Abstract
Convergent evidence implicates regional neural responses to reward anticipation in the pathogenesis of several psychiatric disorders, such as schizophrenia, where blunted ventral striatal responses to positive reward are observed in patients and at-risk populations. In vivo oxygen amperometry measurements in the ventral striatum in awake, behaving rats reveal reward-related tissue oxygen changes that closely parallel blood oxygen level dependent (BOLD) signal changes observed in human functional magnetic resonance imaging (fMRI), suggesting that a cross-species approach targeting this mechanism might be feasible in psychopharmacology. The present study explored modulatory effects of acute, subanaesthetic doses of ketamine—a pharmacological model widely used in psychopharmacological research, both preclinically and clinically—on ventral striatum activity during performance of a reward anticipation task in both species, using fMRI in humans and in vivo oxygen amperometry in rats. In a region-of-interest analysis conducted following a cross-over placebo and ketamine study in human subjects, an attenuated ventral striatal response during reward anticipation was observed following ketamine relative to placebo during performance of a monetary incentive delay task. In rats, a comparable attenuation of ventral striatal signal was found after ketamine challenge, relative to vehicle, in response to a conditioned stimulus that predicted delivery of reward. This study provides the first data in both species demonstrating an attenuating effect of acute ketamine on reward-related ventral striatal (O2) and fMRI signals. These findings may help elucidate a deeper mechanistic understanding of the potential role of ketamine as a model for psychosis, show that cross-species pharmacological experiments targeting reward signaling are feasible, and suggest this phenotype as a promising translational biomarker for the development of novel compounds, assessment of disease status, and treatment efficacy.
Introduction
Anticipation of reward is known to have a critical role in cognition, and disruption of this mechanism may contribute to many neuropsychiatric disorders. The salience of cues that predict reward can be evaluated using a number of different neuroimaging tasks, of which the monetary incentive delay (MID) task has proven especially fruitful. Blood oxygen level dependent (BOLD) signal increases have been consistently observed in the ventral striatum (VS) during the anticipation phase of the MID task in healthy subjects (Ernst et al, 2004; Kirsch et al, 2003; Knutson et al, 2001a). In schizophrenia, attenuated VS activation during reward anticipation is observed (Esslinger et al, 2012; Grimm et al, 2012; Juckel et al, 2006; Nielsen et al, 2012), where the degree of attenuation correlates with symptom severity (Juckel et al, 2006; Nielsen et al, 2012). Besides being measurable in chronic schizophrenic patients (Grimm et al, 2012), reduced VS activation is seen in unmedicated patients (Esslinger et al, 2012; Juckel et al, 2006; Nielsen et al, 2012) and also prodromally in defined ultra-high risk populations (Juckel et al, 2012). The attenuated VS signal is sensitive to pharmacological treatment, as atypical antipsychotics have been shown to partially normalise VS dysfunction in schizophrenia (Juckel et al, 2006; Nielsen et al, 2012).
Reward pathways are highly conserved across species (Juckel et al, 2006; Nielsen et al, 2012; Ongur and Price, 2000), and many aspects of their function and activity generalize between humans and rodents (Knutson and Cooper, 2005) suggesting the possibility to compare, align, and translate results and paradigms from one species to the other. However, back translation of task-based functional magnetic resonance imaging (fMRI) per se to rodents, beyond simple somatosensory stimuli, is extremely difficult owing to the requirements of immobilization and, often, anesthesia. Constant potential amperometry (CPA) is an alternative approach that allows real-time monitoring of regional brain tissue O2 levels in freely moving rats (Knutson and Cooper, 2005; Lowry et al, 2010), opening the way to studying changes in brain activity while the rodents perform behavioral tasks. This technique has recently been coupled with a rodent-reward task, revealing VS activation specifically following rewarded cue onset before reward delivery and also during the first day of extinction. VS activation was modulated by both reward magnitude and the motivational state of the rodent suggesting a response more specific to reward anticipation, thereby bearing striking similarity with human BOLD signal changes (Francois et al, 2012, 2014).
In the present paper, ventral striatal activity was studied in the context of acute ketamine administration, a translational ‘disruption model' of schizophrenia. Subanaesthetic doses of ketamine have been used acutely to induce neurophysiological and behavioral alterations bearing significant resemblance to an acute schizophrenic episode (De Simoni et al, 2013; Duncan et al, 1999; Krystal et al, 1994; Langsjo et al, 2003; Littlewood et al, 2006; Moghaddam et al, 1997) in both rodents and humans and are widely used in both experimental medicine and preclinical investigations. The aim of the present study was to use O2 amperometry and fMRI to assess the effect of acute ketamine administration on VS activation during a reward task in rodents and healthy human subjects, respectively, and hence to ascertain the generalizability of the blunted VS activation phenotype and the degree to which it is translatable across species.
Subjects and methods
Subjects: Humans
The study was designed as single-centre, subject- and observer-blind, placebo-controlled, randomized, three-period cross-over study in healthy subjects with fully counterbalanced, single-dose administrations of either saline (placebo condition), ketamine (0.5 mg/kg body weight), or scopolamine (4 μg/kg body weight) administered as a constant intravenous infusion over 40 min. In this paper we focus only on the comparison of intravenous placebo vs ketamine conditions. The study was approved by the local ethics committee (medical faculty Mannheim, University of Heidelberg, Germany). Subjects underwent three consecutive fMRI sessions over the course of 3 weeks. Twenty-four participants completed the study (12 female, mean age 25 years, mean body weight 70 kg). One female participant was later excluded from the data analysis due to side effects under ketamine (fainting, orthostatic dysregulation) and the subsequent inability to perform the fMRI task. Additional information on eligibility and behavioral assessment details can be found in the Supplementary Materials and Methods.
