Abstract
Production of influenza vaccines requires a minimum of six months after the circulating strain is isolated and the use of infectious viruses. The hemagglutinin (protective antigen) of circulating influenza viruses mutates rapidly requiring reformulation of the vaccines. Our goal is to eliminate the risk of working with infectious virus and reduce significantly the production time.
A cDNA fragment encoding the influenza virus A/Vietnam/1203/2004 (H5N1) HA gene was prepared using RT-PCR with viral RNA as a template. Recombinant HA (rHA) protein was produced in Escherichia coli and purified from isolated inclusion bodies by urea solubilization and Ni-ion column chromatography. Vaccine candidates were prepared by treating the rHA with formalin, adsorption onto alum or with both. Mice were injected subcutaneously with candidate vaccines 2 or 3 times 2 weeks apart. Sera were collected one week after the last injection and antibody measured by ELISA and hemagglutination inhibition (HI). The highest antibody response (449 EU) was elicited by three injections of 15 μg alum-adsorbed rHA. Dosages of 5 μg of rHA formulated with formalin and alum, and 5 μg alum adsorbed rHA elicited IgG anti-HA of 212 EU and 177 EU, respectively. HI titers, ≥ 40 were obtained in ≥ 80% of mice with three doses of all formulations.
We developed a method to produce rHA in a time-frame suitable for annual and pandemic influenza vaccination. Using this method, rHA vaccine can be produced in three to four weeks and when formulated with alum, induces HA antibody levels in young outbred mice consistent with the FDA guidelines for vaccines against epidemic and pandemic influenza.
Keywords: influenza, hemagglutinin, rapid production
INTRODUCTION
Influenza A virus causes annual epidemics of acute respiratory disease and worldwide pandemics [1, 2]. The lipid envelope surface of the virus is covered with approximately 1000 protruding protein spikes each consisting of three identical hemagglutinin (HA) molecules [3, 4]. Serum IgG against these spikes (anti-HA) neutralizes viral infectivity [5-10]. The segmented viral genome is negative, single-stranded RNA. Genetic mutations are acquired during replication by the virus encoded, error-prone RNA polymerase. Mutations beneficial to viral survival, such as eluding the host immune defenses, are conserved by the evolving virus. Genetic drift mutations in the gene encoding the HA protein necessitate frequent changes of the vaccine. Although uncommon, a major genetic shift can occur by reassortment of the segmented RNA genome leading to a change in the circulating sub-type in humans [11-13], potentially causing a pandemic. Currently, 16 sub-types of HA have been identified in avian influenza A viruses, three of which are also identified in human strains [14].
The speed of vaccine production, especially for potential pandemic viruses, is limited by current manufacturing processes. Each year, circulating virus strains are characterized by RNA sequence and immunological cross-reactivity with other strains. From these data, candidate strains are identified and released to vaccine manufacturers. The majority of influenza manufacturing relies on embryonated chicken eggs to propagate the vaccine virus. If the circulating virus strain is not lethal to eggs, it is grown in eggs, purified, inactivated chemically, tested and then distributed. Highly pathogenic strains that cannot be grown in eggs require genetic modification, which prolongs the production schedule. Typically the current vaccine production process produces only enough vaccine for one dose per person and is not available until just before the flu season begins in the fall. In perspective, the peak of the 1918 influenza pandemic lasted only four months and resulted in 50 to 100 million deaths [15, 16]. Innovative ideas for the rapid production of influenza vaccines are needed.
We devised a method which uses only viral sequence data or a small sample of viral RNA and produces recombinant HA (rHA) in E. coli. This eliminates the handling of potentially lethal virus and produces a vaccine for testing in 3 to 4 weeks. Four unique features were incorporated into the rHA immunogen: 1) removal of the signal or leader sequence, which is not a part of the mature HA0 protein. 2) truncation of the C-terminal domain which transverses virus capsid region and terminates within the virus particle. This truncated region is not important immunologically and it interferes with purification of the HA. 3) replacement of the truncated region with a His-tag to facilitate rapid purification. 4) inclusion of the polybasic amino acid region located at the HA1/HA2 host proteinase cleavage site. This site is an important characteristic of highly pathogenic avian influenza H5N1 viruses; it is essential for virus activation and entry into the host cell. By necessity, highly pathogenic virus strains supplied to vaccine developers and manufacturers have the polybasic amino acid site removed to provide a margin of safety during manufacturing processes. Our method produces rHA immunogen with the polybasic amino acid site intact rapidly and safely. This is an advantage over methods that produce antigens that do not represent fully this essential viral activation site.
