Abstract
[Purpose] To determine the effects of lumbar stabilization exercise with thoracic extension exercise on chronic low back pain patients. [Subjects and Methods] Thirty patients with chronic low back pain were randomly divided into a lumbar stabilization exercise group (group A) and a lumbar stabilization exercise with thoracic extension exercise group (group B). Group B did 15 min of lumbar stabilization exercises and 15 min of thoracic extension exercises, while group A did 30 min of lumbar stabilization exercises five times a week for 4 weeks. For assessing lumbosacral alignment, the lordotic angle, lumbosacral angle, and sacral angle were evaluated. The Oswestry disability index was used for assessment of disability due to low back pain. [Results] Both groups showed improvement in lumbosacral alignment and in the disability index. Group B showed greater changes in the lordotic angle and in the Oswestry disability index than group A, although the differences were not statistically significant. [Conclusion] Lumbar stabilization exercise with thoracic extension exercise can be recommended for improvement of chronic low back pain, although the improvements seen in lumbosacral alignment and low back pain disability index in this study did not achieve statistical significance.
Key words: Lumbar stabilization exercise, Thoracic extension exercise, Lumbosacral alignment
INTRODUCTION
Low back pain is one of the most widespread disorders in modern societies. It can limit the daily activities of patients, and the cost of management can be considerable1). The causes of low back pain are varied and complex, should be dealt with from various viewpoints2). Socioenvironmental factors as well as personal constitution and habits can all play a part in the etiology of low back pain3). In recent studies, low back pain has been shown to be caused by weakness of the deep muscles of the lumbar region, reduction in postural sense and kinesthetic ability due to imbalance, and reduced proprioceptive sense. These factors result in an unstable spine and lead to recurrence of low back pain4). Bae et al.5) reported that exercise on an unstable surface was better for enhancing the size of the trunk muscles and improving balance ability than exercise on a stable surface. Selective exercises for the deep abdominal muscles and lumbar stabilization exercises could thicken the transversus abdominis, which is a deep abdominal muscle, and thereby help in adjusting posture and stabilizing the trunk6).
Chronic low back pain can cause postural problems due to pelvic torsion and lumbar lordosis, both of which lead to repeated attacks of low back pain7). Disorder of proprioceptive sensibility has been reported to occur due to incorrect alignment8, 9). Poor proprioceptive sensibility and somesthesia, as well as diminished vision, combine to cause disorder of balance control10). Recent studies on the treatment of low back pain have focused on the stabilization provided by strengthening of the deep muscles in the lumbar spine and pelvis. Trunk movement patterns can be altered by changing trunk muscle activities or lengths11). The current study aimed to determine the effects of thoracic extension exercise in improving lumbosacral alignment and relieving low back pain.
SUBJECTS AND METHODS
This double-blind, randomized clinical trial was conducted with 30 patients who were admitted to a clinic inside H Company or a physiotherapy clinic in H Hospital for complaints of low back pain for more than 3 months. All participants gave written informed consent for inclusion in the study. The subjects were divided into a lumbar stabilization exercise group (group A; n = 15) and a lumbar stabilization exercise with thoracic extension exercise group (group B; n =15). The mean age, mean height, and mean weight in group A were 39.8 years, 165.5 cm, and 64.9 kg, respectively vs 40.1 years, 165.8 cm, and 64.5 kg, respectively, in group B; these differences were not statistically significant.
Each group performed their respective exercises regularly for 4 weeks. The changes in the lumbosacral alignment and low back pain disability index (Oswestry disability index; ODI)12, 13) were measured and compared between the groups after the intervention as well as within the groups before and after the intervention. The lumbar stabilization exercise consisted of previously studied exercises14,15,16,17,18); the exercise methods proposed by Hur et al.19) were referred to as the thoracic extension exercise. In both groups, the exercise program began with a 5-min warm-up session of stretching; this was followed by 30 min of stabilization exercises and thoracic extension exercise, and ended with a 5-min cool-down session (Table 1)
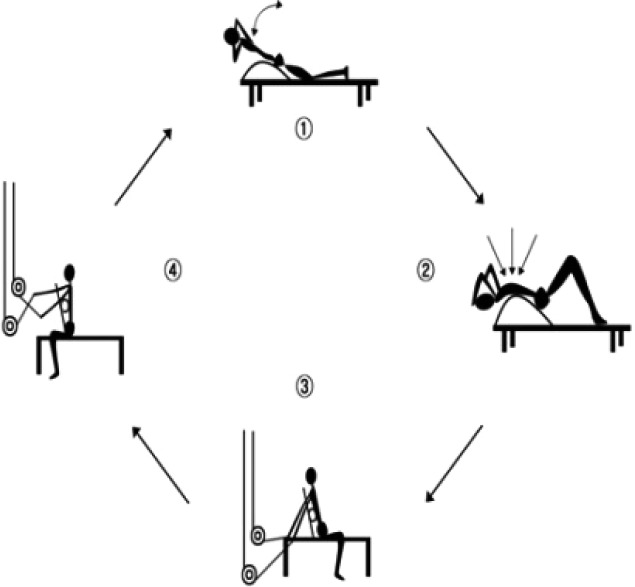
Fig. 1.
