Abstract
Objective
Child health is strongly influenced by social determinants. Little is known about the opinions of primary caregivers regarding the physicians’ role in addressing social needs. Our objective was to examine caregivers’ opinions about that role and any associations between those opinions, previous exposure to screening for needs by pediatric residents, and socioeconomic status (SES).
Methods
Cross-sectional survey study of caregivers of hospitalized children. The survey collected information on caregiver opinion regarding their ability to ask physicians for help with social needs, whether physicians know how to help with those needs, and whether physicians should ask about social needs. The chi square test was used to identify associations between caregiver opinions, prior screening by a resident at admission, and SES (determined by census tract median household income.)
Results
Surveys were completed by 143 caregivers (79% participation). Most respondents agreed that they could ask their physician for help (54.5%), that their physician knows how to help (64.3%), and that physicians should ask about social needs (71.3%). Previously screened caregivers had more favorable opinions about asking for help (76.2% vs. 45.5%, P<0.01), whether their physician knows how to help (81.0% vs. 57.4%, P=0.02), and physician screening for unmet needs (85.7% vs. 65.3%, P=0.03). There were no SES differences in opinion.
Conclusions
Caregivers have favorable opinions of the physician’s role in addressing the social determinants of health, especially after being screened. Physicians should be confident in the acceptability of screening families for social needs.
Keywords: social determinants of health, socioeconomic factors, vulnerable populations, health status disparities, poverty
INTRODUCTION
Socioeconomic status (SES) is one of the most powerful predictors of child health in the United States: as SES decreases, mortality and chronic conditions increase.1–3 The complex mechanisms through which SES influences child health include stress,4,5 social supports,6,7 and psychological factors (e.g., self-efficacy).8,9 Material deprivation is also a critical cause of SES-related disparities in child health within the United States. Material deprivation influences child health through pathways including food insecurity,10,11 inadequate health insurance and access to health care,3,12 homelessness and poor housing conditions.13,14 Moreover, the combination of multiple social needs has a cumulative effect on child health.15 Acknowledging the impact of SES on health and health care utilization,16 the Institute of Medicine recently recommended the routine collection of data related to patient SES and the National Quality Forum endorsed the use of SES in adjusting hospital quality measures.17,18
Previous studies have demonstrated that physicians overwhelmingly recognize the importance of unmet social needs and the connection between those needs and poor health.19–21 A recent survey conducted through the Robert Wood Johnson Foundation found that 85% of polled physicians believed that unmet social needs directly lead to worse health and that addressing a patient’s social needs is as important as addressing their medical needs.19 Despite recognition of these negative influences on health, however, physician screening for social needs is rare.20,22,23 Among pediatric residents, one study found that more than 90% residents believed it was important to address patient social needs, but fewer than 20% routinely screened for those needs.20 Additional studies reveal that, even when patients mentioned social factors critical to their care, physicians probed for further information only 51% of the time.24 As a result, physicians commit contextual errors in up to 78% of socially-complex cases.24 Examples of these contextual errors include failing to address the poor housing environment of a patient with asthma or prescribing an antibiotic that requires refrigeration to a homeless patient. In contrast, 70% of parents of pediatric patients believed their physician should be competent in assisting them with their social needs.20
Although lack of training is one possible reason for the lack of current screening by providers, it is likely that other reasons contribute. An additional possible reason for low rates of physician screening for unmet social needs may be physician perceptions that patients and families will be uncomfortable with the personal nature of the screening (e.g., lack of food in the home.) Some physicians may even fear that families of ill children will be offended by the screening, interpreting such screening as implying blame for the patient’s condition or distracting attention from their child’s immediate medical needs.
There is little evidence regarding patient and caregiver opinions of the physician’s role in addressing unmet social needs.20,22,23 Previous research in this area has been limited to the outpatient setting and most often utilized computer-based screening.20,22,23,25 Family opinion of physician screening for unmet social needs in the setting of an acute illness, such as a hospitalization, remains unknown. In addition, since the previous studies did not survey families who were not screened, it is unknown whether opinions about physician screening for unmet screening might change after having been screened by a physician.
In this study, we examined the opinion of parents of in-hospital patients about physician screening for unmet social needs. We also explored associations of parental opinion with family SES and whether the family was screened for unmet social needs by a pediatric resident at the time of admission. We hypothesized that parents of in-hospital patients would have favorable opinions of physician screening for unmet social needs. We also hypothesized that families with lower SES and families who were screened by a resident physician on admission would have more favorable opinions of physician screening.