Subjects: Rats
The experiment was conducted in accordance with the regulations laid down in the United Kingdom Animals (Scientific Procedures) Act, 1986, with the approval of the Lilly Research Laboratories Institutional Animal Care and Use Committee. Twenty-eight adult male Sprague–Dawley rats (200–250 g; Charles River, Margate, UK) were housed in standard housing conditions (4 per cage, 07:00 h to 19:00 h light phase, controlled temperature and humidity, ad libitum water) for a period of 7 days before behavioral training started. During this time, they were acclimated to the food-restriction regime (85% of their free-feeding weight) and handled regularly.
Drug Administration: Humans
On each day of the experiment, and ~60 min prior to the start of the MRI scan, subjects received intravenous cannulation followed by an infusion scan via a certified IV pump (Braun Medical, Melsungen, Germany). The order of substance application was randomly permutated across all 24 participants and yielded six balanced sequences of substance ordering. All study participants and personnel involved in the experiments were blind to the respective substance given. Individual doses of ketamine hydrochloride were adjusted to body weight (0.5 mg/kg) following previously published protocols (Diazgranados et al, 2010), diluted in saline, and applied over 40 min. The placebo condition consisted of a 40-min saline infusion. MRI scanning took place after drug administration, with the reward task starting ~40 min following cessation of the intravenous infusion. On each day of the experiment and before discharge, a medical examination was carried out by a physician. Behavioral assessment of the effects of ketamine on mood were carried out with the MDBF self-rating scale (Hinz et al, 2012; Steyer et al, 1997). The MDBF consists of 30 items rated from one to five, which are combined to provide three bipolar measures and thereby sum scores for ‘Good Mood vs Bad Mood', ‘Calmness vs restlessness', and ‘Alertness vs Tiredness'. Participants were rated before and after drug application.
Drug Administration: Rats
The NMDA receptor antagonist S-(+)-ketamine hydrochloride was administered after rodents reached stable performance on the Pavlovian conditioning paradigm. Ketamine (10 mg/kg; dissolved in 5% (w/v) glucose, Sigma-Aldrich, UK) was injected subcutaneously 30 min before the test session started. Dose and route of administration were chosen on the basis of previous studies (Gastambide et al, 2013; Gilmour et al, 2009). A between-subject design was used in this experiment with 14 rodents receiving either vehicle or ketamine. A between-subjects design was chosen here as effect sizes were anticipated to be large based on previous work in our laboratory, thereby expediting study completion to maximize the experimental lifespan of subjects.
Data Acquisition: Human fMRI
Data measurement took place using a 3 Tesla MRI system (Siemens Trio, Erlangen, Germany), using an ~9 min echo-planar imaging time series with whole-brain coverage, 3 × 3 × 3 mm3 voxels and repetition time 1.79 s. Details of the reward paradigm are provided below, and additional acquisition details are given in the Supplementary Materials and Methods.
Data Acquisition: Rat In vivo Amperometry
Additional details of in vivo amperometric methodology have been included in Supplementary Materials and Methods. Carbon paste (CPE), reference and auxiliary electrodes were constructed and calibrated in vitro as previously described (Francois et al, 2012). Surgeries were performed at Charles River. CPE electrodes were implanted in the nucleus accumbens (from bregma: AP+2.0 mm, ML±0.5 mm, DV: −2.0 mm). Reference and auxiliary electrodes were positioned over the posterior cortex. Changes in extracellular tissue oxygen concentration (O2) were measured using CPA at CPEs as described previously (Francois et al, 2012, 2014; Lowry et al, 1997) at a sample rate of 200 Hz. Histological verification of placements was performed after behavioral testing (Neuroscience Associates, Knoxville, TN, USA).
Reward Anticipation Paradigm: Humans
Brain function during reward anticipation was studied with fMRI and a well-established and reliable monetary incentive delay paradigm (Grimm et al, 2014; Kirsch et al, 2003; Plichta et al, 2012). Briefly, subjects were instructed to respond as fast as possible with a button press to a brief flashing of the screen. Four experimental conditions were indicated by different arrows preceding the flash: (i) a win (or CS+) condition (vertical arrow pointing up) indicating that subjects will earn 2€ if they respond fast enough, (ii) a loss avoidance (or CS−) condition (vertical arrow pointing down) indicating that subjects will lose 2€ if they respond too slow, (iii) a verbal feedback condition (double-headed vertical arrow) indicating that subjects will receive a positive or negative visual feedback to their response without monetary consequences (‘you reacted fast!' or ‘you reacted slow!'), and (iv) a neutral condition (double-headed horizontal arrow) without subsequent flashing of the screen. A balance sheet of the money won so far was presented at the end of each trial. The experiment contained 10 trials per condition in a pseudo-randomized order. Reaction time thresholds were adaptively adjusted to individual response times (ie, a 5% increase after slow responses and a 5% decrease after fast responses.
Reward Anticipation Paradigm: Rats
Rodents were tested in standard operant chambers housed in sound and light attenuation chambers (Med Associates, USA). Rats were then trained to discriminate between two auditory cues to receive food reward (Pellets (Noyes, 45 mg, Formula P): a discriminative stimulus (CS+) which predicted the delivery of reward after cue offset with 100% probability, and a non-rewarded stimulus (CS−) that had no consequence. Auditory cues (tone or clicker) were counterbalanced across the squad of rodents. CS+ and CS− cues (10-s duration) were presented pseudo-randomly according to 3 pre-defined lists of cue presentation (CS), where each list was not used for more than 3 consecutive days (30-min session with a VI 60 s inter-trial interval (ITI)). For each session, behavioral performance was assessed by measuring the number of head entries made during CS, normalized to the equivalent period of time immediately before CS (PreCS). The number of head entries made within a similar period during the ITI was also measured as an index of non-specific drug effects. The number of head entries was analyzed by factorial ANOVA with treatment and cue as factors, followed as appropriate by multiple comparisons tests.