Thoracic extension exercise
.
Table 1. Lumbar stabilization exercise and thoracic extension exercise program.
| Type | Program | Time taken |
|---|---|---|
| Warm-up exercise | General stretching | 5 min |
| Lumbar stabilization exercise | 1. Lower extremity lifting in a bridge posture 3. Lower extremity lift in a prone position on a ball 4. Upper extremity lift in a prone position on a ball 5. Moving the body forward grasping a sling in a kneeling position 6. Lifting the buttocks with the lower extremity hooked on a sling in a supine position |
Group A; 30 min (10–12 times× 4 sets) Exercise time per set (30–40 s) Group B; 15 min (10–12 times × 2 sets) Exercise time per set (30–40 s) |
| Thoracic extension exercise | Fig. 1. | Group B; 15 min (10–12 times × 2 sets) Exercise time per set (30–40 s) |
| Cool-down exercise | General stretching | 5 min |
| Total | 40 min | |
Group B: Lumbar stabilization exercise with thoracic extension exercise group; Group A: Lumbar stabilization exercise group
To assess lumbosacral alignment, lateral radiographs of the lumbosacral spine in the standing position were taken; all radiographs were taken by the same radiographer. Many methods have been used to measure lumbosacral alignment. In this study, we used the method proposed by Wiltse et al., which uses the lordotic angle (LA), lumbosacral angle (LSA), and sacral angle (SA) for measuring changes in lumbosacral alignment20). The ODI was used to evaluate disability due to low back pain.
The independent t test was used to perform a homogeneity analysis between the groups before and after the intervention and the paired t test was used to analyze the changes in the variables before and after exercise. PASW for Windows (ver. 18.0) was used for the statistical analysis. The significance level (p) was set to 0.05.
RESULTS
In the within-group comparison of the variables before and after the intervention, both groups showed significant increases in LA, LSA, SA, and ODI after 4 weeks of exercise (p < 0.05; Table 2).
Table 2. Lumbosacral alignment and ODI index pre- and postintervention (N = 30).
| Variable | Group | Preintervention (mean ± SD) | Postintervention (mean ± SD) |
|---|---|---|---|
| Lordotic angle (°) | Group B* | 24.3 ± 4.9 | 28.0 ± 3.5 |
| Group A* | 26.0 ± 7.0 | 27.0 ± 6.7 | |
| Lumbosacral angle (°) | Group B* | 17.1 ± 4.0 | 15.1 ± 3.1 |
| Group A* | 15.7 ± 4.7 | 13.5 ± 3.4 | |
| Sacral angle (°) | Group B* | 37.2 ± 5.0 | 33.8 ± 2.7 |
| Group A* | 34.1 ± 6.3 | 31.3 ± 4.3 | |
| ODI (%) | Group B* | 40.4 ± 9.4 | 23.0 ± 6.0 |
| Group A* | 36.7 ± 5.4 | 23.9 ± 7.6 | |
*p < 0.05. Group B: lumbar stabilization exercise with thoracic extension exercise group; Group A: lumbar stabilization exercise group
There were no significant differences between the groups before the intervention. After the intervention, group B showed greater increase in LA and less decrease in LSA, SA, and ODI than group A; however, the differences were not statistically significant (Table 3).
Table 3. Comparison between the groups pre- and postintervention (N = 30).