METHODS
Design & Study Participants
For this cross-sectional survey design study, we recruited a convenience sample of English-speaking biological parents and legal guardians (“caregivers”) of patients less than 18 years admitted to a resident-staffed inpatient general pediatrics service at a freestanding children’s hospital. Only biological parents and legal guardians were permitted to participate; other caregivers, including foster parents or relatives without legal guardianship were not enrolled. All patients were admitted by a pediatric resident. Caregivers were approached within 24 hours of admission to a resident-based inpatient teaching service. If two caregivers were present, the caregivers chose who took the survey. Demographic and clinical characteristics of the patients were gathered through chart review. Collected characteristics included age, gender, race, ethnicity, payor, length of stay, and the presence of a complex chronic condition (CCC). Race categories included white, black, and other. Ethnicity was dichotomized into Hispanic and non-Hispanic. The non-Hispanic category included unknown/missing. “Public” payor included Medicaid, Medicare, and Title V. “Commercial” payor included privately purchased health insurance and TRICARE. The “Other” payor category included self-pay, no charge, and unknown/missing. A CCC is defined as “any medical condition that can be reasonably expected to last at least 12 months (unless death intervenes) and to involve either several different organ systems or one system severely enough to require specialty pediatric care and probably some period of hospitalization in a tertiary care center.”26 We included CCCs to examine if residents preferentially screened patients for unmet social needs who were or were not medically complex. In order to create a proxy for SES, the each patient’s census tract median household income (HHI) was determined. First, the home address of each survey participant was geocoded to determine their census tract. Three addresses (2.1%) could not be geocoded. Census tract HHI was then extracted from the 5-year 2013 American Community Survey, the US Census Bureau’s survey most closely approximating the study period and which also included data at the census tract level. Census tract HHI has previously been shown to be a useful proxy for individual SES.27–29 Census tract HHI was then evenly divided into four quartiles (lowest $0–38,852, low $38,853–49,348, high $49,349–66,359, and highest $66,360 and higher.) These quartiles approximated the following 2013 federal poverty limits (FPL) for a family of four: lowest 0–150% FPL, low 150–200% FPL, high 200–300% FPL, and highest >300% FPL. The study was approved by the Institutional Review Board of Children’s Mercy Hospitals and Clinics.
Primary Exposure and Primary Outcome Measures
The primary exposure was resident physician screening for unmet social needs at the time of admission using a social history method called “IHELP”. Not all admissions were screened for unmet social needs by resident physicians because not all resident physicians had been trained in the IHELP method. (See “Resident Screening for Unmet Social Needs” below.) To determine whether a family was screened by the resident for unmet social needs on admission, we both 1) examined the social history section of the admission history and physical and 2) included in the survey instrument a question to the family whether they had been asked about unmet social needs by a physician when admitted to the hospital. In analyses of the effect of prior physician screening on caregiver opinion, we chose to use the survey participant’s answer regarding whether they had been screened by a resident physician at the time of admission since caregiver recollection would likely be more relevant to caregiver opinion. In addition, census tract median HHI (as a proxy for SES) was examined as a secondary exposure. The primary outcome measures were the scores on each of the three caregiver opinion survey questions.
Resident Physician Screening for Unmet Social Needs
The study occurred within the context of an intervention to improve the social histories of intern physicians rotating on one general pediatrics inpatient service. The interns were instructed on the IHELP social history method in order to improve their detection of actionable, unmet social needs.30 IHELP screens for family concerns regarding income, health insurance, homelessness, poor housing conditions, hunger or food insecurity, educational needs, intimate partner violence, immigration and power of attorney/guardianship needs. The monthly intervention included several components including teaching IHELP, brief role-playing with IHELP, a badge-card of the IHELP questions, attending feedback on the use of IHELP in history and physicals, and, each morning at the start of rounds, the attending asked if there were any “IHELP issues” for the newly admitted patients. The educational intervention to teach IHELP and increase its use included only the daytime interns rotating on the inpatient team. Due to overnight coverage by resident-staffed night teams (which included both interns and upper-level residents), most of whom had not been instructed in IHELP, many families were not screened by a resident on admission. This situation serendipitously allowed us to compare the opinions of screened and unscreened families.