Antibodies that bind to the fusion peptide sequence immediately following the polybasic amino acid protease cleavage site can protect against lethal H5N1 viral infection [17]. It has also been shown that antibodies that bind to a highly conserved epitope within a pocket in the HA stem region can neutralize virus infectivity. This pocket is comprised of the conserved fusion peptide as well as the polybasic protease cleavage site [18]. Structural hindrance around the conserved epitope may limit its ability to induce antibody production or the ability of an antibody to effectively bind to the epitope. However, if antibodies can bind to amino acid residues within the conserved pocket and block protease cleavage, infectivity will be reduced since the virus cannot infect the host cell without the released HA2 fusion peptide to interact with the host membrane.
MATERIALS AND METHODS
Cloning the gene encoding the HA protein
The rHA construct was designed to represent the mature configuration of HA0. The amino-terminal signal sequence was removed and replaced with Met-Gly amino acid residues. NcoI and NotI restriction sites were incorporated into the construct to facilitate cloning into the pET28 protein expression vector (Novagen, San Diego, CA). In addition, the carboxyl terminal portion spanning viral membrane was deleted and replaced by 3xGly linker and six His amino acid residues followed by multiple stop codons.
The gene encoding the HA protein was amplified by RT-PCR using RNA of influenza virus A/Vietnam/1203/2004 (H5N1) as a template (kindly provided by Kanta Subbarao, LID/NIAID/NIH). Viral RNA was extracted using RNAeasy® (Qiagen, Inc. Valencia, CA) according to the manufacturer's protocol. A 5 μL aliquot of RNA was amplified into a double stranded DNA fragment using Superscript III One-Step® (Invitrogen, Carlsbad, CA) following the manufacturer's protocol. The PCR sense and anti-sense primers are described below. Amplification was carried out using an ABI thermocycler programmed for 45° C for 30 min, then 94° C for 2 min followed by 45 cycles at 94° C for 15 sec, 50° C for 30 sec and 68° C for 3 min. At the end of the 45 cycles, the run-off synthesis was carried out for 7 min at 68° C. The reaction mixture was then stored at 4°C. PCR primer design was based on the viral sequence data provided by the Centers for Disease Control and Prevention (CDC) for A/Vietnam/1203/2004 HA (vaccine strain CDC E2 VN1203-PR8-HA Ruben Donis, CDC, Atlanta, GA) [19].
The PCR primer for the 3’-end of the HA gene produced a truncated rHA gene in which the carboxyl terminal was replaced by six histidine residues (His-6x). In addition, the design incorporated multiple translational stop codons, a Gly-Gly-Gly linker, and recognition sites for restriction enzymes MscI and NotI for cloning into the pET28 protein expression vector. The sequence encoding the His-6x tag can be removed from the expression vector using restriction enzymes MscI and NotI and replacing the gap with a MscI/NotI DNA oligonucleotide linker containing translation stop codons. In this primer, the rare ATA codon for Ile was replaced with ATT. The underlined sequence is identical to the 3’-end of the negative viral RNA strand for the HA gene. The 3’-end primer was named 3HA0H5N1 (84-mer); with the sequence 5’-AAG GAA AAA AGC GGC CGC TCA TTA ATG GTG ATG ATG ATG GTG GCC ACC GCC TTG GTA AAT TCC AAT TGA TTC CAA TTT TAC TCC.
The PCR primer for the 5’-end of the HA gene produced the mature rHA0 protein with the amino-terminal signal sequence removed and replaced with Met-Gly amino acid residues. In addition, the design incorporated an NcoI restriction site for cloning the DNA fragment into the pET28 expression vector. In this primer, the rare ATA codon for Ile was changed to ATT. The underlined sequence is complementary to the 5’-end of the negative strand viral RNA for the HA gene. The 5’-end primer was named 5HA0H5N1 (82-mer); with the sequence CAT GCC ATG GGT GAT CAG ATT TGC ATT GGT TAC CAT GCA AAC AAC TCG ACA GAG CAG GTC GAC ACA ATT ATG GAA AAG AAC G.