Data Processing and Analysis: Human fMRI
Data were processed using statistical parametric mapping following previously published procedures (Grimm et al, 2014; Kirsch et al, 2003; Plichta et al, 2012; http://www.fil.ion.ucl.ac.uk/spm/). Images were realigned to the first image of the scan, slice-time corrected, spatially normalized to standard stereotactic space (Montreal Neurological Institute (MNI) template), resampled to 3-mm isotropic voxels, and smoothed with an 8-mm full-width at half maximum Gaussian kernel. Statistical analysis consisted of a two-level procedure. At the first level, individual general linear models were specified by modeling a set of delta functions corresponding to task events and were convolved with a canonical hemodynamic response function (HRF). Regressors of interest were the onsets of the different anticipatory events, a regressor indicating onsets of all targets, one no-target regressor for the neutral condition and the six movement parameters were used as regressors of no interest. At the model-estimation stage, the data were high-pass filtered with a cutoff of 128 s, and an autoregressive model of the first order was applied. Contrast images were calculated on the basis of our a priori hypothesis to identify brain regions with greater activation during the anticipation of monetary reward vs no conditioned stimulus (contrast: (WIN (CS+))>(NEUTRAL (CS−))).The contrast estimates were used in a second-level model to calculate the ketamine vs placebo difference in a paired t-test. For small volume correction, a region-of-interest mask of the nucleus accumbens based on the Harvard–Oxford atlas (http://www.cma.mgh.harvard.edu/) with a probability threshold of 50% was used.
Histology: Rat In vivo Amperometry
Rodents were deeply anaesthetized with pentobarbital and perfused transcardially with 0.9% (w/v) saline followed by 10% (w/v) buffered paraformaldehyde solution. Brains were removed and placed in 10% (w/v) buffered paraformaldehyde and shipped for histological processing (Neuroscience Associates, Knoxville, TN), which involved 40 mm coronal sectioning of implanted regions and staining with thionin for Nissl bodies. Upon return, microscopic assessment confirmed CPE placement with reference to a standard rat brain atlas (Paxinos and Watson, 2009). All inaccurate placements were excluded from subsequent analyses.
Data Processing And Analysis: Rat In Vivo Amperometry
Following exclusion (misplaced electrodes n=4, unstable or noisy O2 signals n=3), 10 (ketamine group; KET) and 11 (vehicle group; VEH) rodents passed quality criteria for inclusion in subsequent analyses. In both the KET and VEH groups, three rodents only had one electrode that passed quality criteria. As a preliminary statistical analysis revealed no main effect of hemisphere (F(1,64)=0.55, P=0.45) and no hemisphere × group interaction (F(1,64)=1.22, P=0.27), only one electrode was randomly chosen per rodent in those that had bilateral placements for all subsequent analyses. Each trial type (CS+ or CS−) was analyzed separately and time zero was taken as the time of cue onset with a 1 s preceding period used as a baseline. Data were analyzed for 30 s following cue onset. Area under the curve (AUC) and maximum amplitude (Ypeak) were calculated. A 2-D boxplot statistical analysis was used to identify the outliers that were removed from the final analysis. When possible, ie, when both electrodes were correctly implanted in an rodent, the effect of side (left or right) was assessed. If no statistical effect of side was obtained, only one electrode contributed to the final analysis data set per rodent, where side was randomly chosen. Statistical analysis on averaged curves and extracted measures was conducted using repeated measure two-way ANOVA with cue (CS+, CS−) and group (VEH, KET) as factors and time as the repeated measure. The extracted measures (AUC, peak) were analyzed using a two-way ANOVA with cue (CS+, CS−) and group (VEH, KET) as factors. All main analyses were followed when appropriate by a Fisher's LSD post hoc test for multiple comparisons using the Statistica 9.0 Software (Statsoft, Bedford, UK).
Pharmacokinetics: Humans
Two blood samples for pharmacokinetic analysis were drawn. The first (T1) was drawn immediately before the participant entered the scanner, about 10 min after the end of the infusion. The second (T2) was 80 min after the end of the infusion. The samples were centrifuged (1100 r.p.m., 4° C) and frozen at −80° C. The consecutive chromatographic analysis was done in a commercial certified medical laboratory (Labor Limbach, Heidelberg, Germany) using liquid chromatography–mass spectrometry. One subject's blood sample was missing for the first sample (T1, n=22). Exact numbers are given in Table 1.
Table 1. Ketamine Plasma Levels in Human Volunteers.
| Sample size | Mean (ng/ml) | Standard deviation (ng/ml) | |
|---|---|---|---|
| T1 ketamine | 22 | 561.55 | 397.22 |
| T2 ketamine | 23 | 162.94 | 109.52 |
| T1 norketamine | 22 | 45.70 | 20.19 |
| T2 norketamine | 23 | 41.41 | 14.55 |
Results
Human Pharmacokinetics And Behavioral Data
Each participant reached sufficient and measurable ketamine and norketamine levels as assessed by the two blood samples (T1 and T2, prior to and following the scanning session, respectively). In one subject blood sampling was not possible (therefore n=23). Side effects over the whole experiment were significantly more common during the ketamine condition (nausea ketamine 10 vs placebo 0, P=0.002; visual disturbances/dissociation ketamine 13 vs placebo 0 P<0.001; ‘feeling drunk' ketamine 3 vs placebo 1, P=0.62; dizziness ketamine 19 vs placebo 1, P<0.001, statistics given via binomial distributed McNemar test). No participant experienced psychotic symptoms.
With regard to the three factors of the MDBF scale (valence, alertness, and calmness), no significant effect of pre- and post-ketamine infusion was seen (P>0.08). Further, task-specific reaction time was not influenced by ketamine compared with placebo during the CS+ (mean reaction time placebo 249.28 msec SD vs mean reaction time ketamine 254.28 msec SD 5.26; P=0.53).
Plasma ketamine levels were (mean±SD) 561±397 ng/ml at sampling time T1 (~10 min after infusion cessation), and this had decreased to 163±110 ng/ml at sampling time T2 (~80 min after infusion cessation; Table 1). Norketamine plasma levels were more stable, measured at 46±20 ng/ml at T1 and 41±15 ng/ml at T2.
