Introduction
Adolescence is marked by a multitude of physiological and psychosocial transitions (Blakemore, Berenbaum, & Liben, 2009; Susman & Dorn, 2009). These changes, compounded with academic and social pressures and shifts in family dynamics characteristic of this period, may induce significant stress, frequently on a daily basis. As a result, roughly one-fourth of all adolescents are diagnosed with a depression or anxiety disorder prior to graduating high school (Johnson & Greenberg, 2013). Others, however, seem to navigate the challenges of this period with minimal hardship, finding their way through the disappointments and struggles of this period with comparatively fewer scars than their counterparts (Compas, 2004).
What personality traits or distinctive ways of managing daily stressors might contribute to these different outcomes? Self-compassion, defined as treating oneself with kindness when confronted with difficulties, maintaining perspective amid life’s challenges, and understanding that challenges are inherent in the human condition (Neff, Kirkpatrick, & Rude, 2007), may protect against negative self-evaluation, thereby holding anxiety and depression at bay. For example, social self-preservation theory (Dickerson & Kemeny, 2004) suggests that negative self-evaluation results in a physiological stress response via hypothalamic-pituitary-adrenal (HPA) axis activation. According to this theory, one is constantly monitoring the environment for potential threats to one’s social status and then builds physiological, psychological, and behavioral responses to defend against these threats. Social support is one mechanism that helps to protect adolescents from these social threats and is linked to healthy adjustment (Hauser & Bowlds, 1990). Self-compassion may be viewed as social support turned inwards (Breines et al., 2014), providing a way in which adolescents can directly support themselves emotionally. Therefore, one would expect that those with higher self-compassion would evidence a diminished physiological stress response in the presence of a social stressor than those with lower self-compassion.
In fact, Breines et al. (2014, 2015) reported evidence of this effect. Adults with higher self-compassion exhibited lower interleukin-6 production, an inflammatory marker, and lower salivary alpha amylase production, a marker of sympathetic nervous system activation, in response to the Trier Social Stress Test (TSST), an acute laboratory social stressor which participants generally interpret as threatening to social status (Breines et al., 2014, 2015). Extending these findings, a brief, self-compassion training was reported to buffer effects of the TSST when compared to an attention and no-training control condition (Arch et al., 2014). Those who had experienced the self-compassion training demonstrated significantly lower salivary alpha-amylase production and higher heart rate variability in response to the social stressor, both of which are indicators of a lower stress response. Subjective measures reflected this finding; individuals in the self-compassion training self-reported less anxiety than those in the control condition. Furthermore, Rockliff et al. (2008) found that for adults who have close relationships and experience the world as safe, a self-compassion imagery induction resulted in greater increases in heart rate variability and decreases in cortisol, indicative of lowered sympathetic and hypothalamic pituitary adrenal (HPA) axis stress, respectively, compared to a relaxation or control imagery task.
Leary, Tate, Adams, Allen, and Hancock (2007) undertook several studies investigating how self-compassion enables undergraduate students to cope with unpleasant life events. In one of the investigated studies in which individuals were asked to imagine how they would react to negative events, individuals with high self-compassion predicted that they would be better able to depersonalize the experience of defeat without catastrophizing, and to maintain equanimity compared to those with low self-compassion. In a second study in which participants believed that they were being evaluated on a videotaped task, those with high self-compassion were more adept at managing feedback about their performance. These high self-compassionate individuals responded to both positive and neutral feedback similarly; those with low self-compassion attributed positive feedback more to themselves and negative feedback less to themselves. The authors concluded that self-compassion may be a protective factor and buffer against unpleasant life events (Leary et al., 2007). In a mock job interview, Neff et al. (2007) asked undergraduates to write their answer to the question “What is your greatest weakness? Tell me about a time or situation in the past when this has affected you.” Results indicated that self-compassion had a protective effect against the experience of anxiety (Neff et al. 2007). In addition, a recent meta-analysis of correlational studies concluded that self-compassion has strong inverse associations with psychopathology in adults (MacBeth & Gumley, 2012).
Yet despite these important findings, there are few published studies examining self-compassion among adolescents. Among the few, there are similar to that of adults, inverse associations were reported between self-compassion and both perceived stress and negative affect, and positive associations between self-compassion and life satisfaction in a sample of students from a private middle school and a public high school in the southeast U.S. (Bluth & Blanton, 2014a). Additionally, Neff and McGehee (2010) found comparable relationships in a sample of adolescents age 14–17 from a private high school in the southwest U.S.; self-compassion correlated negatively with depression and anxiety and positively with social connectedness (Neff & McGehee, 2010). In another study, self-compassion was positively correlated with self-esteem and negatively with aggression in a population of 16–18 year old males in a residential program for adolescents who had dropped out of school (Barry, Loflin, & Doucette, 2015).
The potential protective effect of self-compassion is demonstrated in several recently published studies. For example, recognizing that adolescents with low self-esteem experience lower mental health than those with higher self-esteem, self-compassion was reported to moderate the link between self-esteem and mental health in a large sample of Australian 9th and 10th graders. Those adolescents with higher self-compassion demonstrated a weaker association between self-esteem and mental health in this longitudinal study (Marshall et al., 2015). Finally, self-compassion was reported to have a protective role in guarding against the potentially negative effects of a traumatic event (the Mount Carmel Forest Fire disaster) in a sample of 15–19 year olds in Israel. In this study which used a mediational cross-lagged analysis, findings indicated that higher levels of self-compassion at two separate time points predicted lower levels or less increase of post-traumatic stress and panic symptoms in the ensuing time points. Additionally, self-compassion was inversely associated with depression and suicidality symptoms at each of the three separate time points (Zeller, Yuval, Nitzan-Assayag, and Bernstein, 2014).
Although this burgeoning research demonstrates the potentially protective effects of self-compassion on stress in adolescents, no known research has expanded this investigation to explore how self-compassion might be associated with the physiological stress response to a social stressor. The current study addresses this gap in the literature. We hypothesize that a) adolescents with high self-compassion will report greater emotional wellbeing (i.e., less perceived stress, anxiety and negative affect, greater life satisfaction and positive affect) than those with low self-compassion, and b) adolescents with high self-compassion will exhibit a lower physiological stress response (i.e., lower cortisol output, greater heart rate variability and more complete recovery following stressor, less increase in heart rate and blood pressure) than those with low self-compassion when exposed to a social stressor in a laboratory setting.
Method
Participants
Upon university IRB approval, participants were recruited through flyers posted in the community and via listservs through the university community and the Program on Integrative Medicine at a university medical school. To be eligible, participants had to be between age 13 and 18, read and understand English, and score below 10 on the Kutcher Adolescent Depression Scale (LeBlanc, Almudevar, Brooks, & Kutcher, 2002). In addition, adolescents were excluded if they endorsed an item on the scale indicating that they had thoughts of self-injury or suicide. Participants in the study were 76% female (n = 22) and 24% male (n = 7). Forty-one percent of participants (n = 12) were age 13–14, 38% (n = 11) were age 15–16, and 21% (n = 6) were age 17–18; 17% (n = 5) were Black/African American, 62% (n = 18) were White, 7% (n = 2) were Asian, 10% (n = 3) were Hispanic/Latino and 3% (n = 1) were “other”. Eighty-six percent (n = 25) of participants’ mothers and 70% (n = 20) of participants’ fathers had at least a college degree, and 24% (n = 7) of participants’ mothers and 17% (n = 5) of participants fathers had a doctorate or professional degree.
