within their environmental conditions (Orem, 1995). There is no uniform terminology related to self-care, but this term is often used interchangeably with “self-management,” “compliance,” and “adherence” as in this article. For persons with T2DM, self-care involves a series of behaviors that encompass diet, exercise, medication taking (insulin or oral hypoglycemic agents), self-monitoring of blood glucose (SMBG), and foot care (Xu, Savage, Toobert, Wei, & Whitmer, 2008).
Self-care is regarded as a cornerstone of diabetes care. Therefore, an accurate assessment of diabetes self-care is crucial to identify and understand problem areas in the management of T2DM, to facilitate better glucose control, and to reduce complications of uncontrolled T2DM. Although the number of self-care instruments has increased significantly over the past two decades, systematic evaluations of these instruments are scarce. A critical review of existing self-care instruments can help health care professionals select high-quality instruments and adequately assess self-care behaviors of persons with T2DM. The two aims of this systematic review were to summarize the characteristics of self-report instruments used to assess self-care behavior among persons with T2DM and to compare and contrast the documented psychometric properties of the various instruments.
Material and Method
Search Strategy
A systematic literature search was conducted in PubMed, CINAHL, and PsycInfo electronic databases for articles published in January 1990–April 2014. The following combination of key words was used: (a) diabetes type 2 or noninsulin-dependent diabetes mellitus, (b) self-care or self-management or adherence or compliance, and (c) instrument or tool or measure* (including measure, measures and measurement) or scale or questionnaire. A hand search was also done to identify potentially relevant studies.
Review Process
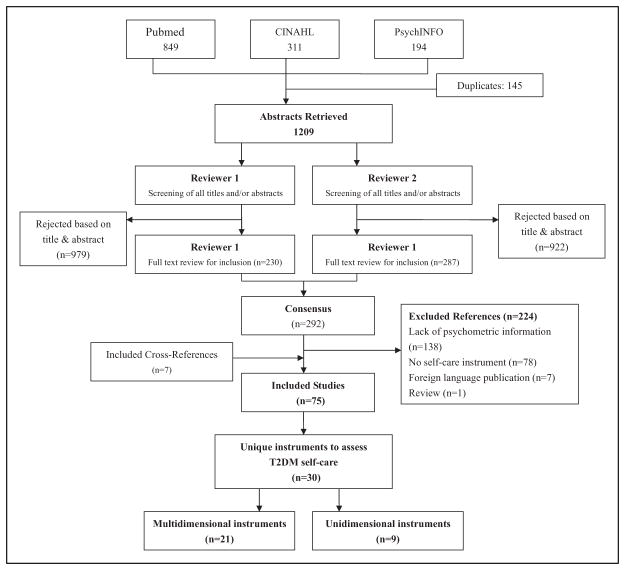
The initial search yielded 1,354 abstracts with 145 duplicate studies, and 1,209 abstracts remained for the initial screening. Two authors (Y.L. and J.X.) independently reviewed the titles and abstracts of the retrieved articles. The articles included in this review were original studies that (a) focused on a population with T2DM; (b) used self-report instruments to measure diabetes self-care behaviors such as diet, physical activity, medication, SMBG, or foot care; (c) were validation studies or studies that used any instruments addressing self-care behavior; or (d) reported psychometric properties of the instrument (i.e., reliability, validity, or both). In addition, articles were restricted to peer-reviewed journals published in English.
Based on the inclusion criteria, 292 articles were identified for full-text review. While reviewing, a structured form was created to ensure study eligibility, to record reasons for rejection, and to extract information on characteristics of each study selected (setting, characteristics of patients such as age, sex, disease duration, etc.) and self-care instrument (number of items, response format, domains, and psychometric properties, etc.). Of the 292 full-text articles reviewed, 224 were rejected for lack of psycho-metric information (n = 138), no self-care instrument (n = 78), foreign language publication (n = 7), or review article (n = 1), yielding 68 articles. Hand searches of cross-references yielded seven additional publications. As a result, 75 articles were included in our review. The study selection process is summarized in Figure 1.
Figure 1.
Study selection/review process.
The self-care instruments reported in the included articles were then evaluated for psychometric properties. For internal consistency reliability, a Cronbach’s α coefficient of .7 or higher was considered acceptable. In addition, average interitem correlations of .15–.50 and item to total correlations of .30–.70 were considered adequate (Nunnally & Bernstein, 1994). For convergent validity, a κ coefficient between .6 and .8 was considered acceptable and .8 or higher was considered desirable (Landis & Koch, 1977). Finally, the correlation coefficients (Pearson r, Spearman’s ρ) of .5 or higher against similar constructs were considered to have good construct validity (Eliasziw, Young, Woodbury, & Fryday-Field, 1994).
Results
Overview of the Studies
Of the 75 studies, 25 were validation studies (12 for original instruments, 11 for trans-cultural adaptation, and 2 for revision of an original instrument), 37 were descriptive studies, and 13 were intervention studies. Thirty-four studies reported both reliability and validity testing of the instrument used. Almost half (n = 37) included patient populations in Asia, followed by North America (n = 12 for the United States, n = 5 for Canada) and Europe (n = 9). The sample size of the studies ranged from 10 to 1,369. Of these, 30 unique diabetes self-care instruments were identified.
Characteristics of the T2DM Self-Care Instruments
Details of each T2DM self-care instrument, illustrating its various content areas, number of items, response format, and psychometric evaluation are presented in Table 1. Of the 30 instruments, 21 addressed multiple dimensions of key self-care areas such as diet, physical activity, medication, SMBG, or foot care, in addition to other less common areas such as problem solving, interaction with providers, or management of hypoglycemia. Nine were unidimensional measures: three focused on medication taking, three on diet, one on physical activity, one on SMBG, and one on oral care. Most (22 of 30) were developed within the last 10 years.
Table 1.
Self-Report Instruments Used to Measure Self-Care Behaviors of Persons With Type 2 Diabetes Mellitus (T2DM).
| Name | Content areas | # Items | Response Format | Validity | Reliability | Studies, Authors, (Publication Year) |
|---|---|---|---|---|---|---|
| Adherence and Self-Management Monitoring Tool (ASMMT) | Medication and SMBG | 16 | — | Face and content validites | — | Yusuff, Obe, and Joseph (2008) |
| Adherence to Therapeutic Regimen | Medication, exercise, diet, foot care, and SMBG | 68 | 5-point Likert-type | Content validity | Test–retest reliability: .90 | Nesari, Zakerimoghadam, Rajab, Bassampour, and Faghihzadeh (2010) |
| A scale for patients’ assessment of their diabetes self-management | Taking medications, exercising, following an eating plan, SMBG, and foot care | 20 | 5-point Likert-type | Criterion validity: p < .05 (HbA1c), concurrent validity: p < .05 (receipt of necessary diabetes services) | Internal consistency: Cronbach’s α = .68 | Heisler, Smith, Hayward, Krein, and Kerr (2003) |
| Diabetes Care Profile (DCP) | Self-care adherence and diet adherence | 8 | 5-point Likert-type | Criterion validity: r = .28/0.15 (GHb), concurrent validity: r = −.35 (CES-D), r = .23 (social provisions scale), r = .23 (happiness and satisfaction scale) | Internal consistency: Cronbach’s α = .70–.87 (community), .70–.89 (medical center) | Fitzgerald, Davis, et al. (1996) |
| — | Internal consistency: Cronbach’s α = .74–.85 | Fitzgerald, Anderson, et al. (1998) | ||||
| Criterion validity: r = .24/.17 (HbA1c), convergent validity: r = −.43/.13 (Beck Depression Inventory, BDI) r = .19/.29 (Diabetes Family Behavior Checklist, DFBC) | Internal consistency: Cronbach’s α = .58–.76 | Cunningham et al. (2005) | ||||
| — | Internal consistency: Cronbach’s α = .68–.86 | Chasens, Korytkowski, Sereika, and Burke (2013) | ||||
| Diabetes Health Promotion Self-Care Scale (DHPSC) | Interpersonal relationships, diet, SMBG, personal health responsibility, exercise, adherence to the recommended regimens, and foot care | 26 | 5-point Likert-type | Content validity: reviewed by experts, CVI = .94, construct validity: 7 factors accounted for 69.31% of the total variance, concurrent validity: r = .14–.39 (satisfaction subscales of Diabetes Quality of Life), r = .23–.49 (Diabetes Empowerment Scale), r =.10 (HbA1c) | Internal consistency: Cronbach’s α = .78–.94, Item-total correlations: .30–.70 (except for 3 items from the adherence to recommended regimens subscale and 1 item from the foot care subscale), test–retest reliability: ICC = .76–.95 | Wang (2012) |
| Diabetes Self-Care Ability Questionnaire (DSCAQ) | Diet, exercise and activity, SMBG, information and follow-up, hygiene and foot care, and medication-taking routine | 36 | 4-point Likert-type | — | Internal consistency: Cronbach’s α = .83 | Partiprajak, Hanucharurnkul, Piaseu, Brooten, and Nityasuddhi (2011) |
| — | Internal consistency: Cronbach’s α = .87 | Mekwiwatanawong, Hanucharurnkul, Piaseu, and Nityasuddhi (2013) | ||||
| Diabetes Self-management Assessment Report Tool (D-SMART) | Exercise, eating, medication, SMBG, problem solving, barriers to diabetes self-management and living with diabetes | 49 | 4–5-point Likert-type | — | Internal consistency: Cronbach’s α = .65–.80, test–retest reliability: ICC = .83–.89 | Fain (2007) |
| Diabetes Self-Management Instrument (DSMI) | SMBG, self-integration, self-regulation, interaction with providers, and adherence | 35 | 4-point Likert-type | CVI = .90, construct validity: 5 factors accounted for 46% of the total variance | Internal consistency: Cronbach’s α = .94, interitem correlation: .30–.70, test–retest reliability: .73 | Lin, Anderson, Chang, Hagerty, and Loveland-Cherry (2008) |
| Diabetes Self-Management Scale (DSMS) | SMBG, exercise, diet, glucose monitoring, problem solving, and reducing risks | 60 | 5-point Likert-type | CVI = 0.70–1.00 | — | Sousa, Hartman, Miller, and Carroll (2009) |
| Diabetes Self-Care Scale (DSCS) | — | 35 | 6-point Likert-type | Construct validity: 3 factors accounted for 67.2% of the total variance; the meaningfulness of the item endorsability order and the consistency of that order across respondent supported construct validity | Internal consistency: respondent separation reliability = .80, item separation reliability = .99 | N. Lee and Fisher (2005) |
| DSCS(Turkey) | 4-point Likert-type | — | Internal consistency: Cronbach’s α = 0.70 | Karakurt and Kasikci (2012) | ||
| Modified Insulin Management Diabetes, Self-Care Scale (M-IMDSCS) | Medication, exercise, diet, and general management | 30 | 6-point Likert-type | Divergent validity: r = −.37 (HbA1c), r = .83 (self-efficacy) | Internal consistency: Cronbach’s α = .73–.90 | Ludlow and Gein (1995) |
| Diabetes Self-Care Scale (DSC) (Chinese) | Medication, exercise, diet, SMBG, foot care, and prevention of unstable blood sugar | 27 | 5-point Likert-type | — | Internal consistency: Cronbach’s α = .88, test–retest reliability: .91 | Bai, Chiou, and Chang (2009) |
| — | Internal consistency: Cronbach’s α = .90 | Kang et al. (2010) | ||||
| Content validity, construct validity: 6 factors accounted for 74% of the total variance; criterion validity: r = .11 (HbA1c) | Internal consistency: Cronbach’s α = .81, test–retest reliability: ICC = .83 | Wang, Wu, and Hsu (2011) | ||||
| — | Internal consistency: Cronbach’s α = .94 | Huang, Hung, Stocker, and Lin (2013) | ||||
| Disease-Specific Adherence Scale for Diabetes | Following a low-fat or weight loss diet, following a diabetic diet, taking prescribed medications, checking blood for sugar, exercising regularly, checking feet for minor injuries, carrying something with sugar in it, carrying medical supplies for self-care | 8 | 6-point Likert-type | Criterion validity: r = −.33 (blood glucose level), r = −.25 (HbA1c) | Internal consistency: Cronbach’s α = .69 | Kravitz et al. (1993) |