The amplified DNA fragment was purified by agarose gel electrophoresis and treated with NcoI and NotI restriction enzymes. The NcoI/NotI DNA fragment was purified by agarose gel electrophoresis and ligated into the NcoI and NotI restriction sites of the E. coli protein expression plasmid, pET28. The ligated plasmid was transformed into E. coli DH5-alpha and selected on LB-agar plates in the presence of 30 μg/ml kanamycin. Antibiotic resistant bacterial colonies were screened for plasmid inserts by direct PCR amplification using T7 promoter and T7 terminator sequencing primers and agarose gel electrophoresis. Mini-preparations of bacterial colonies containing the plasmid with the insert were sequenced for verification of the HA gene sequence by direct DNA sequencing using standard T7 promoter and T7 terminator primers and internal HA gene specific primers. One bacterial colony, which carried the pET plasmid with the correct HA gene sequence, was selected and a maxi-preparation of the plasmid, which we named pET-28HA-5, was prepared from the DH5-alpha E. coli. The purified pET-28HA-5 plasmid was transformed into E. coli BL21(DE3) Rosette II cells (Novagen) and selected on LB agar containing 30 μg/ml kanamycin and 34 μg/ml chloramphenicol. A seed stock of transformed cells was prepared and stored at −70° C in LB media containing 50% glycerol.
Bacterial cell growth condition
A starter culture was grown overnight from frozen stock using Luria Bertani (LB) broth containing kanamycin and chloramphenicol at 37° C with shaking at 250 rpm. A 7.0 liter bench top fermentor (New Brunswick Scientific, Edison, NJ) was charged with 4 liters of modified LB media containing per liter: 10 g Bacto tryptone, 5 g Bacto yeast extract, 5 g K2HPO4, and 5 g NaCl heat sterilized for 30 minutes at 121° C. The media was allowed to cool to 37° C and 10 ml of 1 M MgSO4, 25 g glucose, 30 mg kanamycin, and 34 mg chloramphenicol per liter were added. The fermentor was inoculated with 200 ml of an overnight culture and grown at 37° C. The pH was maintained at 7.0 with the addition of 7 N NH4OH, and the dissolved oxygen was maintained at 30% air saturation (using an adaptive control algorithm interfaced to a MD-Biostat system (Sartorius BBI System INC, Allentown, PA) by adjusting the agitation and the air flow [20]. Protein production was induced by adding IPTG (Sigma, St. Louis, MO) to 1 mM final concentration when the optical density (OD600) of the culture reached 16 (4 hours). The culture continued for an additional 4 hours under the same conditions resulting in a final OD600 of 28. The total fermentor time for this vaccine lot was 8 hours. Bacteria were collected by centrifugation at 8,000 RPM and stored at −20° C until further processing.
Purification of the recombinant HA
Recombinant HA in the inclusion bodies was solubilized with 6M urea later removed by dialysis. Solubilized rHA was bound to Ni+-ion chelation affinity column, washed, and the rHA eluted and analyzed by SDS-PAGE and Western blotting analyses. Anti-His-tag monoclonal antibody and ferret anti-H5 of Vietnamese strain were used for detection.
One hundred fifteen grams of frozen cells collected by centrifugation from the 4-liter fermentor culture supernatant as described in the “Bacterial cell growth condition” were suspended in 400 ml of “lysis buffer” (20 mM Tris-HCl pH 8.0 containing 500 mM NaCl and 5 mM immidazole) at 4° C. The cell suspension was passed twice through a cell disrupter at 9,000 psi (Manton Gaulin homogenizer, APV, NY USA). The broken cell suspension was centrifuged at 14,000 RPM for 40 minutes and the pellet, 66.5 grams, comprised of inclusion bodies with entrapped cellular debris collected and stored at −20° C until further processing. This vaccine preparation lot was assigned lot number NIH20060613.
