Repeated experience with dichoptic perceptual learning tasks and dichoptic game play have been shown to be effective in improving the visual acuity of amblyopic children and adults.1–4 However, whether the visual acuity gains achieved with binocular treatment are long lasting has not yet been addressed. We examined the durability of visual acuity improvements obtained as a result of binocular iPad game play in childhood amblyopia.
Methods
This study protocol was approved by the University of Texas Southwestern Medical Center Institutional Review Board. Written informed consent was obtained from a parent or guardian prior to enrollment in the study. Amblyopic children aged 4 to 12 years who participated in our previous study of binocular iPad games,4 had best-corrected visual acuity (BCVA) improvement of at least 0.1 logMAR (1.0 line; Snellen equivalent 20/25) in the amblyopic eye after 4 to 8 weeks of compliant binocular iPad game play, and did not patch after cessation of iPad game play were eligible for enrollment in the follow-up study. For comparison, we also enrolled children whose amblyopic eye BCVA had improved at least 0.1 logMAR after 4 to 12 weeks of compliant binocular iPad game play but who did patch after cessation of binocular iPad game play. The referring pediatric ophthalmologist decided whether the child had concurrent patching treatment (at a different time of day) during the binocular iPad game play or afterward. The inclusion criteria and protocol of our previous study are available online.4 The BCVA was obtained for each eye with the Amblyopia Treatment Study HOTV method5 (for those aged <7 years) or electronic Early Treatment Diabetic Retinopathy Study method6 (for those aged ≥7 years) at the baseline and outcome visits and 3, 6, and 12 months after the outcome visit.
Results
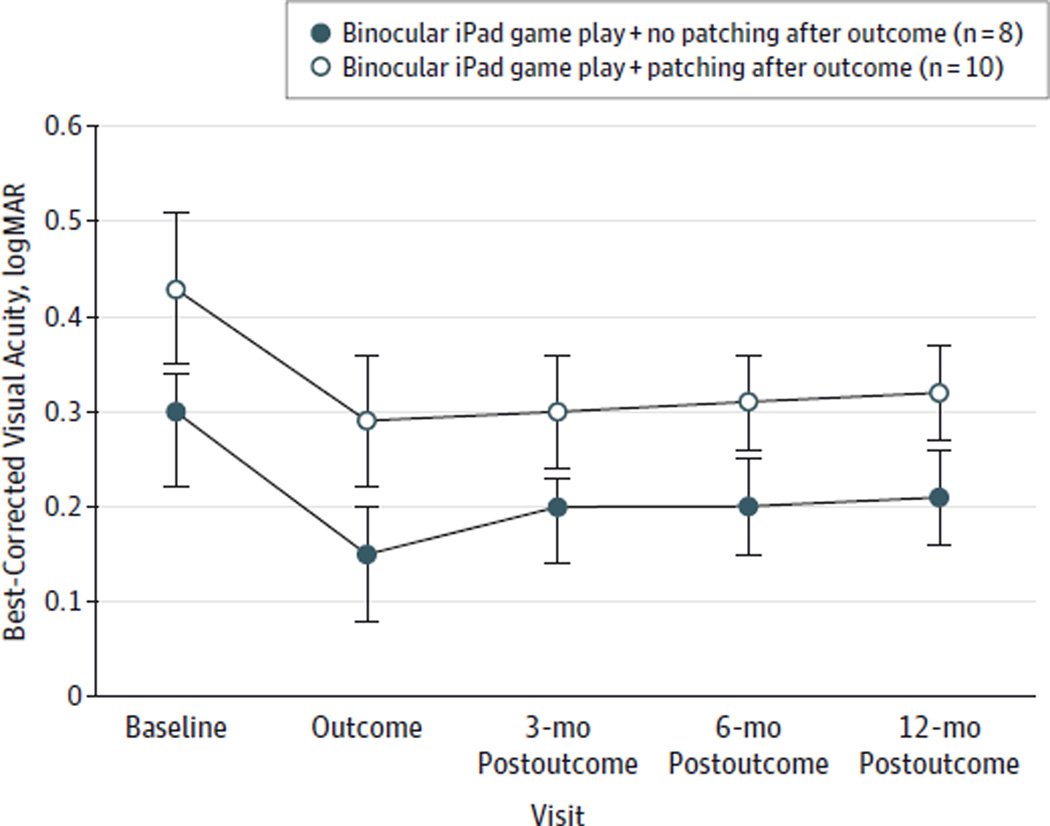
Eight amblyopic children aged 4.8 to 12.7 years were enrolled in the primary group with binocular iPad game play and no patching after outcome, and 10 children aged 4.0 to 10.2 years were enrolled in the group with binocular iPad game play and patching after outcome. Amblyopic eye BCVA at each time is illustrated in the Figure. For the primary group with binocular iPad game play and no patching after outcome, the mean (SE) baseline BCVA improved from 0.30 (0.04) logMAR at baseline to 0.15 (0.05) logMAR (Snellen equivalent, improvement from 20/40 to 20/28) after 4 to 8 weeks of binocular iPad game play. For the group with binocular iPad game play and patching after outcome, the mean (SE) baseline BCVA improved from 0.43 (0.08) logMAR at baseline to 0.29(0.07) logMAR (Snellen equivalent, improvement from 20/54 to 20/39) after 4 to 12 weeks of binocular iPad game play. A2-way repeated-measures analysis of variance (visit by postoutcome treatment) found a main effect of visit on visual acuity (F1,16 = 10.77; P < .001) but was not able to identify an effect of patching after outcome on visual acuity (F4,64 = 2.41; P = .14). Pairwise post hoc comparisons found that baseline BCVA was significantly different from the BCVAs at the outcome visit and the 3-, 6-, and 12-month postoutcome visits (P < .001), but the BCVAs did not differ between the outcome and postoutcome visits (P ≥ .58).