| — | Internal consistency: Cronbach’s α = .61 | Y. Y. Lee and Lin (2009) | ||||
| Revised Adherence in Diabetes Questionnaire (RADQ) | Diet, exercise, medicine, SMBG, and frequency of reexaminations | 10 | 4-point Likert-type | — | Internal consistency: Cronbach’s α = .87 | Zhang et al. (2013) |
| Self-Care Activity Questionnaire | Medication, exercise, diet, and SMBG | 45 | 5–7 point Likert-type, Yes/No | Content validity | Internal consistency: Cronbach’s α = .69–.76 | Tan and Magarey (2008) |
| Self-Care Behavior Scale | Exercise, diet, medication and SMBG, self-care of feet, and prevention of high, and low blood glucose | 26 | 5-point Likert-type | — | Internal consistency: Cronbach’s α = .92 | Huang and Hung (2007) |
| Self-Care Inventory (SCI) | Internal consistency: Cronbach’s α = .53–.81 | Polonsky et al. (1995) | ||||
| SCI-R | Diet, SMBG, medication administration, exercise, low glucose levels, preventive/routine aspects of self-care | 15 | 5-point Likert-type | Content validity, concurrent validity: r = .63 (SDSCA), convergent validity: r = −.37 (HbA1c), r = −.37 (PAID) r = −.30 (perceived barriers to diabetes subscale) r = .25 (self-esteem), r = .47 (self-efficacy), r = −.36 (diabetes-related emotional distress), Construct validity: a large general factor | Internal consistency: Cronbach’s α = 0.87, item-to-total correlations: .34–.67 | Weinger, Welch, Butler, and La Greca (2005) |
| Internal consistency: Cronbach’s α = .85 | Ogbera and Adeyemi-Doro (2011) | |||||
| Adherence to Self-Care Behaviors Questionnaire | Regular clinic attendance, blood tests, medication and/or insulin use, sticking to the recommended diet, and regular physical activity | 10 | 5-point Likert-type | Construct validity: 1 factor model | Internal consistency: Cronbach’s α = .75 | Cohen and Kanter (2004) |
| Summary of Diabetes Self-Care Activities (SDSCA) | Medication, exercise, diet, and SMBG | 12 | 4–7 point Likert-type | construct validity: three-factor explained 67.6% of the variance | Internal consistency: Cronbach’s α = .74 (diet), .85 (exercise), and .75 (SMBG) | Talbot, Nouwen, Gingras, Gosselin, and Audet (1997) |
| Internal consistency: Cronbach’s α = .71 | Gallegos, Ovalle-Berumen, and Vinicio Gomez-Meza (2006) | |||||
| Internal consistency: Cronbach’s α = .71 (diet) and .84(exercise) | Bean, Cundy, and Petrie (2007) | |||||
| Diet | Internal consistency: Cronbach’s α = .68, test–retest reliability: ICC = .73 | Nouwen et al. (2011) | ||||
| SDSCA-revised | Medication, exercise, diet, SMBG, foot care, and smoking | 11 core and 14 optional items | 7-point Likert-type | Internal consistency: Cronbach’s α = .62, item-to-total correlations: .11–.63 | Weinger et al. (2005) | |
| Internal consistency: Cronbach’s α = .80 | Sacco et al. (2007) | |||||
| Internal consistency: Cronbach’s α = .62 | Costa, Pereira, and Pedras (2012) | |||||
| Internal consistency: Cronbach’s α = .61 | Kroese, Adriaanse, and De Ridder (2012) | |||||
| Internal consistency: Cronbach’s α = .65 | Kroese, Adriaanse, Vinkers, van de Schoot, and de Ridder (2014) | |||||
| Diet and exercise | Internal consistency: Cronbach’s α = .67–.89 | Janzen Claude, Hadjistavropoulos, and Friesen, (2014) | ||||
| Diet and exercise | Construct validity: factor analysis yielding two factors | Internal consistency: Cronbach’s α = .65 (exercise)/.75 (diet) | Oftedal, Bru, and Karlsen (2011) | |||
| Diet, exercise, and SMBG | Inter-item correlations: >.56 | Sultan, Attali, Gilberg, Zenasni, and Hartemann (2011) | ||||
| Diet, exercise, and SMBG | Internal consistency: Cronbach’s α = .70–.72 | Trouilloud and Regnier (2013) | ||||
| SDSCA (Chinese Mainland) | 8–25 | 7-point Likert-type | Construct validity: five factors accounted for 91% | Internal consistency: Cronbach’s α = .68, inter-item correlation: .69–.77 | Xu, Savage, Toobert, Wei, and Whitmer (2008) | |
| CVI = .91 | Internal consistency: Cronbach’s α = .83 | Shi, Ostwald, and Wang (2010) | ||||
| — | Internal consistency: Cronbach’s α = .82 | Gao et al. (2013) | ||||
| SDSCA (Chinese Hong Kong) | CVI = .80; Construct validity: eight-factor model | Internal consistency: Cronbach’s α = .62–.98 | Tang, Pang, Chan, Yeung, and Yeung (2008) | |||
| SDSCA (Chinese Taiwan) | — | Internal consistency: Cronbach’s α = .70–.86 | Vivienne Wu et al. (2008), Wu, Courtney, et al. (2007), and Wu, Huang, et al. (2011) | |||
| SDSCA (Korean) | 9 | 7-point Likert-type | Construct validity: four factors explained 64% of total variance. Concurrent validity: r = −.43 (Diabetes Management Self-Efficacy Scale) | Internal consistency: Cronbach’s α = .69 | Choi et al. (2011) | |
| SDSCA (Turkish) | 12 | 7-point Likert-type | Construct validity: factor analysis yielding six factors | Internal consistency: Cronbach’s α = .46–.93 | Kav et al. (2010) | |
| Content validity: CVI = .97 | Internal consistency: Cronbach’s α = .59–.94 | Cosansu and Erdogan (2014) | ||||
| SDSCA (Thailand) | Content validity | Item-total correlation = .43, test–retest reliability: .89 | Keeratiyutawong, Hanucharurnkul, Eramo Melkus, Panpakdee, and Vorapongsathorn (2006) | |||
| — | Internal consistency: Cronbach’s α = .57 (diet)/.94 (medication) | Sowattanangoon, Kochabhakdi, and Petrie (2008) | ||||
| — | Internal consistency: Cronbach’s α = .73 | Nyunt, Howteerakul, Suwannapong, and Rajatanun (2010) | ||||
| — | Internal consistency: Cronbach’s α = .73 | Navicharem (2012) | ||||
| SDSCA (Arabic) | Content validity | — | Jarab, Alqudah, Mukattash, Shattat, and Al-Qirim (2012) | |||
| SDSCA (Maltese) | — | Internal consistency: Cronbach’s α = .50 | Gatt & Sammut (2008) | |||
| SDSCA (Portuguese) | Content validity | Internal consistency: Cronbach’s α = .57 (diet) | Gucciardi, Demelo, Lee, and Grace (2007) | |||
| Diabetes Self-Care Activity Questionnaire (Greek) | Sociodemographic, risk factors, physical and mental health, physician–patient communication, self-care activities, self-care recommendations, and compliance with medical orders | 38 | Content validity, convergent validity: r = .768–.876 (Habit, Attitudes and Knowledge questionnaire); Discriminant validity | Internal consistency: Cronbach’s α = .83, test–retest reliability: ICC = .90 | Intas et al. (2012) | |
| The Diabetes Activities Questionnaire (TDAQ) | Lifestyle, monitoring, and treatment | 13 | Visual analogue scale | Content validity, construct validity: two-factor model | Internal consistency: Cronbach’s α = .82, test–retest reliability: .78, item-total correlation: >.30 (except for 2 items) | Hernandez (1997) |
| Cronbach’s α = .84 | Chlebowy and Garvin (2006) | |||||
| DSBQ | Diet | 89 | 5-point Likert-type | — | Internal consistency: Cronbach’s α = .55–.81 | Taru, Tsutou, Nakawatase, Usami, and Miyawaki (2008) |
| Kristal Food Habits Questionnaire | Diet | 20 | — | — | Internal consistency: Cronbach’s α = .67 | Kroese, Adriaanse, Vinkers, et al. (2014) |
| Modified version of Dobson’s 17-item Short Fat Questionnaire | Diet | — | — | — | Internal consistency: Cronbach’s α = .82 | Clarke (2009) |
| Evaluation Scale for Self-Management, Behavior related to Physical Activity of T2DM (ES-SMBPA-2D) | Physical activity | 38 | 5-point Likert-type | Content validity, construct validity: Factor analysis, criterion validity: r = .14–.16 (IPAQ) | Internal consistency: Cronbach’s α = .56–.90, test–retest reliability: .60–.88 | Nakawatase et al. (2007) |
| Medication Adherence Report Scale (MARS) | Medication | 5 | 5-point Likert-type | — | Internal consistency: Cronbach’s α = .79 | Barnes, Moss-Morris, and Kaufusi (2004) |
| — | Internal consistency: Cronbach’s α = .97 | Clarke (2009) | ||||
| — | Internal consistency: Cronbach’s α = .79 | Aflakseir (2012) | ||||
| — | Internal consistency: Cronbach’s α = .65–.75 | Kroese, Adriaanse, et al. (2012) | ||||
| — | Internal consistency: Cronbach’s α = .83 | Kroese, Adriaanse, Vinkers, et al. (2014) | ||||
| Measurement of Adherence to Treatment (MAT) | Oral Antidiabetics (MAT OADs), Insulin Therapy (MAT insulin) | 14 | 6-point Likert-type | Content validity, criterion-related validity: ROC curves: .83 (MAT OADs), .77 (MAT insulin), sensitivity: .84 (MAT OADs), .60 (MAT insulin), specificity: .35 (MAT OADs), .21 (MAT insulin) | Internal consistency: Cronbach’s α = .84 (MAT OADs), .68 (MAT insulin), item-total correlation: .38–.77(MAT OADs), .20–.53(MAT insulin) | Boas, Lima, & Pace (2014) |
| Morisky Medication Adherence Scale (MMAS-4 item) | 4 | Yes/no | — | Internal consistency: Cronbach’s α = .54 | Parada, Horton, Cherrington, Ibarra, and Ayala (2012) | |
| MMAS-4 item (Chinese) | Content validity, construct validity: one-factor model, convergent validity: association with HbA1c and adherence to diet and physical exercise | Internal consistency: Cronbach’s α = .62 | Wang (2012) | |||
| MMAS-4 item (Arabic) | Content and face validity | — | Jarab et al. (2012) | |||
| MMAS-8 item (Malaysian) | Medication adherence | 8 | Yes/No 5-point Likert-type | Convergent validity: r = .79 (original MMAS), r = −.43 (HbA1c), sensitivity: 78%, specificity: 45% | Internal consistency: Cronbach’s α = .68, test–retest reliability: .82 | Al-Qazaz et al. (2010) |
| MMAS-8 item (Korean) | Medication adherence | 8 | Yes/No 5-point Likert-type | Convergent validity: r = .88 (original MMAS), construct validity: three-factor model explaining 62.4% of the total variance, OR = 2(1.21–3.36; HbA1c), sensitivity (74.1%), specificity (38.3%) | Internal consistency: Cronbach’s α = .66, item-total correlation: .23–.66, test–retest reliability: ICC = .79 | W. Y. Lee et al. (2013) |
| MMAS-8 item (Thai) | Medication adherence | 8 | Yes/No 5-point Likert-type | Convergent validity: r = .77 (3-item MMAS), r = .57 (medication adherence visual analog scale), OR = 1.84 (HbA1c), construct validity: factor analysis, sensitivity (51%), specificity (64%) | Internal consistency: Cronbach’s α = .61, test–retest reliability: .83 | Sakthong, Chabunthom, and Charoenvisuthiwongs (2009) |
| MMAS-8 item (Iran/Persian) | Medication adherence | 8 | Yes/No, 5-point Likert-type | Content validity | Internal consistency: Cronbach’s α: > .70, test–retest reliability: ICC = .8 | Negarandeh, Mahmoodi, Noktehdan, Heshmat, and Shakibazadeh (2013) |
| A scale to measure adherence to self-monitoring of blood glucose | SMBG | 15 | 9-point Likert-type | Content validity, Construct validity: two factors accounted for 43.2% of variance | Internal consistency: Cronbach’s α = .84 | Wagner, Schnoll, and Gipson (1998) |
| The UISESS-B scale | Oral care | 35 | 3-point Likert-type | Content validity, construct validity: 68.85% of variance (habits subscale), 62.29% of variance (self-perception subscale), convergent validity: r = .70 (CPO: a worldwide oral health scale) | Internal consistency: Cronbach’s α = .78–.84, test–retest reliability: ICC = .64–.73 | Salcedo-Rocha, Garcia-de-Alba-Garcia, Velasquez-Herrera, and Barba-Gonzalez (2011) |
Note. OR = odds ratio; SMBG = self-monitoring of blood glucose; ICC = Intraclass correlation coefficient; PAID = Problem Areas in Diabetes Scale; IPAQ = International Physical Activity Questionnaire; ROC = Receiver Operating Characteristics.
