Abstract
The Community Health Improvement Partnership (CHIP) model has supported community health development in more than 100 communities nationally. In 2011, four rural Oregon CHIPs collaborated with investigators from the Oregon Rural Practice-based Research Network (ORPRN), a component of the Oregon Clinical and Translational Research Institute (OCTRI), to obtain training on research methods, develop and implement pilot research studies on childhood obesity, and explore matches with academic partners. This article summarizes the experiences of the Lincoln County CHIP, established in 2003, as it transitioned from CHIP to Community Health Improvement and Research Partnership (CHIRP). Our story and lessons learned may inform rural community-based health coalitions and academicians who are engaged in or considering Community-based participatory research (CBPR) partnerships. Utilizing existing infrastructure and relationships in community and academic settings provides an ideal starting point for rural, bidirectional research partnerships.
Keywords: Community-based participatory research, community health partnerships, rural health, obesity, child
Clinical and Translational Science Awards (CTSAs) have been tasked with speeding the translation of research into practice and communities, ensuring that research reaches diverse populations and is generalizable outside controlled laboratory settings.1 Practice-based research networks, a component of some CTSA programs, are identified as a key element in this final step of research translation.2 However, many CTSAs and practice-based research networks are located in urban settings and few studies describe the perspectives of rural communities and academic partners in translational research.
Rural populations experience many medical and social disparities compared with their urban counterparts.3,4 National and regional studies document that the obesity epidemic, a contributor to many chronic diseases, is especially severe in rural areas.5–8 Rural populations may be excluded from research initiatives for many reasons (e.g., barriers in access, cost, sample size), yet interventions demonstrated to be effective in urban settings may not translate into rural areas (e.g., owing to differences in resource availability and population characteristics). Given the unique features of rural settings, involving community members in the conduct and translation of research is critical to generating local evidence, developing context-specific interventions, and creating sustainable health outcomes. CBPR, a collaborative method that engages community partners as equitable contributors in all stages of the research process,9,10 is the prevailing paradigm to reduce disparities associated with the social determinants of health (e.g., the physical, social, and economic factors present where an individual lives).11–13
In 2011, the Lincoln County Community Health Improvement Partnership (CHIP) and three other CHIPs (Figure 1), partnered with the Oregon Rural Practice-based Research Network (ORPRN), a component of the Community and Practice Program of the Oregon Clinical and Translational Research Institute (OCTRI), on a CTSA community-engagement supplement to build a foundation for bi-directional research partnerships to address rural health disparities. This article highlights the experiences and lessons learned community (JYL, NK, AH, JKS) and academic (NR, SA, PM, MMD) partners as we transformed the Lincoln County CHIP into a Community Health Improvement and Research Partnership (CHIRP). Analysis of the CHIP to CHIRP transition across all four rural counties is described elsewhere.14
Figure 1.
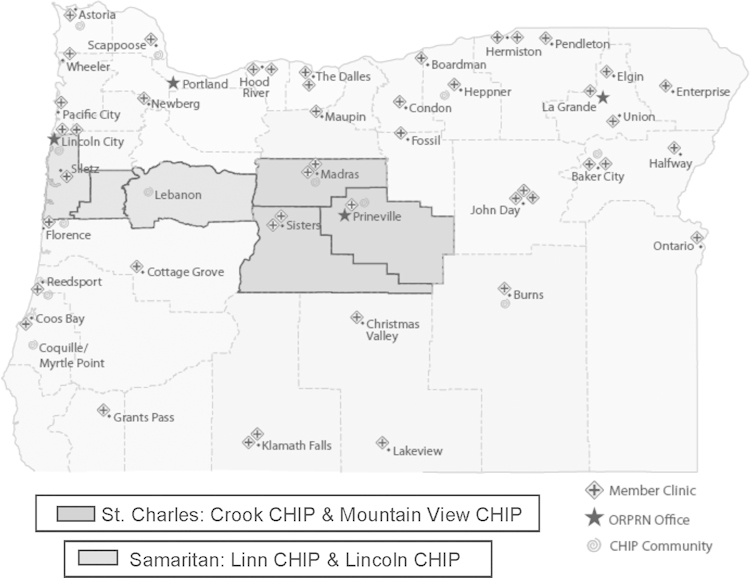
Participating CHIP to CHIRP regions and ORPRN member clinics.