Human Pharmacological fMRI
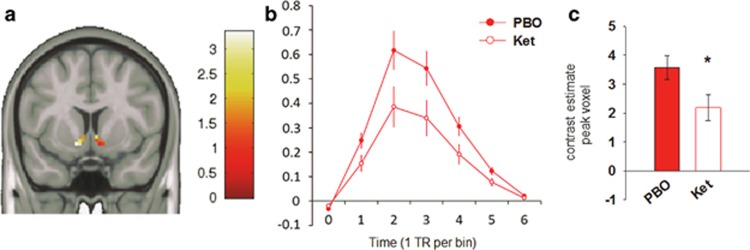
Analysis of the task performance data did not show any significant differences between the ketamine and the placebo condition. Specifically, there was neither a significant difference between the amount of money won (reward balance t(22)=0.70, P=0.49) nor a difference in the reaction time to the CS+ (t(22)=0.05, P=0.96). The analysis of fMRI data in humans confirmed a strong significant main effect of the reward condition in the placebo condition on nucleus accumbens activation (CS+ vs CS−: Z=6.01, Pmax<0.001, family-wise error corrected for NAcc ROI, whole-brain effect see Figure 1a). The comparison of this functional contrast between the ketamine and placebo drug conditions yielded a significantly lower activation within our region-of-interest mask in the nucleus accumbens under ketamine (Z=2.98, PFWE=0.036, corrected for NAcc ROI, local maximum: x=−12, y=8, z=−10; Figure 2). An exploratory whole-brain analysis did not show family-wise error corrected effects for both contrast directions. A summary of non-corrected brain effects is presented in Supplementary S4 and Supplementary Figure S2.
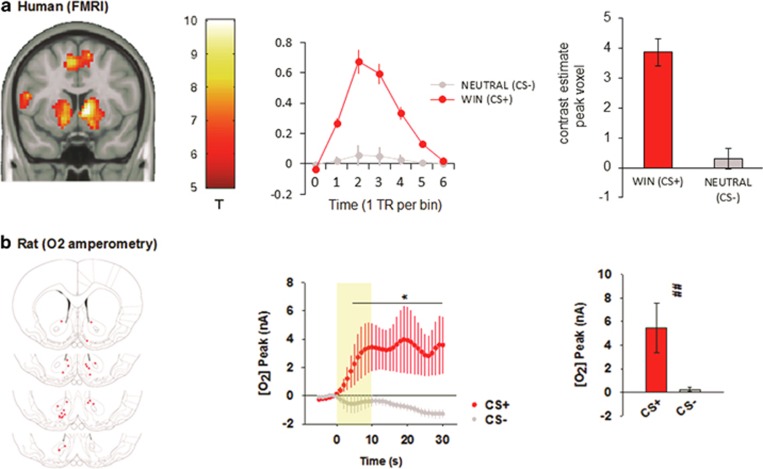
Figure 1.
Ventral striatal responses to reward stimuli in humans and rats. (a) Ventral striatal response to the contrast win (CS+)>neutral (CS−) in the placebo condition in humans. Left: T-map showing strong reward response (thresholded with PFWE<0.05, k=30, one sample t-test of the placebo condition). Middle: observed peri-stimulus time courses were obtained as first eigenvariate after fitting single-subject finite impulse-response models for each individual (adjusted for constant, movement, residuals, and experimental conditions of no interest) and subsequent averaging of estimates for each time point. Peri-stimulus plot are shown for the WIN (or ‘CS+' red) and the NEUTRAL condition (or ‘CS−' gray). x-axis gives units in TR (1.79 s per bin), y-axis is in arbitrary units. Error bars represent standard errors. Right: contrast bar plot from the maximum peak voxel. Data are shown as mean±SEM. (b) Ventral striatal response to CS+> CS− conditions in rats. Left: histological validation of probe placement in the nucleus accumbens. Middle: group-mean time course of O2 responses to CS+ and CS− conditions. Right: bar plot of peak O2 response to CS+ and CS− conditions. (AUC responses are very similar and shown in the Supplementary Materials and Methods.)
Figure 2.
Attenuation of the ventral striatum BOLD response to anticipatory reward following systemic ketamine administration in humans. (a) Axial slice of a paired t-test of the region-of-interest mask within the nucleus accumbens for the contrast win (CS+)>neutral (CS−). The color bar indicates the range of t-values. (b) Observed peri-stimulus time courses were obtained as first eigenvariate after fitting single-subject finite impulse-response models for each individual (adjusted for constant, movement, residuals, and experimental conditions of no interest) and subsequent averaging of estimates for each time point within drug condition. Error bars represent SEM. x-axis gives units in TR (1.79 s per bin), y-axis is in arbitrary units. (c) Bar plot showing the difference between peak voxel contrast estimates between placebo and ketamine condition (*PFWE<0.05). Data are shown as mean±SEM.
Rat Pharmacokinetics
Plasma and brain exposures achieved following the dose of ketamine and route of administration used in this study have been previously measured (Gastambide et al, 2013) and were not collected in this experiment. On the basis of these previous data, we expected ketamine plasma concentrations to be declining from 150 ng/ml to around 50 ng/ml, and brain concentrations to be declining from 1000 ng/g to 500 ng/g, during the time of task execution.
Rat In vivo O2 Amperometry
Full details of statistical analyses calculated for both behavioral and amperometry data can be found in Supplementary Materials and Methods. Vehicle-treated rodents made a significantly greater number of head entries during CS+ presentation compared with CS− presentation (CS+ VEH vs CS− VEH, P<0.01), indicating that conditioning was achieved to the reward-associated cue. With regard to averaged (O2) amperometry signals, this cue-dependent behavioral dissociation was reflected in a significantly increased NAc (O2) signal during CS+ CS relative to CS− CS (CS+ VEH vs CS− VEH, P<0.01; Figure 1b). Both AUC and peak measures reflected these results, with both significantly greater following CS+ presentation (CS+ VEH vs CS− VEH, both P<0.01, see Supplementary Materials and Methods).