One gram of washed inclusion bodies was resuspended in “binding buffer” (0.5 M NaCl, 20 mM Tris-HCl, 5 mM immidazole, pH 7.9) containing 6 M urea. The suspension was centrifuged at 12,000 RPM for 30 minutes to remove insoluble material and the supernatant loaded onto a 3 ml chromatography column containing chelating resin (His·Bind® Resin Novagen) charged with Ni-ion and equilibrated with binding buffer containing 6 M urea. The column was washed extensively with binding buffer-urea followed by “washing buffer” (0.5 M NaCl, 20 mM Tris-HCl, 60 mM immidazole, pH 7.9) containing 6 M urea. The rHA was eluted with “elution buffer” (0.5 M NaCl, 20 mM Tris-HCl, 1 M immidazole, pH 7.9) containing 6 M urea and collected in 1 ml fractions. Each fraction was analyzed by SDS-PAGE, or by Western blot analysis following standard procedures [21]. The Western blots were developed using either anti-His tag monoclonal antibody (Novagen) or anti-H5N1 A/Vietnam/1203/2004 ferret serum (CDC, Atlanta, GA). Fractions containing the rHA were pooled and diluted to less than 0.1 mg/ml by slow addition of the pooled fraction to “refolding buffer” (50 mM glycine, 5 mM EDTA, 5 mM DTT, pH 9.0) using rapid stirring and a gravity-fed, 27-gauge needle attached to a 10 ml syringe barrel. The diluted solution containing the rHA was dialyzed against 3 liters of “dialysis buffer” (50 mM glycine, 5 mM EDTA, pH 9.0) with three changes. The dialyzed solution was concentrated using an Amicon® Ultra-10k 10,000 MW spin-filter (Millipore Corp. Billerica, MA) and the protein content of the concentrated solution determined using the BCA Protein Assay reagent (Pierce, Rockford, IL) against a BSA standard.
Adsorption onto alum and treatment with formalin
Alum-adsorption and formalin treatment of rHA employed standard procedures [22]. Alhydrogel® 2% aluminum hydroxide (Brenntag Biosector, Denmark) was used to adsorb the rHA. Formalin treatment, before or after adsorption, used 25 mM lysine and 0.035% formalin [23]. The final vaccine preparation was stored in 0.01% merthiolate at 4° C.
Immunization of mice
Groups of 10 female NIH Swiss mice were injected subcutaneously with either 5 or 15 μg rHA/0.1 ml two or three times two weeks apart. Controls were injected with PBS. Blood samples were collected one week after the last immunization.
Serologic
Anti-HA IgG was measured by enzyme-linked immunosorbent assay (ELISA). Nunc 96-well Flat-bottom Immune® plates (Nalgene Nunc International, Rochester, NY) were coated with rHA at a concentration 2 μg/ml (PBS pH 7.4) (determined by checkerboard titration) at 4° C overnight. Antigen-coated plates were washed six times with “ELISA washing buffer” (0.14 M NaCl, 0.1% Brij 35, 0.02% NaN3) and test and control sera added in duplicates in twofold dilutions. Following overnight incubation at room temperature, the plates were washed six times with Elisa washing buffer and anti-HA specific IgG detected using goat anti-mouse IgG conjugated to alkaline phosphatase (KPL, Gaithersburg, MD) diluted 1:1000 in “ELISA diluent buffer” (PBS pH 7.4 containing 1% BSA and 0.1% Tween). The plates were incubated at room temperature 4 hours and washed six times with Elisa washing buffer. One hundred microliters of freshly prepared substrate (1 mg of 4-nitrophenyl phosphate disodium hexahydrate in 1 ml of “substrate buffer” (1 M Tris-HCl pH 9.8 with 3 mM MgCl2) was added to each well, the enzyme-substrate reaction was carried out at room temperature for 20 min, and absorbance measured at 405 nm. Antibody concentration was calculated from a standard curve of pooled high responders’ serum from this study and assigned a value of 100 ELISA units (EU). The results were analyzed using an ELISA data-processing program (Biostatistics and Information Management Branch, Centers for Disease Control and Prevention) based on a four-parameter logistic-log function with a Taylor series linearization algorithm. Antibody levels are expressed as geometric means (GM) and 25th - 75th centiles.
Hemagglutination inhibition (HI) was performed by standard procedures in 96-well V-bottom plates using 1% (vol/vol) horse red blood cells (HRBC). Sera were pre-treated with receptor destroying enzyme, RDE (II) “Seiken” (Denka Seiken Co., Ltd., Tokyo, Japan) from Vibrio cholerae (1 volume of sera: 3 volume of RDE) for 16 hours at 37° C prior to heat inactivation for 30 min at 56° C and diluted serially twofold in PBS starting at 1:10 and an equal volume of 4 HA units of virus antigen (BPL inactivated avian strain of H5 from CDC) was added to the dilutions. After 15 min incubation at room temperature an equal volume of 1% (v/v) HRBC in PBS was added and the plates read after 1 hour.