CHIP
CHIP is a community development process that engages rural community members in developing solutions to improve local health care systems and the health status of area residents.15 The CHIP model has been successfully implemented in more than 100 communities in the United States, including 12 in rural Oregon.16 In Oregon, CHIP is often a collaboration between local hospitals and the Oregon Office of Rural Health; this allows hiring a local coordinator to lead the initiative in each community.
CHIP membership is diverse, frequently representing the socioeconomic and demographic composition of each community. Through a facilitated community health assessment process that involves reviewing county demographic, health status, and health utilization data, and conducting key informant interviews, residents identify local needs and priorities. 15 Priorities identified by CHIPs in Oregon have included building environments to support healthy communities; improving access to services for chronic disease management; facilitating access to services for oral, medical, and mental health needs; and addressing obesity.17 CHIP members actively work to identify and implement strategies to address these health disparities, such as building community gardens, developing safe routes to school, operating cancer support groups, supporting prescription assistance programs, and coordinating dental outreach services. CHIP engages citizens as active participants in decisions that affect their communities and provides a strong foundation for community-based participatory research (CBPR).9,16,18
From CHIP to CHIRP
In 2007 Mr. McGinnis, an ORPRN staff member with more than 30 years of experience supporting rural community health development, began integrating research training into one CHIP to transition it into CHIRP.16 The CHIRP model provides brief, facilitated research training and supports pilot research studies addressing a locally identified health concern. As Figure 2 demonstrates, CHIRP is designed to establish a foundation for collaborative research across various topics, community health segments, and methods.
Figure 2.
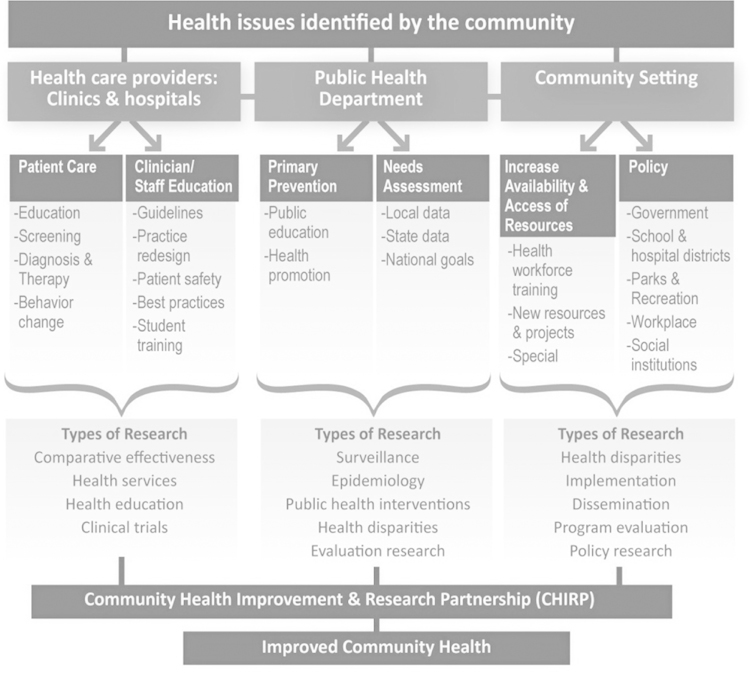
Adding research to the CHIP model—CHIP to CHIRP.
Adapted from McGinnis et al.16
In the current study, financial resources supported engagement by regional health system leadership; time for the CHIP to CHIRP coordinator to plan with the academic partners, coordinate local meetings, and manage the pilot study; and pilot study activities. Nine research training sessions were offered to CHIP to CHIRP participants, covering Research 101, Research Methods, Developing a Pilot Study (Part 1 and 2), Literature Review, Protection of Human Subjects, Implementing a Research Project, Analyzing and Interpreting Research Data, and Grant Writing Tips (Table 1).14 Popular titles described each training session, such as “Beyond Google/Mind the Gap” for Conducting a Literature Review and “Where’s the Map?!” for Implementing a Research Project. Adult learning principles and opportunities for local reflection were built into each session. Pilot research activities focused on childhood obesity, a health concern identified by all four CHIPs, including Lincoln County (the Oregon childhood obesity rate is 26.8%; the Lincoln County childhood obesity rate is 28.9%).19
Table 1.