Figure. Best-Corrected Visual Acuity of Amblyopic Eyes at Each Visit.
Best-corrected visual acuity of amblyopic eyes at each visit for participants in the primary group with binocular iPad game play and no patching after outcome vs those in the group with binocular iPad game play and patching after outcome. Each data point represents the mean; error bars, standard error.
Discussion
To our knowledge, this study provides the first evidence that BCVA improvements obtained with binocular iPad game play are retained for at least 12 months after the treatment ends. Along with our previous study,4 this demonstrates that home-based binocular iPad games may be an effective treatment for amblyopia. Compared with the traditional patching treatment, which usually takes months to years, the binocular iPad game play appears to improve visual acuity rapidly (in only weeks).
Acknowledgments
Funding/Support: This work was supported by grant EY022313 from the National Eye Institute, a 2013 postdoctoral award from Fight for Sight, and the Crystal Charity Ball, Dallas, Texas.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Drs Li and Birch had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Stager, Birch.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Li.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Li.
Obtained funding: Birch.
Administrative, technical, or material support: Jost, Morale, De La Cruz, Dao.
Study supervision: Stager, Birch.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
References
- 1.Hess RF, Thompson B, Black JM, et al. An iPod treatment of amblyopia: an updated binocular approach. Optometry. 2012;83(2):87–94. [PubMed] [Google Scholar]
- 2.Li J, Thompson B, Deng D, Chan LY, Yu M, Hess RF. Dichoptic training enables the adult amblyopic brain to learn. Curr Biol. 2013;23(8):R308–R309. doi: 10.1016/j.cub.2013.01.059. [DOI] [PubMed] [Google Scholar]
- 3.Hess RF, Babu RJ, Clavagnier S, Black J, Bobier W, Thompson B. The iPod binocular home-based treatment for amblyopia in adults: efficacy and compliance. Clin Exp Optom. 2014;97(5):389–398. doi: 10.1111/cxo.12192. [DOI] [PubMed] [Google Scholar]
- 4.Li SL, Jost RM, Morale SE, et al. A binocular iPad treatment for amblyopic children. Eye (Lond) 2014;28(10):1246–1253. doi: 10.1038/eye.2014.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moke PS, Turpin AH, Beck RW, et al. Computerized method of visual acuity testing: adaptation of the Amblyopia Treatment Study visual acuity testing protocol. Am J Ophthalmol. 2001;132(6):903–909. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 6.Beck RW, Moke PS, Turpin AH, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135(2):194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]