RESULTS
Cloning, expression and purification of rHA
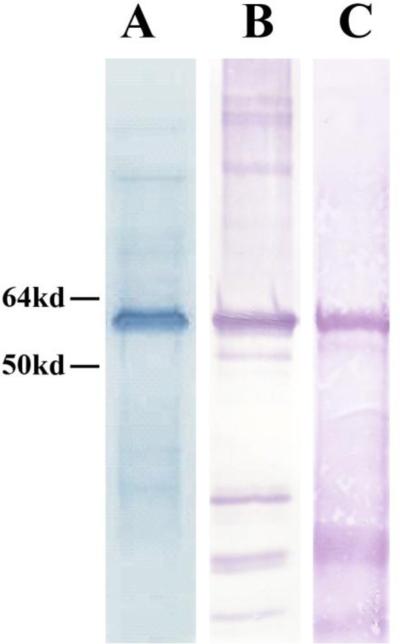
These methods resulted in a non-glycosylated 60 kDa rHA protein of the expected characteristics as judged by polyacrylamide gel electrophoresis and Western blot analysis using anti-His tag monoclonal antibody and ferret serum against the A/Vietnam/1203/2004 virus (Fig.1).
Figure 1.
SDS-PAGE and Western blot analysis of rHA protein purified from inclusion bodies by urea solubilization and Ni-ion chelating chromatography, and refolded. Lane A: 12% SDS-PAGE, Lane B: Western blot using anti-His-tag monoclonal antibody, Lane C: Western blot using anti-H5N1 A/Vietnam/1203/2004 ferret serum.
Serum antibody responses elicited by different rHA vaccine formulations
The pre-immunization levels of all mice were below the detection limit. All four vaccine formulations and two dosages of rHA (5 and 15 μg) were immunogenic and induced booster responses. Alum-adsorbed rHA induced significantly higher IgG anti-rHA than the non-adsorbed preparations. Three injections of the 15 μg/mouse dose induced the highest antibody levels (449 EU). Formalin treatment by itself or before adsorption onto alum made little difference in the immune response: 40.1 vs. 61.5, 212.7 vs. 177.8; NS. However, treatment with formalin after adsorption reduced antibody levels significantly: 10 vs. 40.1, 61.5 p=0.02, 10 vs. 177.8, 212.7 p<0.0001. Among mice immunized with three 5 μg doses, groups injected with rHA-formalin-alum and rHA-alum had the highest antibody levels; GM of 212.7 and 177.8 EU, and 100% and 80% HI titer ≥40 with the Vietnam H5 influenza virus A respectively. (Table 1)
Table 1.
HA antibody levels (EU) and hemagglutination inhibition (HI) response in mice
| G.M. IgG anti-HA | No. with | |||
|---|---|---|---|---|
| Immunogen | Dosage | EU (25-75 centiles) | HI ≥40 | |
| rHA-alum | 5 μg × 2 | 14.4 | (10.6-21.2) | 8/10 |
| rHA-alum | 5 μg × 3 | 177.8 | (112-286) | 8/10 |
| rHA-formalin | 5 μg × 2 | 26.6 | (22.2-41.3) | 8/10 |
| rHA-formalin | 5 μg × 3 | 40.1 | (33.5-52.2 | 10/10 |
| rHA-formalin-alum | 5 μg × 2 | 14.4 | (10.9-20.1) | 3/10 |
| rHA-formalin-alum | 5 μg × 3 | 212.7 | (119.3-270.8) | 10/10 |
| rHA-alum-formalin | 5 μg × 2 | 3.2 | (1.7-9.15) | 5/10 |
| rHA-alum-formalin | 5 μg × 3 | 10.0 | (7.95-17.1) | 9/10 |
| rHA | 5 μg × 3 | 61.5 | (24.7-249) | 9/9 |
| rHA-alum | 15 μg × 3 | 449.4 | (224-757) | 10/10 |
| PBS (control) | 0.01 | (0.005-0.005) | 0/10 | |
Mice, 5-6 week old, were injected s.c. 2 or 3 times 2 weeks apart and bled 1 week after the last injection.
