Abstract
Background
The aim of the present study was to examine demographic and socioeconomic differences and time trends of bariatric surgery in Sweden during 1990–2010.
Methods
An open cohort of all individuals aged 20–64 years was followed between 1990 and 2010. Socioeconomic differences were examined during two periods: 1990–2005 and 2006–2010 using cumulative rates in a closed cohort. Hazard ratios (HRs) of bariatric surgery were calculated in these two periods using Cox regression models.
Results
A majority of the 22,198 individuals that underwent bariatric surgery were women (76.3 %). Women were more likely to undergo surgery in younger ages (30–39 years), while men were more likely to undergo surgery around 10 years later (40–49 years). The number of surgeries increased substantially during the second period. During the whole period, the dominating surgical method was gastric bypass contributing to 69.4 % of the procedures. HRs for bariatric surgery were highest for individuals with intermediate educational level and intermediate-low income in both periods. For married/cohabiting and/or employed individuals, the HRs were highest during the first period whereas an opposite pattern was seen in the second period.
Conclusions
Individuals in the lowest socioeconomic groups undergo bariatric surgery less often than those with intermediate income and educational level, although previous research has shown that those with low socioeconomic status have the highest rates of morbid obesity. The failure to identify eligible individuals for surgery may result in negative effects on those individuals with the largest need for weight loss.
Keywords: Obesity, Bariatric surgery, Socioeconomic differences, Time trends
Introduction
Obesity (i.e., body mass index [BMI] ≥30 kg/m2) is one of the major global health problems [1]. In Sweden, the prevalence of obesity has doubled over the last 20 years [2]. Obesity is associated with numerous comorbidities, such as diabetes, hypertension, cardiovascular disease, and sleep apnea syndrome [3, 4].
Lifestyle modification (diet and exercise) is most often recommended for obese individuals, including those morbidly obese (BMI≥40 kg/m2) [5–7]. However, conventional methods of weight loss have often been ineffective in achieving sustained weight loss in morbidly obese individuals. The best weight loss programs have only maintained a sustained excess body weight loss of 10 %. This small reduction in excess body weight has little if any effect on obesity-related comorbidities in the morbidly obese population [8–10].
Bariatric surgery may be an appropriate treatment in patients refractory to nonsurgical therapy and who have either morbid obesity or moderate obesity (BMI 35.0–39.9 kg/m2) plus a major obesity-related comorbidity [6, 7]. Studies have demonstrated that bariatric surgery reduces weight by 33 % in the early postoperative years [11] and 14–25 % after 10 years [12]. Surgery is associated with remission rates of 66–88 % in medical comorbidities [13] and significant reduction in 15-year mortality in comparison to nonsurgical-matched controls [12]. Quality of life, self-esteem, and employment status are also improved after surgery, [14] and surgical costs appear to be recouped within 2–4 years [15].
In countries with private health-care insurance systems, socioeconomic factors play a major role in determining which individuals undergo bariatric surgery, despite medical eligibility. Significant disparities according to race, income, educational level, and insurance type exist [16]. Since Sweden has a universal health-care insurance system, the patients’ socioeconomic factors should not be a major barrier to receiving surgery. However, we hypothesize that there still may be socioeconomic disparities among patients that undergo bariatric surgery. In Sweden, all hospital care, publicly funded and private, is registered by the National Board of Health and Welfare that administrates a nationwide registry including surgical and diagnostic codes [17]. To the best of our knowledge, this is the first nationwide study that tests our hypothesis, in a country with universal health-care system, meaning that the access to health care will not constitute a confounder in the present study, which represents a novel contribution to previous literature.
The primary aim of this study was to investigate the potential impact of sociodemographic characteristics on the rate of bariatric surgery. The secondary aim was to evaluate time trends in terms of incidence rates as well as choice of surgical methods between 1990 and 2010.