Lincoln County CHIP to CHIRP Community Participants, Sessions Attended
|
Research Training Sessions
|
Pilot Study Sessions
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Organization | Pre-Assessment Survey and Interview | Research 101 | Types and Selection of Research Methods | Part 1. Developing a Pilot Project | Conducting a Literature Review | Protection of Human Subjects and the IRBa | Part 2. Developing a Pilot | Implementing a Research Project | Analyzing and Interpreting Data | Grant Writing Tipsa | Planning 1 | Planning 2 | Analysis and Debrief | Post Assessment |
| Samaritan Health Servicesb,c,d | × | × | × | × | × | × | × | × | × | × | × | × | × | × |
| County Health & Human Servicesb,c,d | × | × | × | × | × | × | × | × | × | × | × | × | ||
| County Commission on Children & | × | × | × | × | × | × | × | × | × | × | × | × | ||
| Familiesb,c,d | ||||||||||||||
| Community Member | × | × | × | × | × | × | × | × | × | × | × | × | × | × |
| Community Member | × | × | × | × | × | × | × | × | × | × | × | × | × | |
| Oregon Pacific AHEC | × | × | × | × | × | × | × | × | × | × | × | |||
| Oregon Pacific AHEC | × | × | × | × | × | × | × | × | × | × | × | × | × | × |
| Pacific Communities Health District | × | × | × | × | × | × | × | × | × | × | × | × | × | |
| Foundationb,c | ||||||||||||||
| Community Memberb,c,d | × | × | × | × | × | × | × | × | × | × | × | × | × | × |
| County Health & Human Services | × | × | × | × | × | × | × | |||||||
| Community Member | × | × | × | |||||||||||
| Participation Rate (%) | 100.0 | 90.9 | 90.9 | 90.9 | 90.9 | 63.6 | 90.9 | 81.8 | 81.8 | 72.7 | 72.7 | 72.7 | 63.6 | 81.8 |
AHEC, Area Health Education Centers.
Session offered via webinar and available online
Part of Childhood Obesity Partnership before CHIP to CHIRP.
Attended local, pre-intervention CHIP to CHIRP Buy-in Meeting.
Attended CHIP to CHIRP Kick Off Symposium at Oregon Health & Science University (OHSU).
Case Study: Lincoln County CHIP To CHIRP
Lincoln County spans 980 square miles with a population of 46,034.20 Historically, residents have relied on a resource-based economy involving commercial fisheries and logging
but, owing to measurable declines in recent years, they are becoming increasingly dependent upon the tourism industry. These economic challenges are reflected in the 8.8% unemployment rate (Oregon average is 8.6%)21 and median household income of $39,738 (Oregon average is $49,260).20 Overall, 16.2% of Lincoln County residents are living below the federal poverty level, although the rate is higher in specific areas of the county, such as Lincoln City (23%).20 Key socioeconomic and health indicators for Lincoln County and Oregon are summarized in Table 2.
Table 2.