14.4 vs 177.8, 212.7 p<0.0001; 26.6 vs 40.1 p Not Significant (NS);
3.2 vs 10 p NS; 177.8 vs 40.1, 10 p<0.0001; 177.8 vs 212.7 p NS;
449.4 vs 177.8, 212.7 p<0.01
DISCUSSION
Using viral RNA and recombinant DNA technology, we prepared safely, in a short time and in high yield, recombinant H5N1 Vietnam HA suitable for vaccine use. The recombinant protein expressed in E. coli was nonglycosylated and its molecular weight and antigenic characteristics conformed to those of influenza HA. It was immunogenic by itself, showed booster and dose responses and alum adsorption increased the antibody levels. The rHA-induced antibodies demonstrated HI activity though the titers did not correlate with ELISA levels, consistent with findings of other investigators. However, the HI activity is consistent with the FDA guidelines for vaccines against epidemic and pandemic influenza [24, 25].
An advantage of our protocol is that the gene encoding the HA protein can be engineered using only sequence data and modified for optimal production in protein expression systems. Our protocol eliminates the handling of live virus and expensive egg propagation systems or insect cell cultures and facilitates the rapid production (weeks) of high yields of immunogen (275,000 15 μg doses per 50 liter fermentor) compared to current methods requiring one to two eggs per vaccine dose [26] and a minimum of six months after the circulating strain is isolated [2]. We have adapted this procedure for preparation of rHA from the A/Indonesia/5/2005 influenza (H5N1) strain, A/Qinghai/1A/2005 (H5N1) strain, and the A/California/04/2009 (H1N1) pandemic swine strain. This material is currently undergoing testing and evaluation.
Bacterial expression systems are used widely for routine production of recombinant proteins. Several single component influenza H5 virus vaccines have been developed using rHA proteins produced in mammalian, insect and bacterial expression systems. Early test results of these candidate vaccines in animals [27, 28] and in humans are encouraging; however, as shown by Treanor et al. [29] even the highest dose (90 μg) of baculovirus expressed H5 rHA induced a putative protective antibody titer in only 52% of human subjects. Such a vaccine, although well tolerated, is sub-optimal against a pandemic because of the high dosage required and modest immunogenicity. Shen et al. [27] compared the neutralizing antibody response against the N-terminal rHA ectodomain portion (truncated before the HA1/HA2 polybasic cleavage site) produced in bacteria with the full-length rHA of H5N1 virus produced in insect cells. The results of this study indicate that the nonglycosylated HA produced in bacteria elicited neutralizing titers only four times lower than the glycosylated protein expressed in insect cells. Both antisera were similar in inhibiting viral entry into susceptible cells.
Production of influenza vaccines is now sufficient for only one injection before the flu season. An optimal response of naïve individuals to a new protein requires 2-3 doses spaced at least 6 weeks apart [30-34]. While an immunization scheme of three doses against a rapidly evolving virus may be impractical on an annual basis, it would be useful for protection against particularly lethal strains of pandemic influenza. As the past three pandemics occurred in waves, timely protection could be offered through effective vaccination subsequent to the initial wave. Studies with this rHA will include further modification of the protein, assessment in other mammals, and challenge studies with homologous and heterologous viruses. But, the above described methodology for producing a rHA vaccine is cheaper, safer, and more productive than the available technology to meet urgent needs in a world health emergency.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Collins S. Excess Mortality from Causes Other than Influenza and Pneumonia During Influenza Epidemics. Vol. 11. United States Public Health Service; Washington, D.C.: Nov, 1932. p. 1932. [Google Scholar]
