Abstract
The enactment of the Patient Protection and Affordable Care Act (ACA) has been expected to improve the coverage of health insurance, particularly as related to the coordination of seamless care and the continuity of elder care among Medicare beneficiaries. The analysis of longitudinal data (2007 through 2013) in rural areas offers a unique opportunity to examine trends and patterns of rural disparities in hospital readmissions within 30 days of discharge among Medicare beneficiaries served by rural health clinics (RHCs) in the eight southeastern states of the Department of Health & Human Services (DHHS) Region 4. The purpose of this study is twofold: first, to examine rural trends and patterns of hospital readmission rates by state and year (before and after the ACA enactment); and second, to investigate how contextual (county characteristic), organizational (clinic characteristic) and ecological (aggregate patient characteristic) factors may influence the variations in repeat hospitalizations. The unit of analysis is the RHC. We used administrative data compiled from multiple sources for the Centers of Medicare and Medicaid Services for a period of seven years. From 2007 to 2008, risk-adjusted readmission rates increased slightly among Medicare beneficiaries served by RHCs. However, the rate declined in 2009 through 2013. A generalized estimating equation of sixteen predictors was analyzed for the variability in risk-adjusted readmission rates. Nine predictors were statistically associated with the variability in risk-adjusted readmission rates of the RHCs pooled from 2007 through 2013 together. The declined rates were associated with by the ACA effect, Georgia, North Carolina, South Carolina, and the percentage of elderly population in a county where RHC is located. However, the increase of risk-adjusted rates was associated with the percentage of African Americans in a county, the percentage of dually eligible patients, the average age of patients, and the average clinical visits by African American patients. The sixteen predictors accounted for 21.52 % of the total variability in readmissions. This study contributes to the literature in health disparities research from the contextual, organizational and ecological perspectives in the analysis of longitudinal data. The synergism of multiple contextual, organizational and ecological factors, as shown in this study, should be considered in the design and implementation of intervention studies to address the problem of hospital readmissions through prevention and enhancement of disease management of rural Medicare beneficiaries.
Keywords: Rural health clinics, Affordable Care Act, Hospital readmissions, Risk-adjusted rate, Generalized estimating equation
1 Introduction
Repeated hospitalization has been identified as one of the major health care issues in the effort of monitoring and improving the quality of care. Empirical studies suggest that demographic attributes, diagnostic conditions, transfer or discharge status, health care system factors, and geographical distance to the hospital are potential risk factors for readmissions [1–6]. Little is known about how the contextual (county characteristic), organizational (clinic characteristic) and ecological (aggregate RHC patient characteristic) factors contribute to the variability in readmissions when the influence of patient characteristics is being simultaneously controlled for in the investigation.
According to Jencks et al. [7], repeated hospitalization rates of Medicare patients for all conditions ranged from 19.6 % (readmitted within 30 days of discharge from an acute care hospital) to 34 % (within 90 days of discharge). Hospital readmission rates for all conditions of Medicare beneficiaries were 19 % from 2007 through 2011 and declined to 18.5 % in 2012 as posted in MedicareCompare.gov. Brennan [8] reported the cost estimate of repeated admissions at $25 billion per year. About $17.4 billion of the cost for readmissions may be avoidable. The Centers for Medicare and Medicaid Services (CMS) has started monitoring avoidable hospitalizations and readmissions by implementing a hospital readmissions reduction program or a financial sanction plan in an attempt to mitigate this hospital quality problem. In fact, it penalized hospital reimbursements with high readmission rates for Medicare patients treated for congestive heart failure, acute myocardial infarction, or pneumonia. Beginning October 2012, Medicare payments were to decrease by 1–2 % in 2013 and by 3 % in 2014 for hospitals with high readmission rates for Medicare patients treated for congestive heart failure, acute myocardial infarction, or pneumonia. Beginning in October 2014, the readmission rate for Medicare patients with chronic obstructive pulmonary conditions was also monitored. Starting in 2015 the readmission rate for hip and knee replacements is included in the readmissions reduction program. Concomitantly, the enactment of the Patient Protection and Affordable Care Act (abbreviated as the ACA) in March 23, 2010 is expected to enhance patient-centric care and improve the delivery of ambulatory care and prevention through the expansion of health insurance coverage for the uninsured. The ACA Section 3025 will also solidify the importance of readmission reduction effort.
Research literature suggests that the severity of illness and other personal characteristics may explain the differential rates in readmissions. However, high readmission rates have been attributable to the lack of transitional care [2, 9, 10], inadequate or poor access to primary care [11, 12], and the provision of poor quality of hospital care [7, 13].
The rural health clinic (RHC) database we constructed for the seven years from 2007 through 2013 (including the pre-ACA period and the post-ACA period) offers a unique opportunity to examine trends and patterns of rural disparities in hospital readmissions in eight states of Region 4 (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee).
Two specific aims of this study are: first, to examine rural trends and patterns of hospital readmission rates by state and year (before and after the ACA enactment); and second, to investigate how contextual (county characteristic), organizational (clinic characteristic) and ecological (aggregate patient characteristic) factors may influence the variations in repeat hospitalizations, holding patient characteristics constant by employing a risk adjustment method. More specifically, three research questions relevant to the patterns and trends of repeat hospitalization of Medicare patients in selected rural areas are addressed in this empirical study when patient differences are simultaneously controlled for through statistical risk adjustment.
Have rehospitalization rates decreased over the past seven years (2007 through 2013)? Can the change be reflected by the period effect attributable to the Affordable Care Act when other influencing factors are simultaneously considered?
Can the variability in the 30-day rehospitalization rates be explained by rurality, regardless of the cause of readmission?
Do rehospitalization rates vary by demographic and socioeconomic status characteristics of the county where the RHC is located?
The present study uses time-series data from 2007 through 2013 aggregated into RHC years as the unit of analysis, using multivariate modeling analytics to identify statistically significant factors influencing the variation in risk-adjusted readmission rates. The identification of contributing factors to the high prevalence of hospital readmissions may shed some light on potential policy development or interventions targeting the mutable county characteristics (e.g., state, rurality classification, poverty, demographic characteristics, health and professional resources distribution, etc.), clinic characteristics (e.g., provider status/ownership, staff size, and health system affiliation), and aggregated RHC patient characteristics (e.g., gender, age and racial compositions, dual eligibility status and service utilization).