Socioeconomic and Health Status Indicators for Oregon and Lincoln County
| Indicators | Lincoln County | Oregon |
|---|---|---|
| Crude death ratea | 12.1 | 8.3 |
| Heart disease | 121.0 | 162.8 |
| Cancer | 138.0 | 195.4 |
| Stroke | 31.0 | 49.7 |
| Diabetes | 10.0 | 28.0 |
| Preventive risk factors (%)b | ||
| Smoke | 15.9% | 17.1% |
| High blood pressure | 16.9% | 25.8% |
| High cholesterol | 20.2% | 33.0% |
| Obesity and health behaviors (%) | ||
| Obese | 26.2% | 24.5% |
| Overweight | 37.2% | 36.1% |
| Meeting CDC physical activity recommendations | 55.7% | 55.8% |
| Consuming ≥5 servings of fruits/veggies daily | 25.6% | 27.0% |
| Socioeconomicsc | ||
| Population, 2010 | 46,034 | 3,831,074 |
| Persons per square mile, 2010 | 47 | 40 |
| Hispanic or Latino, 2011 | 8.1% | 12.0% |
| Median household income 2006–2010 | $39,738 | $49,260 |
| At or below poverty level, 2006–2010 | 16.2% | 14.0% |
| Unemployment rated | 8.8% | 8.6% |
| Food Stamps (SNAP)e | 24.8% | 20.4% |
| Free/reduced lunch6 | 62.9% | 52.0% |
Oregon Department of Human Services, Office of Disease Prevention and Epidemiology, Center for Health Statistics and Vital Records 2009. Crude death rate is per 1,000 population otherwise data are per 100,000 population.
Oregon Department of Human Services, Center for Health Statistics, 2006–2009 Adult BRFSS Survey. Values reported are age adjusted.
United States Census Bureau State and County QuickFacts.
WorkSource, Oregon. Unemployment Rate Chart (2012).
Oregon County Monitor. Oregon State University (August 2011).
Oregon Department of Education, Statistics and Reports, School Finance Data and Analysis 2010–2011.
The Lincoln County CHIP was established in 2003 as a collaboration between the Oregon Office of Rural Health and Samaritan Health Services.17 Membership includes representatives from public health, primary care, and local government as well as educators, retired citizens, and engaged parents. The Lincoln County CHIP has identified diverse priority areas for the community (e.g., oral health, chronic disease, childhood obesity). Members of the Childhood Obesity Partnership coalition, a CHIP sub-committee, were invited to collaborate in CHIRP.
As summarized in Table 1, five CHIRP participants were Childhood Obesity Partnership members and six individuals were recruited based on their interest and relevant work in the county. These 11 community members participated in a mixed methods study approved by the Oregon Health & Science University Institutional Review Board (IRB, #7768) to explore changes in research knowledge, self-efficacy, and trust in academic partnerships before and after CHIRP trainings. Community members were also co-investigators on a CBPR pilot study to test knowledge and shopping skills of high school students following participation in the “Shopping (Cooking) Matters Program”22 (approved by Samaritan Health Services IRB, #12-023). Israel and colleagues23,24 identified eight key principles that contribute to the success of community-based research. Table 3 links these principles to the Lincoln County CHIP to CHIRP transition and we provide additional details below.
Table 3.
Key Principles of Community-based Research and the Lincoln County CHIP to CHIRP Experience
| Key Principles | Community Perspective |
|---|---|
| Recognizes community as a unit of identity. | Academics partnered with the Lincoln County CHIP, a coalition established in 2003 that engages diverse members of the geographic area in community health development activities. |
| Builds on strengths and resources within the community. |
Lincoln County CHIP membership includes representatives from diverse socioeconomic and demographic segments of the community.
Coalition members and their local connections brought personal strengths and resources to the project; the pilot study would not have been feasible without existing connections at the high school. |
| Facilitates collaborative, equitable partnerships in all phases of the research. |
Research training modules were delivered at times convenient to our partnership and tailored based on participant feedback.
Coalition members identified 21 options for the pilot study and a consensus process was used to select a research question. Members provided input at each stage of the pilot study – helping design, implement, interpret, and disseminate results. |
| Promotes co-learning and capacity building among all partners. |
ORPRN partners collaborated with coalition leadership to facilitate meetings. Many coalition members considered the research training as professional development.
Academic partners spent time attending CHIP meetings and other local events to learn about regional interests and support future academic-community matches. |
| Integrates and achieves a balance between research and action for the mutual benefit of all partners. |
Coupling CHIP with CHIRP allowed community partners to continue pursuing action-oriented interventions while simultaneously engaging in a novel research effort to improve teen shopping habits.