Survey Instrument
The survey instrument asked about the extent to which the caregiver participants agreed with three statements: (1) “I can ask my child’s doctor for help with social issues, like housing, having enough food, and health insurance”; (2) “I believe that my child’s doctor knows how to get me help with social issues like housing, having enough food, and health insurance”; (3) “I believe that my child’s doctor should ask me about my need for help with social issues like housing, having enough food, and health insurance”. These statements were used with permission and modified from a previously published instrument (personal communication A. Garg).20 The three statements are hereafter collectively referred to as “opinion questions” and individually as (1) “I can ask”, (2) “My doctor can help”, and (3) “My doctor should ask”. Responses were on a 5-point Likert scale (1=strongly disagree, 3=neutral, 5=strongly agree). Because Spearman correlations of the survey participant responses to each of these statements were only weak to moderate (r = 0.14 – 0.49), the statements were examined independently and were not combined for a total or mean score.
Analysis
Descriptive statistics were used to examine patient demographic and clinical characteristics and mean opinion scores. For bivariate analyses, there were no meaningful differences in outcomes when analyzing caregiver responses as a five category outcome (strongly disagree disagree, neutral, agree, strongly agree) compared to collapsing the categories into three levels (Disagree-Neutral-Agree.) Using three levels also prevented small cell sizes and facilitated ease of interpretation. As a result, we used a three level outcome, wherein “disagree” and “strongly disagree” were collapsed into a single “disagree” category and “agree” and “strongly agree” were collapsed into a single “agree” category. Bivariate analyses were performed using the chi square test; the Fisher exact test was used when 20% or more of cells had counts less than 5. All statistical analyses were performed using SPSS v.20 (IBM Corporation, Armonk, NY), and p-values <0.05 were considered statistically significant.
RESULTS
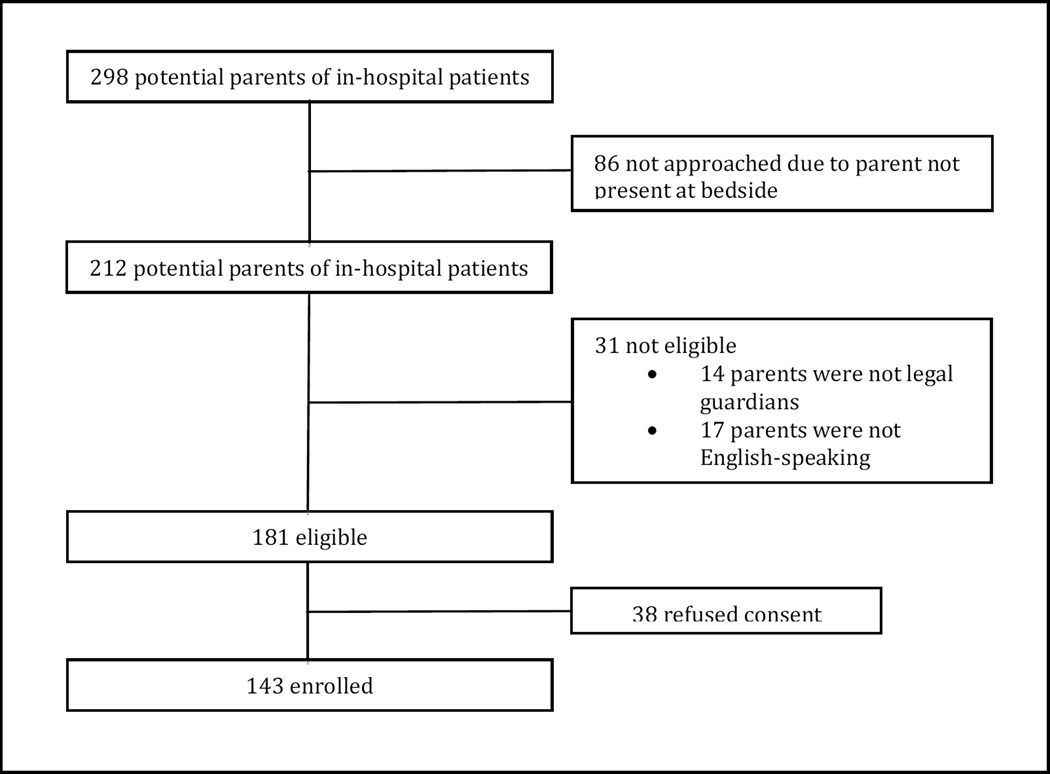
Of the 181 eligible caregivers approached, 143 (79.0%) participated (Figure 1). Majorities of the patients were male, non-Hispanic, and white (Table 1). There were similar proportions of patients with public and commercial insurance. Approximately 1/5 of the study patients had a CCC. Half of the patients were below 200% of the FPL for a family of four. Most respondents agreed with “I can ask” (54.5%), “my doctor can help” (64.3%), and “my doctor should ask” (71.3%) (Table 2). Less than 15% disagreed for all 3 statements.