- 2.Osterholm MT. Preparing for the next pandemic. The New England journal of medicine. 2005 May 5;352(18):1839–42. doi: 10.1056/NEJMp058068. [DOI] [PubMed] [Google Scholar]
- 3.Wrigley NG. Electron microscopy of influenza virus. British medical bulletin. 1979 Jan;35(1):35–8. doi: 10.1093/oxfordjournals.bmb.a071539. [DOI] [PubMed] [Google Scholar]
- 4.Waterfield MD, Espelie K, Elder K, Skehel JJ. Structure of the haemagglutinin of influenza virus. British medical bulletin. 1979 Jan;35(1):57–63. doi: 10.1093/oxfordjournals.bmb.a071543. [DOI] [PubMed] [Google Scholar]
- 5.Hobson D, Curry RL, Beare AS, Ward-Gardner A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. The Journal of hygiene. 1972 Dec;70(4):767–77. doi: 10.1017/s0022172400022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Potter CW, Oxford JS. Determinants of immunity to influenza infection in man. British medical bulletin. 1979 Jan;35(1):69–75. doi: 10.1093/oxfordjournals.bmb.a071545. [DOI] [PubMed] [Google Scholar]
- 7.Virelizier JL. Host defenses against influenza virus: the role of anti-hemagglutinin antibody. J Immunol. 1975 Aug;115(2):434–9. [PubMed] [Google Scholar]
- 8.Robbins JB, Schneerson R, Szu SC. Perspective: hypothesis: serum IgG antibody is sufficient to confer protection against infectious diseases by inactivating the inoculum. J Infect Dis. 1995 Jun;171(6):1387–98. doi: 10.1093/infdis/171.6.1387. [DOI] [PubMed] [Google Scholar]
- 9.Belshe RB, Gruber WC, Mendelman PM, Mehta HB, Mahmood K, Reisinger K, et al. Correlates of immune protection induced by live, attenuated, cold-adapted, trivalent, intranasal influenza virus vaccine. J Infect Dis. 2000 Mar;181(3):1133–7. doi: 10.1086/315323. [DOI] [PubMed] [Google Scholar]
- 10.Treanor J, Wright PF. Immune correlates of protection against influenza in the human challenge model. Developments in biologicals. 2003;115:97–104. [PubMed] [Google Scholar]
- 11.Schild GC, Oxford JS, Virelizier JL. Immunity to influenza. Developments in biological standardization. 1975;28:253–72. [PubMed] [Google Scholar]
- 12.Meiklejohn G, Eickhoff TC, Graves P, I J. Antigenic drift and efficacy of influenza virus vaccines, 1976--1977. J Infect Dis. 1978 Nov;138(5):618–24. doi: 10.1093/infdis/138.5.618. [DOI] [PubMed] [Google Scholar]
- 13.Barry RD, Mahy BW. The influenza virus genome and its replication. British medical bulletin. 1979 Jan;35(1):39–46. doi: 10.1093/oxfordjournals.bmb.a071540. [DOI] [PubMed] [Google Scholar]
- 14.Wang R, Soll L, Dugan V, Runstadler J, Happ G, Slemons RD, et al. Examining the hemagglutinin subtype diversity among wild duck-origin influenza A viruses using ethanol-fixed cloacal swabs and a novel RT-PCR method. Virology. 2008 May 25;375(1):182–9. doi: 10.1016/j.virol.2008.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett DJ, Balicer RD, Lucey DR, Everly GS, Jr., Omer SB, Steinhoff MC, et al. A systematic analytic approach to pandemic influenza preparedness planning. PLoS medicine. 2005 Dec;2(12):e359. doi: 10.1371/journal.pmed.0020359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic. Bulletin of the history of medicine. 2002;76(1):105–15. doi: 10.1353/bhm.2002.0022. Spring. [DOI] [PubMed] [Google Scholar]
- 17.Prabhu N, Prabakaran M, Ho HT, Velumani S, Qiang J, Goutama M, et al. Monoclonal antibodies against the fusion peptide of hemagglutinin protect mice from lethal influenza A virus H5N1 infection. J Virol. 2009 Mar;83(6):2553–62. doi: 10.1128/JVI.02165-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sui J, Hwang WC, Perez S, Wei G, Aird D, Chen LM, et al. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nature structural & molecular biology. 2009 Mar;16(3):265–73. doi: 10.1038/nsmb.1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Subbarao K, Katz JM. Influenza vaccines generated by reverse genetics. Current topics in microbiology and immunology. 2004;283:313–42. doi: 10.1007/978-3-662-06099-5_9. [DOI] [PubMed] [Google Scholar]