Materials and Methods
Data used in this study were retrieved from a nationwide database, at the Center for Primary Health Care Research, Lund University [18, 19]. The database incorporates longitudinal hospitalization data for the entire population from the Swedish Inpatient Register, provided by the National Board of Health and Welfare. Population-wide documentation regarding demographic and socioeconomic variables was obtained from the Total Population Register, provided by Statistics Sweden, the Swedish government-owned census bureau. Additional individual-level linkages in the database included data from the national Cause of Death Register [18] and the Immigration Register (to identify dates of immigration and/or emigration). All linkages were performed by the use of an individual national identification number that is assigned to each permanent resident in Sweden for their lifetime. This number was replaced by a serial number for each person in order to provide anonymity.
The follow-up period started on January 1, 1990 and proceeded until first hospitalization for bariatric surgery, death, emigration, or the end of the study period on December 31, 2010. We divided this period into two periods, i.e., 1990–2005 and 2006–2010 since there was a large increase in the number of surgeries during the second period.
Outcome Variable
The outcome variable was bariatric surgery. We used the Swedish Inpatient Register to identify main diagnoses of obesity and operation in the study population. The International Classification of Disease (ICD) versions 9 and 10 were used to identify patients with a diagnosis of obesity (ICD-9, 278A and ICD-10, E66) [20]. The Swedish Classification of Operations and Major Procedures was used to identify patients undergoing bariatric surgery: operation codes 4751– 4753 before 1997, or codes JDF00–JDF01, JDF10–JDF11, and JDF20–JDF21 from 1997 and onwards. The subtypes of bariatric surgery were defined as gastroplasty (codes 4751 and JDF00–JDF01), gastric bypass (codes 4752 and JDF10–JDF11), and gastric banding (codes 4753 and JDF20–JDF21).
Individual Variables
The individual variables were defined at baseline.
Gender Male or female
Age
Age was categorized as 20–29, 30–39, 40–49, or 50–64 years.
Family Income
Family income was calculated as annual family income divided by the number of members in the family. The income calculation was weighted, taking the ages of the family members into account. Children were given lower consumption weights than adults. The calculation was performed as follows: the sum of all family members’ incomes was multiplied by the individual's consumption weight divided by the family members’ total consumption weight. The final variable was calculated as empirical quartiles from the distribution [21] and classified as low, intermediate-low, intermediate-high, and high.
Marital Status
Individuals were classified as married/cohabitating or single.
Educational Attainment
Educational attainment was classified as follows:
Low: completion of compulsory school or less (≤9 years)
Intermediate: practical high school or some theoretical high school (10–11 years)
High: theoretical high school and/or college (≥12 years)
Employment was defined as yes or no.
Statistical Analysis
1. Incidence rates
Person-years were calculated for all individuals from the start of follow-up until first hospitalization for bariatric surgery, death, emigration, or closing date (December 31, 2010). Age, gender, period, and subtypes of operation-specific incidence rates were calculated for the whole follow-up period. Relative weights used to calculate the incidence rates were based on the 2000 European standard population [22].
2. Hazard ratios (HRs)
Separate analyses were performed for the periods 1990 to 2005 and 2006 to 2010. The rationale for dividing the entire follow-up period into two unequal periods was that there was a large increase in the number of performed bariatric surgery from 2006, and one of the goals of this study was to examine time trends.
The associations between the individual variables and the outcome were analysed with Cox regression models. Cox proportional hazard models are used to study the association between certain variables and the time it takes for a specified event to happen, in this case the first event of bariatric surgery. First, a univariate Cox regression was performed for each variable. Next, a multivariate Cox regression model including all variables was calculated. All analyses were performed using the SAS version 9.2 (SAS Institute, Cary, NC, USA) [23].
Ethical Considerations
This study was approved by the Ethics Committee at Lund University.
Results
As shown in Table 1, a total number of 22,198 individuals (5,258 men, 23.7 %, and 16,940 women, 76.3 %), aged 20–64 years underwent bariatric surgery between 1990 and 2010 in Sweden. Women underwent surgery mainly between 30 and 39 years of age (32.2 %), while men underwent surgery mainly between 40 and 49 years of age (34.3 %).
Table 1.