Figure 1.
Enrollment of Parents of In-Hospital Patients and Survey Completion
Table 1.
Demographic and Clinical Characteristics of the Patient Population
| Characteristic | Study Population, n (%) | |
|---|---|---|
| Total Study Population | 143 (100.0) | |
| Age | <1 | 47 (32.9) |
| 1–4y | 37 (25.9) | |
| 5–12y | 38 (26.6) | |
| 13–17y | 21 (14.7) | |
| Gender | Male | 82 (57.3) |
| Female | 61 (42.7) | |
| Ethnicity* | Hispanic | 8 (5.6) |
| Non-Hispanic | 132 (92.3) | |
| Race | White | 101 (70.6) |
| Black | 25 (17.5) | |
| Other | 17 (11.9) | |
| Payor* | Public | 59 (41.3) |
| Commercial | 71 (49.7) | |
| Other | 10 (7.0) | |
| Census Tract Median Household Income** | Highest (>$66,359) | 35 (25.0) |
| High ($49,349–66,359) | 35 (25.0) | |
| Low ($38,853–49,348) | 35 (25.0) | |
| Lowest (<$38,853) | 35 (25.0) | |
| Complex Chronic Condition | 28 (19.6) | |
| Screened by Physician for Social Needs | Yes | 42 (29.4) |
| No/Unsure | 101 (70.6) | |
Unknown category for ethnicity and payor not displayed.
The census tracts for 3 patients (2.1%) could not be determined.
Table 2.
Caregiver Opinions of Physician Screening for Unmet Social Needs by Patient Characteristic
| Characteristic | I can ask my child’s doctor for help with social issues, n (%) |
My child’s doctor knows how to get me help with social issues, n (%) |
My child’s doctor should ask me about social issues, n (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Disagree | Neutral | Agree | P | Disagree | Neutral | Agree | P | Disagree | Neutral | Agree | P | ||
| Total Study Population | 15 (10.5) | 50 (35.0) | 78 (54.5) | 15 (10.5) | 36 (25.2) | 92 (64.3) | 12 (8.4) | 29 (20.3) | 102 (71.3) | ||||
| SES (Median Household Income)* | Highest (>$66,359) | 3 (8.6) | 15 (42.9) | 17 (48.6) | 0.82 | 4 (11.4) | 12 (34.3) | 19 (54.3) | 0.42 | 3 (8.6) | 6 (17.1) | 26 (74.3) | 0.38 |
| High ($49,349– 66,359) | 4 (11.4) | 14 (40.0) | 17 (48.6) | 2 (5.7) | 7 (20.0) | 26 (74.3) | 2 (5.7) | 8 (22.9) | 25 (71.4) | ||||
| Low ($38,853– 49,348) | 5 (14.3) | 11 (31.4) | 19 (54.3) | 6 (17.1) | 10 (28.6) | 19 (54.3) | 5 (14.3) | 10 (28.6) | 20 (57.1) | ||||
| Lowest (<$38,853) | 3 (8.6) | 10 (28.6) | 22 (62.9) | 3 (8.6) | 7 (20.0) | 25 (71.4) | 2 (5.7) | 4 (11.4) | 29 (82.9) | ||||
| Screened by Physician for Social Needs | Yes | 2 (4.8) | 8 (19.0) | 32 (76.2) | <0.01 | 1 (2.4) | 7 (16.7) | 34 (81.0) | 0.02 | 3 (7.1) | 3 (7.1) | 36 (85.7) | 0.03 |
| No/Unsure | 13 (12.9) | 42 (41.6) | 46 (45.5) | 14 (13.9) | 29 (28.7) | 58 (57.4) | 9 (8.9) | 26 (25.7) | 66 (65.3) | ||||
The census tracts for 3 patients (2.1%) could not be determined; SES analysis limited to 140 participants.