Of the 30 instruments, 8 were translated or revised versions of an original instruments, another 4 (Medication Adherence Report Scale [MARS], Morisky Medication Adherence Scale [MMAS], UISESS-B and Kristal Food Habits Questionnaire) were not specific to diabetes and were used in other chronic illness fields, and the remaining were original instruments on T2DM self-care. Only 10 of the 30 instruments were used more than once. The shortest instrument (MMAS) had 4 items and the longest (Diet Self-Management Behavior Questionnaire [DSBQ]) had 89 items. Response formats included dichotomous (yes/no) or Likert-type (from 4- to 9-point). Only 19 of the 30 instruments had both reliability and validity information, though two of them simply tested content validity by expert review.
Of the 30 instruments, a full list of items was available for 15 instruments, of which 1 (Diabetes Care Profile) was available on the Internet (Michigan Diabetes Research and Training Center, 2014). In addition, a portion of the items of five instruments was available in the included articles. Although every effort was made to get a comprehensive list of the items, none of the authors for the other 10 instruments could be contacted, because of either missing or outdated contact details or nonresponse. Nevertheless, all 30 instruments were included in this review to provide a comprehensive description of instruments for assessing self-care in persons with T2DM. In the following section, each of the 30 instruments measuring T2DM self-care is critically reviewed and summarized in the order of multidimensional measures followed by the unidimensional instruments (see Table 2).
Table 2.
Example Items used in the Self-Report of T2DM Self-Care Behaviors.
| Source | Item examples | Responses | Time frame |
|---|---|---|---|
| Domain—Diet | |||
| DCP (Fitzgerald, Davis, et al., 1996) | How often do you follow a meal plan or diet? How often do you weight or measure your food? |
Never Always |
— |
| DHPSC (Wang, Lin, Cheng, Hsu, and Kao, 2012) | I follow the rules of diet control for diabetes when having a meal out or in an unfamiliar setting | Never—Always | — |
| DSCAQ (Mekwiwatanawong, Hanucharurnkul, Piaseu, and Nityasuddhi, 2013; Partiprajak, Hanucharurnkul, Piaseu, Brooten, and Nityasuddhi, 2011) | How often do you eat desserts between meals? | Rarely/never—Always | Within a week |
| DSMI (Lin, Anderson, Chang, Hagerty, and Loveland-Cherry, 2008) | I consider effect on blood sugar when making food choices | Never—Always | — |
| DSMS (Sousa, Hartman, Miller, and Carroll, 2009) | I eat at least three meals every day | Strongly disagree—strongly agree | — |
| DSCS (N. Lee and Fisher, 2005) | I stay on diet when I eat at restaurants I stay on my diet when I go to parties |
Strongly disagree Strongly agree |
— |
| Disease-Specific Adherence Scale for Diabetes (Kravitz et al., 1993; Y. Y. Lee and Lin, 2009) | How often have you followed a low-fat or weight-loss diet? How often have you followed a diabetic diet? |
None of the time— All of the time |
Past 4 weeks |
| Self-Care Activity Questionnaire (Tan and Magarey, 2008) | Last week, each time when you ate your sweetened food or drinks, did you reduce your intake of carbohydrate food during meals? | Never—All the time | — |
| SDSCA (Toobert, Hampson, and Glasgow, 2000) | How often did you follow your recommended diet over the last 7 days? What percentage of time did you successfully limit your calories as recommended in health eating for diabetes control? Last week, how many meals did you eat each day including snacks? |
Always—Never 0–100% 1–7 or more |
Previous 7 days Last week |
| TDAQ (Hernandez, 1997) | I follow my meal plan exactly as suggested by my dietitian. | Never—Always | — |
| DSBQ (Taru, Tsutou, Nakawatase, Usami, and Miyawaki, 2008) | I use 50–100 g servings of meat or fish for a single meal I eat more vegetable fat than animal fat I prepare dishes to make them more attractive and appealing to the eye |
Never Always |
— |
| Kristal Food Habits Questionnaire (Kroese, Adriaanse, Vinkers, et al., 2014) | When you eat chicken, how often has it been fried How often do you use fat-free diary products? |
— | — |
| Domain—Physical activity | |||
| DCP (Fitzgerald, Davis, et al., 1996) | How often do you have trouble getting enough exercise because it takes too much effort? How often do you have trouble getting enough exercise because you have a health problem? |
Rarely Often |
— |
| DHPSC (Wang, Lin, Cheng, Hsu, and Kao, 2012) | I keep exercising regularly | Never—Always | — |
| DSCAQ (Mekwiwatanawong, Hanucharurnkul, Piaseu, and Nityasuddhi, 2013; Partiprajak, Hanucharurnkul, Piaseu, Brooten, and Nityasuddhi, 2011) | How often do you exercise until you sweat for at least 30 minutes? | Rarely/never—Always | Within a week |
| D-SMART (Fain, 2007) | How often have you exercised for at least 20 minutes per day in the past 3 months? | — | Past 3 months |
| DSMI (Lin, Anderson, Chang, Hagerty, and Loveland-Cherry, 2008) | I exercise to control blood sugar and weight. | Never—Always | — |
| DSCS (N. Lee and Fisher, 2005) | I exercise regularly. I get enough exercise | Strongly disagree—Strongly agree | — |
| Disease-Specific Adherence Scale for Diabetes (Kravitz et al., 1993; Y. Y. Lee and Lin, 2009) | How often have you exercised regularly? | None of the time—All of the time | Past 4 weeks |
| Self-Care Activity Questionnaire (Tan and Magarey, 2008) | How much time do you spend sitting/standing/walking? How often do you read book/magazine/newspaper, watch TV, play or work on a computer during your leisure hours? |
Almost all the time—Almost none of the time All the time-Never |
Last week — |
| SDSCA (Toobert, Hampson, and Glasgow, 2000) | On how many of the last 7 days did you participate in at least 20 minutes of physical exercise? | 0–7 | Previous 7 days |
| TDAQ (Hernandez, 1997) | I exercise as often as my educator advised me to I only do exercises/activities recommended by my educator |
Never Always |
— |
| ES-SMBPA-2D (Nakawatase et al., 2007) | Doing the housework oneself instead of asking someone else to do it Making detours when going somewhere |
Never Always |
— |
| Domain—SMBG | |||
| DHPSC (Wang, Lin, Cheng, Hsu, and Kao, 2012) | I measure blood glucose or urine glucose according to the suggestions of health care providers | Never—Always | — |
| DSMI (Lin, Anderson, Chang, Hagerty, and Loveland-Cherry, 2008) | I test blood sugar when feel sick I test blood sugar to help make diabetes self-care decisions |
Never Always |
— |
| DSCS (N. Lee and Fisher, 2005) | I test my blood sugar | Strongly disagree—Strongly agree | — |
| Disease-Specific Adherence Scale for Diabetes (Kravitz et al., 1993; Y. Y. Lee and Lin, 2009) | How often have you checked your blood for sugar? | None of the time—All of the time | Past 4 weeks |
| Self-Care Activity Questionnaire (Tan and Magarey, 2008) | Last week, how many times did you change your treatment plan like modify your diet intake or physical activity or medicine based on your blood glucose reading(s)? | 0–7 or more | Last week |
| SDSCA (Toobert, Hampson, and Glasgow, 2000) | On how many of the last 7 days (that you were not sick) did you test your glucose (blood sugar) level? | Every day—None of the days | Previous 7 days |
| TDAQ (Hernandez, 1997) | I test my blood sugar at the times suggested by my educator | Never—Always | — |
| Domain—Medication/regimen | |||
| DHPSC (Wang, Lin, Cheng, Hsu, and Kao, 2012) | I take diabetic medicine on time even when out | Never—Always | — |
| DSMI (Lin, Anderson, Chang, Hagerty, and Loveland-Cherry, 2008) | I take medications at the prescribed times I take prescribed amount of medicine |
Never Always |
— |
| DSCS (N. Lee and Fisher, 2005) | I take my diabetes pills as ordered I adjust my insulin dosage according to my blood sugar |
Strongly disagree Strongly agree |
— |
| Disease-Specific Adherence Scale for Diabetes (Kravitz et al., 1993; Y. Y. Lee and Lin, 2009) | How often have you taken prescribed medication? | None of the time—All of the time | Past 4 weeks |
| Self-Care Activity Questionnaire (Tan and Magarey, 2008) | Last week, how many times did you need help in taking your diabetes medicine(s)? | 0–7 or more | Last week |
| SDSCA (Toobert, Hampson, and Glasgow, 2000) | How many of your recommended insulin injections did you take that you were supposed to? | All of them—I do not take injections | Previous 7 days |
| TDAQ (Hernandez, 1997) | I only adjust the dose of my insulin/pills if my educator tells me to | Never—Always | — |
| MARS (Kroese, Adriaanse, et al., 2012) | Some people forget to take their medicines. How often does this happen to you? Some people miss out a dose of their medications or adjust it to suit their own needs. How often do you do this? |
Always true Never true |
— |
| MAT (Boas, Lima, and Pace, 2014) | Have you ever forgotten to take the tablets/administer the insulin for the diabetes? Have you ever not taken the tablets/administered the insulin for the diabetes because of feeling better? |
Always Never |
— |
| MMAS (Parada, Horton, Cherrington, Ibarra, and Ayala, 2012; W. Y. Lee et al., 2013) | Stop taking medications when feeling worse? Stop taking medications when well controlled? How often do you have difficulty remembering to take medications? |
Yes/No Yes/No 5-point Likert-type |
— |
| A scale to measure adherence to self-monitoring of blood glucose (Wagner, Schnoll, and Gipson, 1998) | If I feel my blood sugar is low, I test When I am sick, I test |
Lower adherence Greater adherence |
— |
| Domain—Foot care | |||
| DHPSC (Wang, Lin, Cheng, Hsu, and Kao, 2012) | I wear appropriate shoes and socks when out or traveling | Never—Always | — |
| DSCAQ (Mekwiwatanawong, Hanucharurnkul, Piaseu, and Nityasuddhi, 2013; Partiprajak, Hanucharurnkul, Piaseu, Brooten, and Nityasuddhi, 2011) | How often do you examine your feet? | Rarely/never—Always | Within a week |
| DSMS (Sousa, Hartman, Miller, and Carroll, 2009) | I wear closed-toe shoes every time I am outside my home | Strongly disagree—strongly agree | — |
| DSCS (N. Lee and Fisher, 2005) | I routinely wear socks I keep my toenails trimmed |
Strongly disagree Strongly agree |
— |
| Disease-Specific Adherence Scale for Diabetes (Kravitz et al., 1993; Y. Y. Lee and Lin, 2009) | How often have you checked your feet for minor bruises, injuries, and ingrown toenails? | None of the time All of the time |
Past 4 weeks |
| SDSCA (Toobert, Hampson, and Glasgow, 2000) | On how many of the last seven days did you wash your feet? | 0–7 | Last 7 days |
| TDAQ (Hernandez, 1997) | I examine my feet daily | Never—Always | — |
| Domain—Management of hypoglycemia | |||
| DSMI(Lin, Anderson, Chang, Hagerty, and Loveland-Cherry, 2008) | I make decisions based on experience I treat low blood sugar reactions |
Never—Always | — |
| DSCS (N. Lee and Fisher, 2005) | I take candies or sugar tablets when my blood sugar is low I take candies or sugar tablets when I am away from home |
Strongly disagree Strongly agree |
— |
| Disease-Specific Adherence Scale for Diabetes (Kravitz et al., 1993; Y. Y. Lee and Lin, 2009) | How often have you carried something with sugar in it (a source of glucose) for emergencies when outside your home? | None of the time—All of the time | Past 4 weeks |
| TDAQ (Hernandez, 1997) | I When I have a reaction I only eat/drink the amount suggested by my educator Domain—Management of oral care Item Examples |
Never—Always | — |
| UISESS-B (Salcedo- Rocha, Garcia-de- Alba-Garcia, Velasquez-Herrera, and Barba-Gonzalez, 2011) | I take much water to avoid dryness I wash my teeth after meals |
Never—Always | — |
| Domain—Interaction with health professionals and significant others | |||
| DHPSC (Wang, Lin, Cheng, Hsu, and Kao, 2012) | I find ways to satisfy the needs of intimate relationships I express care, love, and warmth to others |
Never Always |
— |
| DSCAQ (Mekwiwatanawong, Hanucharurnkul, Piaseu, and Nityasuddhi, 2013; Partiprajak, Hanucharurnkul, Piaseu, Brooten, and Nityasuddhi, 2011) | How often do you ask health care providers about your medical problems, treatments, and self-care activities? | Rarely/never—Always | Within a week |
| DSMI (Lin, Anderson, Chang, Hagerty, and Loveland-Cherry, 2008) | Comfortable discussing degree of flexibility in treatment plan with health care provider Comfortable asking others for diabetes management tips |
Never Always |
— |
| DSCS (N. Lee and Fisher, 2005) | I ask health care provider(s) about how to prevent complications I consult my doctor when my blood sugar is low |
Strongly disagree Strongly agree |
— |
Multidimensional Instruments
Adherence and self-management monitoring tool (ASMMT)
The ASMMT—a 16-item questionnaire developed in Nigeria (Yusuff, Obe, & Joseph, 2008)—focuses mainly on patients’ experience with SMBG, optimal blood glucose target, and prevention of complications from poor glycemic control. No example items are available. The only forms of tested psychometric properties were face and content validities. Due to very limited information on the instrument’s characteristics such as unknown domain categories, response format, scoring method, and psychometric testing, it is difficult to judge whether the ASMMT is an appropriate tool to measure diabetes self-care behavior.