2 Related research
Rehospitalization is considered an important measure of hospital performance [14]. Brennan [8] reported findings from CMS research on Medicare and suggested that high rehospitalization rates represent quality problems. The CMS Hospital Readmissions Reduction Program penalizes acute care hospitals that have a higher readmission rate for older adult patients who were admitted with congestive heart failure (CHF), an acute myocardial infarction (MI), or pneumonia. Readmission following an elective hip replacement or knee replacement will be added as a performance measure to Medicare’s Hospital Compare in 2015 (www.medicare.gov).
Using 2003–2004 data, Jencks et al. [7] showed that rehospitalization rates across Region 4 (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee) varied from 18.1 % in South Carolina to 21.9 % in Mississippi. An analysis of rehospitalization rates for CHF, MI, and pneumonia using Medicare fee-for-service claims for 2007–2009 found rehospitalization rates for CHF, MI, and pneumonia of 24.8, 19.9, and 18.3 % respectively. No differences were observed based on age, gender, and race [15]. An analysis of Medicare claims data from 2005 to 2006 revealed that 22 % of readmissions occurred at a different hospital [16]. Patients from rural areas and women had a lower incidence of rehospitalization. In a recent CMS report, Brennan [8] noted that a consistent annual rate of 19 % for readmissions within 30 days of discharge was observed in the period of 2007–2011. The rate declined to 18.5 % in 2012 and 17.9 in 2013. In addition, smaller hospitals tended to have experienced a slightly faster decline in readmissions than larger hospitals.
Hospital readmissions can be further reduced with a better understanding of the determinants of readmission rates, holding patient characteristics (such as the severity of illness, comorbidity, age, gender, race/ethnicity and socioeconomic status) constant by means of risk adjustment. The present study explores how the availability of rural health clinics, the ACA period effect, rurality, dual eligibility, and many aggregated patient and organizational characteristics at the RHC level may influence the patterns and trends of risk-adjusted readmission rates for the period of 2007 through 2013.
3 Research methodology
3.1 Design and data sources
We conducted a longitudinal analysis of hospital readmissions based on administrative and claims data gathered from a variety of data sources compiled for CMS. Readmissions of rural Medicare patients (2007 through 2013) were captured in the CMS’s inpatient claims files of the Chronic Conditions Warehouse. The presence of hospital billing codes for admissions was coded as a hospitalized case (coded 1) or not-hospitalized case (coded 0). The same-day transfers were excluded from the analysis. The readmission rate for all conditions is computed by the total number of Medicare claims for readmissions within 30 days of discharge from the index stay (inpatient admission where patient did not die in a hospital) divided by the total number of index hospital claims of patients served by each RHC per year. The formulas used are as follows:
Using logistic regression analysis of the Medicare claims file with the Charlson Index and other factors as risk adjusters [17], (including age, gender, race, and other personal factors), an expected number of readmissions was calculated for each RHC per year. The risk-adjusted readmission rate was then calculated by using the expected number of readmissions (the numerator) divided by the total index hospital admissions (the denominator).
Our analysis focuses on rural disparities in RHCs so that variations in the risk adjusted rate of readmissions may be accounted for by the contextual, organizational, and ecological factors. Analyses present major characteristics of RHCs serving Medicare beneficiaries in several categories of rural areas as defined by Rural Urban Community Area (RUCA) codes.1 The rurality is classified into the urbanized, large rural, small rural, and isolated rural areas. The total rural elderly studied ranged from 202,707 patients in 2007 to 270,769 patients in 2013. Excluding the missing cases for not having the total number of patients documented in the Medicare claims file, we retained 591 RHCs for this research.
3.2 Measurements
The contextual variables, derived from the Health Resources and Services Administration (HRSA) Area Resource File, include: for example, the percentage population in poverty, rurality (in four levels), racial composition, and state. The organizational factors included, for example, years of RHC certification, staff mix (a ratio of physician visits to the total number of health clinic visits), clinical staff size, provider-based or independent clinic, and RHC ownership. Personal attributes of Medicare beneficiaries such the size of patient population served, average age of patients, percentage female patients, percentage Hispanic patients, percentage White patients, and percentage dually eligible patients are considered as aggregated indicators or ecological factors of RHCs in this analysis. In addition, a dichotomized predictor variable showing the potential period effect of the ACA on RHC performance was created: before 2010 (2007 through 2009) coded 0 and after 2009 (2010 through 2013) coded 1.
A summary of operational definitions of the study variables is presented in Appendix 1.