Procedure
Participants for this study were part of an intervention study. The intervention study (results of which will be reported elsewhere) included a six-week mindfulness course that focused on developing skills to bring one’s attention and awareness to the present moment and an active control condition which was a healthy lifestyle course. Both courses were presented weekly to participants in 1.5 hour classes. The procedures and results reported here are from the baseline measures of the intervention study, which consisted of a laboratory assessment and online survey. Participants were compensated a total of $35 for their participation in the initial lab and online survey.
Upon arriving at the study location, parents/guardians provided written consent and adolescents provided written assent. Adolescents were then taken into the laboratory and asked to sit in a comfortable chair. During the initial 20 minute baseline period, blood pressure (BP) and heart rate (HR) were assessed at minutes 0, 3, 6, 10, 13, 15 and 18 and heart rate variability (HRV) was monitored continuously for two 5-minute intervals during the last 10 minutes of the 20 minute baseline. At the end of this period, participants provided a baseline saliva sample for cortisol testing and completed the Spielberger State Anxiety Scale (SSAI; Spielberger, Gorsuch, & Lushene, 1970).
A research assistant then explained the details of the Trier Social Stress Test (TSST; Kirschbaum, Pirke, & Hellhammer, 1993), a well-validated social evaluative stressor that has been demonstrated to produce a significant physiological stress response (Kirschbaum, Strasburger, & Langkrar, 1993; von Kanel, Kudielkac, Preckelb, Hanebuthb, & Fischerb, 2006). In keeping with established protocol, participants were given five minutes to prepare a speech, five minutes to give a speech, and five minutes to subtract seven serially from 2023 in front of two ‘committee members’ who were instructed not to engage the participants in any non-essential conversation. The preparation, speech, and serial subtraction tasks were performed in front of a video camera and with a microphone (although video/audio was not actually recorded). The protocol was adapted for this adolescent population in that participants were told that the speech was about their ideal summer job, and the ‘committee members’ were instructed to nod or smile rather than maintain a neutral, cold expression (pilot-testing revealed that the cold facial expression elicited a crying response in several adolescent girls which was deemed to be unacceptable by the investigators). Participants were told that if they performed well on this task they would receive a $5 bonus. Blood pressure (BP) and heart rate (HR) were measured at minutes 0, 2, and 4 during each of the preparation, speech and serial subtraction tasks, and HRV was measured continuously for the entire five-minute preparation period. At the completion of the TSST, a second cortisol sample was taken and participants completed the second SSAI. A 20-minute recovery period followed, in which participants continued to sit in a chair while HR and BP were measured at minutes 0, 3, 5, 8, 14, 17, and 19, and HRV assessed continuously over two separate five minute intervals. Salivary cortisol was sampled during recovery at minutes 0, 10, and 20 after cessation of the TSST since HPA-axis responses to stress are reliably found in this time frame (Harkness, Stewart & Wynne-Edwards, 2011; Peckins, Dockray, Eckenrode, Heaton, & Susman, 2012).
After completion of the laboratory assessment, participants left and three days prior to the beginning of the intervention, they received an email with a link to an online survey comprised of the subjective measures. All surveys were completed prior to the first intervention class. Upon completion of the intervention and the second laboratory assessment, adolescents were fully debriefed about the purpose of the TSST procedure. They were told that they performed as well as the other adolescents, and that this was a fictitious procedure intentionally designed to be difficult and to elicit a stress response. All participants received the $5 bonus, in addition to the $30 compensation for completing the initial lab and online survey.
Measures
Blood pressure and heart rate
The Suntech Exercise BP monitor, Model 4240 (SunTech Medical Instruments, Inc., Raleigh, NC) provided automated measurement of BP and HR during the sessions. The Suntech Exercise BP monitor uses the auscultatory technique, with R-wave Gating. This BP monitor is accurate within ±2 mmHg between 0 mmHg and 300 mmHg. Prior to initiating the baseline rest period, three standard stethoscopic blood pressures were taken simultaneously with the automated pressures in order to ensure correct microphone placement and cuff positioning.
Cortisol
Saliva samples were collected by passive drool. Participants rinsed their mouth 10 minutes prior to collection and had no large meal within the past hour. They were then given a two-inch long plastic drinking straw and a cryovial, instructed to think of their favorite food, and allow saliva to pool in their mouth. With head tilted forward, participants drooled down the straw to collect saliva in the cryovial. All samples were stored at −80°C until batch assay and were then assayed using a highly sensitive enzyme immunoassay (Salimetrics, State College, PA). The lower limit of sensitivity is <0.007 ug/dL (<0.19313 nmol/L) and the standard curve range in the assay is 0.012 ug/dL to 3.0 ug/dL (0.33108 nmol/L to 82.77 nmol/L). The test used 25 uL of saliva per determination and samples were assayed in duplicate. The criteria for repeated testing were variation between duplicates of greater than 15%, and the average of duplicates was used in all analyses. Intra-assay and inter-assay coefficients of variations were 2.5% and 5.7%, respectively.
Heart rate variability
EKG data was assessed via 3 EKG leads and were exported into CardioEdit software (Brain–BodyCenter, University of Illinois at Chicago), where heart periods were visually inspected for artifacts. Editing was conducted by integer arithmetic (e.g., dividing intervals when detections were missed) and CardioBatch software (Brain–Body Center, University of Illinois at Chicago) was used to obtain respiratory sinus arrhythmia (RSA) which is an index of parasympathetic nervous system activity. CardioBatch uses the Porges method (Porges, 1985) to obtain RSA.
Self-Compassion
Self-Compassion Scale (SCS; Neff, 2003) is a 26-item measure in which participants indicate their responses to each item using a 5-point Likert-type scale ranging from 1 (Almost Never) to 5 (Almost Always). Higher score indicates greater self-compassion. Construct validity was established through a reported negative correlation with the self-criticism subscale of the Depression Experience Questionnaire, a positive correlation with the Social Connectedness scale, and all three subscales of the Trait-Meta Mood Scale (Neff, 2003). Content and discriminant validity were also established. Reported reliability is .93 (Neff, 2003; Neff et al., 2007). This scale has been used to measure self-compassion in a number of studies with adolescents (e.g., Barry, Loflin & Doucette, 2015; Bluth & Blanton, 2014a,b; Neff & McGehee, 2010), and Cronbach’s alphas have been reported between .75 and .90.