Impact of Resident Physician Asking About Social Needs on Admission
We next sought to determine the impact of caregivers’ prior experience of being screened for social needs by a physician on their opinions of screening. Prior experience of being screened was determined from their response regarding whether a physician had asked them about unmet needs on admission. Most caregivers (67.8%) stated that they were not asked about unmet social needs at the time of admission (an additional 2.8% were unsure) (Table 1). Among caregivers who responded in the survey that they had not been asked about unmet social needs by a physician at the time of admission, the admission history and physical of 16 (16.5%) of those caregivers recorded that IHELP screening had been performed. Patients screened and not screened by a resident physician at the time of admission did not differ by payor or by SES (using census tract HHI as a proxy, P>0.05.) Patients screened and not screened by a resident physician at the time of admission also were of similar age, gender, race, or CCC (all differences P>0.05). A higher percentage of Hispanic patients were screened than non-Hispanic patients (62.5% vs. 26.5%, P=0.05). The proportion of participants who agreed with the opinion questions was high regardless of whether they stated they had been screened or not (Table 2). The proportion stating they agreed was always at least 45%, regardless of opinion question and screening status. However, caregivers who stated that they had been screened for unmet social needs at the time of admission, had significantly more favorable opinions. More than 3/4 of caregivers who had been screened by a resident, compared to approximately half of unscreened caregivers, agreed that they could ask their child’s physician for help with social issues, that their child’s physician knew how to help them with those needs, and that their child’s physician should ask caregivers about unmet social needs.
Impact of SES on Caregiver Opinion
We then sought to determine any associations of SES and caregiver opinion of the physician’s role in screening and assisting with social needs. The patient’s home census tract median HHI was used as a proxy for their SES and the study population was divided into quartiles. There were no differences in opinion based upon quartile of SES, with the majority of nearly all SES groups agreeing with all three statements and the proportion of participants disagreeing with any statement virtually never exceeding 15% (Table 2).
DISCUSSION
This study describes opinions of caregivers of hospitalized children on the role of physicians in screening and assisting with unmet social needs. A majority of parents felt that they could ask their physicians for assistance with unmet social needs, that their physician knew how to help them with those needs, and that physicians should ask patients about social needs. Parents who reported being asked about unmet needs at the time of admission reported greater confidence in their ability to ask and receive help from their physician and more favorable opinions regarding whether physicians should ask patients about social issues. There were no differences in opinion or in who was screened based upon SES.
These findings have implications for practicing pediatricians as well as directors of pediatric residency programs. Collectively, the acceptability of screening for social needs in this study’s acute setting and previous studies conducted in the outpatient setting support physician screening for unmet social needs.20,22,23 The opinion scores in the current study were comparable to previous outpatient studies (which had favorable opinion scores ranging from 76% – 84%).20,22,23 Our findings should give confidence to pediatricians seeking to address at least one unmet social need even in the acute setting and when priorities are naturally focused on the current illness. Furthermore, our findings suggest that families have more favorable opinions of the physicians’ role in addressing those needs after they have been screened. Although preliminary and based on a proxy for SES, rather than a more direct measurement of SES, our findings also suggest that caregivers of different SES similarly approve of physician screening for social determinants.
Pediatricians are further supported in their screening for unmet social needs as a part of the patient-centered medical home by such guidelines as Bright Futures and other policy statements of the American Academy of Pediatrics.4,13,31 Screening for unmet social needs has been successfully implemented in a variety of ways—including waiting room paper-based screening instruments,20,32,33 computer-based questionnaires,22,23,25 and the physician’s social history30—and integrated into the electronic health record.34 Furthermore, with new advocacy training requirements for all US pediatric residency programs,35 it is possible that newly trained pediatricians will consider screening for unmet social needs a routine part of pediatric practice. Several descriptions on how physicians can assist families once an unmet need had been detected have been described, including comprehensive social work programs,36 readily available databases or patient-guided computer programs,22,23,32 as well as programs such as Health Leads37 and medical-legal partnerships.38,39 However, further studies are needed to determine whether patients receive needed services, if the unmet need is rectified, and if child health and health care utilization are affected.40