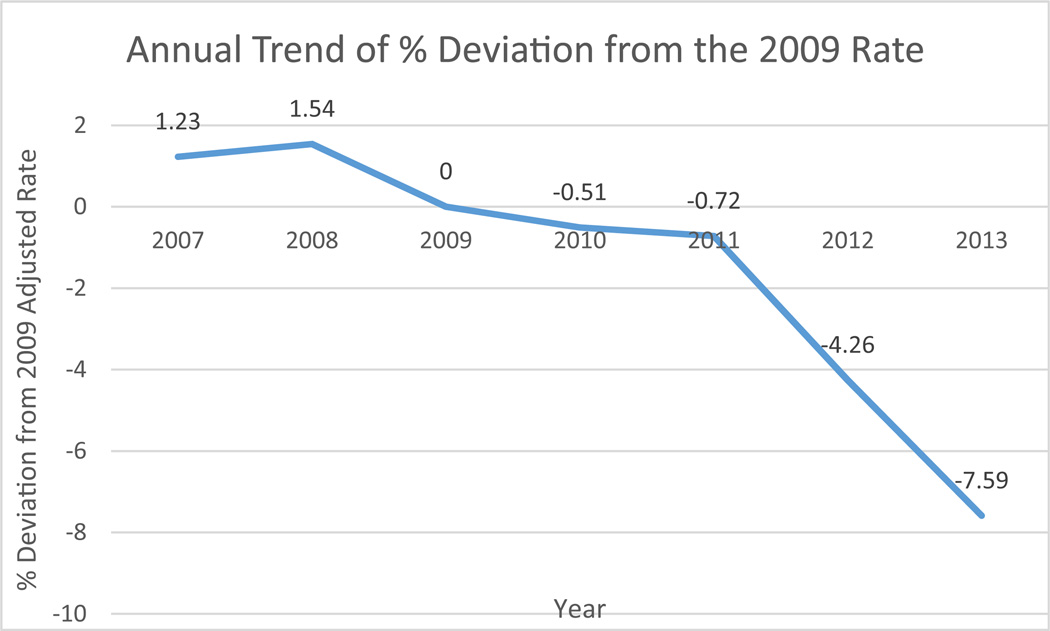
For presenting the trend of risk-adjusted readmission rates, a disparity ratio was calculated as follows: (the deviation of an annual rate from the reference average rate in 2009 divided by this reference average rate)* 100. The percentage deviation from an average rate or a norm is used to compare the changes in risk-adjusted readmission rates of RHCs. For this research, an average rate in 2009 of all study RHCs was used as a reference value so that the percentage deviation from an average rate of readmissions per year refers to the disparity: a positive value refers to a higher repeated hospitalization rate for the clinics’ Medicare beneficiaries as compared to the average RHC rate in 2009, and a negative value (lower rate) indicates performance lower repeated hospitalization rate.
Because of the problematic issue of missing values in the claims file, longitudinal data from 2007 to 2013 were pooled together in the analysis. Thus, the unit of analysis for the dependent variable is referred to as “RHC-year” with all eight states combined in seven years. The number of RHCs varied by year and by state with the largest number of RHCs located in Mississippi and the smallest number in Tennessee. The pre-ACA period consists of 2007 and 2009, whereas the post-ACA period includes 2010 through 2013.
3.2.1 Analytical methods
Three statistical methods were used to analyze the pooled data for the years 2007 to 2013; each was similar to a time-series without using a panel group of RHCs in the longitudinal analysis. First, descriptive statistics were calculated to illustrate the general characteristics of the RHCs in Region 4. Significance tests, at the alpha level of 0.05, were performed when the analysis of variance for eight states for a given attribute or variable was appropriate. Second, correlation analysis of repeated measures of hospital readmissions as well as growth curve modeling of hospital readmission rates were performed for 2007 through 2013. This enabled us to ascertain if any serial correlations of the variables exist [18]. Finally, regression of the dependent variable on selected predictors clustered into contextual, organizational and ecological variables was analyzed by a generalized estimating equation (GEE) method, using the pooled data for all RHCs with complete information for the total number of patients served and readmissions (N = 3918 RHC years) and analyzed using the SAS Institute’s GENMOD procedure.
Both time constant and time-varying predictors were included. The reasons for performing GEE to identify the relevance of selected predictors in accounting for the variability in risk-adjusted readmission rates are: 1) a repeated measure of the risk-adjusted rate of each RHC for the seven years was used as a dependent variable; 2) the predictor variables had many missing variables; 3) robust standard estimates were available for performing more consistent and accurate tests of statistical significance; and 4) Quasi-likelihood Information Criterion [QIC] was available to reflect the relative quality of the proposed model in fitting the data. A detailed statistical description of GEE used for this analysis is presented in the end of this paper.2
4 Research results
4.1 Descriptive statistical analysis
Comparing risk-adjusted hospital readmission rates of rhcs between the pre- and post-aca periods
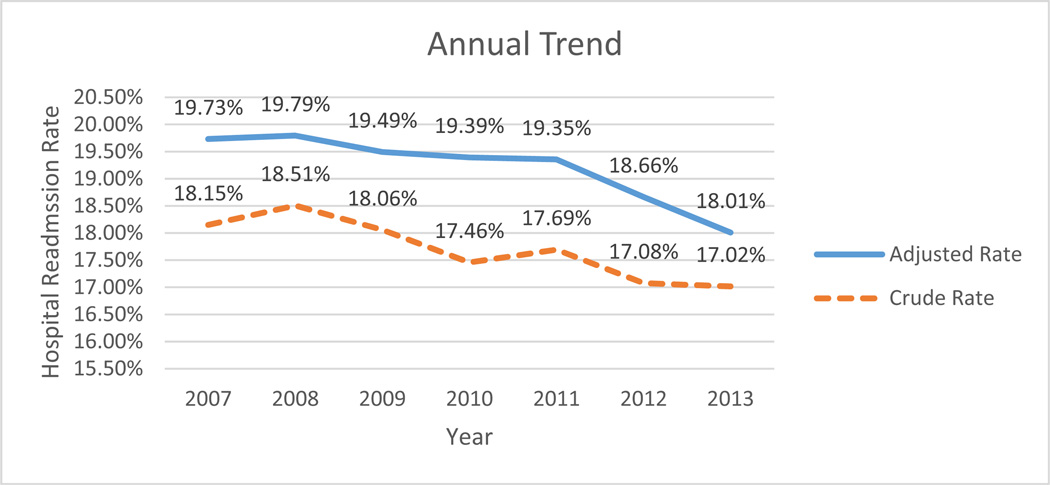
For the risk-adjusted readmission rates at the RHC level, all eight states located in Region 4 tend to have varying levels of hospital readmissions with a statistical significance at 0.001 or lower level, irrespective of year (Table 1). Lower rates were found in 2013 than in other years. Mississippi had the highest rate than other states in Region 4 for five out of seven years. North Carolina had the lowest rate for 2010 through 2013. Region 4 showed a steady decrease of risk-adjusted readmission rates from 2009 (18.49) to 2013 (18.01) with a change rate of 2.60 % (Fig. 1). One-way analysis of variance was performed to detect yearly and state variations separately. The results show that both yearly and state variations were statistically significant at 0.001 level.
Table 1.