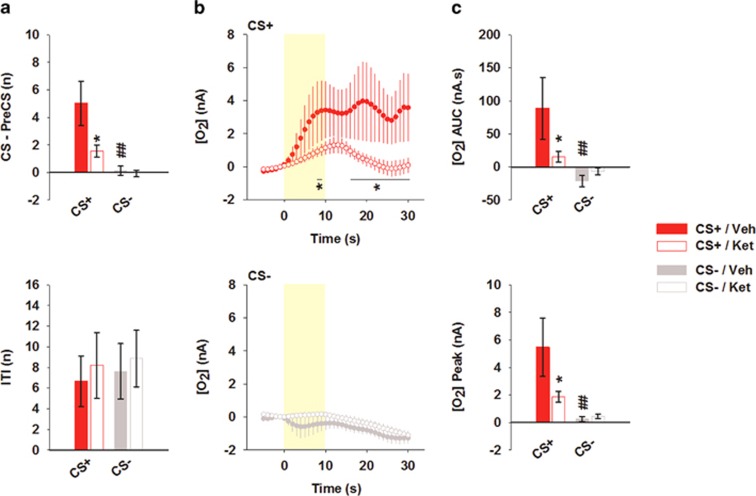
Systemic injection of ketamine induced a significant decrease in the number of head entries performed during CS+ CSs (CS+ VEH vs CS+ KET, P<0.01), whereas those associated with the CS− cue remained unchanged (CS− VEH vs CS− KET, P=0.86, Figure 3a). The number of head entries performed during the ITI was unchanged after ketamine, confirming the behavioral specificity of the ketamine effect. Also, following ketamine treatment the significant dissociation between CS+ and CS− was lost both with regard to the behavioral measure (CS+ KET vs CS− KET, P=0.18, Figure 3a) and also the NAc (O2) signal (CS+ KET vs CS− KET, P=0.46, Figure 3b). A statistical analysis conducted only on the 10 s period of CS substantiated this effect of ketamine on the cue-related (O2) signals (time × cue × drugF19,342=2.12, P<0.01; CS+ VEH vs CS− VEH, P=0.04; CS+ KET vs CS− KET, P=0.66). AUC and peak measures were consistent, showing that ketamine significantly attenuated NAc activation during CS+ CS, whereas activation during CS− CS remained unchanged (AUC: CS+ VEH vs CS+ KET, P<0.05; CS− VEH vs CS− KET, P=0.62; YPeak: CS+ VEH vs CS− VEH, P<0.05; CS− VEH vs CS− KET, P=0.88, Figure 3b and c.
Figure 3.
Effect of a systemic injection of ketamine on behavioral performance and ventral striatum O2 responses during a Pavlovian cue discrimination task in the rat. (a) Behavioral performance was assessed by measuring the number of head entries made during CSs normalized to the number of head entries made during the equivalent period of time immediately before CS (CS–PreCS), and by the number of head entries made during the inter-trial interval period (ITI) in vehicle (VEH, solid red, solid gray) and ketamine treated rodents (KET, open red, open gray). Data are shown as mean±SEM; *P<0.05 compared with the vehicle group; ##P<0.01 compared with the CS+ cue. (b) Averaged (O2) amperometric signals recorded in Nac, associated with the rewarded cue (CS+, red circles) and the non-rewarded cue (CS−, gray circles). Cue onset and offset are represented by at the shaded area between 0 and 10 s, respectively. Data are shown as mean±SEM; *P<0.05 compared with the CS+ cue. (c) Area under the curve (AUC) and maximum amplitude (Ypeak) extracted from the averaged curve presented in b for vehicle- (VEH, solid red, solid gray) and ketamine- (KET, open red, open gray) treated animals. Data are shown as mean±SEM; *P<0.05 compared with the vehicle group; ##P<0.01 compared with the CS+ cue.
Discussion
The present study provides evidence that the blunted ventral striatal reward anticipation response, previously observed in schizophrenic patients and subjects at genetic risk for the disorder (Grimm et al, 2014), extends to a relevant pharmacological model and that this phenotype may be conserved in the awake rodent. In both humans and rats, an acute dose of ketamine was found to markedly attenuate activation of the ventral striatum in response to a conditioned cue that predicts reward, indicating an effect of ketamine on basic reward-processing mechanisms. Both the baseline measurement of ventral striatal activation during reward-related processing and its attenuation by ketamine were robustly preserved across species. Thus, by using a clinically relevant pharmacological perturbation and in vivo O2 amperometry in rats as a surrogate of the human BOLD response, a compelling preclinical analogue of the human pharmacological fMRI paradigm has been demonstrated.
Both human and rat data demonstrated a robust activation of the ventral striatum upon presentation of a cue that predicted reward. These baseline effects were in accordance with previous reports from human imaging (Knutson et al, 2001a), rat amperometry (Francois et al, 2012, 2014) and rat electrophysiology studies (Bissonette et al, 2013; Martin and Ono, 2000; Schultz et al, 1997) utilizing a number of different reward anticipation paradigms. However, there are procedural differences between species and other study limitations that should be considered during interpretation of the findings.
First, differences in the brain activation measure used in both species have to be considered. Indeed, the electrochemical signal measured by the CPE electrodes in the rat reflects extracellular concentrations of tissue oxygen, in contrast to the BOLD signal in human fMRI which is largely weighted by microvasculature contributions, although both likely reflect the dynamic balance between oxygen consumption and supply with similar second-level temporal resolution. Moreover, similar responses have been obtained following oxygen inhalation during simultaneous O2 amperometry and BOLD recordings suggesting a close relationship between the two measures (Lowry et al, 2010). Also, event-averaged O2 AUC signals as measured in the rodent study could differ physiologically from the event-related fMRI measure used in humans. In this regard, the validity of this comparison has previously been described, as shown in terms of the translatability of task-dependent signals in rats to human findings (Francois et al, 2012).