Life satisfaction
Student’s Life Satisfaction Scale (SLSS; Huebner, 1991) is a 7-item scale which measures how one broadly evaluates one’s life. Participants indicated responses to each item using a 4-point Likert-type scale ranging from 0 (never) to 3 (almost always). Higher scores indicate greater life satisfaction. Construct and discriminant validity have been established and reported Cronbach alphas for adolescent samples are between .82 to .86 (Dew & Huebner, 1994; Gilman & Huebner, 1997; Huebner, 1991).
Perceived Stress
Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) is a well-established 14-item scale that is designed to assess the degree to which respondents find their lives “unpredictable, uncontrollable, and overloading” (Cohen et al., 1983). Participants indicated their responses to each item using a 5-point Likert-type scale ranging from 0 (never) to 4 (very often). Construct validity in an adolescent sample has been established and reported reliability is .86 (Martin, Kazarian, & Breiter, 1995).
Positive and negative affect
Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988) is a well-validated measure containing two subscales, one of which contains 10 emotion words that assess positive emotions (e.g., strong, proud, excited) and the other of which contains 10 words that assess negative emotions (e.g., nervous, distressed, upset). Participants indicate their responses of how they have felt over the last few days using a 4-point scale ranging from 1 (very slightly or not at all) to 4 (most of the time). Higher scores for PA indicate higher positive affect, and higher scores for NA indicate higher negative affect. Cronbach’s alphas are reported as .84 to .87 for negative affect and .86 to .90 for positive affect (Watson et al., 1988). Discriminant and convergent validity has been established in adolescent samples (Huebner & Dew, 1995; Melvin & Molloy, 2000) and the two-factor structure has been confirmed in adolescent samples (Crocker, 1997).
Spielberger State Anxiety Inventory. (SSAI; Spielberger et al., 1970)
This measure is a widely used 20-item measure of state anxiety with good psychometric properties. Respondents rated their current levels of anxiety on a 4-point Likert-type scale ranging from 1 (not at all) to 4 (very much so). Reported reliabilities range from .65 and .96 (Barnes, Harp, & Jung, 2002).
Analytic Strategy
Analyses were completed with Stata Software, Version 13 (StataCorp, LP, College Station, TX). All variables used in the analyses were examined for univariate distributions with histograms and univariate tests for normality, using the Shapiro-Wilk test. Variable transformations were chosen based on a ladder of powers procedure (Tukey, 1977) and through inspection of quantile plots of the transformed variables. Several variables were statistically significantly non-normal according to the Shapiro-Wilk test: the self-compassion score, the baseline anxiety score, the diastolic blood pressure change (ΔDBP) during the speech task, the heart rate change variables during all tasks, cortisol AUCi, and one of the heart rate variability measures. Most of these variables were successfully transformed as documented by the Shapiro-Wilk test and inspection of the quantile plot. Self-compassion scores, cortisol AUCi, and ΔDBP variables were log-transformed and the heart rate change variables were square-root transformed. Unfortunately, change in heart rate during the preparation period and heart rate variability response to the TSST remained non-normal (Shapiro-Wilk test) after transformation. Consequently, in the tables, medians are reported along with means for these variables, along with p values based on Wilcoxon rank-sum tests.
To determine if the TSST induced a significant stress response, we conducted repeated measures analysis of variance (RM-ANOVA) with physiologic data and a paired t-test with SSAI. We assessed changes in cortisol by first normalizing the data using a log-transformation and then measuring the area under the curve with respect to increase (AUCi) using the formula from Pruessner et al. (Pruessner, Hellhammer, Pruessner, & Lupien, 2003). We then examined change in HR and BP by averaging the values within each period (baseline, preparation, speech, serial subtraction, recovery) to establish a mean systolic (SBP), diastolic (DBP), and heart rate (HR) value for each period, and created cardiovascular reactivity scores for each period (mean stressor value – mean baseline value). For HRV, the two 5-minute HRV intervals in the baseline period were averaged, as were the two 5-minute HRV intervals in the recovery period. We then conducted repeated measures analysis of variance (RM-ANOVA) to determine significant change.
To test our hypotheses as to whether those high in self-compassion would self-report higher emotional wellbeing and indicate a lower stress response than those low in self-compassion, we sought to examine how those with low and high self-compassion differed on self-reported measures of wellbeing and physiological stress responses. We used the median split to dummy code self-compassion into a dichotomous variable; those with high self-compassion were at the median or higher (HSC) and those with low self-compassion were below the median (LSC). Median split approach has been used in similar studies to examine difference between groups high and low in a specific variable (Campbell, Labelle, Bacon, Faris, and Carlson, 2012; Pace et al., 2009; Pace et al., 2010). We then compared means of the different variables across the two self-compassion groups (i.e., HSC and LSC) using a series of independent t-tests. If the variables were non-normal by the Shapiro-Wilk test, nonparametric (Wilcoxon rank-sum) tests were conducted to ensure that violation of assumptions did not impact interpretations. In addition, effect size calculations were performed using variables transformed to approximate normality.
Since recent statistical reporting guidelines recommend using effect sizes rather than statistical significance (Cumming, 2014; Kline, 2013), effect sizes are included here using Hedges’ g, an effect size estimate that includes a correction factor for small samples (Borenstein, Hedges, Higgens, & Rothstein, 2009). Nonsignificant findings with Hedges’ g > .20 (consistent with more than a small effect) are interpreted as meaningful; a small effect size is .20, a moderate effect size is .50, and a large effect size is .80 (Borenstein et al., 2009; Kline, 2013).
In addition to the median split analyses, we explored the relationships between self-compassion scores as a continuous variable and the measures of wellbeing and physiologic stress response with linear regression models. We calculated the difference in each measure with a one unit increase in the self-compassion score (beta coefficient) as well as a standardized beta in both unadjusted models and models controlling for race (white vs. other) and gender (male vs. female). Adjusted models are reported because of large mean differences across race and gender in self-compassion and many of the dependent variables, defining race and gender as potential confounding variables. Where the variable distributions were significantly non-normal (Shapiro-Wilk test), we used transformed variables. We calculated mean difference values based on the untransformed variables, but used the transformed variables to calculate standardized coefficients and p-values.
Results
Demographic variables according to HSC and LSC are presented in Table 1. T-tests were conducted, and no significant differences were found between groups except for gender and BP (gender: χ2(1, N = 28) = 5.73; p<.05; SBP: t(26) = −2.10, p<.05; DBP: t(26) = −2.48, p<.05). All six males in the study were in the high self-compassion group. LSC had lower resting SBP and DBP than HSC but that is likely driven by the greater number of females in LSC since females have lower resting BP than males (Reckelhoff, 2001).
Table 1.
