Abstract
Perivascular spaces are an emerging marker of small vessel disease. Perivascular spaces in the centrum semiovale have been associated with cerebral amyloid angiopathy. However, a direct topographical relationship between dilated perivascular spaces and cerebral amyloid angiopathy severity has not been established. We examined this association using post-mortem magnetic resonance imaging in five cases with evidence of cerebral amyloid angiopathy pathology. Juxtacortical perivascular spaces dilation was evaluated on T2 images and related to cerebral amyloid angiopathy severity in overlying cortical areas on 34 tissue sections stained for Amyloid β. Degree of perivascular spaces dilation was significantly associated with cerebral amyloid angiopathy severity (odds ratio = 3.3, 95% confidence interval 1.3–7.9, p = 0.011). Thus, dilated juxtacortical perivascular spaces are a promising neuroimaging marker of cerebral amyloid angiopathy severity.
Keywords: 7 T magnetic resonance imaging, amyloid angiopathy, histology, microbleeds, perivascular spaces
Introduction
Perivascular spaces (PVS) are increasingly recognized as markers of cerebral small vessel disease in aging and dementia.1 PVS are spaces filled with interstitial fluid (ISF) surrounding small penetrating vessels. In magnetic resonance imaging (MRI), PVS have signal intensity similar to cerebrospinal fluid and follow the typical course of a vessel. Accumulating evidence suggests that PVS are involved in drainage of ISF and solutes from the brain.2,3 In cerebral amyloid angiopathy (CAA), it has been suggested that dilation of PVS and failure of drainage of ISF may result from deposition of Amyloid β (Aβ) in cortical and leptomeningeal arteries.4 Previous in vivo MRI studies have shown an association between PVS in the white matter at the level of the centrum semiovale and lobar (micro)hemorrhages, markers of CAA.5,6 Moreover, a recent combined positron emission tomography (PET)–MRI study suggested an association between whole cortex amyloid burden and PVS in the centrum semiovale in both patients with probable CAA and healthy elderly.7 However, a direct topographical association of degree of PVS dilation with degree of CAA severity has not been established.
This study investigates the association of degree of juxtacortical PVS dilation on post-mortem 7 T MRI with histopathological CAA score in the overlying cortex. We hypothesized that increasing dilation of PVS is accompanied by increasing CAA severity in the overlying cortical vessels, thus pointing toward an etiological link between the two.
Methods
Cases
From a database of autopsy cases with Alzheimer pathology, five cases with CAA were included. None of the cases had an intracerebral hemorrhage (ICH). The cases were scanned within 2 years after autopsy at the University Medical Center Utrecht (UMCU), the Netherlands. From each case, at least three formalin-fixed 10-mm-thick coronal brain slabs were selected for imaging, taken from the frontal, temporo-parietal, and occipital lobes. Slabs submerged in 10% formalin were placed in a purpose-built Perspex container. The use of these brain specimens was in accordance with local regulations and approved by the UMCU medical ethics committee. Informed consent was obtained prior to autopsy, according to local (UMCU) ethical guidelines.
MRI
Scans were acquired on a whole-body 7 T magnetic resonance (MR) system (Philips Healthcare, Cleveland, OH, USA) with a 32-channel transmit/receive head coil (Nova Medical, Wilmington, MA, USA). The protocol included, among other sequences, a 3D T2-weighted image (acquired isotropic resolution = 400 × 400 × 400 µm3, TR = 3500 ms, TE = 164 ms, scan duration = 1 hr 52 min).