Secondly, the present study was based on standard reward anticipation paradigms in humans and rats that were known to evoke a ventral striatum response. However, this did mean that there were some differences in the variety of cues being presented, the response outcomes required and potentially the psychological processes under examination. The rat task utilized a between-subjects Pavlovian conditioning schedule with certain CS+ and CS− cues, and two clear outcomes (food or nothing). In contrast, the human task used a within subjects operant discrete trial procedure with four stimuli conditions and six response outcomes. As the CS− condition was not associated with reward delivery in both species, it was considered appropriate for this to be the main comparator condition in each study. Also, there was a clear difference in the level of training required for subjects to perform the task. Humans can perform a reward anticipation task immediately with minimal verbal instruction, whereas it takes rats several days to reach a level of performance that is believed to reflect a reliable level of behavioral control and hence task ‘awareness'. This may be important when trying to consider the relative magnitude of response in the ventral striatum elicited during reward anticipation, as anticipation responses and prediction error signals can diminish with increasing predictability and/or familiarity of the cues (Berns et al, 2001; Francois et al, 2014). It may be the case therefore, that humans and rats were essentially being studied during test contexts when accumbens engagement in the task might be fundamentally different. This may be especially important in the consideration of pharmacological study designs, particularly if they were to involve subchronic or chronic drug treatment. A third obvious difference between the studies lies in the nature of reward used, which was monetary for humans but food reward for rats. Although there are clearly different psychological and physiological drives associated with the desire to obtain different reward types across species, there is much evidence to suggest the nature of the reward itself is not likely to evoke substantially different anticipation-activation patterns in the accumbens (Carelli, 2002). For instance, human imaging studies have shown a consistent activation of the NAc to the presence of many different types of reward such as monetary gain (Knutson et al, 2001b), pleasant taste (O'Doherty, 2004) and smilling faces (Spreckelmeyer et al, 2009). However, for interaction studies using pharmacology that may directly impact appetitive motivation, different reward types may be required in the rat. Alternatively, food reward could be used in humans to increase translational validity. Finally, another important aspect of translational validity here is gaining confidence that, to the best extent possible, pharmacologically equivalent doses of ketamine have been compared. Unfortunately, in the absence of a recognized marker of target engagement of the NMDA receptor by ketamine in either species, this remains preliminary. Human and rat studies effectively used widely employed, ‘standard' paradigms, but this still left potentially important differences. The human study occurred ~35 min after a 40-min infusion of racemic ketamine, whereas the rat study used a subcutaneous bolus of (s)-(+)-ketamine, the latter being 2–3 times more potent (Himmelseher and Pfenninger, 1998). As such, it was likely that rats received a higher maximal brain exposure than humans, though this would have been elevated for longer in humans. Further, the qualitative behavioral effects of ketamine were different across species. All human participants reported a change in perceptual, emotional, and cognitive quality, eg, ‘feeling drunk' and some degree of dissociative feelings. However, this vanished within 10 min after end of the infusion and was not present anymore during the reward task itself. In contrast, a behaviorally specific effect of ketamine was observed in the reward anticipation task in rats. Ketamine specifically decreased the number of head entries being made during the CS period compared with the preCS period whilst leaving ITI head entry unchanged. Despite these methodological differences and a clear need for future studies to understand the cross-species pharmacokinetic/pharmacodynamic relationships more thoroughly, the effect of ketamine on rewardevoked VS response was strikingly similar across species.
Although the present study focused on a potential substrate of the effects of ketamine in the ventral striatum and its interpretation in the context of mechanisms underlying psychosis and the risk for psychosis, there is of course a parallel literature regarding the antidepressant effects of ketamine (Iadorola et al, 2015). It is not clear at present the extent to which findings within both fields of research can be reconciled and several factors need to be carefully considered here. It is not clear at present whether both psychotomimetic and antidepressant effects of ketamine always occur as a consequence of the same treatment regimen or whether different regimens favor the expression of one effect over the other. Although not definitively established, the onset of antidepressant effects of ketamine may also be somewhat delayed relative to its psychotomimetic effects (Coyle and Laws 2015). If both effects can co-occur, it may be that there are important differences in their regional locus. For instance, recent work has implicated regions such as the hippocampus and anterior cingulate cortex (Lally et al, 2015), as well as network level modulation of default mode activity as potential substrates of antidepressant efficacy (Scheidegger et al, 2012). A more global account of the effects of ketamine will certainly require study of more than just the ventral striatum. Finally, it is always important to consider the baseline from which different ketamine effects are being measured from. ‘Psychosis' studies are typically conducted in healthy human volunteers, whereas antidepressant studies are typically conducted in clinically diagnosed—usually treatment refractory—depressed patients. There should be no a priori assumption that ketamine will behave equally in each study population. In fact, blunted reward anticipation has been described previously in medication-free depressed patients (Ubl et al, 2015), indicating that each study population may have different baseline characteristics of ventral striatal function to begin with. Interestingly, a recent PET imaging study has suggested that anti-hedonic effects of ketamine in bipolar depression patients is not specifically associated with changes in glucose metabolism in the ventral striatum (Lally et al, 2015).
In conclusion, the present study demonstrated equivalent effects of an acute dose of ketamine on ventral striatal activation during a reward anticipation task in humans and rodents. This approach may help to provide construct validity to this model via results that can now be extrapolated between species. Homologous regional effects in pharmacological fMRI and in vivo amperometry may provide insight into the validity of specific rodent models such as blunted striatal activation and therefore help psychiatric preclinical translation, with the added potential to provide more valuable and accurate tools for the discovery and development of psychiatric therapies.
