Abstract
A patient with locally advanced adenocarcinoma of the rectum was operated with abdominoperineal resection and perineal reconstruction with a vertical rectus abdominis musculocutaneous flap. Six days postoperatively, there was herniation of the small bowel, between the anterior and posterior rectus sheaths, to a subcutaneous location.
Keywords: Vertical rectus abdominis musculocutaneous flap, perineal defect, rectal adenocarcinoma
Introduction
The vertical rectus abdominis musculocutaneous flap (VRAM) is a reliable method for primary closure of perineal skin defects up to medium size, which otherwise might have been left for healing by secondary intention [1–18]. The VRAM-flap is indicated not only for closure of perineal skin defects, following (e.g. abdominoperineal resection of the rectum), but also for reconstruction of the posterior vaginal wall and not the least obliteration of dead-space in the pelvis following resection of the levator ani muscles [2,4,5,9,19,20]. The flap provides well-vascularized tissue in an area, which frequently has been subjected to preoperative radiation therapy, and may contribute to wound healing [11,16–20]. The flap can further prevent herniation of the bowel to a subcutaneous location in the perineum if the muscular portion of the flap is sutured to the remnants of the levator ani muscles [9,13,15,17,18].
Following flap harvest, the donor site can usually be closed without excessive tension. Lateral undermining above the abdominal fascia can, if necessary, be performed to facilitate skin closure if a wide skin paddle has been used. The hernia is the most common donor site complication with a reported incidence of 19% [21], followed by skin infections reported in 15–21% [22–24].
Wound infection is the most common perineal complication, reported in 10–12% of patients in retrospective as well as prospective studies. Wound dehiscence has been reported in 7–11% of the patients and wound abscess in 3–4% [6,22,23,25]. Less common complications in the perineum are partial or total flap and/or fat necrosis in the case of pedicle kinking or twisting [6,8,11,15,16,18].
Patient and method
Our report concerns a 52-year-old male patient presenting with an adenocarcinoma of the rectum T4b, N1b, M0 with metastatic spread to mesorectal lymph nodes and engagement of the right levator muscle. Preoperatively, the patient received 50.4 Gy radiation therapy and concomitant chemotherapy with Capecitabine (Xeloda®). The tumor downsized whereupon the patient was operated with an abdominoperineal resection of the rectum. Due to engagement of the levator muscles and need of a wide skin excision, a reconstruction of the perineum with a musculocutaneous VRAM-flap was planned.
In the supine position, a standard abdominoperineal resection was first performed. A VRAM flap was then elevated with a skin island positioned vertically over the right rectus muscle, from slightly below the level of the umbilicus to the xiphoid. The entire posterior rectus sheath, as well as the anterior rectus sheath below the umbilicus, were left intact, and the rectus muscle was divided at the costal margin. The cranial tip of the elevated VRAM flap skin island was sutured to the rectal specimen, carefully securing a correct orientation of the flap when transferring it into the pelvic cavity to prevent twisting of the pedicle.
The rectus sheath was repaired with a double PDS suture. A colostomy was constructed through the left rectus abdominis muscle before turning the patient to a prone position.
After completion of the posterior dissection and removal of the rectum, the VRAM flap was pulled out through the perineal defect. The lateral and medial edges of the rectus muscle and the anterior rectus sheath were sutured to the remnants of the levator muscles. After de-epithelization of the distal portion of the skin island, the remaining island skin was sutured to the surrounding perineal skin.
Six days postoperatively, the patient presented with nausea and gastric retention. Bowel discharge ceased. A CT-scan showed small intestinal herniation at the level of the umbilicus (Figures 1 and 2). The patient was readmitted to OR and a herniation of the small bowel between the anterior rectus sheath of the lower abdomen and arcuate line/posterior rectus sheath was found. The bowel was considered viable and was repositioned into the abdomen followed by renewed and reinforced suturing of the upper posterior to the lower anterior rectus sheath. Particular care was taken when suturing the linea semilunaris/arcuate line. Healing was thereafter without complications, and the patient could quickly be mobilized and subsequently discharged. At follow-up three weeks after discharge, the perineal and the donor areas had healed, and no signs of an incisional hernia or abdominal bulging were evident.