Adherence to the therapeutic regimen
This scale—developed for an Iranian intervention study to determine the effect of telephone follow-up calls on adherence to diabetes therapeutic regimens (Nesari, Zakerimoghadam, Rajab, Bassampour, & Faghihzadeh, 2010)—consists of 68 items on a 5-point Likert-type scale: diet (27 items), exercise (18 items), foot care (15 items), medication taking (7 items), and SMBG (1 item). No further item information is available. The total score of each domain was accumulated individually and converted into a percentage. Content validity by a panel of experts was the only form of validity tested. The test–retest reliability was acceptable, with a coefficient of .9. This instrument was used only once in a small sample (N = 61) in Iran; hence, the application in other ethnicities is questionable. The long list of items may also preclude its use in busy clinical settings.
A scale for patients’ assessment of their diabetes self-management
Heisler, Smith, Hayward, Krein, and Kerr (2003) used a 20-item scale for patients’ assessment of their diabetes self-management over the past year (How difficult has it been for you to do each of the following exactly as the doctor who takes care of your diabetes suggested?) in the following five areas: medication taking, exercise, diet, SMBG, and foot care. The items were rated on a 5-point Likert-type scale from “So difficult that I couldn’t do it at all” to “Not difficult, I got it exactly right.” Higher scores indicate greater treatment adherence. The internal consistency reliability coefficient was lower than the acceptable cutoff of .70. The validity was tested by showing those with higher scores on the scale having a significantly lower glycosylated hemoglobin (HbA1c) and receipt of necessary diabetes services (Heisler, Smith, Hayward, Krein, & Kerr, 2003). This scale was used only once in a sample of Veterans’ Affairs persons with diabetes. Its application to other populations warrants appropriate validation.
Diabetes Care Profile
The Diabetes Care Profile (DCP) is a standardized self-administered instrument developed by Michigan Diabetes Research and Training Center for comprehensive assessment of social, psychological, and therapeutic aspects of diabetes (Fitzgerald, Davis, et al., 1996). Two of the 16 DCP subscales are related to adherence to treatment regimen, including Self-Care Adherence in relation to SMBG, weight control, medication, and exercise (4 items) and the Diet Adherence (4 items). An example item includes “How often do you follow a meal plan or diet?” The DCP’s psychometric properties were originally established in two separate studies conducted in a community setting and a medical center, with similar reliability coefficients at or greater than the acceptable level (Fitzgerald, Davis, et al., 1996). The relationships between DCP and HbA1c and several previously validated scales (e.g., the Center for Epidemiologic Studies Depression Scale) also support its validity (Fitzgerald, Davis, et al., 1996). The DCP has been tested in multiple ethnic groups such as Caucasian, Hispanic, and African Americans (Chasens, Korytkowski, Sereika, & Burke, 2013; Cunningham et al., 2005; Fitzgerald, Anderson, et al., 1998; Fitzgerald, Davis, et al., 1996). Although it includes evidence of reliability and validity in varying ethnicities and settings, the DCP does not address a full scope of self-care behaviors that are important to T2DM control such as foot care.
Diabetes Health Promotion Self-Care Scale
The Diabetes Health Promotion Self-Care Scale (DHPSC) is a 26-item multidimensional instrument developed in Taiwan (Y. Wang, Lin, Cheng, Hsu, & Kao, 2012). The authors conceptualized diabetes self-care as a set of behaviors performed by persons with T2DM to improve their physical and psychosocial well-being. The DHPSC consists of seven subscales, namely, interpersonal relationships, diet, SMBG, personal health responsibility, exercise, adherence to treatment regimen, and foot care. Example items include “I find ways to satisfy the needs of intimate relationships” and “I follow the rules of diet control when having meals.” Psychometric testing was done using internal consistency; item-total correlations; test–retest reliability; and content, construct, and concurrent validities—all with generally adequate values. The original validation was done in Taiwanese patients in Chinese, hence limiting the generalization beyond the language group. Further validation in different populations in different countries is warranted before the DHPSC can be used widely.
Diabetes Self-Care Ability Questionnaire
The Diabetes Self-Care Ability Questionnaire (DSCAQ)—developed in Thailand (Mekwiwatanawong, Hanucharurnkul, Piaseu, & Nityasuddhi, 2013; Partiprajak, Hanucharurnkul, Piaseu, Brooten, & Nityasuddhi, 2011)—includes 36 items covering 6 domains: diet, exercise, SMBG, information and follow-up, hygiene and foot care, and medication taking. Example items include “How often do you examine your feet?” and “How often do you exercise until you sweat for at least 30 minutes?” Responses are graded on a 4-point Likert-type scale ranging from 0 (rarely to never done) to 3 (always). A higher total score indicates a higher ability to perform diabetes self-care, categorized as low (0 ~ 35.99), moderate (36 ~ 71.99), and high (72 ~ 108). The content validity was cited with an index of .83. The internal reliability coefficients ranged from .83 to .87 (Mekwiwatanawong et al., 2013; Partiprajak et al., 2011). Considering that the tool was developed and used exclusively in Thailand and that there were no other forms of validation (except for content validity) done, its application to other cultural and linguistic groups is questionable.
Diabetes Self-Management Assessment Report Tool
Diabetes Self-Management Assessment Report Tool (D-SMART) is a 49-item tool to assess self-care behavior, priorities for behavior change, and barriers to making appropriate behavior change (Charron-Prochownik et al., 2007; Fain, 2007). It was developed by the American Association of Diabetes Educators to guide diabetes educators in facilitating patient behavior change. D-SMART contains seven areas, five of which focus on self-care behaviors: exercise, eating, medication, SMBG, and problem solving. The remaining items focus on barriers to diabetes self-management and living with diabetes (“How much does diabetes interfere with your job, school, or daily activities?”). The wording of questions and selection of answers were deemed satisfactory (Charron-Prochownik et al., 2007). The tool was adapted and tested in Spanish. Only the internal consistency (.65–.80) and test–retest reliability coefficients (.83–.89) were reported in the subscales of barriers to diabetes self-management and living with diabetes (Fain, 2007); however, no validity testing was done, limiting the utility of the instrument in samples beyond the original development sample. In addition, the large number of items may not be practical for use in clinical settings.
Diabetes Self-Management Instrument
The Diabetes Self-Management Instrument (DSMI)—a 35-item scale developed to measure self-management of adults with T2DM—was validated in a Taiwanese population sample (N = 634; Lin, Anderson, Chang, Hagerty, & Loveland-Cherry, 2008). The author conceptualized diabetes self-management as an active, flexible process in which patients develop strategies for achieving desired goals by regulating their own actions, collaborating with health care providers and significant others. An example item includes “I exercise to control blood sugar and weight.” Content, face, and construct validities as well as internal consistency and test–retest reliability were reported. Exploratory and confirmatory factor analyses both provided the support of a five-factor model, including “self-integration,” “self-regulation,” “interaction with health professionals and significant others,” “SMBG,” and “adherence to recommended regimen.” Nevertheless, a high Cronbach’s α of .94 for the total scale suggests potential redundancy among the items included in the scale. In addition, the utility of the DSMI may be limited because of its development sample and long items.
Diabetes Self-Management Scale
The Diabetes Self-Management Scale (DSMS) was modified from the Insulin Management Diabetes Self-Care Scale (Hurley, 1988) for use in insulin-treated individuals with T2DM (Sousa, Hartman, Miller, & Carroll, 2009). The DSMS consists of 60, 6-point (0 = strongly disagree to 5 = strongly agree) Likert-type items encompassing the following areas: diet, physical activity, SMBG, medication, problem solving, and risk reduction for disease-related complications. Sample items include “I eat at least three meals every day” and “I wear closed-toe shoes every time I am outside my home.” Composite scores range from 0 to 300, with higher scores indicating greater diabetes self-management. Content validity was the only form of validity tested, with no reliability testing done (Sousa et al., 2009). Further psychometric testing is warranted.
Diabetes Self-Care Scale (DSCS)
The Diabetes Self-Care Scale (DSCS) is a 35-item scale, modified from the Insulin Management Diabetes Self-Care Scale (Hurley, 1988). Each item is rated on a 6-point Likert-type scale ranging from 1 (strongly disagree) to 6 (strongly agree; N. Lee & Fisher, 2005). The reliability is satisfactory, ranging from .80 (respondent separation reliability) and .99 (item separation reliability). In addition to principal component analysis, the meaningfulness of the item difficulty order displayed by the Wright variable map and the consistency of that order across respondents supported the construct validity. Although DSCS is a reliable and valid instrument, further validation is needed among more representative and diverse populations, as acknowledged by the developer. The DSCS was adapted in Turkish to determine the effect of diabetes education on self-care. The internal consistency reported in the Turkish study was greater than the acceptable cutoff of .70 (Karakurt & Kasikci, 2012).
Modified Insulin Management Diabetes Self-Care Scale (M-IMDSCS)
This scale was also adapted from the Insulin Management Diabetes Self-Care Scale (Hurley, 1988) by modifying the original subscales of exercise and medication for application for T2DM (Ludlow & Gein, 1995). The Modified Insulin Management Diabetes Self-Care Scale (M-IMDSCS) has 30 items that cover four domains of diabetes self-care (general management, diet, exercise, and insulin/oral hypoglycemic agents), with a higher score indicating a higher level of self-care. No example items are available. Internal consistency reliability coefficients met the acceptable cutoff of .70. In addition, diabetes self-care as measured by M-IMDSCS was negatively correlated with HbA1c (r =−.37, p < .01) and positively correlated with self-efficacy (r = .83, p < .01), suggesting construct validity (Ludlow & Gein, 1995). M-IMDSCS was used only once in a Canadian sample and covers only part of diabetes self-care; hence, its adequacy as a comprehensive diabetes self-care instrument is questionable.
Diabetes Self-Care Scale-Chinese version
The Diabetes Self-Care Scale (DSC) was originally developed by Hurley and Shea, 1992 for use in T1DM patients and was translated into Chinese by Wang et al. (1998) in Taiwan. The Chinese version contains items related to exercise, diet, medication, SMBG, foot care, and prevention and management of hypo- and hyperglycemia, with a total of 27 items (Bai, Chiou, & Chang, 2009; Huang, Hung, Stocker, & Lin, 2013; Kang et al., 2010; R. H. Wang, Wu, & Hsu, 2011). Responses are graded on a 5-point Likert-type scale, with higher scores indicating better adherence. There is good support for its reliability and validity (Bai et al., 2009; Huang et al., 2013; Kang et al., 2010; R. H. Wang et al., 2011). Using DSC scores, R. H. Wang, Wu, and Hsu (2011) constructed a path model to test relationships between diabetes self-care behavior, glycemic control, and health-related quality of life with significant path coefficients (r = .109–.441; p < .05 for all coefficients). Due to its being tested and used exclusively in Taiwan, its application to other ethnicities is questionable.
Disease-specific adherence scale for diabetes
This scale was developed for the Medical Outcomes Study to measure adherence among patients with chronic medical conditions: diabetes mellitus, hypertension, and heart disease (Kravitz et al., 1993; Y. Y. Lee & Lin, 2009). The diabetes part covers eight behaviors recommended for patients with diabetes such as following a low-fat low-calorie diet, checking blood for sugar, and taking prescribed medications. The patients are asked about the extent to which they followed the eight behaviors referred to earlier during the past 4 weeks on a 6-point Likert-type scale from none of the time to all of the time. Internal consistency reliability coefficients were lower than the acceptable cutoff of .70 (Kravitz et al., 1993; Y. Y. Lee & Lin, 2009). Among diabetic patients taking insulin, higher adherence was associated with lower fasting blood glucose and lower HbA1c (Kravitz et al., 1993). Overall, the tool has limited evidence of reliability and validity. More rigorous psychometric testing is warranted before it is used widely.