Demographics and baseline physiologic measures of sample of male and female adolescents age 13–18 (n = 28)
| Frequency (Percent) | ||
|---|---|---|
|
| ||
| HSC | LSC | |
|
| ||
| Variables | ||
| Gender | ||
| Male | 6 (38) | |
| Female | 10 (63) | 12 (100) |
| Age | ||
| 13–14 | 7 (44) | 5 (42) |
| 15–16 | 4 (25) | 7 (58) |
| 17–18 | 5 (31) | |
| Highest education level of parents | ||
| 4-year college degree or less | 8 (50) | 2 (17) |
| Advanced degree | 8 (50) | 10 (83) |
| Race/Ethnicity | ||
| White | 8 (50) | 10 (83) |
| Other (Black, Asian, Hispanic/Latino) | 8 (50) | 2 (17) |
| Mean (SD) Baseline SBP (mmHg) | 110.82 (7.71) | 104.12 (9.19) |
| Mean (SD) Baseline DBP (mmHg) | 65.17 (4.32) | 61.14 (4.17) |
| Mean (SD) Baseline HR (bpm) | 74.08 (11.95) | 75.39 (6.57) |
| Mean (SD) Baseline Cortisol (ug/dL) | .06 (.04) | .09 (.04) |
| Mean (SD) Baseline RSA | 7.10 (.93) | 7.36 (.71) |
Note. HSC–high self-compassion group; LSC–low self-compassion group;
SBP-systolic blood pressure; DBP-diastolic blood pressure; HR-heart rate;
RSA-Respiratory sinus arrhythmia (measure of heart rate variability);
We conducted a RM-ANOVA to determine if the TSST induced the anticipated stress response. For all RM-ANOVA analyses, the test of sphericity was significant indicating that the variance was not equal at each time point; we therefore interpreted the Greenhouse-Geisser test. Results indicated a significant effect of phase such that SBP, DBP, HR, and cortisol increased from baseline in response to the TSST then returned to close to baseline levels during recovery. As expected, RSA decreased from baseline levels during the preparation phase of the TSST and then returned to close to baseline levels (SBP: F(1, 28)=134.41, p < .001, DBP: F(1, 28) = 154.98, p < .001; HR: F(1, 28) = 51.62, p < .001; cortisol: F(1, 28) = 4.21, p < .05, RSA: F(1, 28) = 18.81, p < .001. Also, self-reported anxiety increased significantly from pre-to post-TSST (pre-TSST: M = 33.55, SD = 7.46; post-TSST: M = 80.86, SD = 11.32; t(28) = −8.15, p < .001). Levels of stress biomarkers at each time-point are included in Table 2.
Table 2.
Mean and standard deviation values of physiological stress before, during, and after TSST in a sample of male and female adolescents age 13–18 (n=28)
| Mean (SD) | |||||
|---|---|---|---|---|---|
|
| |||||
| Baseline | Prep (TSST) | Speech (TSST) | Math (TSST) | Recovery | |
| SBP (mmHg) | 108.53 (9.26) | 120.93 (12.10) | 130.70 (13.19) | 126.28 (11.28) | 111.56 (7.58) |
| DBP (mmHg) | 63.44 (4.56) | 72.11 (6.65) | 78.43 (6.86) | 75.63 (6.65) | 66.57 (6.17) |
| HR (bpm) | 74.79 (9.72) | 90.90 (14.94) | 92.77 (17.27) | 92.48 (16.19) | 76.94 (8.61) |
| RSA | 7.19 (.83) | 6.52 (1.08) | - | - | 7.09 (.82) |
|
| |||||
| Baseline | Immediately post TSST | +10 min post TSST | +20 min post TSST | ||
|
| |||||
| Cortisol (ug/dL) | .08 (.04) | .10 (.07) | .12 (.10) | .10 (.08) | |
Note. TSST-Trier Social Stress Test; SBP-systolic blood pressure; DBP-diastolic blood pressure; HR-heart rate; RSA-Respiratory sinus arrhythmia (measure of heart rate variability);
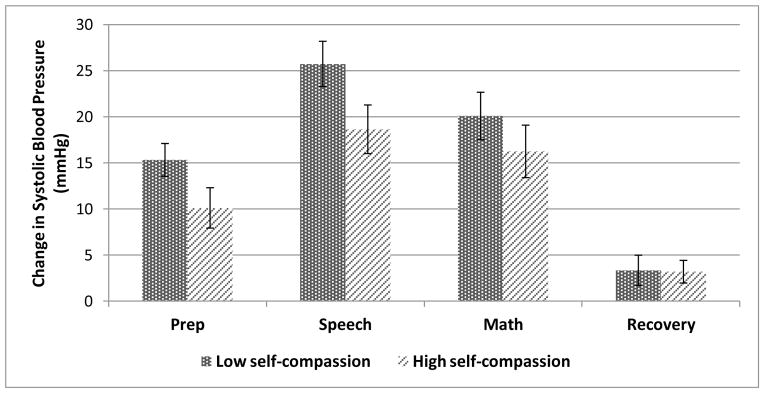
Results of the median split analysis indicated that the associations between HSC and LSC and self-reported measures of wellbeing (assessed from the online survey) were different on most variables in the expected directions (Table 3); that is, adolescents in LSC perceived themselves as being more stressed and anxious and less satisfied with their lives than those in HSC. Effect sizes for all these pre-intervention self-report variables were greater than .20 indicating a meaningful difference between groups (Borenstein et al., 2009). Second, we used a series of independent t-tests to examine if associations between levels of self-compassion and physiological stress responses to the TSST differed as well. Results indicated meaningful differences between groups (i.e., Hedges’ g > 0.20) in all measures except DBP reactivity to speech, and HR reactivity to speech and math (Table 4). No meaningful differences were seen between groups for cortisol, or heart rate variability. The difference between groups in change in SBP is depicted in Figure 1.
Table 3.
Results for mean differences of low and high self-compassion on indicators of wellbeing in a sample of male and female adolescents age 13–18 (n = 28)
| Mean (SD) [Median]
|
t statistic [z statistic] | Hedge’s g (95% CI) | ||
|---|---|---|---|---|
| LSC (n = 12) | HSC (n = 16) | |||
| Baseline anxiety | 36.50 (8.25) [33.5] | 31.75 (6.38) [30.5] | 1.72 [1.65] | 0.64 [−0.11, 1.38] |
| Perceived Stress | 32.08 (5.66) | 27.50 (7.76) | 1.73 | 0.64 [0.11, 1.39] |
| Negative Affect | 24.50 (7.72) | 20.62 (6.67) | 1.42 | 0.53 [0.21, 1.27] |
| Positive Affect | 29.67 (6.02) | 31.19 (8.19) | −0.54 | −0.20 [−0.91, 0.53] |
| Life Satisfaction | 2.33 (0.38) | 2.72 (0.65) | −1.86 | −1.18 [−0.93, 0.53] |
| Δ Anxiety TSST | 20.50 (3.03) | 15.12 (3.05) | 1.22 | 0.45 [−0.29, 1.18] |
Note. HSC–High self-compassion group; LSC–Low self-compassion group; TSST-Trier Social Stress Test; Due to a non-normal distribution, the t statistic and Hedge’s g for baseline anxiety are calculated with the square-root transformed variable. In addition, the medians and z statistics are reported for this variable.
Table 4.