Study findings were used to inform local school policies (e.g., shared with teachers and high school leadership) and the experience was used to refine future data collection efforts. |
| Emphasizes local relevance of public health problems and ecological perspectives that recognize and attend to the multiple determinants of health. |
The research training modules emphasized the social ecological model of health (e.g., individuals are nested in families, nested in communities that are embedded in a larger society). This focus was used to frame data analysis and development of the community pilot project.
Community members addressed critical local concerns (childhood obesity) while developing the language and resources to communicate with academic partners around other areas of potential interest. |
| Involves systems development through a cyclical and iterative process. |
The CHIP to CHIRP transition was iterative. Research modules built upon each other and were refined with input from the four community coalitions.
Trainings fostered collaborative discussions among participants, allowing community members to shape all phases of the research process. |
| Disseminates findings and knowledge gained to all partners and involves all partners in the dissemination process. |
The research training informed many other projects being undertaken by the Lincoln County CHIP.
Coalition members shared their experiences and findings from the pilot project with other community partners and in public meetings. Coalition members helped refine the overall CHIP to CHIRP process and actively contributed to the planning, preparation, and editing of this manuscript. |
Research Training
The CHIRP research training included a Kick-off event at OHSU and a series of meetings in the local community.14 The Kick-off meeting included presentations by experts in obesity research, a campus research tour, and an afternoon symposium exploring best practices for academic–community research partnerships in rural areas.14,25 Over the next several
months, seven of the nine research training sessions were offered locally, and two were available via live streaming on the Internet. The 11 Lincoln County CHIP to CHIRP members attended 80.8% of the research training sessions on average; four partners attended all training sessions and one partner only attended two (Table 1). Nine community partners completed the post-assessment survey. Both partners unable to complete the post-assessment survey reported priority changes at work; one had been asked to focus on patient care and another transitioned to a new job.
Pilot Study
Concurrent with the research training, CHIP to CHIRP members worked with their academic partners to develop, design, and implement a pilot research study that addressed childhood obesity. Research training sessions provided opportunities for community partners to co-create the pilot study. “Designing a Pilot Study Part 1” summarized current research literature on childhood obesity interventions and “Conducting a Literature Search” allowed community partners to explore areas of personal interest. After learning to develop Population/Patient Problem, Intervention, Comparison, and Outcome (PICO) statements, a method used to help formulate questions and facilitate the literature search in evidence-based medicine, partners submitted 21 pilot research ideas for consideration.26 In light of the grant timeline (12 months) and pilot study budget of $11,250, CHIRP members used a consensus process to review and assess the PICO statements for feasibility, and then selected the topic during “Designing a Pilot Study Part 2.”
We designed the pilot study to measure the understanding of nutrition labels and shopping patterns in high school students before and after participation in the “Shopping (Cooking) Matters Program.”22 In partnership with ORPRN investigators and the research director at Samaritan Health Services, CHIRP members refined the research question and developed the IRB application, including study protocols and assessment tools (e.g., observation templates and data collection forms for evaluating quality and cost of purchases). Additionally, we enlisted the assistance of two public health students (undergraduate and graduate) from Oregon State University who helped with data collection and analysis. Coalition members working closely with the high school were also able to recruit a student to inform study design and recruitment. Each CHIRP member involved in pilot study data collection participated in the Collaborative Institutional Training Initiative, the human subjects training required by the Samaritan Health Services IRB. Results from the pilot study suggested that the program increased high school students’ nutritional knowledge. However, the improved understanding of nutrition and healthy dietary choices did not change student’s motivation to purchase unhealthy food. Findings suggested that factors other than knowledge are needed for effective interventions. The study also helped to identify the lack of nutritional programs targeting school-age children in Lincoln County.
Community Perspectives and Lessons Learned
Three methods were used to gather community member perspectives on the CHIP to CHIRP transition. CHIRP members participated in a facilitated debriefing during the final 2-hour group meeting and field notes were taken by the academic partners, the CHIP to CHIRP coordinator conducted an exit survey of members over email, and the post-assessment included open-ended questions evaluating the experience. We used an immersion/crystallization approach to analyze data.27 Community partners (JYL, NK, AH, JKS) reviewed data from the exit survey and prepared an initial list of lessons learned. Academic partners (NR, SA, PM, MMD) reviewed field notes from the debriefing meeting and responses on the post-assessment; then, two authors (JYL, MMD) met to refine the list. Key lessons learned from the community are highlighted below.