Several limitations to our findings must be considered. First, the enrolled study population was drawn from a general pediatrics team and may not be generalizable to all in-hospital families, including those drawn from high admission frequency specialty teams (e.g., hematology-oncology). In addition, approximately 20% of eligible parents refused participation and it is possible that those parents represent a substantially different population. Also, due to limitations in bilingual staff, we were unable to enroll non-English-speaking parents. It is unclear how the opinions of non-English speaking families may differ from our study population. Non-English families may have a higher likelihood of being immigrant families (regardless of whether the patient is an immigrant) and therefore may be more aware of additional restrictions or have additional fears of seeking help for social needs. Although we cannot be certain, the opinions of non-English speaking families may be, therefore, more pessimistic of the role of physicians in helping with social needs. We also cannot assess how resident physicians actually screened for social needs or whether their choices of whom to screen were fundamentally biased. Our findings at least suggest that the screened and unscreened groups were similar, except for ethnicity. However, it is still possible that screened patients differed from unscreened patients. For instance patients who were admitted overnight (and therefore admitted by the overnight team which had not been trained in IHELP) may differ from patients admitted during the day. Even residents who had not been formally trained in IHELP may have learned of IHELP (e.g., during sign-out from the day team) and chose whom to screen without the expectations of screening faced by the day team. The direction of this potential bias is unclear. In addition, our findings of caregiver opinions are limited specifically to physicians. Caregiver opinions may differ in regard to screening by non-physicians, such as office staff and nurses. As a result, our findings may not be applicable to physicians who seek to screen for unmet social needs using other health care personnel. Finally, because the survey was conducted within twenty-four hours of admission, it is uncertain whether the opinion of caregivers may change over time or in reaction to either receiving or not receiving assistance in response to disclosing any unmet needs. We found that some caregivers could not remember whether they had been asked about unmet social needs and some caregivers stated that they were not asked but the admission history and physical documented that IHELP had been used by the admitting resident physician. It is unclear if this discrepancy was due to inaccurate resident physician documentation, forgetfulness by the patient caregiver, or lack of presence at admission by the survey respondent caregiver.
CONCLUSIONS
Caregivers of in-hospital pediatric patients have favorable opinions of the physician’s role in addressing unmet social needs, especially those caregivers who were previously screened by a physician. Given the connection of social needs to health in children, physicians should be confident in the acceptability of screening families for social needs in both the well child and acute settings. Further research is needed to determine the best manner of screening and if physician screening results in the acquisition of ameliorative resources for patient families and ultimately improvements in child health.
WHAT’S NEW.
Caregivers of hospitalized pediatric patients have favorable opinions of physician screening for unmet social needs, especially when previously screened by a pediatric resident. Given the connection to health, physicians should be confident in screening families for social needs.
Acknowledgments
Funding for this project was provided by the Katherine B. Richardson Award from Children’s Mercy Hospitals and Clinics. Research reported in this publication was also supported by the National Institute on Drug Abuse of the National Institutes of Health under award number DA07272. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsors had no role in study design, data collection, analysis or interpretation, the writing of the manuscript, or the decision to submit the manuscript for publication. Survey questions were used with permission and modified from Arvin Garg, M.D. The authors would also like to thank Kathleen Aug, Tiffany Smith, and Rose Thompson for their assistance in administering surveys.
Abbreviations
- CCC
complex chronic condition
- HHI
median household income
- SES
socioeconomic status
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: All of the authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: All of the authors declare no conflicts of interest.
Author Contributions
Jeffrey D Colvin - Has participated in the study design, analysis and interpretation of the data, and was the primary author of the manuscript. He has approved the final version of the manuscript being submitted.
Jessica L. Bettenhausen - Has participated in the study design, analysis and interpretation of the data, and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Kaston D. Anderson-Carpenter - Has participated in the study design, analysis and interpretation of the data, and has provided critical intellectual content in the revision of the manuscript. He has approved the final version of the manuscript being submitted.
Vicki Collie-Akers - Has participated in the study design, analysis and interpretation of the data, and has provided critical intellectual content in the revision of the manuscript. She has approved the final version of the manuscript being submitted.
Paul J. Chung - Has participated in the study design, analysis and interpretation of the data, and has provided critical intellectual content in the revision of the manuscript. He has approved the final version of the manuscript being submitted.
Contributor Information
Jeffrey D. Colvin, Email: jdcolvin@cmh.edu.
Jessica L. Bettenhausen, Email: jlbettenhausen@cmh.edu.
Kaston D. Anderson-Carpenter, Email: kacarpenter@ucla.edu.
Vicki Collie-Akers, Email: vcollie@ku.edu.
Paul J. Chung, Email: paulchung@mednet.ucla.edu.