Revised Adherence in Diabetes Questionnaire (RADQ)
The Revised Adherence in Diabetes Questionnaire is a 10-item Chinese scale to assess patients’ adherence to treatment, including diet, exercise, medicine, SMBG, and the frequency of reexaminations (Zhang et al., 2013). No further item information is available. Each item is rated on a 4-point Likert-type scale, from rarely (1) to always (4), with higher scores indicating better adherence. The internal consistency was satisfactory, with a Cronbach’s α of .87. No other forms of psychometric properties including validity were reported; therefore, further investigation of the scale is warranted.
Self-Care Activity Questionnaire
The Self-Care Activity Questionnaire is a 75-item tool of which 45 are used to assess self-care practices in relation to diet, medication, physical activity, and SMBG in the preceding 7 days (Tan & Magarey, 2008). Example items include “How many days did you eat fruit last week?” and “How many times did you miss taking your diabetes medicine(s)?” Different subscales have different response formats and scoring systems. The Self-Care Activity Questionnaire yielded reliability coefficients at or a little lower than the acceptable level. Content validity by diabetologists, diabetes clinical nurse specialists, dieticians, and adults with diabetes was the only form of validity tested. The Self-Care Activity Questionnaire was used only once in a predominantly Malaysian sample (N = 126) with suboptimal glycemic control; therefore, the application to other ethnicities is questionable.
Self-Care Behavior Scale
The 26-item Self-Care Behavior Scale developed in Taiwan (Huang & Hung, 2007) covers the following domains: exercise, diet, medication, SMBG, foot care, and prevention of high- and low-blood glucose. No further item information is available. Acceptable internal consistency was the only form of psychometric properties reported (Huang & Hung, 2007). Due to the limited validation sample and instrument information, wide application is questionable.
Self-Care Inventory
The Self-Care Inventory (SCI) was originally designed to assess individuals’ perceptions of their adherence to diabetes self-care recommendations during the past months. The original SCI contains 14 items mainly reflecting Type 1 treatment regimens, including SMBG, insulin use, food, and exercise, and was mostly used in children and adolescents, with good psychometric properties (Weinger, Welch, Butler, & La Greca, 2005). Only internal consistency was reported on SCI use among adults with T2DM, ranging from .53 to .81 (Polonsky et al., 1995). Weinge et al. (2005) modified the SCI to reflect current diabetes practice. The SCI Revised (SCI-R) consists of 15 items, of which 4 items address diet, 3 medication, 3 preventative/routine aspects of self-care (e.g., attending clinic appointments and keeping food records), 2 SMBG, 2 hypoglycemia, and 1 exercise. For scoring, items are averaged and converted to a 0- to 100-point scale. A higher score indicates a higher level of self-care. The SCI-R was validated in both type 1 and type 2 diabetic patients, with support for its reliability, concurrent validity (with Summary of Diabetes Self-Care Activity [SDSCA]), and convergent validity (with the Problem Areas in Diabetes Scale and the Benefits/Barriers Scale). A significant relationship (r = −.37) between SCI-R and HbA1c was also reported in a relatively small sample (N = 90; 90% Caucasian; Weinger et al., 2005). The SCI-R was tested in a Nigerian population with acceptable internal consistency reliability (Ogbera & Adeyemi-Doro, 2011). Evidence of good psychometric properties and the brevity of the instrument are strengths, though it does not cover some of the key diabetes self-care areas such as foot care. In addition, due to the small, homogenous validation sample, further validation is warranted in diverse populations before wide application of the instrument.
Adherence to self-care behaviors questionnaire
The Adherence to Self-care Behaviors Questionnaire, adapted from SCI, consists of 10 items covering five areas of self-care behaviors: regular clinic attendance, blood tests, medication and/or insulin use, diet, and physical activity (Cohen & Kanter, 2004). Items are rated on a 5-point Likert-type scale. No example items are available. It yielded acceptable internal consistency reliability. Factor analysis demonstrated a one-factor model. Considering that this instrument was used only once in a small sample of Hebrew-speaking individuals (N = 67) with limited instrument information, its application is questionable.
Summary of Diabetes Self-Care Activity
The Summary of Diabetes Self-Care Activity (SDSCA), developed by Toobert and Glasgow (1994), is a 12-item multidimensional instrument to assess levels of diabetes self-care across five domains: overall diet (2 items), dietary intake of specific foods (3 items), exercise (3 items), medication taking (2 items), and SMBG (2 items). The instrument is based on the self-reported frequency of completing recommended activities during the past 7 days. An example item includes “How often did you follow your recommended diet over the last 7 days?” All responses are converted to percentages. Higher percentages represent better self-care on each subscale. The SDSCA demonstrated evidence of adequate psychometric testing (Bean, Cundy, & Petrie, 2007; Gallegos, Ovalle-Berumen, & Vinicio Gomez-Meza, 2006; Nouwen et al., 2011; Talbot, Nouwen, Gingras, Gosselin, & Audet, 1997; Toobert, Hampson, & Glasgow, 2000). In general, the SDSCA was reliable except for the specific diet subscale, which showed unsatisfactory interitem correlations (Toobert et al., 2000). The SDSCA has been used in a number of settings and studies (Oftedal, Bru, & Karlsen, 2011; Sacco et al., 2007; Sultan, Attali, Gilberg, Zenasni, & Hartemann, 2011) and has been recommended for a standardized evaluation of quality improvement interventions in T2DM in Canada (Majumdar et al., 2005). Its brevity and psychometric support contribute to its practicality as a research tool.
In 2000, the SDSCA was revised to include items on foot care and cigarette smoking, with 11 core items and 14 supplemental items, totaling 25 (Toobert et al., 2000). Recent most of studies revealed unsatisfactory internal consistency for the revised scale with Cronbach’s αs lower than .70 (Costa, Pereira, & Pedras, 2012; Janzen Claude, Hadjistavropoulos, & Friesen, 2014; Kroese, Adriaanse, & De Ridder, 2012; Kroese, Adriaanse, Vinkers, van de Schoot, & de Ridder, 2014; Trouilloud & Regnier, 2013; Weinger et al., 2005), limiting the utility of the revised tool. Nevertheless, the revised SDSCA has been translated into cross-cultural versions, such as Chinese, Tai, Korean, Turkish, Arabic, Portuguese, and Maltese (Choi et al., 2011; Cosansu & Erdogan, 2014; Gao et al., 2013; Gatt & Sammut, 2008; Gucciardi, Demelo, Lee, & Grace, 2007; Jarab, Alqudah, Mukattash, Shattat, & Al-Qirim, 2012; Kav et al., 2010; Keeratiyutawong, Hanucharurnkul, Eramo Melkus, Panpakdee, & Vorapongsathorn, 2006; Navicharern, 2012; Nyunt, Howteerakul, Suwannapong, & Rajatanun, 2010; Shi, Ostwald, & Wang, 2010; Sowattanangoon, Kochabhakdi, & Petrie, 2008; Tang, Pang, Chan, Yeung, & Yeung, 2008; Vivienne Wu et al., 2008; Wu, Courtney, et al., 2007; Wu, Huang, et al., 2011; Xu et al., 2008). But, most cross-cultural versions did not achieve acceptable internal consistency, especially for diet subscale (Choi et al., 2011; Cosansu & Erdogan, 2014; Gatt & Sammut, 2008; Gucciardi et al., 2007; Kav et al., 2010; Tang et al., 2008; Xu et al., 2008). Although SDSCA has been used widely, its psychometric properties still require further rigorous testing (e.g., validity for the revised version).
Diabetes Self-Care Activity Questionnaire—Greek version
This instrument was developed in Greece (Intas et al., 2012), adapted from four existing questionnaires: SDSCA, Patient Health Questionnaire, 12-item Short Form Health Survey, and Diabetes Self-care Behaviors and Barriers Instrument. It contains 38 items covering 7 areas, including sociodemographics, risk factors, physical and mental health, physician-patient communications, self-care activities, self-care recommendations, and compliance. No example items are available. After being reviewed by a panel of health care professionals, adapted, and piloted, systematic psychometric testing was done in a relatively large sample (N = 480). The tool yielded satisfactory internal consistency and test–retest reliability. The high correlation with the Habit, Attitudes, and Knowledge questionnaire and the discrimination between patients with different levels of compliance supported the evidence of validity. As is the case for other instruments developed in international settings with a language other than English, the utility of the instrument is limited to those in Greece unless further validation is done with diverse populations and languages.
The Diabetes Activities Questionnaire
The The Diabetes Activities Questionnaire (TDAQ) is a 13-item instrument, scored on a visual analogue scale (VAS) 100 mm in length (Chlebowy & Garvin, 2006; Hernandez, 1997). An example item includes “I follow my meal plan exactly as suggested by my dietitian.” In the original validation study (N = 153), reliability testing was done using internal consistency, test–retest reliability, and item-total correlations, with generally adequate values. Construct validity was tested by principle components analysis, revealing two factors: lifestyle/monitoring and treatment (Hernandez, 1997). The psychometric properties of TDAQ seem to be adequate, with evidence of reliability and validity. The unique response format, VAS, is easy to administer, simple to understand, and helpful to lessen the likelihood of responses being made in a socially desirable manner. Nevertheless, as a new instrument with limited use, ongoing testing of validity and reliability in diverse samples are warranted.
Unidimensional Instruments
In the following section, several self-care instruments that were designed to measure one particular self-care behavior are discussed. As was the case for the multidimensional instruments described previously, most of the unidimensional measures were used just once in their own validation studies.
Diet Self-Management Behavior Questionnaire
The Diet Self-Management Behavior Questionnaire (DSBQ)—a diet-specific instrument developed in Japan (Taru, Tsutou, Nakawatase, Usami, & Miyawaki, 2008)—contains two parts with 89 items on a 5-point Likert-type scale from never (0) to always (5). The first part—”following instructions of dietary regimen”—is used to assess adherence to the dietary regimen. An example item includes, “I use 50 g–100 g servings of meat or fish for a single meal.” The second part—”coping behavior regarding factors interfering with dietary regimen”—is related to three categories regarding coping with factors interfering with the dietary regimen. An example item includes “to reduce my stomach size and thus curb my appetite, I try to reduce my overall food intake.” The DSBQ had reliability coefficients ranging from .55 to .83. The correlation between the DSBQ and dietary intakes obtained by the food frequency questionnaire such as total energy, lipids, and carbohydrate intake supported its validity. Because the applicability of the tool has been limited exclusively to a Japanese population, application in other ethnicities is questionable. Also, the long list of items and unsatisfactory reliability warrant future effort to improve the tool.
Kristal Food Habits Questionnaire
The 20-item Food Habit questionnaire was developed by Kristal (Kristal, Shattuck, & Henry, 1990) to assess dietary patterns related to selecting low-fat diets, including “excluding high-fat ingredients and preparation techniques,” “modifying high-fat foods,” “substituting specially manufactured low-fat foods,” and “replacing high-fat foods with low-fat laternatives.” An example item includes “when you eat chicken, how often has it been fried?” In an intervention study targeting the development of proactive coping skills, only internal consistency reliability of this tool was reported, lower than .7 (Kroese, Adriaanse, Vinkers, et al., 2014). The limited use and inadequate testing of this tool warrant further evaluation in the population of T2DM.
Modified version of Dobson’s 17-item Short Fat Questionnaire
Dobson’s 17-item Short Fat Questionnaire is a self-administered and self-coded measure of dietary fat intake (Dobson et al., 1993). In Clarke’s study (Clarke, 2009), the questionnaire was modified to measure self-reported dietary fat intake behavior. Internal consistency reliability was the only form of psychometrics testing, with an acceptable level. Adequacy of this tool as a research instrument is questionable because of limited psychometric evidence.
Evaluation Scale for Self-Management Behavior Related to Physical Activity of Type 2 Diabetic Patients
The Evaluation Scale for Self-Management Behavior Related to Physical Activity of Type 2 Diabetic Patients (ES-SMBPA-2D) was developed based on one of the key behaviors to diabetes self-management (i.e., physical activity) and its measurement defined as core measures of outcomes performance by the American Association of Diabetes Educators and semi-structured interviews of persons with T2DM in Japan (Nakawatase et al., 2007). Respondents were asked to report the frequency of self-care behavior related to the enhancement (e.g., spending a large amount of time on shopping) and maintenance (e.g., making time to enjoy favorite physical activities) of daily physical activity, using a 5-point Likert-type scale from 1 (never) to 5 (always). Content experts confirmed the content validity. Concurrent validity was tested by correlations between the ES-SMBPA-2D and the Japanese version of the International Physical Activity Questionnaire subscale (r = .16). The Cronbach’s α was generally satisfactory. The test–retest reliability coefficients ranged from .60 to .88 (Nakawatase et al., 2007). Although evaluated thoroughly, the inadequate psychometric properties and limitation of validation sample warrant further rigorous testing and application in other ethnic populations before being used widely.