Distribution of population, number of bariatric surgery events, and age-standardized incidence rates (IR) (per 100,000 person-years) of bariatric surgery, 1990–2010, open cohort
| Men (N=6,082,206) |
Women (N=6,092,368) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | IR | 95 % CI | No. | % | IR | 95 % CI | |||
| Total bariatric surgery events | 5,258 | 5.6 | 5.5 | 5.8 | 16,940 | 18.5 | 18.2 | 18.8 | ||
| Gastroplasty | 801 | 15.2 | 0.8 | 0.8 | 0.9 | 2,891 | 17.1 | 3.1 | 3.0 | 3.2 |
| Gastric bypass | 3,754 | 71.4 | 3.9 | 3.7 | 4.0 | 11,651 | 68.8 | 12.5 | 12.2 | 12.7 |
| Gastric banding | 703 | 13.4 | 0.7 | 0.7 | 0.8 | 2,398 | 14.2 | 2.6 | 2.5 | 2.7 |
| Age (years) at surgery | ||||||||||
| 20–29 | 640 | 12.2 | 5.1 | 4.7 | 5.5 | 2,721 | 16.1 | 22.7 | 21.9 | 23.6 |
| 30–39 | 1,383 | 26.3 | 10.2 | 9.7 | 10.7 | 5,460 | 32.2 | 42.0 | 40.9 | 43.1 |
| 40–49 | 1,803 | 34.3 | 13.1 | 12.5 | 13.7 | 5,153 | 30.4 | 38.6 | 37.6 | 39.7 |
| 50–64 | 1,432 | 27.2 | 7.9 | 7.5 | 8.3 | 3,606 | 21.3 | 20.2 | 19.6 | 20.9 |
| Period | ||||||||||
| 1990–1994 | 726 | 13.8 | 3.6 | 3.3 | 3.9 | 2,439 | 14.4 | 12.5 | 12.0 | 13.0 |
| 1995–1999 | 614 | 11.7 | 2.7 | 2.4 | 2.9 | 2,327 | 13.7 | 10.5 | 10.1 | 11.0 |
| 2000–2004 | 580 | 11.0 | 2.5 | 2.3 | 2.7 | 1,896 | 11.2 | 8.6 | 8.2 | 9.0 |
| 2005–2010 | 3,338 | 63.5 | 13.0 | 12.6 | 13.5 | 10,278 | 60.7 | 42.0 | 41.2 | 42.8 |
Table 2 shows cumulative rates for the two periods 1990–2005 and 2006–2010. Bariatric surgery was more common in women in both periods. Individuals who were married/cohabitating, had intermediate-low income, or intermediate educational level had the highest rates in both periods. The cumulative rates were highest for employed individuals during the first period whereas it was equal for employed and unemployed individuals during the second period.
Table 2.
Population, bariatric surgery events, and age-adjusted cumulative rates (per 1,000 individuals) by individual characteristics, closed cohorts
| Period 1990–2005 |
Period 2006–2010 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Population | Events | Rate | 95 % CI | Population | Events | Rate | 95 % CI | |||
| Total population | 5,517,045 | 8,350 | 1.51 | 1.48 | 1.55 | 6,061,363 | 12,533 | 2.07 | 2.03 | 2.10 |
| Gender | ||||||||||
| Men | 2,804,513 | 1,903 | 0.68 | 0.65 | 0.71 | 3,090,682 | 3,125 | 1.01 | 0.98 | 1.05 |
| Women | 2,712,532 | 6,447 | 2.38 | 2.32 | 2.43 | 2,970,681 | 9,408 | 3.17 | 3.10 | 3.23 |
| Age at baseline (years) | ||||||||||
| 20–29 | 1,407,140 | 2,940 | 2.09 | 2.01 | 2.16 | 1,266,894 | 2,121 | 1.67 | 1.60 | 1.75 |