Mean differences of low and high self-compassion on physiological stress reactivity to TSST during the preparatory phase, speech, and math tasks in a sample of male and female adolescents age 13–18 (n = 28)
| Mean (SD) [Median]
|
t statistic [z statistic] | Hedge’s g (95% CI) | ||
|---|---|---|---|---|
| LSC (n = 12) | HSC (n = 16) | |||
| ΔSBP (prep) | 15.34 (6.16) | 10.14 (8.75) | 1.76 | 0.65 [−0.10, 1.40] |
| ΔSBP (speech) | 25.74 (8.52) | 18.66 (10.53) | 1.91 | 0.71 [−0.04, 1.46] |
| ΔSBP (math) | 20.10 (8.93) | 16.26 (11.40) | 0.96 | 0.36 [−0.38, 1.09] |
| ΔDBP (prep) | 9.80 (3.91) | 7.79 (6.20) | 0.98 | 0.41 [−0.32, 1.15] |
| ΔDBP (speech) | 14.97 (5.08) [13.67] | 14.29 (5.64) [12.64] | 0.47 [0.53] | 0.17 [−0.55, 0.90] |
| ΔDBP (math) | 12.69 (4.84) | 11.12 (6.30) | 0.72 | 0.27 [−0.46, 1.00] |
| ΔHR (prep) | 17.98 (13.39) [14.14] | 14.77 (11.85) [12.05] | 0.32 [0.50] | 0.13 [−0.64, 0.88] |
| ΔHR (speech) | 17.77 (14.63) [9.57] | 17.98 (15.55) [15.19] | 0.04 [−0.325] | 0.01 [−0.71, 0.74] |
| ΔHR (math) | 19.41 (14.78) [16.29] | 16.92 (15.25) [12.12] | 0.38 [0.418] | 0.14 [−0.59, 0.87] |
| Cortisol (AUCi) | 1.16 (2.34) [0.05] | 0.43 (1.07) [0.12] | 0.31 [0.51] | 0.12 [−0.61, 0.84] |
| RSA (prep-baseline) | −0.78 (0.61) [−0.79] | −0.63 (1.01) [−0.40] | −0.45 [−1.11] | 0.17 [−1.04, 0.71] |
| RSA (recovery-prep) | 0.68 (0.55) [0.51] | 0.55 (0.86) [0.30] | −0.47 [0.98] | 0.17 [−0.63, 0.98] |
| RSA (recovery-baseline) | −0.10 (0.39) [−0.23] | −0.08 (0.49) [−0.10] | −0.09 [0.23] | 0.03 [−0.80, 0.74] |
Note. LSC–low self-compassion group, HSC–high self-compassion group; TSST-Trier Social Stress Test; ΔSBP-change in systolic blood pressure; ΔDBP-change in diastolic blood pressure; ΔHR-change in heart rate; AUCi-area under the curve with respect to increase; RSA-Respiratory sinus arrhythmia (measure of heart rate variability); prep-preparatory phase of the Trier; . Heart rate variables were square-root transformed and cortisol AUCi and the diastolic blood pressure with the speech task were log-transformed to achieve normality prior to calculation of the t statistic and Hedge’s g. Where variable distributions were non-normal, Wilcoxon rank-sum tests were used to confirm results. Effect sizes for the RSA variables are reported with bootstrapped confidence intervals.
Figure 1.
Change from baseline in systolic blood pressure in response to the Trier Social Stress Test during preparation, speech, math, and recovery phases in a sample of male and female adolescents age 13–18 (n=28). Error bars correspond to a standard error above and below the mean.
Results of the regression analyses indicated that self-compassion was statistically significantly associated with other pre-intervention self-report measures, again in the expected directions both in unadjusted models and models adjusted for gender and race (Table 5). For example, for every one-point increase on the self-compassion scale, perceived stress decreased by 7.49 points. Conversely, pre-intervention self-compassion was not statistically significantly associated with a change in self-reported anxiety during the TSST. In addition, self-compassion, as a continuous (log-transformed) variable was not statistically significantly associated with any of the physiologic variables tested during the TSST (Table 6). Interestingly, the change in systolic blood pressure with the speech task was 3.36 mmHg lower (SE = 3.50) for each one point increase in self-compassion, controlling for the differences in race and gender. Similarly, with the math task, with each one point increase in self-compassion, the change in heart rate was 6.15 beats per minute less (SE = 4.98).
Table 5.
Association of self-compassion with self-reported wellbeing in linear regression models in a sample of male and female adolescents age 13–18 (n = 28)
|
|
||||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted for race and gender | |||||
|
|
|
|||||
| B (SE) | Beta | p-value* | B (SE) | Beta | p-value* | |
|
|
|
|||||
| Baseline Anxiety | −5.58 (2.04) | −0.4689 | 0.012 | −4.94 (2.34) | −0.4191 | 0.05 |
| Perceived Stress | −6.74 (1.79) | −0.5710 | 0.002 | −7.49 (1.79) | −0.6629 | <0.001 |
| Negative Affect | −6.28(1.88) | −0.5317 | 0.004 | −6.61 (2.17) | −0.5697 | 0.008 |
| Positive Affect | 4.04 (2.10) | 0.3313 | 0.08 | 6.16 (2.14) | 0.5483 | 0.008 |
| Life Satisfaction | 0.50 (0.15) | 0.5299 | 0.004 | 0.58 (0.14) | 0.6402 | 0.001 |
| Δ Anxiety in TSST | −2.56 (3.56) | −0.1612 | 0.41 | −0.68 (4.0) | −0.0521 | 0.71 |
Note. TSST—Trier Social Stress Test; Because of non-normal distributions, p-values and betas are reported for the log-transformed self-compassion score, and the square-root transformation of baseline anxiety. Adjusted models included terms for gender (male = 1, female = 0) and race (white = 1, other = 0).
Table 6.