REFERENCES
- 1.Singh GK, Yu SM. US childhood mortality, 1950 through 1993: Trends and socioeconomic diffferentials. American Journal of Public Health. 1996;86(4):505–512. doi: 10.2105/ajph.86.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Victorino CC, Gauthier AH. The social determinants of child health: variations across health outcomes – a population-based cross-sectional analysis. BMC Pediatr. 2009;9(1):53. doi: 10.1186/1471-2431-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newacheck PW, Hung YY, Park MJ, Brindis CD, Irwin CE. Disparities in adolescent health and health care: does socioeconomic status matter? Health Serv Res. 2003;38(5):1235–1252. doi: 10.1111/1475-6773.00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shonkoff JP, Garner AS, et al. The Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, and Section on Developmental and Behavioral Pediatrics. The Lifelong Effects of Early Childhood Adversity and Toxic Stress. Pediatrics. 2011;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- 5.Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Annals of the New York Academy of Sciences. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 6.Kawachi I, Kennedy BP. Income inequality and health: pathways and mechanisms. Health Serv Res. 1999;34(1 Pt 2):215–227. [PMC free article] [PubMed] [Google Scholar]
- 7.Berkman L, Glass T. Social integration, social networks, social support, and health. In: Berkman L, Kawachi I, editors. Social Epidemiology. New York, NY: 2000. pp. 137–173. [Google Scholar]
- 8.Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. J Pers Soc Psychol. 1998;74(3):763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- 9.Adler N, Snibbe A. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Pscyhological SCience. 2003;12(4):119–123. [Google Scholar]
- 10.Casey PH, Szeto KL, Robbins JM, et al. Child health-related quality of life and household food security. Archives of Pediatrics and Adolescent Medicine. 2005;159(1):51–56. doi: 10.1001/archpedi.159.1.51. [DOI] [PubMed] [Google Scholar]
- 11.Kirkpatrick SI, McIntyre L, Potestio ML. Child hunger and long-term adverse consequences for health. Archives of Pediatrics and Adolescent Medicine. 2010;164(8):754–762. doi: 10.1001/archpediatrics.2010.117. [DOI] [PubMed] [Google Scholar]
- 12.Larson K, Halfon N. Family Income Gradients in the Health and Health Care Access of US Children. Matern Child Health J. 2009;14(3):332–342. doi: 10.1007/s10995-009-0477-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Council on Community Pediatrics. Providing Care for Children and Adolescents Facing Homelessness and Housing Insecurity. Pediatrics. 2013;131(6):1206–1210. doi: 10.1542/peds.2013-0645. [DOI] [PubMed] [Google Scholar]
- 14.Rosenstreich DL, Eggleston P, Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med. 1997;336(19):1356–1363. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 15.Frank DA, Casey PH, Black MM, et al. Cumulative Hardship and Wellness of Low-Income, Young Children: Multisite Surveillance Study. Pediatrics. 2010;125(5):e1115–e1123. doi: 10.1542/peds.2009-1078. [DOI] [PubMed] [Google Scholar]
- 16.Fieldston ES, Zaniletti I, Hall M, et al. Community household income and resource utilization for common inpatient pediatric conditions. Pediatrics. 2013;132(6):e1592–e1601. doi: 10.1542/peds.2013-0619. [DOI] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: National Academies Press; 2014. pp. 1–375. [PubMed] [Google Scholar]
- 18.Fiscella K, Burstin HR, Nerenz DR. Quality measures and sociodemographic risk factors: to adjust or not to adjust. JAMA. 2014;312(24):2615–2616. doi: 10.1001/jama.2014.15372. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein D, Holmes J. 2011 Physicians' Daily Life Report. 2011:1–104. Available at: http://www.rwjf.org/vulnerablepopulations/product.jsp?id=73679. [Google Scholar]
- 20.Garg A, Butz AM, Dworkin PH, Lewis RA, Serwint JR. Screening for Basic Social Needs at a Medical Home for Low-Income Children. Clinical Pediatrics. 2008;48(1):32–36. doi: 10.1177/0009922808320602. [DOI] [PubMed] [Google Scholar]
- 21.Klein MD, Kahn RS, Baker RC, Fink EE, Parrish DS, White DC. Training in social determinants of health in primary care: does it change resident behavior? Academic Pediatrics. 2011;11(5):387–393. doi: 10.1016/j.acap.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 22.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families' Health-Related Social Problems and Missed Referral Opportunities. Pediatrics. 2007;119(6):e1332–e1341. doi: 10.1542/peds.2006-1505. [DOI] [PubMed] [Google Scholar]