CHIRP members enjoyed the research training, but wanted more time and reinforcement. Overall, community members believed that they obtained a good understanding of translational research and the goals of CBPR by participating in the training modules and interacting with academic partners. One community partner stated, “Prior to this experience, I did not know anything about CBPR. Now I have a better understanding of the goals and the outcomes and benefits to a community participating in CBPR.” Community members indicated that the trainings raised their awareness to new factors in the community influencing childhood obesity.
However, community members wanted more time to complete the research training and to design and implement their pilot study. Some community members struggled to see the connection between the training sessions and the pilot study. Others noted that the material covered was unfamiliar and complicated, and too much time in between sessions made the information difficult to retain. One coalition member commented that, “The training modules need to be closer together in time and longer in length . . . it was too much to absorb in such short timeframes . . . so a month later, much of what I learned was gone.” Another noted, “This is a long-term process and inevitably grant funding, project prioritization, and the challenges of sustaining focus rarely support the 3–5 year span needed to actually yield a community group equipped with research tools that can be applied to addressing community concerns.”
Balancing project resources with coalition interests required tradeoffs; CHIRP members desired a community-versus a county-level focus. One of the first challenges for the coalition was narrowing down an ambitious research agenda to one that was feasible but still answered questions important to the community. Although a consensus process was used to review pilot study suggestions, it was difficult to reach agreement on a specific question. A couple of community members lost interest when their questions were not selected; this contributed to partner attrition.
Although CHIP initiatives in Lincoln County have traditionally been countywide, this pilot study engaged one school in one community. Coalition members commented on the importance of focusing at the community level. A community partner stated, “One disadvantage [of this project] was that Lincoln County was treated as a single unit, but those of us who live here see our communities as distinct.” Coalition members noted that, although many of the issues faced by individual communities may be similar in scope, the strategies to address these challenges are likely to vary based on resources and local interest. Another community member commented, “I would participate again if the projects were community-based rather than countywide.”
Community-based infrastructure was essential for coordinating the CHIP to CHIRP transition. Grant resources were allocated so the CHIP coordinator could help to plan meetings and debrief with the academic partners. Although this was adequate to support the research training requirements, the CHIRP was not as prepared for the time-intensive attention to detail required when conducting research. Fortunately, CHIRP leadership secured assistance from two university interns who provided additional research support. Applying resources from the pilot study budget to provide time for these interns was critical to achieving our goals within the project timeline.
Author Reflections
Our author team noted a few key challenges and facilitators as the group transitioned from CHIP to CHIRP in Lincoln County. Securing time for activities was identified as a notable challenge by academic and community partners, a common finding in CBPR.24,28–31 Partners would have benefitted from having additional time to accomplish the study objectives (e.g., 24 versus 12 months). Delivering research training during a consecutive block of time (e.g., 2-day retreat), which other CTSA and academic partners recommend,32,33 may have reduced the travel burden and allowed more time for the pilot study and facilitating other research collaborations. However, this change could potentially make it more difficult for community partners to retain the new information or attend owing to their other work obligations.
Defining the community and maintaining healthy interpersonal dynamics also emerged as challenges. Although previous CHIP projects focused on the county level, CHIRP members noted the importance of focusing research activities on individual communities. Additionally, although CHIP to CHIRP members agreed on a joint vision that addressed reducing childhood obesity, occasionally interpersonal challenges emerged between community partners, such as when discussing the feasibility of the PICO statements. Other small conflicts emerged around how to allocate the pilot study resources in a way that would be the most equitable for community partners. Previous studies emphasize the importance of negotiating academic and community dynamics34–36; in our experience, attending to internal community relations is also critical.