Association of self-compassion with physiological stress reactivity to TSST in linear regression models (n = 28)
| Unadjusted | Controlled for race and gender | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| B (SE) | Beta* | p-value* | B (SE) | Beta* | p-value* | |
| ΔSBP (prep) | −2.54 (2.44) | −0.2237 | 0.25 | −1.35 (2.76) | −0.1319 | 0.56 |
| ΔSBP (speech) | −4.02 (3.05) | −0.2864 | 0.14 | −3.36 (3.50) | −0.2532 | 0.26 |
| ΔSBP (math) | −3.20 (3.15) | −0.2300 | 0.24 | −1.90 (3.60) | −0.1537 | 0.50 |
| ΔDBP (prep) | −0.38 (1.65) | −0.0750 | 0.71 | 0.11 (1.90) | −0.1319 | 0.56 |
| ΔDBP (speech) | −0.03 (1.64) | −0.0425 | 0.83 | 0.46 (1.87) | 0.0248 | 0.91 |
| ΔDBP (math) | −0.88 (1.74) | −0.1107 | 0.58 | −0.88 (2.02) | −0.1151 | 0.62 |
| ΔHR (prep) | −3.53 (3.77) | −0.1232 | 0.54 | −1.46 (4.22) | −0.0851 | 0.72 |
| ΔHR (speech) | −3.60 (4.54) | −0.1470 | 0.45 | −3.70 (5.24) | −0.1489 | 0.52 |
| ΔHR (math) | −6.36 (4.41) | −0.2411 | 0.22 | −6.15 (4.98) | −0.2276 | 0.31 |
| Cortisol (AUCi) | −0.667 (0.52) | −0.0918 | 0.61 | −0.48 (0.60) | −0.0208 | 0.93 |
| RSA (prep- baseline) | 0.035 (0.26) | 0.0119 | 0.95 | 0.009 (0.26) | 0.0026 | 0.99 |
| RSA (recovery- prep) | −0.017 (0.23) | −0.0046 | 0.94 | −0.001 (0.24) | 0.0010 | 1.0 |
| RSA (recovery- baseline) | 0.018 (0.14) | 0.0150 | 0.94 | 0.008 (0.15) | 0.0065 | 0.98 |
Note. TSST-Trier Social Stress Test; ΔSBP-change in systolic blood pressure; ΔDBP-change in diastolic blood pressure; ΔHR—change in heart rate; AUCi-area under the curve with respect to increase; RSA- Respiratory sinus arrhythmia (measure of heart rate variability); prep-preparatory phase of the Trier. Because of non-normal distributions and small sample size, p-values and betas (standardized) are reported for the log-transformed self-compassion score, cortisol, and the diastolic blood pressure change score for the speech task as well as square-root transformations for the change in heart variables. The heart rate variability vairables functioned best without transformation. Adjusted models included terms for gender (male = 1, female = 0) and race (white = 1, other = 0).
Discussion
Previous evidence has demonstrated support for the buffering effect of self-compassion on stress in adult samples. The current study investigated that effect in adolescents through assessing self-reported indicators of wellbeing and physiological responses to a lab social stress test. First, results indicated that when the sample was split at the median (low and high self-compassion), all six males were in the HSC group. This is consistent with other findings in studies with adolescents which reported males to be more self-compassionate than females (Bluth & Blanton, 2014a, 2014b). Second, we found partial support for the hypotheses that high self-compassion is related to a) greater emotional wellbeing and b) lower physiological stress response. Namely, those higher in self-compassion self-reported less anxiety, stress, and negative affect, and greater life satisfaction and positive affect. This was confirmed with the regression analyses.
In relation to cardiovascular reactivity to the lab stressor, when analyzed using a median split, those in HSC had lower SBP reactivity compared to those in LSC during the majority of time points and, in regression analyses, increasing self-compassion scores were associated with decreases in SBP responses to stress. Although no meaningful difference in change of HR was evidenced between the HSC and LSC in the speech and math tasks, this may be because of a ceiling effect, as both those high and low in self-compassion evidenced a brisk increase in HR with these tasks. Similarly, regression analyses failed to show any statistically significant changes in HR with increasing self-compassion scores, although the changes seen were in the expected direction. For example, heart rate increases were lower for those with higher self-compassion scores. Adolescents in HSC also had a lower overall cortisol output during the TSST, indicative of a lower physiological stress response, although these differences were not considered meaningful according to Hedges g. It should be noted that males have a stronger cardiovascular and HPA axis response to stress than females (Kajantie & Phillips, 2006) and all males were in the HSC group. Therefore, it is possible that some of the lack of difference evidenced between HSC and LSC groups in cardiovascular reactivity is because of the higher expected reactivity of the HSC group due to the presence of all males in this group. Self-compassion appears to buffer the SBP response in this HSC group but not the other physiologic measures. It should also be noted that the TSST tasks in which the greatest difference between groups is observed are those that we would expect to be less stressful (e.g., the preparation period). It may be that self-compassion is able to buffer the lower stress of the preparation task but not the higher stress of the speech and math tasks.
There was no difference in HRV between the low and high self-compassionate groups. A possible explanation for the lack of difference in HRV between the low and high self-compassionate groups is that those who have lower self-compassion exercise a different coping strategy in response to a stressor compared to those who are more self-compassionate; those with lower self-compassion respond by “toughening up” and exerting greater self-regulation, thereby raising their HRV (Segerstron & Nes, 2007). In contrast, those with higher self-compassion respond by self-soothing, which does not raise HRV. However, in all, small changes were noted in regression analyses with increasing self-compassion scores, consistent with the median split analysis findings. Clearly, further research with a larger sample is necessary to determine if self-compassion buffers a physiologic stress response and whether these posited explanations hold true.
These findings support our first hypothesis that self-compassion is associated with self-reported emotional wellbeing, and offer some indication for our second hypothesis that self-compassion is also related to reduced physiological stress reactivity to a social stressor. Thus, similar to adults, self-compassion may serve a protective function for adolescents experiencing stress. Further, because self-compassion associations with dimensions of emotional wellbeing differed relative to level of self-compassion, these protective factors may extend outside the laboratory settings into adolescents’ daily lives where stressful events which are out of adolescents’ control are frequently encountered. As explained by Dickerson and Kemeny’s social self-preservation theory (Dickerson & Kemeny, 2004), being exposed to an uncontrollable event such as the TSST (or not being invited to a party, for example) threatens one’s sense of social status, thereby activating the physiological stress response. It may be that individuals who are higher in self-compassion may not be as threatened by this social stressor as those who are lower in self-compassion. It may also be that these self-compassionate adolescents are able to offer support to themselves or soothe themselves at stressful moments, thereby protecting themselves from the negative effect of the stressor. In essence, these adolescents may have learned to “make friends with themselves.”
Viewing self-compassion as social support turned inward is further supported by the literature on social support and physiological stress reactivity. In laboratory stress research, social support has been shown to have buffering effects on both hypothalamic-pituitary-adrenal (HPA) axis and cardiovascular reactivity (Ditzen & Heinrichs, 2014). In general, having a supportive person present, particularly a person who was well-known to the individual, attenuated the physiological stress response following a stressful task. Further, the quality of the interaction strengthened the effect; positive or neutral behavior offered by the supportive person had the greatest effect on reducing BP and HR increases during stress. In studies which utilized the TSST, those who reported having high social support had more rapid cortisol recovery than those who did not. Thus, it is not surprising that those with high self-compassion, or those who offer themselves regular and positive “social support”, may have lower stress reactivity than those with low self-compassion.
These findings suggest that developing ways to strengthen self-compassion in adolescents may be advantageous in guarding against negative mood states which can then result in lifelong psychological and cognitive struggles (Lupien, McEwan, Gunnar, & Heim, 2009; Pine, Cohen, & Brook, 1999). As evidence-based forms of stress reduction for adolescents are often limited to cognitive-based therapy which may have limited efficacy over the long term (Curry, 2014) and active coping measures which have limited effectiveness on psychological functioning particularly with uncontrollable interpersonal stressors (Clarke, 2006), strengthening one’s ability to be self-compassionate may offer adolescents an additional personal resource which they can access when needed. The Mindful Self-Compassion program for adults, created and piloted by Neff and Germer (2013), has demonstrated that self-compassion can be developed and maintained. Results over the 8-week course indicated increases in self-compassion which predicted increases in emotional wellbeing, and were maintained a year later. A parallel program which would be developmentally appropriate for adolescents may produce similar results, thereby promoting healthier emotional states and setting the stage for a more salubrious lifelong trajectory. Modifications of the program to meet the developmental needs of adolescents would be necessary; relative to the adult program, a program for adolescents would need to have shorter sessions, include more hands-on activities, and incorporate a session on the developing adolescent brain.