Funding and disclosure
NEWMEDS—the research leading to these results, has received support from the Innovative Medicine Initiative Joint Undertaking under Grant Agreement No. 115008 of which resources are composed of European Federation of Pharmaceutical Industries and Associations (EFPIA) in-kind contribution and financial contribution from the European Union's Seventh Framework Programme (FP7/2007–2013). We have received the following Grants: ECNP Neuropsychopharmacology Award, Prix ROGER DE SPOELBERCH. JF is an employee of Vertex Pharmaceuticals (Europe). GG is an employee and shareholder of Eli Lilly. CR is an employee of F Hoffmann-La Roche. AJS is an employee and shareholder of Eli Lilly. AM-L received consultant fees and travel expenses from Alexza Pharmaceuticals, Astra Zeneca, Bristol-Myers Squibb, Defined Health, Decision Resources, Desitin Arzneimittel, Elsevier, F Hoffmann-La Roche, Gerson Lehrmann Group, Groupo Ferrer, Les Laboratoires Servier, Lilly Deutschland, Lundbeck Foundation, Outcome Sciences, Outcome Europe, Pricespective, and Roche Pharma, speaker's fees from Abbott, Astra Zeneca, BASF, Bristol-Myers Squibb, Glaxo SmithKline, Janssen-Cilag, Lundbeck Foundation, Pfizer Pharma, and Servier Deutschland. AM-L received the consultancy fees from: Astra Zeneca, Elsevier, F. Hoffmann-La Roche, Gerson Lehrman Group, Lundbeck Foundation, Outcome Europe Sárl, Outcome Sciences, Roche Pharma, Servier International, and Thieme Verlag, and lecture fees—including the travel fees—from: Abbott, Astra Zeneca, Aula Médica Congresos, BASF, Groupo Ferrer International, Janssen-Cilag, Lilly Deutschland, LVR Klinikum Düsseldorf, Servier Deutschland, Otsuka Pharmaceuticals.
Footnotes
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Supplementary Material
References
- Berns GS, McClure SM, Pagnoni G, Montague PR (2001). Predictability modulates human brain response to reward. J Neurosci 21: 2793–2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bissonette GB, Burton AC, Gentry RN, Goldstein BL, Hearn TN, Barnett BR et al (2013). Separate populations of neurons in ventral striatum encode value and motivation. PloS One 8: e64673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carelli RM (2002). The nucleus accumbens and reward: neurophysiological investigations in behaving animals. Behav Cogn Neurosci Rev 1: 281–296. [DOI] [PubMed] [Google Scholar]
- Coyle CM, Laws KR (2015). The use of ketamine as an antidepressant: a systematic review and meta-analysis. Hum Psychopharmacol 30: 152–163. [DOI] [PubMed] [Google Scholar]
- Diazgranados N, Ibrahim L, Brutsche NE, Newberg A, Kronstein P, Khalife S et al (2010). A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression. Arch Gen Psychiatry 67: 793–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Simoni S, Schwarz AJ, O'Daly OG, Marquand AF, Brittain C, Gonzales C et al (2013). Test-retest reliability of the BOLD pharmacological MRI response to ketamine in healthy volunteers. Neuroimage 64: 75–90. [DOI] [PubMed] [Google Scholar]
- Duncan GE, Miyamoto S, Leipzig JN, Lieberman JA (1999). Comparison of brain metabolic activity patterns induced by ketamine, MK-801 and amphetamine in rats: support for NMDA receptor involvement in responses to subanesthetic dose of ketamine. Brain Res 843: 171–183. [DOI] [PubMed] [Google Scholar]
- Ernst M, Nelson EE, McClure EB, Monk CS, Munson S, Eshel N et al (2004). Choice selection and reward anticipation: an fMRI study. Neuropsychologia 42: 1585–1597. [DOI] [PubMed] [Google Scholar]
- Esslinger C, Englisch S, Inta D, Rausch F, Schirmbeck F, Mier D et al (2012). Ventral striatal activation during attribution of stimulus saliency and reward anticipation is correlated in unmedicated first episode schizophrenia patients. Schizophr Res 140: 114–121. [DOI] [PubMed] [Google Scholar]
- Francois J, Conway MW, Lowry JP, Tricklebank MD, Gilmour G (2012). Changes in reward-related signals in the rat nucleus accumbens measured by in vivo oxygen amperometry are consistent with fMRI BOLD responses in man. Neuroimage 60: 2169–2181. [DOI] [PubMed] [Google Scholar]
- Francois J, Huxter J, Conway MW, Lowry JP, Tricklebank MD, Gilmour G (2014). Differential contributions of infralimbic prefrontal cortex and nucleus accumbens during reward-based learning and extinction. J Neurosci 34: 596–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gastambide F, Mitchell SN, Robbins TW, Tricklebank MD, Gilmour G (2013). Temporally distinct cognitive effects following acute administration of ketamine and phencyclidine in the rat. Eur Neuropsychopharmacol 23: 1414–1422. [DOI] [PubMed] [Google Scholar]
- Gilmour G, Pioli EY, Dix SL, Smith JW, Conway MW, Jones WT et al (2009). Diverse and often opposite behavioural effects of NMDA receptor antagonists in rats: Implications for ‘NMDA antagonist modelling' of schizophrenia. Psychopharmacology 205: 203–216. [DOI] [PubMed] [Google Scholar]
- Grimm O, Heinz A, Walter H, Kirsch P, Erk S, Haddad L et al (2014). Striatal response to reward anticipation: evidence for a systems-level intermediate phenotype for schizophrenia. JAMA Psychiatry 71: 531–539. [DOI] [PubMed] [Google Scholar]
- Grimm O, Vollstadt-Klein S, Krebs L, Zink M, Smolka MN (2012). Reduced striatal activation during reward anticipation due to appetite-provoking cues in chronic schizophrenia: a fMRI study. Schizophr Res 134: 151–157. [DOI] [PubMed] [Google Scholar]
- Himmelseher S, Pfenninger E (1998). The clinical use of S-(+)-ketamine—a determination of its place. Anasthesiol Intensivmed Notfallmed Schmerzther 33: 764–770. [DOI] [PubMed] [Google Scholar]