Medication Adherence Report Scale
The Medication Adherence Report Scale (MARS) is a self-reported measure of nonadherence behavior to prescribed medications (e.g., changing doses, stopping, or forgetting to take medication; Horne & Weinman, 1999). MARS has 5 items on a 5-point Likert-type scale. The summed score ranges from 5 to 25, with higher scores indicating higher levels of adherence to the prescribed medication recommendations. Examples of items include “Some people forget to take their medicines. How often does this happen to you?” and “Some people miss out a dose of their medications or adjust it to suit their own needs. How often do you do this?” Only internal consistency was reported, ranging from .65 to .97 (Aflakseir, 2012; Barnes, Moss-Morris, & Kaufusi, 2004; Clarke, 2009; Kroese, Adriaanse, et al., 2012; Kroese, Adriaanse, Vinkers, et al., 2014). Barnes, Moss-Morris, and Kaufusi (2004) added 2 items to the MARS to address traditional medicine use and behavior relating to religious beliefs in Tongan patients, with an acceptable Cronbach’s α value. Lack of evidence on validity and low levels of internal consistency reliability warrant further testing and modification of the instrument before it is used widely.
Measurement of Adherence to Treatment
The Measurement of Adherence to Treatment (MAT) is a scale for evaluating adherence to prescribed treatment with medications (Boas, Lima, & Pace, 2014). Considering the complexity of diabetes treatment, Boas, Lima, and Pace (2014) adapted the MAT by presenting the items in two ways: adherence to oral antidiabetics (MAT OADs) and to insulin (MAT insulin). The example items include “Have you ever forgotten to take the tablets/administer the insulin for the diabetes?” and “Have you ever been careless with the time for taking the tablets/administering the insulin for the diabetes?” The MAT consists of 7 items rated on a 6-point Likert-type scale, higher scores indicate greater adherence. The MAT OADs was more reliable than the MAT insulin, with adequate internal consistency and item-total correlations (Boas et al., 2014). Considering the original MAT as the gold standard, criterion-related validity was tested, with coefficients of .83 for the MAT OADs and .77 for the MAT insulin. Despite some evidence of reliability and validity, the scale was tested only once in a small sample (N = 90) in Brazil, requiring additional evaluation for use in diverse populations.
Morisky Medication Adherence Scale
The Morisky Medication Adherence Scale (MMAS; 4-item) is a brief, commonly used, easily administered questionnaire to assess medication adherence in chronic diseases such as diabetes, hypertension, asthma, or heart failure (Parada, Horton, Cherrington, Ibarra, & Ayala, 2012; Y. Wang, Lee, Toh, Tang, & Ko, 2012). The scale assesses both unintentional (forgetting and carelessness) and intentional medication nonadherence (stopping the drug when feeling better/worse) with dichotomous responses (yes/no). Responses are summed within a range of 0 to 4, with scores ≥1 indicating medication nonadherence. The MMAS is available in different languages such as Chinese and Arabic but with inadequate internal consistency reliability coefficients (Jarab et al., 2012; Parada et al., 2012; Y. Wang et al., 2012). In the validation study of the Chinese version (Wang, 2012), validity testing was done using different approaches including content, convergent, and construct validities. The principle analysis showed a single factor model. The relationship between MMAS and HbA1c and adherence to diet and physical exercise was reported (p < .05).
The 4-item MMAS was later revised as an 8-item instrument in a Malaysian, Thai, Korean, and Persian version, still with poor internal consistency, but both yielded acceptable convergent validity with the original version, and the relationship between MMAS (8-item) and HbA1c was established (Al-Qazaz et al., 2010; W. Y. Lee et al., 2013; Negarandeh, Mahmoodi, Noktehdan, Heshmat, & Shakibazadeh, 2013; Sakthong, Chabunthom, & Charoenvisuthiwongs, 2009). Although the MMAS is a brief and easy way to assess medication adherence, it still needs to be improved further for its psychometric properties before being widely used.
A scale to measure adherence to SMBG
This a 15-item tool on a 9-point Likert-type scale, psychometrically sound measure of SMBG adherence (Wagner, Schnoll, & Gipson, 1998). An example item includes “If I feel my blood sugar is low, I test” and “If no one told me to test, I do not test.” After assessment of normality and the determination of the component structure, the remaining 15 items of the scale showed adequate internal consistency, with a Cronbach’s α of .84. The structure model showed two parts: “social influence” and “physical influence.” They are correlated and implied the existence of a higher order latent variable adherence, which can provide valuable implication for understanding and addressing adherence issues in patients. Although this scale is characterized as being brief, easy to explain, and fit for use in clinical and research work, the fact that it was validated in a predominantly White sample and reported only once requires validation in different samples for further generalizability. Further validation for criterion/convergent validity is also necessary.
UISESS-B scale
The UISESS-B scale was developed to evaluate self-care habits and self-perception of oral health for patients with chronic diseases including diabetes mellitus (Salcedo-Rocha, Garcia-de-Alba-Garcia, Velasquez-Herrera, & Barba-Gonzalez, 2011). The UISESS-B consists of two parts: oral health habits (hygiene, food/feeding, and care/protection) and oral health status self-perception (mouth and teeth signs and symptoms), with 35 items rated on 3-point Likert-type scale. Example items include “I take much water to avoid dryness” and “I wash my teeth to get up and go to bed.” The psychometric properties of the UISESS-B seem to be strong, with evidence of reliability and validity, but this tool was newly developed in Mexico and validated in a small sample with diabetes (N = 16); hence, it requires further validation in a large number of patients with diverse backgrounds.
Discussion
Diabetes self-care places patients at the center of illness management. Patients must self-manage their illness with the support and assistance of health care professionals. This interactive process partly depends on patients’ reports on their self-care. As such, the application of self-report measures of diabetes self-care has continued to grow, in particular, within the last decade. We found that 73.3% or 22 of the 30 instruments reviewed were newly developed during the last decade. In addition, two thirds (20 of 30) were used or validated only once.
Psychometrically sound instruments are a prerequisite to an accurate assessment of self-care practices in patients with diabetes. Inadequate reliability and validity of instruments make it difficult to detect the impact of an intervention program on diabetes control behaviors. This systematic review revealed that most diabetes self-care instruments have not been rigorously evaluated, either with insufficient assessment or with unsatisfactory psychometric properties. Less than half (n = 34) out of 75 studies reported information about both reliability and validity, whereas 4 of the studies simply reported initial content validity. More frequently, we faced difficulties with identifying and assessing psychometric testing of different iterations of the same tool. The literature review process showed that quite a few studies adapted or applied part of an already validated tool but without documentation of previous psychometric testing or psychometric testing undertaken at the time of utilizing the tool for the author’s own study. Also, as mentioned earlier, most published instruments were relatively new; even for repeatedly used instruments, there was inconsistent evidence to support their reliability and validity, such as the SDSCA in Chinese (Gao et al., 2013; Shi et al., 2010; Tang et al., 2008; Xu et al., 2008). Nevertheless, among the identified instruments, the SDSCA, DCP, MARS, and MMAS were the most widely used and well-validated instruments: The SDSCA is a comprehensive measure of self-care behaviors, the DCP is a standardized instrument for assessing social and psychological factors related to diabetes and its treatment, and the MARS and MMAS focus exclusively on medication taking.
The generalizability of existing diabetes self-care instruments may be hampered by their limited application to different cultures or language groups. The SDSCA and MMAS were the only two instruments that have been translated and validated in more than one language: Chinese, Korean, Turkish, Thai, Maltese, Arabic, and Portuguese for the SDSCA and Chinese, Arabic, Malaysian, Korean, Persian, and Thai for the MMAS. To evaluate the impact of diabetes self-care intervention in diverse groups of patients, researchers and clinicians need to adapt and apply standard tools after retesting and confirming the psychometric properties. Although the transcultural adaptation—including translation, adjustment, and validation—of a developed instrument in a specific culture can still present some challenges, the use of an existing well-validated instrument may not only save time but also facilitate comparisons across studies.
The self-report instruments used to measure diabetes self-care can be divided into two categories: one relies on patients’ reports on frequency of a specific self-care behavior over a certain time period (e.g., SDSCA and DSCAQ) and another relies on patients’ reports on their perceptions of their self-care behaviors (e.g., SCI). The former is based on the patient’s memory and recall of behaviors and the latter on patients’ ability to summarize their own behaviors. Comparatively, the latter may take into account differences in individual prescriptions, but subjectivity can be relatively stronger. Which method is a more accurate, practical, and an easy-to-use measurement of self-care behavior is questionable and needs further exploration.
Information on scoring was often insufficient. In this review, only 10 instruments provided information on scoring: Disease-Specific Adherence Scale for Diabetes, TDAQ, Self-Care Activity Questionnaire, SCI-R, D-SMART, Diabetes Self-Care Scale, Diabetes Self-Care Ability Questionnaire, MMAS, MAT, and UISESS-B. For multidimensional instruments, either assessing each domain separately or combining scores across different domains may have different implications. For example, Toobert, Hampson, and Glasgow (2000) found that certain self-care domains were not highly correlated with each other, which seemed to indicate that individual scoring of different self-care domains might be more useful in identifying the areas in which an individual has adherence problems. Interpretation of scoring is also important, yet the information about how to interpret scores obtained from the self-care instrument was frequently omitted. Having a threshold of what constitutes a clinically significant self-care score can help clinicians determine whether further education and attention are needed. Researchers need to pay more attention to identifying a meaningful threshold to enhance clinical utility of self-care assessment tools.
Assessing diabetes self-care can be challenging due, in part, to the complexity of diabetes care. Diabetes self-care is multidimensional, and, to date, no universally accepted domains exist. To maintain good blood glucose and prevent complications, patients are traditionally required to perform self-care in multiple domains such as diet, physical activity, medications, SMBG, and foot care. In practice, facing complex and demanding activities for disease control, patients often experience emotional distress (Furler et al., 2008). Thus, as diabetes care progresses, diabetes self-care may need to focus also on behaviors related to psychosocial in addition to physical issues. A few multidimensional instruments included in our review (e.g., DHPSC, Diabetes Self-Care Activity Questionnaire-Greek version, and DSMI) covered psychosocial domains, such as interpersonal relationships, interaction with providers, and personal health responsibility.
Responsiveness to change should be a priority for future research, although it was not an inclusion criterion in this review. The lack of testing for responsiveness to change in health is a major shortcoming of patient-assessed measure for diabetes. In this review, only four instruments reported responsiveness: SDSCA, MMAS-8, MAT, and Diabetes Self-Care Activity Questionnaire. Further research should evaluate responsiveness through longitudinal comparisons of instruments in order to inform decisions regarding the selection of instruments. It is practicable to combine multidimensional and unidimensional instruments. A multidimensional instrument can be used as a screening tool to identify general problems in self-care behavior. Then, from these general problem categories, specific instruments can be used to find the specific underlying problem. The use of this general screening and problem-refining process could be individualized for each patient to provide patient-centered, culturally specific care.
Limitations
This systematic review has some limitations. Our review included articles published in English only, hence limiting the generalizability of the findings. In addition, only published results were analyzed, and there is a chance that studies on diabetes self-care instruments have not been published and hence were not included in this review. Finally, we tried to provide specific examples of the items in each of the main diabetes self-care domains, but we were limited by the public availability of some instruments. Although efforts were made to contact the developers of the instruments, we were unable to access them in a timely manner for this review.