This study has notable strengths. It is the first study to examine self-compassion as a protective factor in adolescents, and the only one that has done so by assessing physiological stress markers. Also, there are several limitations. First, the sample was small, limiting its statistical power. A larger sample would provide more definitive results, particularly in relation to the physiological stress markers. Second, the median split resulted in a gender imbalance in the two groups (with all males in the HSC group). Although potentially problematic in relation to results in self-report measures, this strengthens the findings linking high self-compassion to lower physiologic stress response, since males have been found to have a greater physiological response to stress. Also, the sample was mostly female (76%), white (62%), came from an area within a 50 mile radius, and were of high socioeconomic status, as indicated by parents’ education, limiting the ability to generalize findings to all adolescents. Replicating this study with a larger sample and greater diversity of parent education, gender, and race/ethnicity is suggested.
Implications for future research include exploring whether differences in self-compassion that may exist between genders or age (i.e., younger adolescents vs. older adolescents) are associated with a different physiological stress response or self-reported emotional wellbeing. Further, investigating whether demographic factors or parenting styles are associated with different levels of self-compassion may also be of interest. Finally, as self-compassion has been demonstrated to be a mutable trait and predictive of emotional wellbeing in adults as evidenced by findings from the adult Mindful Self-compassion randomized controlled trial (Neff & Germer, 2013), there is potential that a similar program for adolescents may offer tools to strengthen adolescents’ emotional wellbeing. Such a program may be instrumental in helping adolescents navigate this often challenging developmental stage and establish a positive lifelong emotional health and behavioral trajectory. The development of such a program and subsequent clinical trials would determine the merit of such a program for adolescents.
Contributor Information
Karen Bluth, University of North Carolina-Chapel Hill, Chapel Hill, NC.
Patricia N. E. Roberson, University of Tennessee-Knoxville, Knoxville, TN
Susan A. Gaylord, University of North Carolina-Chapel Hill, Chapel Hill, NC
Keturah R. Faurot, University of North Carolina-Chapel Hill, Chapel Hill, NC
Karen M. Grewen, University of North Carolina-Chapel Hill, Chapel Hill, NC
Samantha Arzon, University of North Carolina-Chapel Hill, Chapel Hill, NC.
Susan S. Girdler, University of North Carolina-Chapel Hill, Chapel Hill, NC
References
- Arch JJ, Brown KW, Dean DJ, Landy LN, Brown KD, Laudenslager ML. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology. 2014;42:49–58. doi: 10.1016/j.psyneuen.2013.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes LLB, Harp D, Jung WS. Reliability generalizations of scores on the Spielberger state-trait anxiety inventory. Educational and Psychological Measurement. 2002;62:603–615. [Google Scholar]
- Barry CT, Loflin DC, Doucette H. Adolescent self-compassion: Associations with narcissism, self-esteem, aggression, and internalizing symptoms in at-risk males. Personality and Individual Differences. 2015;77:118–123. [Google Scholar]
- Blakemore J, Berenbaum S, Liben L. Gender development. Clifton, NJ: Psychology Press; 2009. [Google Scholar]
- Bluth K, Blanton P. The influence of self-compassion on emotional well-being among early and older adolescent males and females. Journal of Positive Psychology. 2014a doi: 10.1080/17439760.2014.936967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluth K, Blanton P. Mindfulness and self-compassion: Exploring pathways of adolescent wellbeing. Journal of Child and Family Studies. 2014b;23:1298–1309. doi: 10.1007/s10826-013-9830-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgens JPT, Rothstein HR. Introduction to meta-analysis. Chichester, U.K: Wiley; 2009. [Google Scholar]
- Breines JG, Thoma MV, Gianferante D, Hanlin L, Chen X, Rohleder N. Self-compassion as a predictor of interleukin-6 response to acute psychosocial stress. Brain Behavior and Immunity. 2014;37:109–114. doi: 10.1016/j.bbi.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breines JG, McInnis CM, Kuras YI, Thoma MV, Gianferante D, Hanlin L, Chen X, Rohleder N. Self-compassionate young adults show lower salivary alpha-amylase responses to repeated psychosocial stress. Self and Identity. 2015 doi: 10.1080/15298868.2015.1005659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell TS, Labelle LE, Bacon SL, Faris P, Carlson LE. Impact of mindfulness-based stress reduction on attention, rumination, and resting blood pressure in women with cancer: A wait-listed controlled study. Journal of Behavioral Medicine. 2012;35:262–271. doi: 10.1007/s10865-011-9357-1. [DOI] [PubMed] [Google Scholar]
- Clarke AT. Coping with interpersonal stress and psychosocial health among children and adolescents: A meta-analysis. Journal of Youth and Adolescence. 2006;35(1):10–23. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Compas BE. Processes of risk and resilience during adolescence: Linking contexts and individuals. In: Lerner R, Steinberg L, editors. Handbook of adolescent psychology. 2. New York: Wiley; 2004. [Google Scholar]
- Cresswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosomatic Medicine. 2007;69:560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Curry JF. Future directions in research on psychotherapy for adolescent depression. Journal of Clinical Child & Adolescent Psychology. 2014;43(3):510–526. doi: 10.1080/15374416.2014.904233. [DOI] [PubMed] [Google Scholar]
- Crocker PRE. A confirmatory factor analysis of the positive affect negative affect schedule (PANAS) with a youth sport sample. Journal of Sport and Exercise Psychology. 1997;19:91–97. [Google Scholar]
- Cumming G. The new statistics: Why and how. Psychological Science. 2014;25:7–29. doi: 10.1177/0956797613504966. [DOI] [PubMed] [Google Scholar]
- D’Agostino RB, Belanger AJ, D’Agostino RB., Jr A suggestion for using powerful and informative tests of normality. American Statistician. 1990;44:316–321. [Google Scholar]
- Dew T, Huebner ES. Adolescents perceived quality of life: An exploratory investigation. Journal of School Psychology. 1994;32:185–199. [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130:355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Ditzen B, Heinrichs M. Psychobiology of social support: the social dimension of stress buffering. Restor Neurol Neurosci. 2014;32:149–162. doi: 10.3233/RNN-139008. [DOI] [PubMed] [Google Scholar]
- Gilman R, Huebner ES. Children’s reports of their life satisfaction: Convergence across raters, time, and response formats. School Psychology International. 1997;18:229–243. [Google Scholar]
- Hains AA, Szyjakowski M. A cognitive stress-reduction intervention program for adolescents. Journal of Counseling Psychology. 1990;37(1):79. [Google Scholar]