Risk-adjusted hospital readmission rates of medicare beneficiaries in rural health clinics by state, 2007 through 2013
| State | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|---|---|---|---|
| Alabama | Mean | 19.59 % | 19.79 % | 19.46 % | 19.54 % | 19.36 % | 18.70 % | 18.29 % |
| N | 46 | 49 | 49 | 47 | 46 | 43 | 38 | |
| SD | 1.15 % | 1.26 % | 1.06 % | 1.18 % | 0.97 % | 1.00 % | 1.06 % | |
| Florida | Mean | 19.36 % | 19.40 % | 19.01 % | 19.22 % | 18.97 % | 18.35 % | 17.79 % |
| N | 85 | 82 | 79 | 78 | 80 | 78 | 75 | |
| SD | 1.13 % | 1.70 % | 0.99 % | 1.12 % | 1.09 % | 1.17 % | 1.16 % | |
| Georgia | Mean | 19.12 % | 19.39 % | 19.11 % | 19.05 % | 19.11 % | 18.25 % | 17.71 % |
| N | 62 | 63 | 60 | 58 | 57 | 55 | 54 | |
| SD | 1.03 % | 0.98 % | 1.04 % | 1.15 % | 0.98 % | 1.08 % | 1.22 % | |
| Kentucky | Mean | 19.85 % | 19.70 % | 19.45 % | 19.25 % | 19.63 % | 18.63 % | 18.00 % |
| N | 103 | 106 | 107 | 108 | 107 | 100 | 94 | |
| SD | 1.08 % | 1.00 % | 1.13 % | 1.01 % | 1.72 % | 1.04 % | 1.40 % | |
| Mississippi | Mean | 20.66 % | 20.42 % | 20.22 % | 20.02 % | 19.62 % | 19.34 % | 18.30 % |
| N | 113 | 119 | 116 | 111 | 109 | 104 | 98 | |
| SD | 1.83 % | 1.76 % | 1.76 % | 1.69 % | 1.88 % | 1.91 % | 1.75 % | |
| North Carolina | Mean | 19.15 % | 19.65 % | 19.15 % | 18.89 % | 18.78 % | 18.15 % | 17.37 % |
| N | 73 | 72 | 72 | 66 | 65 | 61 | 52 | |
| SD | 0.78 % | 0.96 % | 0.86 % | 0.87 % | 0.80 % | 0.83 % | 0.77 % | |
| South Carolina | Mean | 19.72 % | 19.86 % | 19.58 % | 19.61 % | 19.65 % | 18.96 % | 18.17 % |
| N | 60 | 60 | 61 | 60 | 60 | 57 | 54 | |
| SD | 0.80 % | 0.84 % | 1.00 % | 0.83 % | 1.01 % | 0.84 % | 0.92 % | |
| Tennessee | Mean | 19.79 % | 19.75 % | 19.54 % | 19.20 % | 19.50 % | 18.49 % | 18.57 % |
| N | 39 | 40 | 40 | 39 | 38 | 37 | 34 | |
| SD | 1.00 % | 0.81 % | 1.15 % | 1.08 % | 1.15 % | 1.17 % | 2.42 % | |
| F-value | 15.392* | 6.238* | 9.564* | 7.734* | 4.455* | 7.971* | 3.822* | |
| Significance | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | |
| N | 581 | 591 | 584 | 567 | 562 | 535 | 499 |
N number of rural health clinics, SD standard deviation
Statistically significant at 0.05 or lower level
Fig. 1.
Trend plot of risk-adjusted and crude rates for hospital readmission by year
Trends in disparity ratio of hospital readmissions
The risk-adjusted readmission rates for the patients of each RHC were compared to an average rate for 2009 in the pre-ACA period. The percentage deviations from this mean were calculated: the higher the positive value, the poorer the risk-adjusted readmission rate for the RHC’s patients is observed. The disparity trend is shown in Fig. 2: the average rate of 2013 is 7.59 percentage points lower than that of 2009. The post-ACA period (2010 through 2013) had lower risk-adjusted rates for hospital admission than the pre-ACA period.
Fig. 2.
Trend plot for disparity ratios in annual risk-adjusted hospital readmission rates as compared to 2009 by year
4.2 ANOVA of risk-adjusted readmission rates by rurality
The variation in risk-adjusted readmission rates by rurality or rural classification was examined by one-way analysis of variance for each year. Table 2 shows that statistically significant differences in the risk-adjusted readmission rates were found by rurality in 2007 through 2011; RHCs located in an urbanized area had the lowest rate than other rural categories. In general, RHCs located in both small and isolated rural areas tended to experience more readmissions than did the large or urbanized area.
Table 2.
