Abstract
Paracoccidioidomycosis (PCM) is the most common endemic mycosis in Latin America. The etiological agents, which comprise two species, Paracoccidioides brasiliensis and P. lutzii, are thermodimorphic fungi that usually affect previously healthy adults. They primarily involve the lungs and then disseminate to other organs. Such mycosis is rare in organ transplant recipients; there have been only three cases reported in literature, until now. We report a case of PCM in a renal transplant recipient with an unusual dermatological presentation.
Keywords: Paracoccidioidomycosis, Paracoccidioides, Kidney transplantation, Immunosuppression
INTRODUCTION
Fungal infections comprise only 5% of all infections in renal transplant recipients. Both epidemiological exposure and the state of immunosuppression determine the type of systemic fungal infection. Candida and Aspergillus species are the most frequently reported fungal pathogens causing infection following renal transplantation1 , 2.
Paracoccidioidomycosis (PCM) is an endemic infection in Latin America; the etiological agents3, which include two species, P. brasiliensis and P. lutzii, are thermodimorphic fungi that usually affect previously healthy adults. They primarily involve the lungs and then disseminate to other organs. However, such mycosis is rare in organ transplant recipients. There have only been three cases reported in literature, until now, that presented such mycosis complicating the transplantation of solid organs, all of which being renal transplant recipients2 , 4 , 5.
We present one more case of PCM in an organ transplant recipient, with unusual dermatological presentation.
CASE REPORT
A white, sixty-six-year-old man born and residing in Miracema,Rio de Janeiro, was admitted in August 2014 for having had cough for three months, weight loss of six kg in a month, and febrile episodes over the 10 previous days. The patient underwent renal transplantation in January 2013 and he was using prednisone, 5 mg/day; mesalazine, 1,080 mg/day; and tacrolimus, 8 mg/day. He had systemic arterial hypertension, diabetes mellitus and gout, controlled with oral medications. He used to visit a farm and perform soil management frequently. Physical examination showed good general conditions, there was no palpable lymphadenopathy; dermatological examination revealed shallow ulcerated lesions on the palate surrounded by erythema, measuring about 8 mm; multiple mulberry-like erythematous eroded papules giving to the lesion a cobblestone appearance (Aguiar-Pupo stomatitis); erythematous papule with a central umbilication of about 3 mm located at the left nasal wing (Fig. 1); and an infiltrated erythematous plaque with irregular borders and indistinct boundaries, of approximately 1 cm in diameter, located on the left flank (Fig. 2).
Fig. 1. - Erythematous papule with a central umbilication in the left nasal wing, shallow ulcerated lesions on the palate and Aguiar Pupo stomatitis.

Fig. 2. - Infiltrated erythematous plaque on the left flank.

Chest x-rays showed bilateral nodular infiltrate, so it was started empirical treatment for tuberculosis and bacterial pneumonia. AFB bronchial lavage was negative however, the direct mycological examination found fungal structures compatible with paracoccidioidomycosis. Biopsies in the described mucocutaneous lesions were performed, including oral ulcers, which were consistent with this diagnosis (Fig. 3). All materials were subjected to culture and there was growth of P. brasiliensis. Itraconazole, 400 mg daily, was started, but after five days of treatment the patient had clinical worsening and liposomal amphotericin B was introduced. The basal serum cortisol was normal and abdominal CT scan showed no specific changes; however, in lung CT (Fig. 4) an extensive involvement with bilateral nodular infiltrates, an excavated area suggestive of necrosis in the middle third of the right lung, and bilateral pleural effusion, largest in the right lung, were seen. Despite the prescribed therapies, the patient died.
Fig. 3. - A and B - Chronic granulomatous process with pseudoepitheliomatous hyperplasia and ulceration with numerous fungal cells (H&E X40); C - numerous oval / round cells with multiple budding, like a "pilot wheel" cell (Groccot X40).
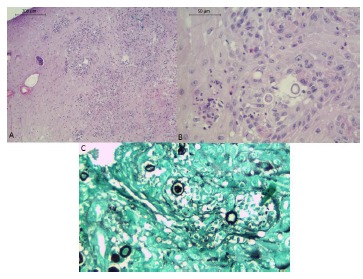
Fig. 4. - Bilateral nodular infiltrates, excavated area with suggestive area of necrosis in the middle third of the right lung and bilateral pleural effusion.