- Harkness KL, Stewart JG, Wynne-Edwards KE. Cortisol reactivity to social stress in adolescents: role of depression severity and child maltreatment. Psychoneuroendocrinology. 2011;36(2):173–181. doi: 10.1016/j.psyneuen.2010.07.006. [DOI] [PubMed] [Google Scholar]
- Hauser S, Bowlds M. Stress, coping and adaptation. In: Feldman S, Elliott G, editors. At the threshold: The developing adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 388–413. [Google Scholar]
- Huebner ES. Initial Development of the Student’s Life Satisfaction Scale. School Psychology International. 1991;12:231–240. doi: 10.1177/0143034391123010. [DOI] [Google Scholar]
- Huebner ES, Dew T. Preliminary validation of thepositive and negative affect schedule with adolescents. Journal of Psychoeducational Assessment. 1995;13(3):286–293. doi: 10.1177/073428299501300307. [DOI] [Google Scholar]
- Johnson D, Greenberg MT. Parenting and early adolescence internalizing: The importance of teasing apart anxiety and depressive symptoms. Journal of Early Adolescence. 2013;33:201–226. doi: 10.1177/0272431611435261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31:151–178. doi: 10.1016/j.psyneuen.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, Hellhammer DH. The ‘Trier Social Stress Test’ -- a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Strasburger CJ, Langkrar J. Attenuated cortisol response to psychological stress but not to CRH or ergometry in young habitual smokers. Pharmacol Biochem Behav. 1993;44:527–531. doi: 10.1016/0091-3057(93)90162-m. [DOI] [PubMed] [Google Scholar]
- Kline RB. Beyond significance testing: Statistics reform in the behavioral sciences. Washington, D. C: APA Books; 2013. [Google Scholar]
- Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. 2007;92(5):887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- LeBlanc JC, Almudevar A, Brooks SJ, Kutcher S. Screening for adolescent depression: comparison of the Kutcher Adolescent Depression Scale with the Beck depression inventory. Journal of Child and Adolescent Psychopharmacologyl. 2002;12:113–126. doi: 10.1089/104454602760219153. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, McEwan BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience. 2009;10:434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- MacBeth A, Gumley A. Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review. 2012;32:545–552. doi: 10.1016/j.cpr.2012.06.003. [DOI] [PubMed] [Google Scholar]
- Marshall SL, Parker PD, Ciarrochi J, Sahdra B, Jackson CJ, Heaven PC. Self-compassion protects against the negative effects of low self-esteem: A longitudinal study in a large adolescent sample. Personality and Individual Differences. 2015;74:116–121. [Google Scholar]
- Martin R, Kazarian S, Breiter H. Perceived stress, life events, dysfunctional attitudes, and depression in adolescent psychiatric inpatients. Journal of Psychopathology and Behavioral Assessment. 1995;17:81–95. [Google Scholar]
- Melvin GA, Molloy GN. Some psychometric properties of the positive and negative affect schedule among Australian youth. Psychological Reports. 2000;86:1209–1212. doi: 10.2466/pr0.2000.86.3c.1209. [DOI] [PubMed] [Google Scholar]
- Neff K, Germer C. A pilot study and randomized controlled trial of the mindful self-compassion program. Journal of Clinical Psychology. 2012;1:1–17. doi: 10.1002/jclp.21923. [DOI] [PubMed] [Google Scholar]
- Neff KD. The development and validation of a scale to measure self-compassion. Self and Identity. 2003;2:223–250. doi: 10.1080/15298860390209035. [DOI] [Google Scholar]
- Neff KD, Kirkpatrick K, Rude S. Self-compassion and its link to adaptive psychological functioning. Journal of Research in Personality. 2007;41:139–154. [Google Scholar]
- Neff KD, Kirkpatrick KL, Rude SS. Self-compassion and adaptive psychological functioning. Journal of Research in Personality. 2007;41:139–154. doi: 10.1016/j.jrp.2006.03.004. [DOI] [Google Scholar]
- Neff KD, McGehee P. Self-compassion and psychological resilience among adolescents and young adults. Self and Identity. 2010;9:225–240. doi: 10.1080/15298860902979307. [DOI] [Google Scholar]
- Pace TWW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, Issa MJ, Raison CL. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendorinology. 2009;34:87–88. doi: 10.1016/j.psyneuen.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace TWW, Negi LT, Sivilli TI, Issa MJ, Cole SP, Adame DD, Raison CL. Innate immune, neuroendocrine, to psychosocial stress do not predict subsequent compassion meditation practice time. Psychoneuroendorinology. 2010;35:310–315. doi: 10.1016/j.psyneuen.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peckins MK, Dockray S, Eckenrode JL, Heaton J, Susman EJ. The longitudinal impact of exposure to violence on cortisol reactivity in adolescents. Journal of Adolescent Health. 2012;51(4):366–372. doi: 10.1016/j.jadohealth.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pine DS, Cohen E, Brook J. Adolescent depressive symptoms as predictors of adult depression: Moodiness or mood disorder? American Journal of Psychiatry. 1999;156:133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- Porges SW. US Patent No. 4,510,944 Method and apparatus for evaluating rhythmic oscillations in a periodic physiological response system. 1985
- Pruessner M, Hellhammer DH, Pruessner JC, Lupien SJ. Self-reported depressive symptoms and stress levels in healthy young men: associations with the cortisol response to awakening. Psychosomatic Medicine. 2003;65:92–99. doi: 10.1097/01.psy.0000040950.22044.10. [DOI] [PubMed] [Google Scholar]
- Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension. 2001;37:1199–1208. doi: 10.1161/01.hyp.37.5.1199. [DOI] [PubMed] [Google Scholar]
- Rockliff H, Gilbert P, McEwan K, Lightman S, Glover D. A pilot exploration of heart rate variability and salivary cortisol responses to compassion-focused imagery. Clinical Neuropsychiatry. 2008;5:132–139. [Google Scholar]
- Segerstron SC, Nes LS. Heart rate variability reflects self-regulatory strength, effort, and fatigue. Psychological Science. 2007;18:275–281. doi: 10.1111/j.1467-9280.2007.01888.x. [DOI] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, Inc; 1970. [Google Scholar]
- Susman E, Dorn L. Puberty: Its role in development. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. 3. New York: Wiley; 2009. [Google Scholar]
- Tukey JW. Exploratory Data Analysis. Reading, MA: Addison–Wesley; 1977. [Google Scholar]
- von Kanel R, Kudielkac BM, Preckelb D, Hanebuthb D, Fischerb JE. Delayed response and lack of habituation in plasma interleukin-6 to acute mental stress in men. Brain Behavior Immunity. 2006;20:40–48. doi: 10.1016/j.bbi.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Watson T, Clark L, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Zeller M, Yuval K, Nitzan-Assayag Y, Bernstein A. Self-compassion in recovery following potentially traumatic stress: Longitudinal study of at-risk youth. Journal of Abnormal Child Psychiatry. 2014:1–9. doi: 10.1007/s10802-014-9937-y. [DOI] [PubMed] [Google Scholar]