| Variables | Stage | Group B (mean ± SD) | Group A (mean ± SD) |
|---|---|---|---|
| Lordotic angle (°) | Preintervention | 24.3 ± 4.9 | 26.0 ± 7.0 |
| Postintervention | 28.0 ± 3.5 | 27.0 ± 6.7 | |
| Lumbosacral angle (°) | Preintervention | 17.1 ± 4.0 | 15.7 ± 4.7 |
| Postintervention | 15.1 ± 3.1 | 13.5 ± 3.4 | |
| Sacral angle (°) | Preintervention | 37.2 ± 5.0 | 34.1 ± 6.3 |
| Postintervention | 33.8 ± 2.7 | 31.3 ± 4.3 | |
| ODI (%) | Preintervention | 40.4 ± 9.4 | 36.7 ± 5.4 |
| Postintervention | 23.0 ± 6.3 | 23.9 ± 7.6 | |
Group B: lumbar stabilization exercise with thoracic extension exercise group; Group A: lumbar stabilization exercise group
DISCUSSION
The lumbosacral region in the spine experiences large applied momentum. The region is not stable and therefore the ligaments, muscles, and joints in the region are prone to injury because of incorrect posture, trauma, and disease. Many structural changes in alignment can occur, which are closely related to low back pain21). The relationship between lumbar lordosis and low back pain has been a controversial for a long time, and researchers have reported different conclusions. Some researchers have said that low back pain is related to increase in lumbar lordosis7), whereas others have claimed that low back pain is related to decreases in lumbar lordosis22). One study has found no correlation between low back pain and lumbar lordosis23). In this study, significant increase in LA was seen in both exercise groups: from 26.01° to 26.99° in group A and from 24.27° to 28.02° in group B. After the intervention, there was no significant difference in LA between the two groups; however, the increase was much greater in group B (3.75° in group B vs. 0.98° in group A). This result is consistent with previous studies where normal people had larger increases in lumbar lordosis than patients with low back pain21, 24). Other studies have suggested that thoracic curves are affected by weight load and motion types, and that the greater the thoracic stiffness, the more movements there are in the lumbar and cervical spine because of a compensatory action, which is a mechanical change in the thoracic vertebral region morphologically25). A previous study has reported that as age increases, women tend to develop more severe lumbar lordosis than men26). A study on growing children and adolescents also found that the lumbar lordotic angle increased from 25° at age 7 to 38° at age 19—an increase of 0.58° every year27). The lumbar lordosis that develops with age involves more of the upper lumbar vertebrae28). The present study showed that thoracic extension exercise affected the recovery of lumbar lordosis, which was curved in the upper lumbar vertebrae.
One study has reported that patients with low back pain have greater SAs than normal persons29). In the present study, the SA decreased from 34.08° to 31.25° in group A and from 37.25° to 33.81° in group B, which is consistent with previous findings. The recovery of the normal sacrum range because of the lumbar stabilization exercise, and the recovery of the upper lumbar lordosis because of the thoracic extension exercise, reduced the sacrum’s excessive inclination.
Many previous studies have reported reduction in the ODI after lumbar stabilization exercises30, 31). In the present study, both groups had significant reductions in ODI: from 36.74% to 23.85% in group A and from 40.44% to 22.96% in group B. No significant difference was found between the two groups after 4 weeks of exercise, but the change in ODI was greater in group B than in group A (17.48% in group B vs. 12.89% in group A).
This study has some limitations. The intervention duration was rather short at 4 weeks. Earlier studies have used different methods to measure the lumbosacral region, so there were large differences in the measured angles in terms of comparison and analysis. In a future study, we intend to measure changes in the thoracic kyphosis angle after thoracic extension exercise and analyze changes in the segmental angles in the upper lumbar vertebrae.
REFERENCES
- 1.O’Sullivan PB: Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. Man Ther, 2000, 5: 2–12. [DOI] [PubMed] [Google Scholar]
- 2.Graves JE, Webb DC, Pollock ML, et al. : Pelvic stabilization during resistance training: its effect on the development of lumbar extension strength. Arch Phys Med Rehabil, 1994, 75: 210–215. [PubMed] [Google Scholar]
- 3.Risch SV, Norvell NK, Pollock ML, et al. : Lumbar strengthening in chronic low back pain patients. Physiologic and psychological benefits. Spine, 1993, 18: 232–238. [PubMed] [Google Scholar]
- 4.O’Sullivan PB, Burnett A, Floyd AN, et al. : Lumbar repositioning deficit in a specific low back pain population. Spine, 2003, 28: 1074–1079. [DOI] [PubMed] [Google Scholar]