- 20.Hsiao J, Ahluwalia M, Kaufman JB, Clem TR, Shiloach J. Adaptive control strategy for maintaining dissolved oxygen concentration in high density growth of recombinant E. coli. Annals of the New York Academy of Sciences. 1992 Oct 13;665:320–33. doi: 10.1111/j.1749-6632.1992.tb42595.x. [DOI] [PubMed] [Google Scholar]
- 21.Burnette WN. “Western blotting”: electrophoretic transfer of proteins from sodium dodecyl sulfate--polyacrylamide gels to unmodified nitrocellulose and radiographic detection with antibody and radioiodinated protein A. Analytical biochemistry. 1981 Apr;112(2):195–203. doi: 10.1016/0003-2697(81)90281-5. [DOI] [PubMed] [Google Scholar]
- 22.Taylor DN, Trofa AC, Sadoff J, Chu C, Bryla D, Shiloach J, et al. Synthesis, characterization, and clinical evaluation of conjugate vaccines composed of the O-specific polysaccharides of Shigella dysenteriae type 1, Shigella flexneri type 2a, and Shigella sonnei (Plesiomonas shigelloides) bound to bacterial toxoids. Infection and immunity. 1993 Sep;61(9):3678–87. doi: 10.1128/iai.61.9.3678-3687.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nencioni L, Volpini G, Peppoloni S, Bugnoli M, De Magistris T, Marsili I, et al. Properties of pertussis toxin mutant PT-9K/129G after formaldehyde treatment. Infection and immunity. 1991 Feb;59(2):625–30. doi: 10.1128/iai.59.2.625-630.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.FDA. In: Guidance for industry: clinical data needed to support the licensure of seasonal inactivated influenza vaccines. Research CfBEa, editor. U.S. Food and Drug Administration; 2007. [Google Scholar]
- 25.Noah DL, Hill H, Hines D, White EL, Wolff MC. Qualification of the hemagglutination inhibition assay in support of pandemic influenza vaccine licensure. Clin Vaccine Immunol. 2009 Apr;16(4):558–66. doi: 10.1128/CVI.00368-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tree JA, Richardson C, Fooks AR, Clegg JC, Looby D. Comparison of large-scale mammalian cell culture systems with egg culture for the production of influenza virus A vaccine strains. Vaccine. 2001 May 14;19(25-26):3444–50. doi: 10.1016/s0264-410x(01)00053-6. [DOI] [PubMed] [Google Scholar]
- 27.Shen S, Mahadevappa G, Oh HL, Wee BY, Choi YW, Hwang LA, et al. Comparing the antibody responses against recombinant hemagglutinin proteins of avian influenza A (H5N1) virus expressed in insect cells and bacteria. J Med Virol. 2008 Nov;80(11):1972–83. doi: 10.1002/jmv.21298. [DOI] [PubMed] [Google Scholar]
- 28.Wei CJ, Xu L, Kong WP, Shi W, Canis K, Stevens J, et al. Comparative efficacy of neutralizing antibodies elicited by recombinant hemagglutinin proteins from avian H5N1 influenza virus. J Virol. 2008 Jul;82(13):6200–8. doi: 10.1128/JVI.00187-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Treanor JJ, Wilkinson BE, Masseoud F, Hu-Primmer J, Battaglia R, O'Brien D, et al. Safety and immunogenicity of a recombinant hemagglutinin vaccine for H5 influenza in humans. Vaccine. 2001 Feb 8;19(13-14):1732–7. doi: 10.1016/s0264-410x(00)00395-9. [DOI] [PubMed] [Google Scholar]
- 30.Schutze H. The optimal spacing of vaccine inoculation. J Path Bact. 1941;53:443–51. [Google Scholar]
- 31.Fecsik AI, Butler WT, Coons AH. Studies on Antibody Production. Xi. Variation in the Secondary Response as a Function of the Length of the Interval between Two Antigenic Stimuli. J Exp Med. 1964 Dec 1;120:1041–9. doi: 10.1084/jem.120.6.1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pittman PR, Mangiafico JA, Rossi CA, Cannon TL, Gibbs PH, Parker GW, et al. Anthrax vaccine: increasing intervals between the first two doses enhances antibody response in humans. Vaccine. 2000 Sep 15;19(2-3):213–6. doi: 10.1016/s0264-410x(00)00174-2. [DOI] [PubMed] [Google Scholar]
- 33.Myers MG, Beckman CW, Vosdingh RA, Hankins WA. Primary immunization with tetanus and diphtheria toxoids. Reaction rates and immunogenicity in older children and adults. Jama. 1982 Nov 19;248(19):2478–80. [PubMed] [Google Scholar]
- 34.Zimmerman RK. Adult vaccination, part 1: vaccines indicated by age. Teaching Immunization for Medical Education (TIME) Project. The Journal of family practice. 2000 Sep;49(9 Suppl):S41–50. [PubMed] [Google Scholar]