| 30–39 | 1,299,787 | 2,548 | 1.96 | 1.88 | 2.04 | 1,410,042 | 4,279 | 3.03 | 2.94 | 3.13 |
| 40–49 | 1,396,672 | 2,156 | 1.54 | 1.48 | 1.61 | 1,387,489 | 3,812 | 2.75 | 2.66 | 2.83 |
| 50–64 | 1,413,446 | 706 | 0.50 | 0.46 | 0.54 | 1,996,938 | 2,321 | 1.16 | 1.11 | 1.21 |
| Family income (quartiles) | ||||||||||
| Low | 1,332,555 | 1,543 | 1.02 | 0.97 | 1.07 | 1,517,062 | 2,535 | 1.51 | 1.45 | 1.57 |
| Intermediate-low | 1,408,640 | 2,872 | 1.91 | 1.84 | 1.98 | 1,514,053 | 4,678 | 3.02 | 2.93 | 3.10 |
| Intermediate-high | 1,380,609 | 2,260 | 1.70 | 1.63 | 1.77 | 1,515,775 | 3,397 | 2.24 | 2.17 | 2.32 |
| High | 1,395,241 | 1,675 | 1.31 | 1.25 | 1.37 | 1,514,473 | 1,923 | 1.31 | 1.25 | 1.36 |
| Marital status | ||||||||||
| Married/cohabiting | 2,637,039 | 3,938 | 1.97 | 1.91 | 2.03 | 2,300,169 | 5,022 | 2.52 | 2.45 | 2.59 |
| Never married, widowed/divorced | 2,880,006 | 4,412 | 1.42 | 1.38 | 1.46 | 3,761,194 | 7,511 | 1.99 | 1.94 | 2.03 |
| Educational attainment | ||||||||||
| Low | 2,149,491 | 2,860 | 1.52 | 1.47 | 1.58 | 1,652,415 | 2,434 | 1.56 | 1.49 | 1.62 |
| Intermediate | 1,672,815 | 3,969 | 2.20 | 2.14 | 2.27 | 1,422,141 | 4,729 | 3.56 | 3.46 | 3.66 |
| High | 1,694,739 | 1,521 | 0.86 | 0.81 | 0.90 | 2,986,807 | 5,370 | 1.76 | 1.71 | 1.80 |
| Employment status | ||||||||||
| Employment | 4,160,163 | 6,889 | 1.64 | 1.60 | 1.68 | 4,108,665 | 8,698 | 2.08 | 2.03 | 2.12 |
| Unemployment | 1,356,882 | 1,461 | 1.13 | 1.07 | 1.19 | 1,952,698 | 3,835 | 2.08 | 2.02 | 2.15 |
Table 3 shows the Cox regression models that estimate the probability of undergoing bariatric surgery in relation to the individual variables in two different models (univariate and multivariate models). Female gender was associated with significantly higher covariate-adjusted hazard ratios (HRs) of surgery in both periods. Additionally, having intermediate educational level and intermediate-low family income was associated with higher probability of undergoing surgery in both periods. All these results were statistically significant except for intermediate-low income in the first period. Being employed was associated with a higher HR to undergo surgery during the first period but a lower HR during the second period. For married/cohabiting individuals, the HRs were highest during the first period whereas an opposite pattern was seen in the second period.
Table 3.
Hazard ratios (HR) of bariatric surgery by individual characteristics, Cox regression analysis
| Period 1990–2005 |