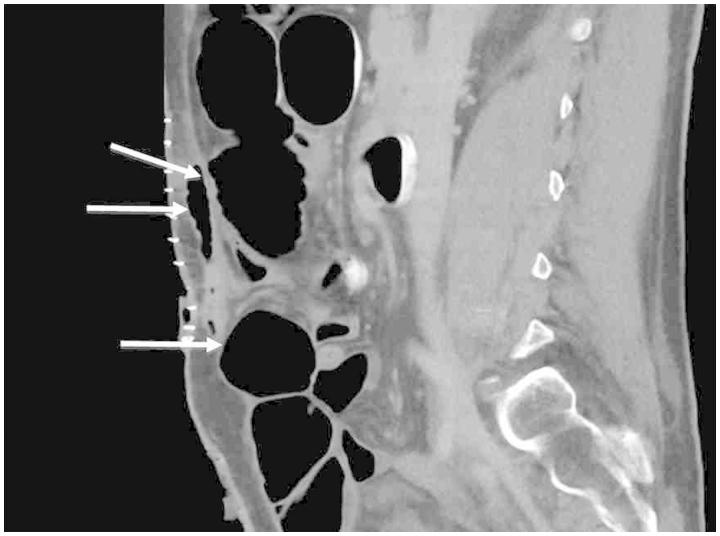
Figure 1.
Postoperative CT sagittal view. Posterior rectus sheath (top arrow). Herniated small bowel beneath the staple-lines (middle arrow). Semilunar line (lower arrow).
Figure 2.
Postoperative CT, transverse view. White arrow showing subcutaneously located small bowel loop anterior to the rectus sheath. Intra-abdominally dilated and fluid-filled proximal loops of small bowel are visualized. Left rectus abdominis muscle (black arrow).
At 1 year follow-up, the flap was viable and the perineum well healed. There were no signs of herniation, neither in the abdomen nor perineum. Unfortunately, a routine CT-scan showed signs of tumor recurrence with peritoneal carcinomatosis.
Conclusion
There are several options for perineal flap reconstruction, such as the gracilis flap, the inferior gluteal artery flap and the omental flap [24,26–28]. An elegant, but technically more challenging, solution for perineal reconstruction is the rectus muscle sparing perforator flap based on the deep inferior epigastric vessels [29].
In our experience, however, the VRAM-flap is robust, quick and useful for closure of perineal skin defects alone or with defects in the posterior vaginal wall. The flap further eliminates pelvic dead space if a wide resection of the levator ani muscles has been necessary. Commonly, the right rectus abdominis muscle is used as the donor site, as the left usually is used for construction of a colostomy.
Our case illustrates that the semilunar or arcuate line, i.e. where the posterior rectus sheath connects to the peritoneum, can be a locus minoris resistentiae with respect to herniation of bowel when raising a VRA flap. The semilunar line is sometimes rather a gradual distal thinning, than a distinct structure (Figure 3), of the posterior rectus fascia below the level of the umbilicus. We have not routinely used alloplastic mesh for donor site reinforcement, but it must be considered if any risk factor of an incisional hernia is present [28,30,31]. No such risk factors were identified in our patient.
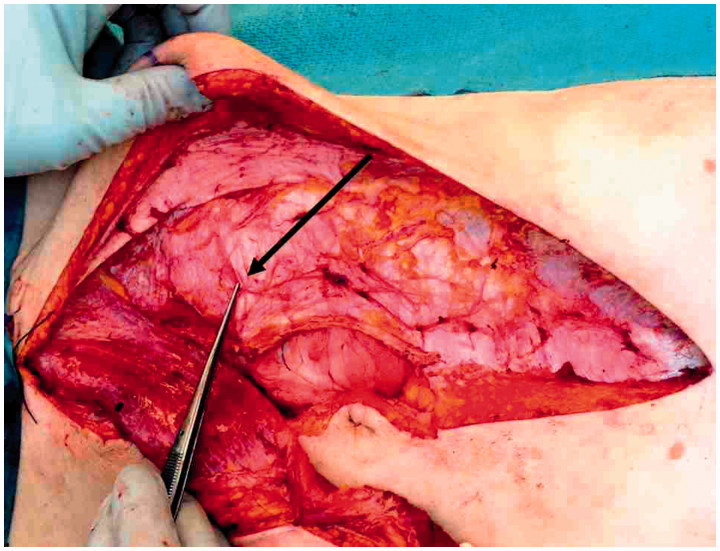
Figure 3.
Intraoperative illustration of linea seminlunaris/arcuate line (arrow).