DISCUSSION
PCM is the most common endemic mycosis in Latin America. Brazil is the country with the largest number of cases of the disease, with an estimated incidence ranging between 10-30 cases/million of inhabitants, and a mortality rate of 1.4 deaths/million of inhabitants. PCM diagnosis is based on clinical symptoms, direct microscopic examination of clinical specimens, isolation of fungus in culture, and detection of specific antibodies by serological techniques4 , 6.
The systemic mycoses most observed in the immediate post-transplant period are coccidioidomycosis and histoplasmosis while PCM and blastomycosis are rare2. PCM in solid organ transplant patients was firstly reported in 19847, with similar presentation in an immunocompetent patient; then in 19955, with severe pulmonary infection that progressed to death; and in 20042, with similar presentation in an immunocompetent patient with unusual radiological findings. This case is the fourth to be reported in literature. In previous reports, patients followed immunosuppressive regimens with combinations of azathioprine, cyclosporine and prednisone. The clinical manifestations of PCM were atypical, with unusual pulmonary manifestations8. The mean time for onset of fungal infections following transplantation was 11 years; in the present case it was one year and seven months, beyond having presented unusual skin lesions, not described in any of the previous PCM cases.
Several radiological findings are found in PCM, but none are pathognomonic. The most common is a mixed alveolar and interstitial infiltrate diffusely distributed in both lungs. Cavitations are infrequent and when present are small, single or multiple, located around central areas of the lungs2 , 9. Therefore, the present report is even rarer for its unusual radiological presentation.
Regarding treatment, amphotericin B deoxycholate (classical amphotericin B) in doses of 0.75 to 1.0 mg/kg/day, at a total dose equivalent of 30 mg/kg of body weight, and itraconazole at doses of 200 to 400 mg/day for six to 12 months, are the therapeutic options10. Maintenance treatment is indicated and can be performed weekly or biweekly with amphotericin B or itraconazole 200 mg/day. We must always consider the possibility of drug interactions between these drugs and those routinely used by transplant patients8.
This case demonstrates the importance of early diagnosis and intervention in diseases that affect immunosuppressed patients; although PCM is an endemic mycosis in Brazil, it is not reported frequently in this group of patients. In addition, if there is appearance of skin lesions, they should always be addressed for early diagnosis.
REFERENCES
- 1.Patel R, Paya CV. Infections in solid-organ transplant recipients. Clin Microbiol Rev. 1997;10:86–124. doi: 10.1128/cmr.10.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zavascki AP, Bienardt JC, Severo LC. Paracoccidioidomycosis in organ transplant recipient: case report. Rev Inst Med trop Sao Paulo. 2004;46:279–281. doi: 10.1590/s0036-46652004000500009. [DOI] [PubMed] [Google Scholar]
- 3.Gegembauer G, Araujo LM, Pereira EF, Rodrigues AM, Paniago AMM, Hahn RC. Serology of paracoccidioidomycosis due to Paracoccidioides lutzii. PLoS Negl Trop Dis. 2014;8:12. doi: 10.1371/journal.pntd.0002986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rassi TNO, Passos RRB, Kumagai KM, Soranz JE, Filho, Freitas JAH. Paracoccidioidomicose crônica multifocal tendo como primeira manifestação o envolvimento palpebral: relato de caso. Arq Bras Oftalmol. 2009;72:822–825. doi: 10.1590/s0004-27492009000600016. [DOI] [PubMed] [Google Scholar]
- 5.Shikanai-Yasuda MA, Duarte MI, Nunes DF, Lacaz CS, Sabagga E, Abdala E. Paracoccidioidomycosis in a renal transplant recipient. J Med Vet Mycol. 1995;33:411–414. doi: 10.1080/02681219580000781. [DOI] [PubMed] [Google Scholar]
- 6.Vieira G de D, Alves T da C, Lima SM, Camargo LM, Sousa CM. Paracoccidioidomycosis in a western Brazilian Amazon State: clinical-epidemiologic profile and spatial distribution of the disease. Rev Soc Bras Med Trop. 2014;47:63–68. doi: 10.1590/0037-8682-0225-2013. [DOI] [PubMed] [Google Scholar]
- 7.Sugar AM, Restrepo A, Stevens DA. Paracoccidioidomycosis in the immunosuppressed host: report of a case and review of the literature. Am Rev Respir Dis. 1984;129:340–342. [PubMed] [Google Scholar]
- 8.Marques SA. Paracoccidioidomicose e esporotricose associada à imunossupressão. Med Cutan Iber Lat Am. 2009;37:159–170. [Google Scholar]
- 9.Magalhães AEA, Guerrini R. Franco M, Lacaz CS, Restrepo-Moreno A, Del Negro G. Paracoccidioidomycosis. Boca Raton: CRC Press; 1994. Roentgenographic patterns of chest lesions. The use of computerized tomography in paracoccidioidomycosis.281-8 [Google Scholar]
- 10.Shikanay-Yasuda MA, Telles FQ, Filho, Mendes RP, Colombo AL, Moretti ML. Consenso em paracoccidioidomicose. Rev Soc Bras Med Trop. 2006;39:297–310. doi: 10.1590/s0037-86822006000300017. [DOI] [PubMed] [Google Scholar]