Period 2006–2010 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate model |
Multivariate model |
Univariate model |
Multivariate model |
|||||||||
| HR | 95 % CI | HR | 95 % CI | HR | 95 % CI | HR | 95 % CI | |||||
| Gender | ||||||||||||
| Men | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Women | 3.45 | 3.28 | 3.63 | 3.49 | 3.32 | 3.68 | 3.11 | 2.99 | 3.24 | 3.08 | 2.95 | 3.21 |
| Age at baseline (years) | ||||||||||||
| 20–29 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 30–39 | 0.91 | 0.86 | 0.96 | 0.90 | 0.85 | 0.95 | 1.74 | 1.65 | 1.83 | 1.73 | 1.64 | 1.83 |
| 40–49 | 0.70 | 0.67 | 0.74 | 0.66 | 0.62 | 0.70 | 1.54 | 1.46 | 1.63 | 1.41 | 1.33 | 1.50 |
| 50–64 | 0.24 | 0.22 | 0.26 | 0.20 | 0.18 | 0.22 | 0.65 | 0.61 | 0.69 | 0.57 | 0.53 | 0.61 |
| Family income (quartiles) | ||||||||||||
| Low income | 1.08 | 1.01 | 1.16 | 0.65 | 0.60 | 0.70 | 1.49 | 1.40 | 1.58 | 1.32 | 1.24 | 1.41 |
| Intermediate-low income | 1.69 | 1.59 | 1.80 | 1.01 | 0.95 | 1.08 | 2.44 | 2.31 | 2.57 | 1.41 | 1.33 | 1.50 |
| Intermediate-high income | 1.36 | 1.28 | 1.45 | 0.97 | 0.91 | 1.04 | 1.77 | 1.67 | 1.87 | 1.27 | 1.20 | 1.36 |
| High income | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Marital status | ||||||||||||
| Married/cohabiting | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Never married, widowed/divorced | 1.08 | 1.04 | 1.13 | 0.91 | 0.87 | 0.96 | 0.96 | 0.92 | 0.99 | 1.11 | 1.07 | 1.15 |
| Educational attainment | ||||||||||||
| Low | 1.60 | 1.50 | 1.70 | 2.38 | 2.23 | 2.54 | 0.91 | 0.87 | 0.95 | 1.67 | 1.59 | 1.76 |
| Intermediate | 2.62 | 2.47 | 2.78 | 2.52 | 2.37 | 2.68 | 1.84 | 1.77 | 1.92 | 2.01 | 1.93 | 2.10 |
| High | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Employment status | ||||||||||||
| Employment | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Unemployment | 0.76 | 0.71 | 0.80 | 0.88 | 0.82 | 0.94 | 1.03 | 0.99 | 1.07 | 1.37 | 1.31 | 1.43 |
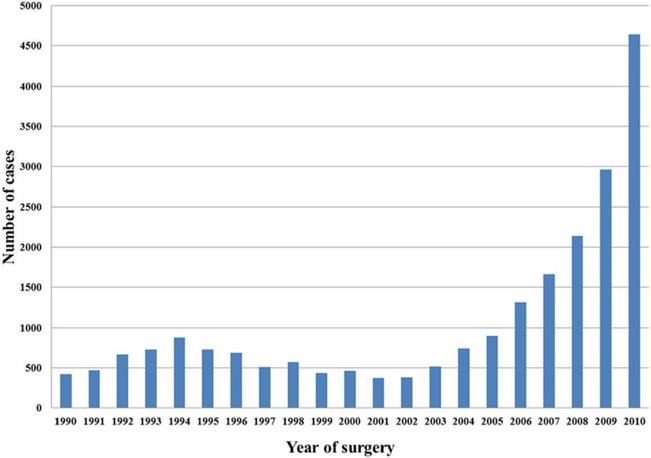
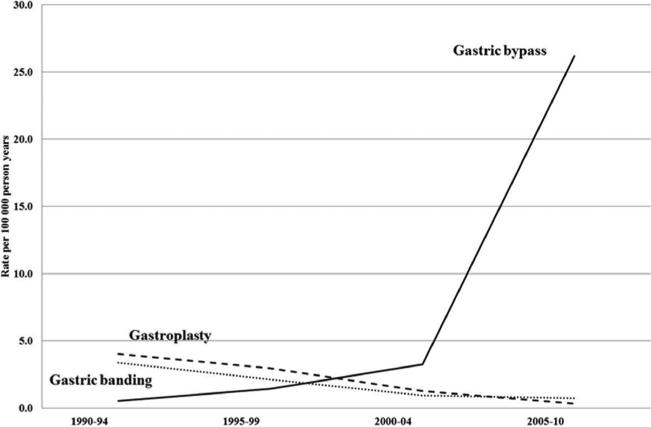
Figure 1 shows the total number of bariatric surgeries for each year between 1990 and 2010. Except for a small peak in 1994, there was a substantial increase in the number of surgeries after 2006. Figure 2 shows the rates of surgery, by the different surgical methods. Gastric bypass was the dominating surgical method during the whole period (69.4 %), and after 2007, it contributed to 97.5 % of all bariatric surgery procedures in Sweden [24].
Fig. 1.
Number of cases of bariatric surgery, ages 20 to 64 years in Sweden, 1990–2010
Fig. 2.