We suggest that the skin and fascial incision of the VRAM flap below the level of the umbilicus is limited, if possible, in order to enable a strong suture of the anterior rectus fascia to the distal part of the posterior rectus sheath. Particular attention is to be taken in suturing the linea semilunaris/posterior rectus sheath of the upper abdomen to the anterior rectus sheath of the lower abdomen if the linea semilunaris is indistinct.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- 1.Kroll SS, Pollock R, Jessup JM, Ota D.. Transpelvic rectus abdominis flap reconstruction of defects following abdominal-perineal resection. Am Surg 1989;55:632–7. [PubMed] [Google Scholar]
- 2.Carlson JW, Soisson AP, Fowler JM, Carter JR, Twiggs LB, Carson LF.. Rectus abdominis myocutaneous flap for primary vaginal reconstruction. Gynecol Oncol 1993;51:323–9. [DOI] [PubMed] [Google Scholar]
- 3.McAllister E, Wells K, Chaet M, Norman J, Cruse W.. Perineal reconstruction after surgical extirpation of pelvic malignancies using the transpelvic transverse rectus abdominal myocutaneous flap. Ann Surg Oncol 1994;1:164–8. [DOI] [PubMed] [Google Scholar]
- 4.Khoo AK, Skibber JM, Nabawi AS, Gurlek A, Youssef AA, Wang B, et al. Indications for immediate tissue transfer for soft tissue reconstruction in visceral pelvic surgery. Surgery 2001;130:463–9. [DOI] [PubMed] [Google Scholar]
- 5.Buchel EW, Finical S, Johnson C.. Pelvic reconstruction using vertical rectus abdominis musculocutaneous flaps. Ann Plast Surg 2004;52:22–6. [DOI] [PubMed] [Google Scholar]
- 6.Chessin DB, Hartley J, Cohen AM, Mazumdar M, Cordeiro P, Disa J, et al. Rectus flap reconstruction decreases perineal wound complications after pelvic chemoradiation and surgery: a cohort study. Ann Surg Oncol 2005;12:104–10. [DOI] [PubMed] [Google Scholar]
- 7.Galandiuk S, Jorden J, Mahid S, McCafferty MH, Tobin G.. The use of tissue flaps as an adjunct to pelvic surgery. Am J Surg 2005;190:186–90. [DOI] [PubMed] [Google Scholar]
- 8.Houvenaeghel G, Ghouti L, Moutardier V, Buttarelli M, Lelong B, Delpero JR.. Rectus abdominis myocutaneous flap in radical oncopelvic surgery: a safe and useful procedure. Eur J Surg Oncol 2005;31:1185–90. [DOI] [PubMed] [Google Scholar]
- 9.Bell SW, Dehni N, Chaouat M, Lifante JC, Parc R, Tiret E.. Primary rectus abdominis myocutaneous flap for repair of perineal and vaginal defects after extended abdominoperineal resection. Br J Surg 2005;92:482–6. [DOI] [PubMed] [Google Scholar]
- 10.Persichetti P, Cogliandro A, Marangi GF, Simone P, Ripetti V, Vitelli CE, et al. Pelvic and perineal reconstruction following abdominoperineal resection: the role of gracilis flap. Ann Plast Surg 2007;59:168–72. [DOI] [PubMed] [Google Scholar]
- 11.Butler CE, Gündeslioglu AO, Rodriguez-Bigas MA.. Outcomes of immediate vertical rectus abdominis myocutaneous flap reconstruction for irradiated abdominoperineal resection defects. J Am Coll Surg 2008;206:694–703. [DOI] [PubMed] [Google Scholar]
- 12.Nelson RA, Butler CE.. Surgical outcomes of VRAM versus thigh flaps for immediate reconstruction of pelvic and perineal cancer resection defects. Plast Reconstr Surg 2009;123:175–83. [DOI] [PubMed] [Google Scholar]
- 13.Hinojosa MW, Parikh DA, Menon R, Wirth GA, Stamos MJ, Mills S.. Recent experience with abdominal perineal resection with vertical rectus abdominis myocutaneous flap reconstruction after preoperative pelvic radiation. Am Surg 2009;75:995–9. [PubMed] [Google Scholar]
- 14.Nisar PJ, Scott HJ.. Myocutaneous flap reconstruction of the pelvis after abdominoperineal excision. Colorectal Dis 2009;11:806–16. [DOI] [PubMed] [Google Scholar]
- 15.Creagh TA, Dixon L, Frizelle FA.. Reconstruction with vertical rectus abdominus myocutaneous flap in advanced pelvic malignancy. J Plast Reconstr Aesthet Surg 2012;65:791–7. [DOI] [PubMed] [Google Scholar]