- Hinz A, Daig I, Petrowski K, Brähler E (2012). Mood in the German population: norms of the Multidimensional Mood Questionnaire MDBF. Psychother Psychosom Med Psychol 62: 52–57. [DOI] [PubMed] [Google Scholar]
- Iadarola ND, NIciu MJ, Richards EM, Vande Voort JL, Ballard ED, Lundin NB et al (2015). Ketamine and other N-methyl-D-aspartate receptor antagonists in the treatment of depression: a perspective review. Ther Adv Chronic Dis 6: 97–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juckel G, Friedel E, Koslowski M, Witthaus H, Ozgurdal S, Gudlowski Y et al (2012). Ventral striatal activation during reward processing in subjects with ultra-high risk for schizophrenia. Neuropsychobiology 66: 50–56. [DOI] [PubMed] [Google Scholar]
- Juckel G, Schlagenhauf F, Koslowski M, Wustenberg T, Villringer A, Knutson B et al (2006). Dysfunction of ventral striatal reward prediction in schizophrenia. Neuroimage 29: 409–416. [DOI] [PubMed] [Google Scholar]
- Kirsch P, Schienle A, Stark R, Sammer G, Blecker C, Walter B et al (2003). Anticipation of reward in a nonaversive differential conditioning paradigm and the brain reward system: an event-related fMRI study. Neuroimage 20: 1086–1095. [DOI] [PubMed] [Google Scholar]
- Knutson B, Adams CM, Fong GW, Hommer D (2001. a). Anticipation of increasing monetary reward selectively recruits nucleus accumbens. J Neurosci 21: RC159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson B, Adams CM, Fong GW, Hommer D (2001. b). Anticipation of increasing monetary reward selectively recruits nucleus accumbens. J Neurosci 21: RC159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson B, Cooper JC (2005). Functional magnetic resonance imaging of reward prediction. Curr Opin Neurol 18: 411–417. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD et al (1994). Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 51: 199–214. [DOI] [PubMed] [Google Scholar]
- Lally N, Nugent AC, Luckenbaugh DA, Niciu MJ, Roiser JP, Zarate CA Jr (2015). Neural correlates of change in major depressive disorder anhedonia following open-label ketamine. J Psychopharmacol 29: 596–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langsjo JW, Kaisti KK, Aalto S, Hinkka S, Aantaa R, Oikonen V et al (2003). Effects of subanesthetic doses of ketamine on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology 99: 614–623. [DOI] [PubMed] [Google Scholar]
- Littlewood CL, Cash D, Dixon AL, Dix SL, White CT, O'Neill MJ et al (2006). Using the BOLD MR signal to differentiate the stereoisomers of ketamine in the rat. Neuroimage 32: 1733–1746. [DOI] [PubMed] [Google Scholar]
- Lowry JP, Boutelle MG, Fillenz M (1997). Measurement of brain tissue oxygen at a carbon past electrode can serve as an index of increases in regional cerebral blood flow. J Neurosci Methods 71: 177–182. [DOI] [PubMed] [Google Scholar]
- Lowry JP, Griffin K, McHugh SB, Lowe AS, Tricklebank M, Sibson NR (2010). Real-time electrochemical monitoring of brain tissue oxygen: a surrogate for functional magnetic resonance imaging in rodents. Neuroimage 52: 549–555. [DOI] [PubMed] [Google Scholar]
- Martin PD, Ono T (2000). Effects of reward anticipation, reward presentation, and spatial parameters on the firing of single neurons recorded in the subiculum and nucleus accumbens of freely moving rats. Behav Brain Res 116: 23–38. [DOI] [PubMed] [Google Scholar]
- Moghaddam B, Adams B, Verma A, Daly D (1997). Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 17: 2921–2927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen MO, Rostrup E, Wulff S, Bak N, Broberg BV, Lublin H et al (2012). Improvement of brain reward abnormalities by antipsychotic monotherapy in schizophrenia. Arch Gen Psychiatry 69: 1195–1204. [DOI] [PubMed] [Google Scholar]
- O'Doherty JP (2004). Reward representations and reward-related learning in the human brain: insights from neuroimaging. Curr Opin Neurobiol 14: 769–776. [DOI] [PubMed] [Google Scholar]
- Ongur D, Price JL (2000). The organization of networks within the orbital and medial prefrontal cortex of rats, monkeys and humans. Cereb Cortex 10: 206–219. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C (2009). The Rat Brain in Stereotaxic Coordinates. 6th edition. Elsevier Academic Press, Amsterdam.
- Plichta MM, Schwarz AJ, Grimm O, Morgen K, Mier D, Haddad L et al (2012). Test-retest reliability of evoked BOLD signals from a cognitive-emotive fMRI test battery. Neuroimage 60: 1746–1758. [DOI] [PubMed] [Google Scholar]
- Scheidegger M, Walter M, Lehmann M, Metzger C, Grimm S, Boeker H et al (2012). Ketamine decreases resting state functional network connectivity in healthy subjects: implications for antidepressant drug action. PloS One 7: e44799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz W, Dayan P, Montague PR (1997). A neural substrate of prediction and reward. Science 275: 1593–1599. [DOI] [PubMed] [Google Scholar]
- Spreckelmeyer KN, Krach S, Kohls G, Rademacher L, Irmak A, Konrad K et al (2009). Anticipation of monetary and social reward differently activates mesolimbic brain structures in men and women. Soc Cogn Affect Neurosci 4: 158–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steyer R, Schwenkmezger P, Notz P, Eid M Der Mehrdimensionale Befindlichkeitsfragebogen (MDBF). Handanweisung: Göttingen, Germany; (1997). [Google Scholar]
- Ubl B, Kuehner C, Kirsch P, Ruttorf M, Diener C, Flor H (2015). Altered neural reward and loss processing and prediction error signalling in depression. Soc Cogn Affect Neurosci 10: 1102–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.