ANOVA results for risk-adjusted hospital readmission rates by rurality, 2007 through 2013
| Rurality Classification | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | |
|---|---|---|---|---|---|---|---|---|
| Urban | Mean | 19.41 % | 19.63 % | 19.25 % | 19.25 % | 19.18 % | 18.33 % | 17.95 % |
| N | 105 | 109 | 108 | 107 | 104 | 98 | 90 | |
| SD | 1.01 % | 1.65 % | 1.13 % | 1.21 % | 1.23 % | 1.16 % | 1.61 % | |
| Large rural | Mean | 19.67 % | 19.62 % | 19.40 % | 19.30 % | 19.18 % | 18.34 % | 17.73 % |
| N | 135 | 134 | 132 | 125 | 127 | 122 | 110 | |
| SD | 1.41 % | 1.37 % | 1.44 % | 1.22 % | 1.46 % | 1.35 % | 1.39 % | |
| Small rural | Mean | 19.97 % | 19.92 % | 19.60 % | 19.46 % | 19.49 % | 18.92 % | 18.17 % |
| N | 188 | 191 | 191 | 187 | 185 | 173 | 165 | |
| SD | 1.39 % | 1.17 % | 1.27 % | 1.24 % | 1.42 % | 1.13 % | 1.41 % | |
| Isolated | Mean | 19.71 % | 19.90 % | 19.62 % | 19.49 % | 19.46 % | 18.86 % | 18.07 % |
| N | 153 | 157 | 153 | 148 | 146 | 142 | 134 | |
| SD | 1.28 % | 1.21 % | 1.20 % | 1.27 % | 1.40 % | 1.45 % | 1.35 % | |
| F-value | 4.335* | 2.228 | 2.564 | 1.173 | 2.035 | 8.393* | 2.204 | |
| Significance | 0.005 | 0.084 | 0.054 | 0.319 | 0.108 | 0.000 | 0.087 | |
| N | 581 | 591 | 584 | 567 | 562 | 535 | 499 | |
N number of rural health clinics, SD standard deviation
Statistically significant at 0.05 or lower level
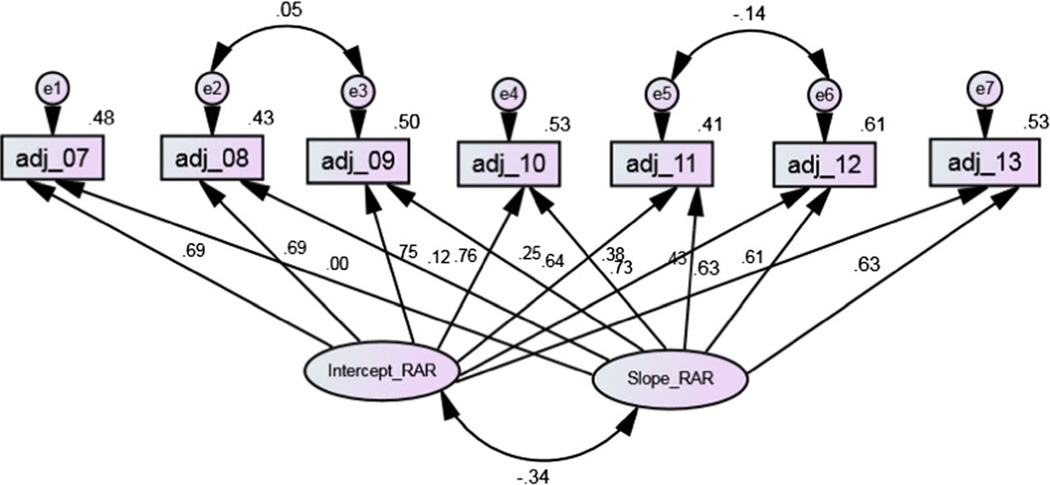
4.3 Latent growth curve modeling of risk-adjusted readmission rates (2007 through 2013)
Serial correlation is considered to be an important methodological problem that had to be addressed in this longitudinal analysis of RHC data. The rates for risk adjusted readmissions for the seven study years are moderately and positively associated. The potential threat of autoregression of the rates has to be examined in latent growth curve modeling and analysis.
Figure 3 shows a latent growth curve model for seven waves of the rates for 499 RHCs (used as a panel for the analysis) formulated to examine the relationship between the two latent growth components - the intercept (Intercept_RAR) reflecting the initial status and the slope (Slope_RAR) of yearly rates showing the trajectories of rate change. This latent growth curve model fits the data very well with a chi-square value of 46.161, 16° of freedom; NFI = 0.961, TLI = 0.955, CFI = 0.974, and RMSEA =0.075. A negative and statistically significant association of the two growth factors (intercept and slope) was found (−0.340). This suggests that the higher the readmission rate in a prior year, the slower the decline of repeated hospitalizations in later years. The relationship between each annual rate and the intercept is 0.691, 0.690, 0.748, 0.760, 0.644, 0.733 and 0.629 from 2007 through 2013, respectively. The relationship between each annual rate and the slope is 0.00, 0.116, 0.251, 0.383, 0.432, 0.615 and 0.633 for the respective years.
Fig. 3.
A latent growth curve model of risk-adjusted hospital readmission (rar) rates: 2007 through 2013
4.4 Generalized estimating equation (GEE) analysis of predictors
GEE offers a unique perspective in the examination of repeated measures such as disparities in risk-adjusted readmission rates for 3,918 RHC years. The analysis follows a two-step hierarchical regression: 1) the risk-adjusted rate, a continuous dependent variable, was regressed on each group of predictors such as the contextual, organizational and aggregate patient attributes independently; and 2) from each group of predictors, those that were statistically significant were combined in the second step of regression analysis using a backward selection method. Rurality was categorized into three dummy variables (large rural, small rural, and isolated rural areas with RHCs located in an urbanized area as a reference group) in the final regression equation. A pre-ACA year was coded 0, whereas a post-ACA year was coded 1. This dummy variable is treated as the ACA effect on readmission rates. The results of substantively meaningful and statistically significant predictors for the dependent variable are presented in Table 3. For the purpose of illustrating the relative importance of each predictor included in the analysis, we present standardized regression coefficients (parameter estimates) and relevant statistics in the table. A positive regression coefficient indicates that an increasing readmissions rate is observed. Similarly, a negative coefficient suggests that a declining average risk-adjusted readmission rate is observed for a given predictor variable. A marginal R2 for the estimating equation was also computed to show the total variance in the dependent variable explained by all predictor variables included in the final model.
Table 3.