- 16.Chokshi RJ, Kuhrt MP, Arrese D, Martin EW Jr.. Reconstruction of total pelvic exenteration defects with rectus abdominus myocutaneous flaps versus primary closure. Am J Surg 2013;205:64–70. [DOI] [PubMed] [Google Scholar]
- 17.Horch RE, Kneser U, Weber K, Hohenberger W, Dragu A.. The transpelvic vertical rectus abdominis flap: one interdisciplinary approach to reduce postoperative complications after surgery for rectal cancer. Ann Surg 2013;257:e16. [DOI] [PubMed] [Google Scholar]
- 18.Horch RE, Hohenberger W, Eweida A, Kneser U, Weber K, Arkudas A, et al. A hundred patients with vertical rectus abdominis myocutaneous (VRAM) flap for pelvic reconstruction after total pelvic exenteration. Int J Colorectal Dis 2014;29:813–23. [DOI] [PubMed] [Google Scholar]
- 19.Horch RE, Gitsch G, Schultze-Seemann W.. Bilateral pedicled myocutaneous vertical rectus abdominus muscle flaps to close vesicovaginal and pouch-vaginal fistulas with simultaneous vaginal and perineal reconstruction in irradiated pelvic wounds. Urology 2002;60:502–7. [DOI] [PubMed] [Google Scholar]
- 20.D'Souza DN, Pera M, Nelson H, Finical SJ, Tran NV.. Vaginal reconstruction following resection of primary locally advanced and recurrent colorectal malignancies. Arch Surg 2003;138:1340–3. [DOI] [PubMed] [Google Scholar]
- 21.McMenamin DM, Clements D, Edwards TJ, Fitton AR, Douie WJ.. Rectus abdominis myocutaneous flaps for perineal reconstruction: modifications to the technique based on a large single-centre experience. Ann R Coll Surg Engl 2011;93:375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abbott DE, Halverson AL, Wayne JD, Kim JY, Talamonti MS, Dumanian GA.. The oblique rectus abdominal myocutaneous flap for complex pelvic wound reconstruction. Dis Colon Rectum 2008;51:1237–41. [DOI] [PubMed] [Google Scholar]
- 23.Barker T, Branagan G, Wright E, Crick A, McGuiness C, Chave H.. Vertical rectus abdominis myocutaneous flap reconstruction of the perineal defect after abdominoperineal excision is associated with low morbidity. Colorectal Dis 2013;15:1177–83. [DOI] [PubMed] [Google Scholar]
- 24.Touny A, Othman H, Maamoon S, Ramzy S, Elmarakby H.. Perineal reconstruction using pedicled vertical rectus abdominis myocutaneous flap (VRAM). J Surg Oncol 2014;110:752–7. [DOI] [PubMed] [Google Scholar]
- 25.Chan S, Miller M, Ng R, Ross D, Roblin P, Carapeti E, et al. Use of myocutaneous flaps for perineal closure following abdominoperineal excision of the rectum for adenocarcinoma. Colorectal Dis 2010;12:555–60. [DOI] [PubMed] [Google Scholar]
- 26.Yamamoto T, Mylonakis E, Keighley MR.. Omentoplasty for persistent perineal sinus after proctectomy for Crohn's disease. Am J Surg 2001;181:265–7. [DOI] [PubMed] [Google Scholar]
- 27.Woods JE, Beart RW Jr.. Reconstruction of nonhealing perineal wounds with gracilis muscle flaps. Ann Plast Surg 1983;11:513–16. [DOI] [PubMed] [Google Scholar]
- 28.Weiwei L, Zhifei L, Ang Z, Lin Z, Dan L, Qun Q.. Vaginal reconstruction with the muscle-sparing vertical rectus abdominis myocutaneous flap. J Plast Reconstr Aesthet Surg 2009;62:335–40. [DOI] [PubMed] [Google Scholar]
- 29.Santanelli F, Paolini G, Renzi L, Persechino S.. Preliminary experience in reconstruction of the vulva using the pedicled vertical deep inferior epigastric perforator flap. Plast Reconstr Surg 2007;120:182–6. [DOI] [PubMed] [Google Scholar]
- 30.Mathes SJ, Bostwick J 3rd.. A rectus abdominis myocutaneous flap to reconstruct abdominal wall defects. Br J Plast Surg 1977;30:282–3. [DOI] [PubMed] [Google Scholar]
- 31.Petrie N, Branagan G, McGuiness C, McGee S, Fuller C, Chave H.. Reconstruction of the perineum following anorectal cancer excision. Int J Colorectal Dis 2009;24:97–104. [DOI] [PubMed] [Google Scholar]