- 5.Bae SH, Lee HG, Kim YE, et al. : Effects of trunk stabilization exercises on different support surfaces on the cross-sectional area of the trunk muscles and balance ability. J Phys Ther Sci, 2013, 25: 741–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee JS, Kim TH, Kim DY, et al. : Effects of selective exercise for the deep abdominal muscles and lumbar stabilization exercise on the thickness of the transversus abdominis and postural maintenance. J Phys Ther Sci, 2015, 27: 367–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christie HJ, Kumar S, Warren SA: Postural aberrations in low back pain. Arch Phys Med Rehabil, 1995, 76: 218–224. [DOI] [PubMed] [Google Scholar]
- 8.Descarreaux M, Blouin JS, Teasdale N: Repositioning accuracy and movement parameters in low back pain subjects and healthy control subjects. Eur Spine J, 2005, 14: 185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dolan KJ, Green A: Lumbar spine reposition sense: the effect of a ‘slouched’ posture. Man Ther, 2006, 11: 202–207. [DOI] [PubMed] [Google Scholar]
- 10.Brumagne S, Cordo P, Verschueren S: Proprioceptive weighting changes in persons with low back pain and elderly persons during upright standing. Neurosci Lett, 2004, 366: 63–66. [DOI] [PubMed] [Google Scholar]
- 11.Kavcic N, Grenier S, McGill SM: Quantifying tissue loads and spine stability while performing commonly prescribed low back stabilization exercises. Spine, 2004, 29: 2319–2329. [DOI] [PubMed] [Google Scholar]
- 12.Sakulsriprasert P, Vachalathiti R, Vongsirinavarat M, et al. : Cross-cultural adaptation of modified Oswestry Low Back Pain Disability Questionnaire to Thai and its reliability. J Med Assoc Thai, 2006, 89: 1694–1701. [PubMed] [Google Scholar]
- 13.Fairbank JC, Pynsent PB: Oswestry disability index. Spine, 2000, 25: 2940–2952, discussion 2952. [DOI] [PubMed] [Google Scholar]
- 14.Yoo WG: Comparison of the isolated contraction ratios of the hip extensors and erector spinae muscles of the lumbar region and thoracic muscles during different back extension exercises. J Phys Ther Sci, 2015, 27: 315–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lehman GJ, Hoda W, Oliver S: Trunk muscle activity during bridging exercises on and off a Swiss ball. Chiropr Osteopat, 2005, 13: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marshall P, Murphy B: Changes in muscle activity and perceived exertion during exercises performed on a swiss ball. Appl Physiol Nutr Metab, 2006, 31: 376–383. [DOI] [PubMed] [Google Scholar]
- 17.McGill SM, Karpowicz A: Exercises for spine stabilization: motion/motor patterns, stability progressions, and clinical technique. Arch Phys Med Rehabil, 2009, 90: 118–126. [DOI] [PubMed] [Google Scholar]
- 18.Stevens VK, Bouche KG, Mahieu NN, et al. : Trunk muscle activity in healthy subjects during bridging stabilization exercises. BMC Musculoskelet Disord, 2006, 7: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hur JG, Song JC, No YM, et al. : Effect on active exercise programs in employees with chronic low back pain. Korean J Occup Environ Med, 2005, 17: 44–57. [Google Scholar]
- 20.Wiltse LL, Winter RB: Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am, 1983, 65: 768–772. [PubMed] [Google Scholar]
- 21.Jackson RP, McManus AC: Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine, 1994, 19: 1611–1618. [DOI] [PubMed] [Google Scholar]
- 22.Tsuji T, Matsuyama Y, Sato K, et al. : Epidemiology of low back pain in the elderly: correlation with lumbar lordosis. J Orthop Sci, 2001, 6: 307–311. [DOI] [PubMed] [Google Scholar]
- 23.Tüzün C, Yorulmaz I, Cindaş A, et al. : Low back pain and posture. Clin Rheumatol, 1999, 18: 308–312. [DOI] [PubMed] [Google Scholar]
- 24.Kim BG, Park RJ, Lee SJ: Difference of lumbar lordosis in patients with low back pain and controls. J Kor Soc Phys Ther, 2000, 12: 185–190. [Google Scholar]
- 25.Edmondston SJ, Singer KP: Thoracic spine: anatomical and biomechanical considerations for manual therapy. Man Ther, 1997, 2: 132–143. [DOI] [PubMed] [Google Scholar]
- 26.Fon GT, Pitt MJ, Thies AC, Jr: Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol, 1980, 134: 979–983. [DOI] [PubMed] [Google Scholar]
- 27.Giglio CA, Volpon JB: Development and evaluation of thoracic kyphosis and lumbar lordosis during growth. J Child Orthop, 2007, 1: 187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suk SL, Lee CS, Lo M, et al. : Normal segmental sagittal angle of the lower dorsal and lumbosacral spine in Korean adult. J Korean Orthop Assoc, 1989, 24: 237–244. [Google Scholar]
- 29.Korovessis P, Stamatakis M, Baikousis A: Segmental roentgenographic analysis of vertebral inclination on sagittal plane in asymptomatic versus chronic low back pain patients. J Spinal Disord, 1999, 12: 131–137. [PubMed] [Google Scholar]
- 30.Hicks GE, Fritz JM, Delitto A, et al. : Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil, 2005, 86: 1753–1762. [DOI] [PubMed] [Google Scholar]
- 31.Ferreira PH, Ferreira ML, Maher CG, et al. : Changes in recruitment of transversus abdominis correlate with disability in people with chronic low back pain. Br J Sports Med, 2010, 44: 1166–1172. [DOI] [PubMed] [Google Scholar]