Analysis of gee parameter estimates for predictors of risk-adjusted hospital readmission rates of rhcs (N = 3,918 RHC years)
| Parameter Estimates of Generalized Estimating Equation (GEE) | ||||||
|---|---|---|---|---|---|---|
| Predictors | Standardized Estimate |
Standard Error | 95 % Confidence Limits |
Z | Pr > |Z| | |
| Contextual: | ||||||
| ACA period effect | −0.2173 | 0.0132 | −0.2432 | −0.1914 | −16.42 | <0.0001 |
| Large rural areas | −0.0058 | 0.0290 | −0.0628 | 0.0511 | −0.20 | 0.8406 |
| Small rural areas | 0.0273 | 0.0291 | −0.0297 | 0.0844 | 0.94 | 0.3474 |
| Isolated rural areas | 0.0387 | 0.0303 | −0.0207 | 0.0981 | 1.28 | 0.2014 |
| Alabama | −0.0380 | 0.0237 | −0.0846 | 0.0085 | −1.60 | 0.1092 |
| Florida | −0.0527 | 0.0369 | −0.1251 | 0.0197 | −1.43 | 0.1535 |
| Georgia | −0.1718 | 0.0269 | −0.2246 | −0.1190 | −6.38 | <0.0001 |
| Kentucky | 0.0242 | 0.0345 | −0.0434 | 0.0919 | −0.70 | 0.4827 |
| North Carolina | −0.1344 | 0.0260 | −0.1854 | −0.0834 | −5.16 | <0.0001 |
| South Carolina | −0.0852 | 0.0289 | −0.1419 | −0.0285 | −2.94 | 0.0032 |
| Tennessee | 0.0103 | 0.0268 | −0.0422 | 0.0628 | 0.38 | 0.7005 |
| % African Americans in county | 0.2114 | 0.0381 | 0.1368 | 0.2860 | 5.55 | <0.0001 |
| % Elderly in county | −0.0654 | 0.0246 | −0.1137 | −0.0171 | −2.66 | 0.0079 |
| Aggregated RHC or ecological: | ||||||
| % Dually eligible | 0.1224 | 0.0261 | 0.0712 | 0.1737 | 4.68 | <0.0001 |
| Average age of patients | 0.1196 | 0.0294 | 0.0620 | 0.1772 | 4.07 | <0.0001 |
| RHC use by native american patients | −0.0250 | 0.0126 | −0.0497 | −0.0002 | −1.98 | 0.0478 |
Marginal R-squared =0.2152; QIC = 3975; QICU =3936
Z- statistics greater or equal to 1.96 are statistically significant at 0.05 level
Table 3 reveals several interesting and statistically significant findings from the GEE analysis as follows: 1) the variable “ACA period” had a statistically inverse relationship with the readmissions rate for RHC patients, showing lower readmission rates of the post-ACA period than the pre-ACA period; 2) the risk-adjusted readmission rates did not vary by rurality; 3) Georgia, North Carolina and South Carolina had a lower rates than other southeastern states; 4) RHCs located in area with higher percentage of African Americans had a higher risk-adjusted rate of readmissions; 5) RHCs located in an area with high percentage of elderly had a lower rate; 6) the percentage of the dually eligible and the average age of patients treated by RHCs were positively related to the risk-adjusted rate; and 7) the utilization rate of RHCs by Native American patients was negatively related to the risk-adjusted readmission rate. The total variance explained by the sixteen predictors shown by the marginal R-squared value is 21.52 %.
5 Discussion
The analysis of RHC data with seven years of observation provides insights to the variability in readmission rates among rural Medicare beneficiaries. The findings of this empirical study offer specific answers to each of the three research questions.
First, rehospitalization rates decreased over the past years, particularly in 2012 and 2013. This changing pattern of hospital readmission rates reflects the potential period effect attributable to the Affordable Care Act when personal risk factors for rehospitalization are simultaneously considered. Both risk-adjusted and unadjusted rates of readmission showed a steady increase from 2007 to 2008 although the speed of increase was relatively small. The latent growth curve model offered more substantive explanation in regard to the nature of hospital readmission rates. Because of the interdependence of the yearly rates, the change trajectories of readmissions had to be carefully considered in a thorough analysis of the contextual, organizational and ecological predictors of the variation in readmissions. Careful analysis of sixteen predictor variables with the generalized estimating equation method revealed that a moderate amount of variance (marginal R2 = 0.2152) in the risk-adjusted readmission rates was accounted for by the predictor variables. In addition, the ACA period effect (with the strongest regression coefficient of −0.2173 relative to other predictors) on readmission rates was also observed when other predictors were simultaneously considered; the post-ACA years had lower readmission rates than the pre-ACA years. Because the decline in post-ACA years may be seen from multiple perspectives, system-based efforts to reduce readmissions are likely, rather than just improvements in certain hospital treatment for specific diseases. The community-based providers such as RHCs or community health centers may also focus on ways to lower readmissions of their patients. Thus, RHC effort may have contributed to the regional decline in the risk-adjusted readmission rates.
Second, the 30-day risk-adjusted rehospitalization rate did not vary significantly by categories of rural areas, regardless of the cause of readmission for five of the seven years (except for 2007 and 2012) in a preliminary analysis without controlling for the effects of other predictors on the variability. RHCs located in smaller and isolated rural areas appear to have a slightly higher readmission rate than large or urbanized area. The finding on the variation by rurality was further examined by multivariate analysis, holding other predictor variables constant. No statistically significant variations by rurality were found.
Third, demographic and socioeconomic factors measured by the county-area characteristics and aggregate patient factors of RHCs appear to be relevant in explaining the variability in risk-adjusted rehospitalization rates. More specifically, the percentage of the dually eligible reflects the relatively poor socioeconomic level and health status of Medicare patients served by RHCs. This variable was positively and statistically significantly associated with the rate of readmissions. It is interesting to note that the other aggregated patient attribute, such as the average number of RHC visits by Native Americans, was negatively associated with the risk-adjusted rate.
These empirical findings are relatively robust since our analyses are based on GEE analysis of longitudinal data with a risk adjustment method to remove patient differences in RHCs. However, this study may be subject to a few methodological limitations. First, the unit of analysis based on RHC year was measured by hospital admission and readmission claims of Medicare patients. The measurement was based on episodes or events of the interest. We cannot infer how the variability in hospital practices in RHC service areas may have contributed to the disparities in readmissions.
Second, the contextual, organizational and ecological factors are those associated with RHCs, not hospitals. Our interest is to determine how the RHC and community area characteristics, reflecting the county, and aggregated RHC patient attributes, may account for the variability in readmissions in multiple RHC years.
Third, because the purpose of this investigation is to focus on the variability in the readmission rates, identification of RHCs with substantially higher rates than an average rate in 2009 can portray the need for further enhancement of their ambulatory or primary care services needed for the specific groups of RHCs. We were unable to explore the full picture of regional variation in hospital readmissions among RHCs in the United States because our data were restricted to the eight southeastern states in Region 4.
Fourth, the severity of illness is an important need-for-care indicator that is predictive of health services use. The present study employed a variable “ercentage of patients with multiple chronic conditions” in the GEE analysis of risk-adjusted readmission rates. However, it was not statistically significant. Because the statistical distribution of this variable showed little variation in RHCs, this may have contributed to the lack of relevance to readmissions. Future research should consider the development and use of more sensitive case-mix indexes or the severity of illness of rural Medicare beneficiaries as predictor variables.