- 23.Hassan A, Blood EA, Pikcilingis A, et al. Youths' Health-Related Social Problems: Concerns Often Overlooked During the Medical Visit. Journal of Adolescent Health. 2013;53(2):265–271. doi: 10.1016/j.jadohealth.2013.02.024. [DOI] [PubMed] [Google Scholar]
- 24.Weiner SJ, Schwartz A, Weaver F, et al. Contextual errors and failures in individualizing patient care: a multicenter study. Ann Intern Med. 2010;153(2):69–75. doi: 10.7326/0003-4819-153-2-201007200-00002. [DOI] [PubMed] [Google Scholar]
- 25.Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A Randomized Trial on Screening for Social Determinants of Health: the iScreen Study. Pediatrics. 2014;134(6):e1611–e1618. doi: 10.1542/peds.2014-1439. [DOI] [PubMed] [Google Scholar]
- 26.Feudtner C, Feinstein JA, Satchell M, Zhao H, Kang TI. Shifting place of death among children with complex chronic conditions in the United States, 1989–2003. JAMA. 2007;297(24):2725–2732. doi: 10.1001/jama.297.24.2725. [DOI] [PubMed] [Google Scholar]
- 27.Krieger N, Chen JT, Waterman PD, Soobader M-J, Subramanian SV, Carson R. Choosing area based socioeconomic measures to monitor social inequalities in low birth weight and childhood lead poisoning: The Public Health Disparities Geocoding Project (US) Journal of Epidemiology & Community Health. 2003;57(3):186–199. doi: 10.1136/jech.57.3.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. American Journal of Public Health. 1992 doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Geronimus AT, Bound J. Use of census-based aggregate variables to proxy for socioeconomic group: evidence from national samples. American Journal of Epidemiology. 1998;148(5):475–486. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- 30.Kenyon C, Sandel M, Silverstein M, Shakir A, Zuckerman B. Revisiting the Social History for Child Health. Pediatrics. 2007;120(3):e734–e738. doi: 10.1542/peds.2006-2495. [DOI] [PubMed] [Google Scholar]
- 31.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd. Elk Grove, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 32.Garg A, Butz AM, Dworkin PH, Lewis RA, Thompson RE, Serwint JR. Improving the Management of Family Psychosocial Problems at Low-Income Children's Well-Child Care Visits: The WE CARE Project. Pediatrics. 2007;120(3):547–558. doi: 10.1542/peds.2007-0398. [DOI] [PubMed] [Google Scholar]
- 33.Keller D, Jones N, Savageau J, Cashman S. Development of a Brief Questionnaire to Identify Families in Need of Legal Advocacy to Improve Child Health. Ambulatory Pediatrics. 2008;8(4):266–269. doi: 10.1016/j.ambp.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 34.Beck AF, Klein MD, Kahn RS. Identifying social risk via a clinical social history embedded in the electronic health record. Clinical Pediatrics. 2012;51(10):972–977. doi: 10.1177/0009922812441663. [DOI] [PubMed] [Google Scholar]
- 35.Accreditation Council for Graduate Medical Education, American Board of Pediatrics. The Pediatrics Milestone Project. 2013:1–124. [Google Scholar]
- 36.Kitchen A, Brook J. Social Work at the Heart of the Medical Team. Social Work in Health Care. 2005;40(4):1–18. doi: 10.1300/J010v40n04_01. [DOI] [PubMed] [Google Scholar]
- 37.Garg A, Marino M, Vikani AR, Solomon BS. Addressing families' unmet social needs within pediatric primary care: the health leads model. Clinical Pediatrics. 2012;51(12):1191–1193. doi: 10.1177/0009922812437930. [DOI] [PubMed] [Google Scholar]
- 38.Zuckerman B, Sandel M, Smith L, Lawton E. Why pediatricians need lawyers to keep children healthy. Pediatrics. 2004;114(1):224–228. doi: 10.1542/peds.114.1.224. [DOI] [PubMed] [Google Scholar]
- 39.Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and Lawyers Collaborating to HeLP Children—Outcomes from a Successful Partnership between Professions. Journal of Health Care for the Poor and Underserved. 2013;24(3):1063–1073. doi: 10.1353/hpu.2013.0147. [DOI] [PubMed] [Google Scholar]
- 40.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing Social Determinants of Health at Well Child Care Visits: A Cluster RCT. Pediatrics. 2015;135(2):e296–e304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]