Age-adjusted incidence rates (per 100,000 person-years) of bariatric surgery, 1990–2010
Discussion
This study showed, for the first time, that there is a potential impact of sociodemographic factors on the rate of bariatric surgery in Sweden, despite its universal health insurance system, which provides equal access to health care to all population groups irrespective of individual income. The HRs for bariatric surgery were highest for individuals with intermediate educational level and intermediate-low income in both periods.
Furthermore, the study investigated time trends in terms of incidence and choice of surgical methods during the two time periods 1990–2005 and 2006–2010.
Socioeconomic Factors
In countries with private insurance settings, socioeconomic factors may exert a significant influence on selection of the individuals that undergo bariatric surgery [16]. However, studies of the impact of socioeconomic factors on the probability of undergoing bariatric surgery are scarce. In Sweden, the costs of surgery should not be the primary limitation to receive surgery. However, the results of the present study are similar to a study from Canada [25], a country with a universal health insurance system similar to Sweden. The Canadian study showed low-income patients were less likely to be recommended for bariatric surgery. The factors that might influence the rate of bariatric surgery include rates of obesity in different socioeconomic group, referral patterns, individuals’ awareness and demand, and surgeons’ elimination criteria.
It is already known from multiple studies that obesity is distributed along a socioeconomic gradient with higher prevalence rates in low socioeconomic groups [26]. Furthermore, obesity-related comorbidities are more common in patients with lower incomes [25]. Despite the established fact that obesity is more common in low-income groups, our study showed that the likelihood of surgery was highest in the intermediate income and educational group. The highest socioeconomic groups underwent surgery less often which might reflect the lower rate of obesity in this group [26, 27] and a better lifestyle, i.e., a healthy diet and physical activity [28].
Although our study did not have access to individual-level data on behavior, there are some possible explanations to our findings that individuals in the lowest socioeconomic groups were less likely to undergo surgery. These individuals may be less likely to demonstrate a commitment to preoperative programs, a major precondition for surgical approval [25]. Successful maintenance of weight loss after bariatric surgery relies on patient compliance with postoperative medical and dietary management. Some of the patients eligible for these operations may have difficulties following the necessary postoperative management schemes because of educational or financial limitations [29]. Another limiting factor may be the referral patterns of care providers, leading to a decreased representation of lower socioeconomic groups [16]. Additionally, previous research indicates that obese patients in lower socioeconomic strata may experience a greater social acceptance of excess body weight [30].
Time Trends
The results of the time trend analyses showed an almost fivefold increase in bariatric surgery in Sweden during the study period. This might be not only due to an increasing incidence of morbid obesity in Sweden [2, 31] but also due to an altered view of obesity as a disease, necessitating treatment. Moreover, the awareness among patients about surgical options may have changed [17]. Additionally, the utilization of bariatric procedures has increased throughout the world in concordance with the expanding evidence base of the beneficial effects of surgery [32]. Most importantly, in Sweden, the increase was presumably in response to the publication of the Swedish obese subjects study [11] which most likely had an impact on rate of surgery and referral practice. The small peak in 1994 coincides with the incidence peak of restrictive procedures, such as gastric banding [17], due to the simplicity of the surgical technique and reversibility but the rate subsided later due to reports of complications of the method [33]. There are some similarities and some differences between the two studied time periods. The main differences were that in the second period, surgery was more common in individuals that were single and unemployed, in contrast to the first period. These differences might be due to the fact that in the first period, the number of surgeries was limited, resulting in a more restricted selection of patients.
Gender
In this study, like many other studies [16, 34], women were overrepresented among operated individuals (76.3 %). This overrepresentation may be due to sociocultural norms about body size [35] encouraging women to seek bariatric surgery more often than men. Additionally, women underwent surgery at a younger age (30–39 years old) compared to men (40–49 years old), indicating that the cosmetic aspect of obesity might have been more important to women whereas men might have been less aware of the possibilities of surgical treatment.
Limitations and Strengths
This study had potential limitations. We were not able to include BMI or other anthropometric parameters as variables. Thus, we were unable to assess whether BMI affected the likelihood of undergoing bariatric surgery. Residual confounding is most likely present. For example, the socioeconomic variables cannot fully measure socioeconomic status. The limitations of the study are somewhat balanced by its strengths. To our knowledge, this is the first nationwide study, which included all patients that underwent bariatric surgery in Sweden during a 20-year period. Another important strength of our study is that it was based on Swedish hospitalization data that is highly complete [19].