Sampling
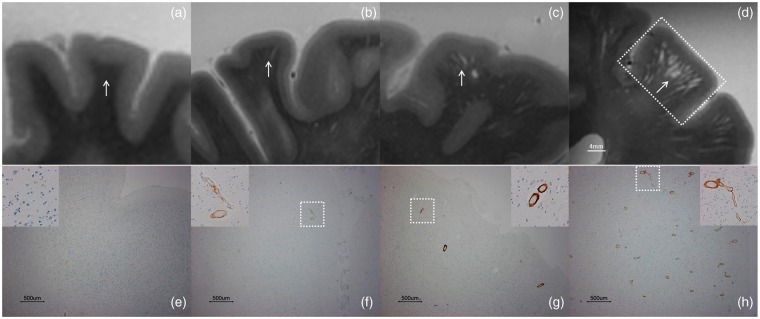
Dilation of juxtacortical PVS was evaluated in each case on the post-mortem T2-weighted image by one rater. First, all scans were inspected to determine the range of degree of juxtacortical PVS dilation in this dataset. Next, a 4-point qualitative ordinal scale of PVS dilation and number within a given juxtacortical area was devised, capturing the observed severity range in this dataset; no MR-visible PVS, some PVS, several enlarged PVS, many severely enlarged PVS. Rating according to this scale was supported by reference templates (Figure 1(a) to (d); additional examples are provided in Supplemental Figure 1). Per case, samples were taken from at least two areas with the highest and two areas with the lowest score, and when present, intermediate scores. Selected samples, including the overlying cortex, were subjected to histopathological evaluation (Figure 1). Areas showing cortical vascular pathology (microinfarcts or microbleeds) on MRI were not considered for sampling. Standardized H&E and Aβ staining was performed on 4-µm adjacent sections. Congo Red staining was performed on 8-µm sections, adjacent to the H&E and Aβ sections.
Figure 1.
PVS on post-mortem T2-weighted MRI and CAA evaluation. Evaluation of PVS dilation (arrows) was based on a 4-point scale: no MR-visible PVS (a), some PVS (b), several enlarged PVS (c), many severely enlarged PVS (d). The square in (d) represents the area sampled for histopathological evaluation, containing the overlying cortex to assess CAA score. Evaluation of cortical CAA score was based on a 4-point scale as developed by Love et al.7; absent (e), scant Aβ deposition (f), some circumferential Aβ (g), and widespread circumferential Aβ (h).
PVS: perivascular spaces; MRI: magnetic resonance imaging; CAA: cerebral amyloid angiopathy; MR: magnetic resonance; Aβ: Amyloid β.
Histopathology
CAA was evaluated on Aβ sections following previously reported guidelines.8 The thicker Congo Red sections were consulted in case of uncertainty. One rater assessed all sections, followed by a second rating and a consensus meeting with an expert neuropathologist, blinded to MRI results and research question. Cortical CAA (i.e. accumulation of Aβ in vessel walls) was scored using a 4-point scale; absent, scant Aβ deposition, some circumferential Aβ, widespread circumferential Aβ (Figure 1). Meningeal CAA was not scored due to the absence of leptomeningeal vessels in the majority of cases. In addition, as recommended in the literature, we assessed the degree of CAA-related vasculopathy (e.g. double-barreling, old hemorrhages, fibrinoid necrosis) separately, on H&E sections on a 3-point scale; absent, occasional vessel, many vessels.8 Parenchymal Aβ plaques were scored on Aβ sections as absent or present.
Statistical analysis
Inter-rater reliability was assessed with Cohen’s kappa. The relation between dilated PVS and cortical CAA score was estimated by Spearman’s rank correlation with inference based on a mixed-model ordinal logistic regression with a fixed effect of PVS score and random case-specific intercepts to account for covariance among repeated samples from the same case. The association between dilated PVS (dichotomized to no MR-visible PVS and some PVS vs. several enlarged PVS and many severely enlarged PVS) and Aβ plaques (present vs. absent) and vasculopathy (absent vs. occasional or many vessels) were assessed with equivalent mixed-model binary logistic regression models. Analyses were performed in SAS (version 9.4, SAS Institute, Cary, NC, USA).
Results
Mean age of the five patients included in this study was 75.6 ± 6.5 years, four were female. A total of 34 tissue samples were taken (4 to 8 per case) and subjected to histopathological evaluation. Inter-rater reliability for the assessment of cortical CAA was good (kappa = 0.72). Demographic details and pathologic findings for all five cases are shown in Supplemental Table I.
In a given region, more severe PVS dilation was significantly associated with higher cortical CAA score (Figure 2; Spearman’s rho = 0.63; cumulative odds ratio (OR) = 3.3, 95% confidence interval (CI) = 1.3–7.9, p = 0.011). PVS dilation was not significantly related to presence of Aβ plaques (OR = 1.7, 95% CI = 0.15–18.7, p = 0.65), or CAA-related vasculopathy (OR = 3.1, 95% CI = 0.53–17.7, p = 0.20), although strong associations could not be excluded given our small sample size.
Figure 2.