Lastly, the study did not include any supply-side variables such as hospital market competition, travel distance from RHC to a nearest hospital, and types of hospital in the model. Alternatively, a two-level multivariate analysis could be performed to include the interaction terms between patient-and community-level predictor variables in the analysis of hospital readmissions. Furthermore, other efforts such as community support for fostering transitional care or post-discharge care through disease management or coordinated care may also be relevant to the declined trend of rehospitalization.
This investigation has enlightened us about the lack of significant variability in hospital readmission rates by rurality since the risk-adjusted rates of rehospitalization did not vary by classification of rural areas when other predictors were simultaneously considered in a multivariate analysis. Future studies should address the variation in types of ambulatory care sensitive conditions of RHC patients. In addition, the effectiveness in detecting the underlying causes or mechanisms for the disparities of hospital readmissions and in implementing feasible organizational or community interventions should be further explored in future rural health research.
6 Conclusion
Our study identifies potential contextual, organizational and ecological factors influencing the variations in hospital readmission rates. The readmission rates of rural Medicare beneficiaries varied by year and by state. There was a steady decline in hospital readmissions of Medicare patients in the eight states from 2009 through 2013. The CMS Hospital Readmissions Reduction Program and other quality improvement initiatives in addition to the ACA effect may account for the rate decline in 2012 and 2013. In order to disentangle the co-variations or synergistic effects of both ACA and Readmissions Reduction Program, researchers have to design and conduct thorough studies to investigate hospital practice variations in rural areas with multiple years.
This study contributes to the literature in health disparities research from the contextual, organizational and ecological perspectives through the analysis of longitudinal data. The results reveal that it is not a single operative factor alone influencing the variations in risk-adjusted readmission rates, although race does play an important role [24]. The general structural characteristics of RHCs such as size, age in operations, staff mix, and provider status/ownership did not account for any statistically significant variability in the readmission rates.
The synergism of multiple contextual and ecological (aggregated patient characteristics of RHCs) factors, as shown in this study, should be considered in the design and implementation of Medicare rehospitalization intervention studies. Our results also affirm the importance of considering county (area demographic) characteristics, and RHC-based ecological factors in accounting for the variability in hospital readmissions (6). The variables measured at the county level, such as area-wide socioeconomic and demographic characteristics, and at the RHC level, such as the dual eligibility status, average patient age and utilization of services by racial groups, should be considered as risk adjusters in the formulation of hospital incentive payment formula in the future.
The results of this study also reaffirm some of the current research literature regarding the factors associated with hospital readmissions [25, 26]. Furthermore, an evidence-based approach to guiding effective and efficient changes in readmission practices coupled with the use of community-based care modalities, such as transitional care and mobile health care management technologies, should be carefully formulated.
Acknowledgments
Research in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number U24MD006954. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix 1
Table 4.
The study variables and their operational definitions
| Variable | Codes | Operational Definition |
|---|---|---|
| Contextual Factors or County Characteristic Variables | ||
| % population in poverty | % of county population that is at 200 % of poverty level | |
| % African American population | % of county population that is African-American | |
| % Hispanic population | % of county population that is Hispanic | |
| %Native American | % of county population that is Native American | |
| %White | % of county population that is White | |
| Rurality classification | 1: urban 2: large rural 3: small rural 4: isolated. |
Four categories based on RUCA code: urban, large rural, Small rural, isolated. |
| Urban: 1.0, 1.1, 2.0, 2.1, 3.0, 4.1, 5.1, 7.1, 8.1, 10.1; Large rural: 4.0, 4.2, 5.0, 5.2, 6.0, 6.1; Small rural: 7.0, 7.2, 7.3, 7.4, 8.0, 8.2, 8.3, 8.4, 9.0, 9.1, 9.2; Isolated: 10.0, 10.2, 10.3, 10.4, 10.5, 10.6. RHC located in urbanized area is a reference variable when rurality levels are treated as dummy variables | ||
| Region 4 states | 1. Alabama 2: Florida 3: Georgia 4: Kentucky 5: Mississippi 6: North Carolina 7: South Carolina 8: Tennessee |
U.S state. Seven dummy variables for the states are used with Mississippi as a reference variable. |
| ACA period effect | 0: before 2010 (2007 through 2009) 1: after 2009 (2010 through 2012) |
The potential period effect of Affordable Care Act on RHC performance |
| Organizational factors or Clinic Characteristic Variables | ||
| Years of RHC operation | Number of years Medicare certified for the participation in RHC program | |
| Staff size | Number of physician + physician assistant + nurse practitioner FTEs | |
| Provider-based practice | 1 = Provider-based RHC 0 = Independent RHC |
RHC type |
| Aggregate RHC Characteristics or Ecological Variables | ||
| Size of Medicare beneficiaries served | Total Medicare patients served by the RHC | |
| % Female patients served | Number of patients aged 65 & older who are female (expressed as a percentage of total patients) | |
| Average patient age of a clinic | Mean age of RHC patients (years) | |
| % African-American patients served | Number of patients aged 65 & older who are African-American (expressed as a percentage of total patients) | |
| % Patients with a dually eligible status | % of Medicare program beneficiaries with at least 3 dually eligible months within one year with both Medicare and Medicaid | |
| Utilization of RHCs by Native Americans | Average number of RHC visits by Native Americans | |
| % Patients with multiple chronic conditions | Average percentage of patients with multiple chronic conditions | |
Footnotes
The RUCA is a classification scheme that uses the Bureau of Census Urbanized Area and Urban
Cluster definitions in combination with work commuting information to characterize U.S.
Census tracts regarding their rural and urban status.