Conclusion
The present nationwide study has contributed to novel findings of associations between socioeconomic factors and bariatric surgery. Even in a country like Sweden with a universal health-care insurance system, those in the lowest socioeconomic groups were less likely to undergo bariatric surgery, which may have a negative effect on individuals with largest need for weight loss. Further studies are needed to examine the potential barriers to bariatric surgery among individuals in the lowest socioeconomic strata.
Acknowledgments
This work was supported by grants to Dr Kristina Sundquist and Dr Jan Sundquist from the Swedish Research Council as well as ALF funding from Region Skåne awarded to Kristina Sundquist and Jan Sundquist.
Footnotes
Conflict of Interest There are no competing interests.
Contributor Information
Ensieh Memarian, Center for Primary Health Care Research, Lund University/Region Skåne, Skåne University Hospital, CRC, Building 28, floor 11, Jan Waldenströms gata 35, 205 02 Malmö, Sweden.
Susanna Calling, Center for Primary Health Care Research, Lund University/Region Skåne, Skåne University Hospital, CRC, Building 28, floor 11, Jan Waldenströms gata 35, 205 02 Malmö, Sweden.
Kristina Sundquist, Center for Primary Health Care Research, Lund University/Region Skåne, Skåne University Hospital, CRC, Building 28, floor 11, Jan Waldenströms gata 35, 205 02 Malmö, Sweden; Stanford Prevention Research Center, Stanford University School of Medicine, Stanford, CA, USA.
Jan Sundquist, Center for Primary Health Care Research, Lund University/Region Skåne, Skåne University Hospital, CRC, Building 28, floor 11, Jan Waldenströms gata 35, 205 02 Malmö, Sweden; Stanford Prevention Research Center, Stanford University School of Medicine, Stanford, CA, USA.
Xinjun Li, Center for Primary Health Care Research, Lund University/Region Skåne, Skåne University Hospital, CRC, Building 28, floor 11, Jan Waldenströms gata 35, 205 02 Malmö, Sweden.
References
- 1.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Welfare SNBoHa . National Public Health Report 2009 (Folkhälsorapport 2009) Swedish National Board of Health and Welfare; Stockholm: 2009. [Google Scholar]
- 3.Buchwald H, Panel CC. Consensus conference statement bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005;1:371–81. doi: 10.1016/j.soard.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Obesity: preventing and managing the global epidemic. World Health Organization; 2000. p. 252. http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/index.html. [PubMed] [Google Scholar]
- 5.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. National Heart, Lung and Blood Institute, National institute of Health; 1998. [Google Scholar]
- 6.Economics OoH Shedding the pounds. Obesity management, NICE guidance and bariatric surgery in England. 2010 2012. Accessed at www.ohe.org.
- 7.Lau DC, Douketis JD, Morrison KM, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ. 2007;176:S1–13. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atkinson RL, Dietz WH, Foreyt JP, et al. Very low-calorie diets. National Task Force on the Prevention and Treatment of Obesity, National Institutes of Health. JAMA. 1993;270:967–74. [PubMed] [Google Scholar]
- 9.Safer DJ. Diet, behavior modification, and exercise: a review of obesity treatments from a long-term perspective. South Med J. 1991;84:1470–4. [PubMed] [Google Scholar]
- 10.Weintraub M, Sundaresan PR, Schuster B, et al. Long-term weight control study. IV (weeks 156 to 190). The second double-blind phase. Clin Pharmacol Ther. 1992;51:608–14. doi: 10.1038/clpt.1992.72. [DOI] [PubMed] [Google Scholar]
- 11.Sjöström L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 12.Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 13.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 14.Livingston EH, Fink AS. Quality of life: cost and future of bariatric surgery. Arch Surg. 2003;138:383–8. doi: 10.1001/archsurg.138.4.383. [DOI] [PubMed] [Google Scholar]