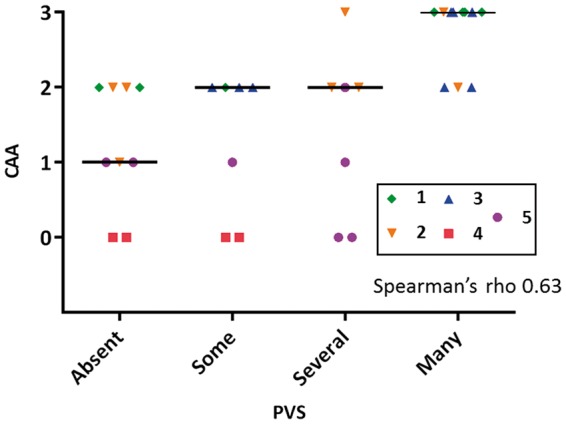
PVS dilation and association with CAA score. Each symbol represents an individual case with multiple samples per case (n = 34 samples in total). Horizontal lines represent median scores. CAA score: 0 = absent, 1 = scant Aβ deposition, 2 = some circumferential Aβ, 3 = widespread circumferential Aβ. In a given region, more severe PVS dilation was significantly associated with higher CAA score (Spearman’s rho = 0.63; cumulative OR = 3.3, 95% CI = 1.3–7.9, p = 0.011).
PVS: perivascular spaces; CAA: cerebral amyloid angiopathy; Aβ: Amyloid β; OR: odds ratio; CI: confidence interval.
Discussion
In this exploratory post-mortem MRI study of cases with known presence of CAA and Alzheimer pathology, we found a positive association between the number and degree of dilation of MR-visible juxtacortical PVS in a given region and higher cortical CAA score in the same area.
Previous cross-sectional in vivo MRI studies have suggested an association between PVS and CAA markers.5,6 In a retrospective multicentre cohort study of 121 patients with ICH, patients with lobar ICH had a higher prevalence of severely dilated PVS in the centrum semiovale compared with patients with non-lobar ICH.5 Further evidence for a link between CAA and dilated PVS was provided by a study on 89 memory clinic subjects, in which subjects with a high degree of dilated white matter PVS had higher counts of lobar microbleeds, a potential marker of CAA pathology. In contrast, a high degree of dilated PVS in the basal ganglia was only associated with hypertension.6 An autopsy study showed that the frequency and severity of PVS dilation in the white matter were significantly greater in Alzheimer cases than controls. Moreover, PVS dilation correlated not only with CAA severity but also with total Aβ load in the cortex and ApoE epsilon 4 genotype.4
The present findings show that there is a direct topographical association of PVS dilation with higher cortical CAA score. Interestingly, this association was not found for Aβ plaques or CAA-related vasculopathy. This strengthens the hypothesis that impaired ISF drainage may directly result from deposition of Aβ in cortical (and leptomeningeal) vessels, causing retrograde dilation of PVS in the underlying white matter. Since PVS dilation is a quantifiable MRI marker, it is conceivable that this measure could be used to estimate regional CAA severity in vivo. For the purpose of this study, we used a 4-point scale for PVS dilation, representing the actual range of PVS abnormalities in this dataset, which allowed distinguishing differences in PVS degree in juxtacortical areas. Because this scale was devised based on the PVS abnormalities observed within this dataset, its external validity will need to be determined. It should be acknowledged that the spatial resolution of current 3 T in vivo MRI protocols might not be able to detect these differences in vivo. The translation of our findings to conventional MRI was beyond the scope of this study and should be a topic of further investigation. Also, it would be interesting to investigate the histopathological nature of MR observed PVS in more detail.
A limitation of this study is the small sample size. Although only five cases were available for this study, we examined (four to eight) samples from each case (n = 34 in total), recognizing that CAA is a patchy and segmented disease, often with substantial regional variations in presence and severity within a given individual.9 Hence, we were able to compare different degrees of PVS dilation with CAA severity in multiple areas within cases. Although we found that PVS dilation was significantly associated with CAA score within cases, we observed substantial variation in CAA severity across cases. It may be that degree of PVS dilation is only a predictor of relative CAA severity and cannot be reliably used to compare severity among individuals. Further studies are needed to better address the question as to whether whole brain PVS correlates with global CAA severity, conceivably using PiB-PET imaging to assess this relationship.7 Moreover, assumptions of normality and applicability of asymptotic approximations cannot be evaluated in such a small sample. Finally, because our study specifically examined CAA cases without ICH, our results may not be generalizable to all forms of CAA.10
Conclusions
Our findings suggest that degree of PVS dilation is a marker of CAA severity. Whether these findings can be used to diagnose or track progression of CAA needs confirmation in larger studies.