Conclusion
Most diabetes self-care instruments included in this review lacked systematic reliability and validity testing. Nevertheless, these instruments provide a starting point from which to develop future measurements of diabetes self-care. A few of the instruments have been tested rigorously and can be used widely, which can contribute to comparisons across studies in diverse samples. Given the rapid growth and severe effect of diabetes on global health, it is imperative to devote more intense effort toward establishing high-quality diabetes self-care instruments. Effective measure of critical diabetes self-care can identify self-care deficiencies, by which health care professionals can provide specific support for their patients to strengthen diabetes management.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Manuscript preparation was supported in part by the National Institutes of Health, National Institute of Nursing Research (T32 NR007968 for J. Xu) and the China Medical Board, China Medical Board Nursing Faculty Research (10-020-201205 for Y. Lu). Editorial support for an earlier version of this manuscript was provided by the Johns Hopkins University School of Nursing Center for Excellence for Cardiovascular Health in Vulnerable Populations (P30 NR011409).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aflakseir A. Role of illness and medication perceptions on adherence to medication in a group of Iranian patients with type 2 diabetes. Journal of Diabetes. 2012;4:243–247. doi: 10.1111/j.1753-0407.2012.00183.x. [DOI] [PubMed] [Google Scholar]
- Al-Qazaz H, Hassali MA, Shafie AA, Sulaiman SA, Sundram S, Morisky DE. The eight-item Morisky Medication Adherence Scale MMAS: translation and validation of the Malaysian version. Diabetes Research and Clinical Practice. 2010;90:216–221. doi: 10.1016/j.diabres.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai YL, Chiou CP, Chang YY. Self-care behaviour and related factors in older people with Type 2 diabetes. Journal of Clinical Nursing. 2009;18:3308–3315. doi: 10.1111/j.1365-2702.2009.02992.x. [DOI] [PubMed] [Google Scholar]
- Barnes L, Moss-Morris R, Kaufusi M. Illness beliefs and adherence in diabetes mellitus: A comparison between Tongan and European patients. The New Zealand Medical Journal. 2004;117:U743. [PubMed] [Google Scholar]
- Bean D, Cundy T, Petrie KJ. Ethnic differences in illness perceptions, self-efficacy and diabetes self-care. Psychology & Health. 2007;22:787–811. doi: 10.1080/14768320600976240. [DOI] [Google Scholar]
- Boas LC, Lima ML, Pace AE. Adherence to treatment for diabetes mellitus: Validation of instruments for oral antidiabetics and insulin. Revista Latino-Americana de Enfermagem. 2014;22:11–18. doi: 10.1590/0104-1169.3155.2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charron-Prochownik D, Zgibor JC, Peyrot M, Peeples M, McWilliams J, Koshinsky J Educ AUD. The Diabetes Self-management Assessment Report Tool (D-SMARV (R))—Process evaluation and patient satisfaction. Diabetes Educator. 2007;33:833–838. doi: 10.1177/0145721707307613. [DOI] [PubMed] [Google Scholar]
- Chasens ER, Korytkowski M, Sereika SM, Burke LE. Effect of poor sleep quality and excessive daytime sleepiness on factors associated with diabetes self-management. Diabetes Education. 2013;39:74–82. doi: 10.1177/0145721712467683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chlebowy DO, Garvin BJ. Social support, self-efficacy, and outcome expectations: Impact on self-care behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. Diabetes Education. 2006;32:777–786. doi: 10.1177/0145721706291760. [DOI] [PubMed] [Google Scholar]
- Choi EJ, Nam M, Kim SH, Park CG, Toobert DJ, Yoo JS, Chu SH. Psychometric properties of a Korean version of the summary of diabetes self-care activities measure. International Journal of Nursing Studies. 2011;48:333–337. doi: 10.1016/j.ijnurstu.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Clarke A. Effects of routine education on people newly diagnosed with type 2 diabetes. EDN Autumn. 2009;6:88–94. [Google Scholar]
- Cohen M, Kanter Y. Relation between sense of coherence and glycemic control in type 1 and type 2 diabetes. Behavioral Medicine. 2004;29:175–183. doi: 10.3200/bmed.29.4.175-185. [DOI] [PubMed] [Google Scholar]
- Cosansu G, Erdogan S. Influence of psychosocial factors on self-care behaviors and glycemic control in Turkish patients with type 2 diabetes mellitus. Journal of Transcultural Nursing. 2014;25:51–59. doi: 10.1177/1043659613504112. [DOI] [PubMed] [Google Scholar]
- Costa V, Pereira MG, Pedras S. Partner support, social-cognitive variables and their role in adherence to self-monitoring of blood glucose in type 2 diabetes. EDN Autumn. 2012;9:81–86. [Google Scholar]
- Cunningham V, Mohler MJ, Wendel CS, Hoffman RM, Murata GH, Shah JH, Duckworth WC. Reliability and validity of the DCP among hispanic veterans. Evaluation & the Health Professions. 2005;28:447–463. doi: 10.1177/0163278705281077. [DOI] [PubMed] [Google Scholar]
- Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating G. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: Systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/s0140-6736(11)60679-x. [DOI] [PubMed] [Google Scholar]
- Dobson AJ, Blijlevens R, Alexander HM, Croce N, Heller RF, Higginbotham N, Walker R. Short fat questionnaire: A self-administered measure of fat-intake behaviour. Australian Journal of Public Health. 1993;17:144–149. doi: 10.1111/j.1753-6405.1993.tb00123.x. [DOI] [PubMed] [Google Scholar]
- Eliasziw M, Young SL, Woodbury MG, Fryday-Field K. Statistical methodology for the concurrent assessment of inter-rater and intra-rater reliability: Using goniometric measurements as an example. Physical Therapy. 1994;74:777–788. doi: 10.1093/ptj/74.8.777. [DOI] [PubMed] [Google Scholar]
- Fain JA. Psychometric properties of the Spanish version of the diabetes self-management assessment report tool. Diabetes Education. 2007;33:827–832. doi: 10.1177/0145721707308355. [DOI] [PubMed] [Google Scholar]
- Fitzgerald JT, Anderson RM, Gruppen LD, Davis WK, Aman LC, Jacober SJ, Grunberger G. The reliability of the diabetes care profile for African Americans. Evaluation & the Health Professions. 1998;21:52–65. doi: 10.1177/016327879802100103. [DOI] [PubMed] [Google Scholar]
- Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the diabetes care profile. Evaluation & the Health Professions. 1996;19:208–230. doi: 10.1177/016327879601900205. [DOI] [PubMed] [Google Scholar]
- Furler J, Walker C, Blackberry I, Dunning T, Sulaiman N, Dunbar J, Young D. The emotional context of self-management in chronic illness: A qualitative study of the role of health professional support in the self-management of type 2 diabetes. BMC Health Services Research. 2008;8:214–232. doi: 10.1186/1472-6963-8-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallegos EC, Ovalle-Berumen F, Vinicio Gomez-Meza M. Metabolic control of adults with type 2 diabetes mellitus through education and counseling. Journal of Nursing Scholarship. 2006;38:344–351. doi: 10.1111/j.1547-5069.2006.00125.x. [DOI] [PubMed] [Google Scholar]
- Gao J, Wang J, Zheng P, Haardorfer R, Kegler MC, Zhu Y, Fu H. Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC Family Practice. 2013;14:66. doi: 10.1186/1471-2296-14-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatt S, Sammut R. An exploratory study of predictors of self-care behaviour in persons with type 2 diabetes. International Journal of Nursing Studies. 2008;45:1525–1533. doi: 10.1016/j.ijnurstu.2008.02.006. [DOI] [PubMed] [Google Scholar]
- Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Research and Clinical Practice. 2014;103:137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Gucciardi E, Demelo M, Lee RN, Grace SL. Assessment of two culturally competent diabetes education methods: Individual versus individual plus group education in Canadian Portuguese adults with type 2 diabetes. Ethnicity & Health. 2007;12:163–187. doi: 10.1080/13557850601002148. [DOI] [PubMed] [Google Scholar]
- Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. How well do patients’ assessments of their diabetes self-management correlate with actual glycemic control and receipt of recommended diabetes services? Diabetes Care. 2003;26:738–743. doi: 10.2337/diacare.26.3.738. [DOI] [PubMed] [Google Scholar]
- Hernandez CA. The development and pilot testing of The Diabetes Activities Questionnaire (TDAQ): An instrument to measure adherence to the diabetes regimen. Applied Nursing Research: ANR. 1997;10:202–211. doi: 10.1016/s0897-1897(97)80596-4. [DOI] [PubMed] [Google Scholar]
- Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. Journal of Psychsomatic Research. 1999;47(6):555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Huang MC, Hung CH. Quality of life and its predictors for middle-aged and elderly patients with type 2 diabetes mellitus. Journal of Nursing Research. 2007;15:193–200. doi: 10.1097/01.jnr.0000387615.87683.13. [DOI] [PubMed] [Google Scholar]
- Huang MC, Hung CH, Stocker J, Lin LC. Outcomes for type 2 diabetes mellitus patients with diverse regimens. Journal of Clinical Nursing. 2013;22:1899–1906. doi: 10.1111/jocn.12123. [DOI] [PubMed] [Google Scholar]
- Hurley AC. Diabetes health beliefs and self care of individuals who require insulin. Dissertation Abstract International. 1988;50:2487B. (UMI No. 9121356) [Google Scholar]
- Hurley AC, Shea CA. Self-efficacy: Strategy for enhancing diabetes self-care. Diabetes Education. 1992;18:146–150. doi: 10.1177/014572179201800208. [DOI] [PubMed] [Google Scholar]
- Intas G, Kalogianni A, Stergiannis P, Bratakos M, Dimoula I, Kelesi M, Marvaki C. Development and validation of a diabetes self-care activities questionnaire. Journal of Diabetes Nursing. 2012;16:100–110. [Google Scholar]
- Janzen Claude JA, Hadjistavropoulos HD, Friesen L. Exploration of health anxiety among individuals with diabetes: Prevalence and implications. Journal of Health Psychology. 2014;19:312–322. doi: 10.1177/1359105312470157. [DOI] [PubMed] [Google Scholar]
- Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with Type 2 diabetes in an outpatient diabetes clinic in Jordan. Journal of Managed Care Pharmacy. 2012;18:516–526. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang CM, Chang SC, Chen PL, Liu PF, Liu WC, Chang CC, Chang WY. Comparison of family partnership intervention care vs. conventional care in adult patients with poorly controlled type 2 diabetes in a community hospital: A randomized controlled trial. International Journal of Nursing Studies. 2010;47:1363–1373. doi: 10.1016/j.ijnurstu.2010.03.009. [DOI] [PubMed] [Google Scholar]
- Karakurt P, Kasikci MK. The effect of education given to patients with type 2 diabetes mellitus on self-care. International Journal of Nursing Practice. 2012;18:170–179. doi: 10.1111/j.1440-172X.2012.02013.x. [DOI] [PubMed] [Google Scholar]
- Kav S, Akman A, Dogan N, Tarakci Z, Bulut Y, Hanoglu Z. Turkish validity and reliability of the summary of diabetes self-care activities measure for patients with type 2 diabetes mellitus. Journal of Clinical Nursing. 2010;19:2933–2935. doi: 10.1111/j.1365-2702.2010.03329.x. [DOI] [PubMed] [Google Scholar]
- Keeratiyutawong P, Hanucharurnkul S, Eramo Melkus GD, Panpakdee O, Vorapongsathorn T. Effectiveness of self-management program for Thais with type 2 diabetes. Thai Journal of Nursing Research. 2006;10:85–97. [Google Scholar]
- Kravitz RL, Hays RD, Sherbourne CD, DiMatteo MR, Rogers WH, Ordway L, Greenfield S. Recall of recommendations and adherence to advice among patients with chronic medical conditions. Archives of Internal Medicine. 1993;153:1869–1878. doi: 10.1001/archinte.153.16.1869. [DOI] [PubMed] [Google Scholar]
- Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. Journal of the American Dietetic Association. 1990;90:214–220. [PubMed] [Google Scholar]
- Kroese FM, Adriaanse MA, De Ridder DT. Boosters, anyone? Exploring the added value of booster sessions in a self-management intervention. Health Education Research. 2012;27:825–833. doi: 10.1093/her/cys062. [DOI] [PubMed] [Google Scholar]
- Kroese FM, Adriaanse MA, Vinkers CD, van de Schoot R, de Ridder DT. The effectiveness of a proactive coping intervention targeting self-management in diabetes patients. Psychology Health. 2014;29:110–125. doi: 10.1080/08870446.2013.841911. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Lee N, Fisher W. Evaluation of the diabetes self-care scale. Journal of Applied Measurement. 2005;6:366–381. [PubMed] [Google Scholar]
- Lee WY, Ahn J, Kim JH, Hong YP, Hong SK, Kim YT, Morisky DE. Reliability and validity of a self-reported measure of medication adherence in patients with type 2 diabetes mellitus in Korea. Journal of International Medical Research. 2013;41:1098–1110. doi: 10.1177/0300060513484433. [DOI] [PubMed] [Google Scholar]
- Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Social Science & Medicine. 2009;68:1060–1068. doi: 10.1016/j.socscimed.2008.12.033. [DOI] [PubMed] [Google Scholar]
- Lin CC, Anderson RM, Chang CS, Hagerty BM, Loveland-Cherry CJ. Development and testing of the diabetes self-management instrument: A confirmatory analysis. Research in Nursing & Health. 2008;31:370–380. doi: 10.1002/nur.20258. [DOI] [PubMed] [Google Scholar]
- Ludlow AP, Gein L. Relationships among self-care, self-efficacy and HbA1c levels in individuals with non-insulin dependent diabetes mellitus (NIDDM) Canadian Journal of Diabetes Care. 1995;19:10–15. [Google Scholar]
- Majumdar SR, Johnson JA, Bowker SL, Booth GL, Harris SB, Hux JE, Toth EL. A Canadian consensus for the standardized evaluation of quality improvement interventions in Type 2 diabetes. Canadian Journal of Diabetes. 2005;29:220–229. [Google Scholar]
- Mekwiwatanawong C, Hanucharurnkul S, Piaseu N, Nityasuddhi D. Comparison of outcomes diabetes of patients with diabetes receiving care by way of three primary care practice models. Pacific Rim International Journal of Nursing Research. 2013;17:39–55. [Google Scholar]
- Michigan Diabetes Research and Training Center. 2014 Retrieved from http://www.med.umich.edu/mdrtc/profs/documents/svi/dcp.pdf.