- 15.Cremieux PY, Buchwald H, Shikora SA, et al. A study on the economic impact of bariatric surgery. Am J Manag Care. 2008;14:589–96. [PubMed] [Google Scholar]
- 16.Martin M, Beekley A, Kjorstad R, et al. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis. 2010;6:8–15. doi: 10.1016/j.soard.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Leffler E, Gustavsson S, Karlson BM. Time trends in obesity surgery 1987 through 1996 in Sweden—a population-based study. Obes Surg. 2000;10:543–8. doi: 10.1381/096089200321593760. [DOI] [PubMed] [Google Scholar]
- 18.National Board of Health and Welfare . Swedish: Värdering av diagnoskvaliteten för akut hjärtinfarkt i patientregistret 1987 och 1995. Epidemiologiskt Centrum, Socialstyrelsen; 2000. Validity of the diagnoses from the Swedish in-care Register 1987 and 1995. [Google Scholar]
- 19.Ludvigsson JF, Andersson E, Ekbom A, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. doi: 10.1186/1471-2458-11-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International Classification of Diseases (ICD) World Health Organization; http://www.who.int/classifications/icd/en/ [Google Scholar]
- 21.Calling S, Li X, Sundquist J, et al. Socioeconomic inequalities and infant mortality of 46,470 preterm infants born in Sweden between 1992 and 2006. Paediatr Perinat Epidemiol. 2011;25:357–65. doi: 10.1111/j.1365-3016.2011.01200.x. [DOI] [PubMed] [Google Scholar]
- 22.Age standardization of rates: a new WHO standard. World Health Organization; 2001. www.who.int/healthinfo/paper31.pdf. [Google Scholar]
- 23.SAS Institute Inc . SAS 9.3. SAS Institute Inc.; NC, USA: 2011. [Google Scholar]
- 24.Yearly report 2011. (Årsrapport 2011) Scandinavian obesity surgery registry (SOREG) 2011 http://www.ucr.uu.se/soreg/index.php/dokument/cat_view/58-dokument/57-arsrappoerter.
- 25.Halloran K, Padwal RS, Johnson-Stoklossa C, et al. Income status and approval for bariatric surgery in a publicly funded regional obesity program. Obes Surg. 2011;21:373–8. doi: 10.1007/s11695-010-0149-4. [DOI] [PubMed] [Google Scholar]
- 26.Kuntz B, Lampert T. Socioeconomic factors and obesity. Dtsch Arztebl Int. 2010;107:517–22. doi: 10.3238/arztebl.2010.0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sundquist J, Johansson SE, Sundquist K. Levelling off of prevalence of obesity in the adult population of Sweden between 2000/01 and 2004/05. BMC Public Health. 2010;10:119. doi: 10.1186/1471-2458-10-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahar D, Shai I, Vardi H, et al. Diet and eating habits in high and low socioeconomic groups. Nutrition. 2005;21:559–66. doi: 10.1016/j.nut.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 29.Livingston EH, Ko CY. Socioeconomic characteristics of the population eligible for obesity surgery. Surgery. 2004;135:288–96. doi: 10.1016/j.surg.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 30.Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989;105:260–75. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- 31.Sjöberg Have lifestyles improved? Statistics Sweden's survey of living conditions (Har levnadsvanorna förbättrats? SCB undersökning om levnadsförhållanden) (ULF). Stat Swed J (Statistiska Centralbyrånstidskrift) 2000:2. [Google Scholar]
- 32.Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294:1909–17. doi: 10.1001/jama.294.15.1909. [DOI] [PubMed] [Google Scholar]
- 33.Westling A, Bjurling K, Ohrvall M, et al. Silicone-adjustable gastric banding: disappointing results. Obes Surg. 1998;8:467–74. doi: 10.1381/096089298765554386. [DOI] [PubMed] [Google Scholar]
- 34.Santry HP, Lauderdale DS, Cagney KA, et al. Predictors of patient selection in bariatric surgery. Ann Surg. 2007;245:59–67. doi: 10.1097/01.sla.0000232551.55712.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuskowska-Wolk A, Rössner S. Inter-relationships between socio-demographic factors and body mass index in a representative Swedish adult population. Diabetes Res Clin Pract. 1990;10(Suppl 1):S271–5. doi: 10.1016/0168-8227(90)90175-s. [DOI] [PubMed] [Google Scholar]