Supplementary Material
Acknowledgments
We acknowledge support from the Biostatistics Core of the Harvard NeuroDiscovery Center.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by grants from ZonMw (VIDI), The Netherlands Organization for Health Research and Development (91711384), and the Netherlands Heart Foundation (2010 T073), and NIH grants R01AG047975, R01AG026484, P50AG005134. Further funding supporting this research was received from the European Research Council under the European Union’s Seventh Framework Programme (FP7/2007-2013)/ERC grant agreement no. 337333.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors' contributions
Susanne J van Veluw was involved in the concept and design of the study, acquisition, analysis, and interpretation of the data, drafting, and revising of the manuscript. Geert Jan Biessels was involved in study supervision and obtaining funding, and in the concept and design of the study, interpretation of the data, and drafting and revising of the manuscript. Willem H Bouvy was involved in the concept and design of the study, interpretation of the data, and revising of the manuscript. Wim GM Spliet was involved in acquisition of the data and revising of the manuscript. Jaco JM Zwanenburg was involved in obtaining funding, in the acquisition of the data, and revising of the manuscript. Peter R Luijten was involved in study supervision and in revising of the manuscript. Eric A Macklin was involved in statistical analysis of the data and in revising of the manuscript. Annemieke JM Rozemuller was involved in acquisition of the data, interpretation of the data, and revising of the manuscript. M Edip Gurol was involved in revising of the manuscript. Steven M Greenberg was involved in study supervision, the concept and design of the study, interpretation of the data, and revising of the manuscript. Anand Viswanathan was involved in study supervision, the concept and design of the study, analysis and interpretation of the data, and revising of the manuscript. Sergi Martinez-Ramirez was involved in the concept and design of the study, analysis and interpretation of the data, and drafting and revising of the manuscript.
Supplementary material
Supplementary material for this paper can be found at http://jcbfm.sagepub.com/content/by/supplemental-data
References
- 1.Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 2013; 12: 822–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carare RO, Bernardes-Silva M, Newman TA, et al. Solutes, but not cells, drain from the brain parenchyma along basement membranes of capillaries and arteries: significance for cerebral amyloid angiopathy and neuroimmunology. Neuropathol Appl Neurobiol 2008; 34: 131–144. [DOI] [PubMed] [Google Scholar]
- 3.Weller RO, Boche D, Nicoll JA. Microvasculature changes and cerebral amyloid angiopathy in Alzheimer's disease and their potential impact on therapy. Acta Neuropathol 2009; 118: 87–102. [DOI] [PubMed] [Google Scholar]
- 4.Roher AE, Kuo YM, Esh C, et al. Cortical and leptomeningeal cerebrovascular amyloid and white matter pathology in Alzheimer’s disease. Mol Med 2003; 9: 112–122. [PMC free article] [PubMed] [Google Scholar]
- 5.Charidimou A, Meegahage R, Fox Z, et al. Enlarged perivascular spaces as a marker of underlying arteriopathy in intracerebral haemorrhage: a multicentre MRI cohort study. J Neurol Neurosurg Psychiatry 2013; 84: 624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martinez-Ramirez S, Pontes-Neto OM, Dumas AP, et al. Topography of dilated perivascular spaces in subjects from a memory clinic cohort. Neurology 2013; 80: 1551–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charidimou A, Hong YT, Jäger HR, et al. White matter perivascular spaces on magnetic resonance imaging: marker of cerebrovascular amyloid burden? Stroke 2015; 46: 1707–1709. [DOI] [PubMed] [Google Scholar]
- 8.Love S, Chalmers K, Ince P, et al. Development, appraisal, validation and implementation of a consensus protocol for the assessment of cerebral amyloid angiopathy in post-mortem brain tissue. Am J Neurodegener Dis 2014; 3: 19–32. [PMC free article] [PubMed] [Google Scholar]
- 9.Vinters HV. Cerebral amyloid angiopathy. A critical review. Stroke 1987; 18: 311–324. [DOI] [PubMed] [Google Scholar]
- 10.Charidimou A, Martinez-Ramirez S, Shoamanesh A, et al. Cerebral amyloid angiopathy with and without hemorrhage: evidence of different disease phenotypes. Neurology 2015; 84: 1206–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.