- Nakawatase Y, Taru C, Tsutou A, Shiotani H, Kido Y, Ohara T, Miyawaki I. Development of an evaluation scale for self-management behavior related to physical activity of type 2 diabetic patients. Diabetes Care. 2007;30:2843–2848. doi: 10.2337/dc07-0685. [DOI] [PubMed] [Google Scholar]
- Navicharern R. Diabetes self-management, fasting blood sugar and quality of life among type 2 diabetic patients with foot ulcers. Journal of the Medical Association of Thailand = Chotmaihet Thangphaet. 2012;95:156–162. [PubMed] [Google Scholar]
- Negarandeh R, Mahmoodi H, Noktehdan H, Heshmat R, Shakibazadeh E. Teach back and pictorial image educational strategies on knowledge about diabetes and medication/dietary adherence among low health literate patients with type 2 diabetes. Primary Care Diabetes. 2013;7:111–118. doi: 10.1016/j.pcd.2012.11.001. [DOI] [PubMed] [Google Scholar]
- Nesari M, Zakerimoghadam M, Rajab A, Bassampour S, Faghihzadeh S. Effect of telephone follow-up on adherence to a diabetes therapeutic regimen. Japan Journal of Nursing Science. 2010;7:121–128. doi: 10.1111/j.1742-7924.2010.00146.x. [DOI] [PubMed] [Google Scholar]
- Nouwen A, Ford T, Balan AT, Twisk J, Ruggiero L, White D. Longitudinal motivational predictors of dietary self-care and diabetes control in adults with newly diagnosed type 2 diabetes mellitus. Health Psychology. 2011;30:771–779. doi: 10.1037/a0024500. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. 3. New York, NY: McGraw-Hill; 1994. [Google Scholar]
- Nyunt SW, Howteerakul N, Suwannapong N, Rajatanun T. Self-efficacy, self-care behaviors and glycemic control among type-2 diabetes patients attending two private clinics in Yangon, Myanmar. Southeast Asian Journal of Tropical Medicine and Public Health. 2010;41:943–951. [PubMed] [Google Scholar]
- Oftedal B, Bru E, Karlsen B. Motivation for diet and exercise management among adults with type 2 diabetes. Scandinavian Journal of Caring Sciences. 2011;25:735–744. doi: 10.1111/j.1471-6712.2011.00884.x. [DOI] [PubMed] [Google Scholar]
- Ogbera A, Adeyemi-Doro A. Emotional distress is associated with poor self care in type 2 diabetes mellitus. Journal of Diabetes. 2011;3:348–352. doi: 10.1111/j.1753-0407.2011.00156.x. [DOI] [PubMed] [Google Scholar]
- Orem DE. Nursing: Concepts of practice. 5. St. Louis, MI: Mosby; 1995. [Google Scholar]
- Parada H, Jr, Horton LA, Cherrington A, Ibarra L, Ayala GX. Correlates of medication nonadherence among Latinos with type 2 diabetes. Diabetes Education. 2012;38:552–561. doi: 10.1177/0145721712445215. [DOI] [PubMed] [Google Scholar]
- Partiprajak S, Hanucharurnkul S, Piaseu N, Brooten D, Nityasuddhi D. Outcomes of an advanced practice nurse-led type-2 diabetes support group. Advanced Practice Nurse. 2011;15:288–304. [Google Scholar]
- Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, King H. The burden of mortality attributable to diabetes: Realistic estimates for the year 2000. Diabetes Care. 2005;28:2130–2135. doi: 10.2337/diacare.28.9.2130. [DOI] [PubMed] [Google Scholar]
- Sacco WP, Wells KJ, Friedman A, Matthew R, Perez S, Vaughan CA. Adherence, body mass index, and depression in adults with type 2 diabetes: The mediational role of diabetes symptoms and self-efficacy. Health Psychology. 2007;26:693–700. doi: 10.1037/0278-6133.26.6.693. [DOI] [PubMed] [Google Scholar]
- Sakthong P, Chabunthom R, Charoenvisuthiwongs R. Psychometric properties of the Thai version of the 8-item Morisky medication adherence scale in patients with type 2 diabetes. Annals of Pharmacotherapy. 2009;43:950–957. doi: 10.1345/aph.1L453. [DOI] [PubMed] [Google Scholar]
- Salcedo-Rocha AL, Garcia-de-Alba-Garcia JE, Velasquez-Herrera JG, Barba-Gonzalez EA. Oral health: Validation of a questionnaire of self-perception and self-care habits in diabetes mellitus 2, hypertensive and obese patients. The UISESS-B scale. Medicina Oral Patología Oral y Cirugia Bucal. 2011:e834–e839. doi: 10.4317/medoral.17108. [DOI] [PubMed] [Google Scholar]
- Shi Q, Ostwald SK, Wang S. Improving glycaemic control self-efficacy and glycaemic control behaviour in Chinese patients with type 2 diabetes mellitus: Randomised controlled trial. Journal of Clinical Nursing. 2010;19:398–404. doi: 10.1111/j.1365-2702.2009.03040.x. [DOI] [PubMed] [Google Scholar]
- Sousa VD, Hartman SW, Miller EH, Carroll MA. New measures of diabetes self-care agency, diabetes self-efficacy, and diabetes self-management for insulin-treated individuals with type 2 diabetes. Journal of Clinical Nursing. 2009;18:1305–1312. doi: 10.1111/j.1365-2702.2008.02729.x. [DOI] [PubMed] [Google Scholar]
- Sowattanangoon N, Kochabhakdi N, Petrie KJ. Buddhist values are associated with better diabetes control in Thai patients. The International Journal of Psychiatry in Medicine. 2008;38:481–491. doi: 10.2190/PM.38.4.g. [DOI] [PubMed] [Google Scholar]
- Sultan S, Attali C, Gilberg S, Zenasni F, Hartemann A. Physicians’ understanding of patients’ personal representations of their diabetes: Accuracy and association with self-care. Psychology Health. 2011;26:101–117. doi: 10.1080/08870441003703226. [DOI] [PubMed] [Google Scholar]
- Talbot F, Nouwen A, Gingras J, Gosselin M, Audet J. The assessment of diabetes-related cognitive and social factors: The multidimensional diabetes questionnaire. Journal of Behavioral Medicine. 1997;20:291–312. doi: 10.1023/a:1025508928696. [DOI] [PubMed] [Google Scholar]
- Tan MY, Magarey J. Self-care practices of Malaysian adults with diabetes and sub-optimal glycaemic control. Patient Education and Counseling. 2008;72:252–267. doi: 10.1016/j.pec.2008.03.017. [DOI] [PubMed] [Google Scholar]
- Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. Journal of Advanced Nursing. 2008;62:74–83. doi: 10.1111/j.1365-2648.2007.04526.x. [DOI] [PubMed] [Google Scholar]
- Taru C, Tsutou A, Nakawatase Y, Usami M, Miyawaki I. Gender differences of dietary self-management behavior affecting control indices in type II diabetes. Kobe Journal of Medical Sciences. 2008;54:E82–E96. [PubMed] [Google Scholar]
- Toobert DJ, Glasgow RE. Assessing diabetes self-management: the summary of diabetes self-care activities questionnaire. In: Bradley C, editor. Handbook of Psychology and Diabetes. Chur, Switzerland: Harwood Academic; 1994. pp. 351–375. [Google Scholar]
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure—results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- Trouilloud D, Regnier J. Therapeutic education among adults with type 2 diabetes: Effects of a three-day intervention on perceived competence, self-management behaviours and glycaemic control. Global Health Promotion. 2013;20:94–98. doi: 10.1177/1757975913483331. [DOI] [PubMed] [Google Scholar]
- Vivienne Wu SF, Courtney M, Edwards H, McDowell J, Shortridge-Baggett LM, Chang PJ. Development and validation of the Chinese version of the diabetes management self-efficacy scale. International Journal of Nursing Studies. 2008;45:534–542. doi: 10.1016/j.ijnurstu.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Wagner JA, Schnoll RA, Gipson MT. Development of a scale to measure adherence to self-monitoring of blood glucose with latent variable measurement. Diabetes Care. 1998;21:1046–1051. doi: 10.2337/diacare.21.7.1046. [DOI] [PubMed] [Google Scholar]
- Wang JS, Wang RH, Lin CC. Self-care behaviors and related factors in outpatients newly diagnosed with non-insulin-dependent diabetes mellitus. J Nurs. 1998;45:60–73. [Google Scholar]
- Wang RH, Lin LY, Cheng CP, Hsu MT, Kao CC. The psychometric testing of the diabetes health promotion self-care scale. Journal of Nursing Research. 2012;20:122–130. doi: 10.1097/jnr.0b013e318254eb47. [DOI] [PubMed] [Google Scholar]
- Wang RH, Wu LC, Hsu HY. A path model of health-related quality of life in type 2 diabetic patients: A cross-sectional study in Taiwan. Journal of Advanced Nursing. 2011;67:2658–2667. doi: 10.1111/j.1365-2648.2011.05701.x. [DOI] [PubMed] [Google Scholar]
- Wang Y, Lee J, Toh MP, Tang WE, Ko Y. Validity and reliability of a self-reported measure of medication adherence in patients with Type 2 diabetes mellitus in Singapore. Diabetic Medicine. 2012;29:e338–e344. doi: 10.1111/j.1464-5491.2012.03733.x. [DOI] [PubMed] [Google Scholar]
- Weinger K, Welch GW, Butler HA, La Greca AM. Measuring diabetes self-care—A psychometric analysis of the self-care inventory-revised with adults. Diabetes Care. 2005;28:1346–1352. doi: 10.2337/diacare.28.6.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu SF, Courtney M, Edwards H, McDowell J, Shortridge-Baggett LM, Chang PJ. Self-efficacy, outcome expectations and self-care behaviour in people with type 2 diabetes in Taiwan. Journal of Clinical Nursing. 2007;16:250–257. doi: 10.1111/j.1365-2702.2006.01930.x. [DOI] [PubMed] [Google Scholar]
- Wu SF, Huang YC, Liang SY, Wang TJ, Lee MC, Tung HH. Relationships among depression, anxiety, self-care behaviour and diabetes education difficulties in patients with type-2 diabetes: A cross-sectional questionnaire survey. International Journal of Nursing Studies. 2011;48:1376–1383. doi: 10.1016/j.ijnurstu.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Xu Y, Savage C, Toobert D, Wei P, Whitmer K. Adaptation and testing of instruments to measure diabetes self-management in people with type 2 diabetes in mainland China. Journal of Transcultural Nursing: Official Journal of The Transcultural Nursing Society/Transcultural Nursing Society. 2008;19:234–242. doi: 10.1177/1043659608319239. [DOI] [PubMed] [Google Scholar]
- Yusuff KB, Obe O, Joseph BY. Adherence to anti-diabetic drug therapy and self management practices among type-2 diabetics in Nigeria. Pharmacy World & Science. 2008;30:876–883. doi: 10.1007/s11096-008-9243-2. [DOI] [PubMed] [Google Scholar]
- Zhang J, Xu CP, Wu HX, Xue XJ, Xu ZJ, Li Y, Liu QZ. Comparative study of the influence of diabetes distress and depression on treatment adherence in Chinese patients with type 2 diabetes: A cross-sectional survey in the People’s Republic of China. Neuropsychiatric Disease and Treatment. 2013;9:1289–1294. doi: 10.2147/NDT.S49798. [DOI] [PMC free article] [PubMed] [Google Scholar]