Generalized estimating equation (GEE) method provides a semi-parametric approach to longitudinal analysis of categorical or continuous (repeated) measurements. GEE’s were introduced by Liang and Zeger [19] and expanded in a book by Diggle, Liang and Zeger [20]. The covariance structure does not need to be specified correctly to estimates regression coefficients and standard errors. The statistical assumptions are as follows: 1) The repeated measures or responses to be correlated or clustered; 2) covariates with a mixture of predictor variables and their interaction terms; 3) no requirement for equal variance or homogeneity of variance; 4) correlated errors assumed independent; 5) not required for multinormal distribution; and 6) a quasi-likelihood estimation rather than maximum likelihood estimation or ordinary least squares to estimate the parameters [21]. The robustness of a GEE model is not determined by conventional goodness of fit statistics. However, an analogous to the Akaike’s Information Criterion (AIC) such as QIC (Quasi-likelihood under the Independence Model Criterion) is used to assess the competing models for varying correlation structures. A marginal R-squared value can be computed to be used as a reference to the magnitude of the total variance explained by predictor variables in the equation [22, 23].
In this report, the GEE model was performed by using SAS with the PROC GENMOD procedure. The model fitting and link function were based on the link function of identity (change nothing in a dependent variable) with an assumption of a normal distribution. The assumption on correlated errors between seven levels of time points or waves on a dependent variable was set to AR(1), which means the following:
We performed hierarchical regression of a continuous response variable on the contextual, organizational and personal predictors separately and kept statistically significant variables for the final equation. When we included them together in the final model, we added additional fixed variables such as year (1 to 6), dummy variables for seven states (using Mississippi as a reference group), and rurality code (three dummy variables using RHC located in urbanized areas as a reference group). The backward selection criterion was used to enter the statistically significant predictors one-by-one at the alpha of 0.1.
References
- 1.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160(8):1704–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 2.Jackson CT, Trygstad TK, DeWalt DA, DuBard CA. Transitional care cut hospital readmissions for North Carolina Medicaid patients with complex chronic conditions. Health Aff (Millwood) 2013;32(8):407–415. doi: 10.1377/hlthaff.2013.0047. [DOI] [PubMed] [Google Scholar]
- 3.Joynt E, Orav JE, Jha AK. Thirty-day readmission rates for medicare beneficiaries by race and site of care. JAMA. 2011;305(7):675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kulkarni P, Smith LD, Woeltje KF. Assessing risk of hospital readmissions for improving medical practice. Health Care Manage Sci. 2015 doi: 10.1007/s10729-015-9323-5. [DOI] [PubMed] [Google Scholar]
- 5.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a medicare managed care plan. Amer J Med. 1999;107:13–17. doi: 10.1016/s0002-9343(99)00159-x. [DOI] [PubMed] [Google Scholar]
- 6.Herrin J, St Andre J, Kenward K, Joshi MS, Audet AJ, Hines SC. Community factors and hospital readmission rates. Health Serv Res. 2015;50(1):20–39. doi: 10.1111/1475-6773.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jencks SF, Williams V, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-services program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 8.Brennan N. Real-time reporting of Medicare readmissions data. Washington, D.C: Centers for Medicare and Medicaid Services; 2014. [Google Scholar]
- 9.Golden A, Ortiz J, Wan TTH. Transitional care: looking for the right shoes to fit elderly patients. Care Manag J. 2013;14(2):1–6. doi: 10.1891/1521-0987.14.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mor V, Besdine RW. Policy options to improve discharge planning and reduce hospitalization. JAMA. 2011;305(3):302–303. doi: 10.1001/jama.2010.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joynt K, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. JAMA. 2011;306(1):45–52. doi: 10.1001/jama.2011.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCall NT, Brody E, Mobley L, Subramanian S. Investigation of increasing rates of hospitalization for ambulatory care sensitive conditions among Medicare fee-for-services beneficiaries. RTI International. A contract report submitted to the Centers for Medicare and Medicaid Services, Durham. 2004 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Reports/Downloads/McCall_2004_3.pdf.
- 13. Medicare.gov. 30-Day Death and Readmission Measures. Available at http://www.medicare.gov/hospitalcompare/Data/30-day-measures.html.
- 14.Horwitz L, Lin Z, Herrin J, Bernheim S, Drye EE, Krumholz HM, Hines HJ, Jr, Ross JS. Association of hospital volume with readmission rates: a retrospective cross-sectional study. BMJ. 2015;350:h447. doi: 10.1136/bmj.h447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dharmarajan K, Hsieh A, Lin Z, Bueno H, Ross JS, Horowitz LI, Barreto-Filho JA, Ki N, Bernheim SM, Suter LG, Dry EE, Krumholz HM. Diagnosis and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kind AJH, Bartels C, Mell MW, Mullahy J, Smith M. For profit hospital status and rehospitalizations at different hospitals: an analysis of Medicare data. Ann Intern Med. 2010;153(11):718–727. doi: 10.1059/0003-4819-153-11-201012070-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical co-morbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 18.Wan TTH. Evidence-Based Health Management: Multivariate Modeling Approaches. Boston: Kluwer Academic Publishers; 2002. [Google Scholar]
- 19.Liang KY, Zeger S. Longitudinal Data Analysis Using Generalized Linear Models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- 20.Diggle PJ, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford, United Kingdom: Oxford University Press; 1994. [Google Scholar]
- 21.Hu J, Gonsahn MD, Nerenz DR. Socioeconomic status and readmissions: evidence for an urban teaching hospital. Health Aff (Millwood) 2014;33(5):778–785. doi: 10.1377/hlthaff.2013.0816. [DOI] [PubMed] [Google Scholar]
- 22.Zheng B. Summarizing the goodness of fit on generalized linear models for longitudinal data. Stat Med. 2000;19:1265–1275. doi: 10.1002/(sici)1097-0258(20000530)19:10<1265::aid-sim486>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 23.Hardin JW, Hilbe JM. Generalized estimating equations. Boca Raton: Chapman and Hall/CRC Press; 2003. [Google Scholar]
- 24.Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57(8):1152–1173. doi: 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Negasako EM, Reidhead M, Waterman B, Dunagan WC. Adding socioeconomic data to hospital readmission calculations may produce more useful results. Health Aff. 2014;33(5):786–791. doi: 10.1377/hlthaff.2013.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Hospital Association. Rethinking the hospital readmissions reduction program. March, Chicago: American Hospital Association; 2015. [Google Scholar]