We also note various facilitators of this partnership. First, this collaboration built on existing infrastructure in the community and academic setting (e.g., Lincoln County CHIP; ORPRN and OCTRI staff). Partners submitted the original CTSA supplement application with a keen awareness that accomplishing the project goals in the time allotted was only conceivable because of existing relationships. Drawing on the CHIP infrastructure allowed communities to solve problems using traditional community health development processes while concurrently exploring research opportunities.16 Further more, the affiliation between ORPRN staff and the local CTSA allows academic partners to continue engaging with community partners beyond this individual project period. Although lack of trust and respect is often identified as a challenge in developing partnerships,24 our history of collaboration and focus on the community-identified need of childhood obesity averted these tensions.
Additionally, collaborative development of the grant proposal allowed partners to allocate resources to support local leadership in ways that equitably distributed power and control.24,36 The involvement of highly receptive, engaged community partners, as evidenced by attendance in trainings and low attrition rates, was also a key factor in project success. Support from the regional health system, which helped to secure student interns, assist with the local IRB application, and provide leadership support for coalition activities, was also instrumental.
CBPR projects build community capacity over time.37,38 The authors note that the CHIP to CHIRP transition is one step in building collaborative, bidirectional research partnerships. Because CBPR is often considered a process rather than an individual project, this work establishes a foundation in Lincoln County. Lincoln County CHIRP members expressed desire to pursue future CBPR opportunities if the research area was of interest, the resources and timeline were adequate, and the academic partner demonstrated a commitment to the community’s needs.
Acknowledgments
The authors thank our colleagues from the Lincoln, East Linn, Jefferson (Mountain View), and Crook County CHIPs who participated in this collaborative project. Michelle Thomas, MSW, and Molly DeSordi assisted with data collection; and David Buckley, MD, MPH, and Lyle J. Fagnan, MD, informed the overall project vision. We are grateful to LeNeva Spires for her editorial assistance.
References
Clinical, and Translational Science Award (CTSA) Consortium’s Community Engagement Key Function Committee. Researchers and their communities: The challenges for meaningful community engagement [updated 2009]. Available from: http://www.ctsaweb.org/index.cfm?fuseaction=committee.viewCommittee&com_ID=3&abbr=CEKFC
Westfall JM, Mold J, Fagnan L. Practice-based research – “Blue Highways” on the NIH Roadmap. JAMA. 2007;297:403–406. doi: 10.1001/jama.297.4.403.
DeNavas-Walt C, Proctor BC, Smith JC. U.S. Census Bureau. Current population reports, P60-235, income, poverty, and health insurance coverage in the United States: 2007. Washington (DC): U.S. Government Printing Office; 2008.
Bennett KJ, Olatosi B, Probst JC. Health disparities: A rural–urban chartbook. Columbia: South Carolina Rural Health Research Center; 2008.
Tai-Seale T, Chandler C. Nutrition and overweight concerns in rural areas: A literature reviewRural healthy people 2010: A companion document to healthy people 2010 College Station: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003.
Jackson JE, Doescher MP, Jerant AF, Hart LG. A national study of obesity prevalence and trends by type of rural county. J Rural Health. 2005;21:140–148. doi: 10.1111/j.1748-0361.2005.tb00074.x.
Patterson PD, Moore CG, Probst JC, Shinogle JA. Obesity and physical inactivity in rural America. J Rural Health. 2004;20:151–159. doi: 10.1111/j.1748-0361.2004.tb00022.x.
Liu J, Bennett KJ, Harun N, Zheng X, Probst JC, Pate RR. Overweight and physical inactivity among rural children aged 10–17: A national and state portrait [updated 2007; cited 2010 Jun 1]. Available from: http://rhr.sph.sc.edu/report/SCRHRC_ObesityChartbook_Exec_Sum_1015.07.pdf
Israel B, Eugenia E, Schulz A, Parker E, editors. Methods in commu nity-based participatory research for health. San Francisco: Jossey-Bass; 2005.
Norris KC, Bruseulas R, Jones L, Miranda J, Duru OK, Mangion CM. Partnering with community-based organizations: A n academic institution’s evolving perspective. Ethn Dis. 2007;17(Suppl 1):S27–S32.
Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA. 2007;297:407–410. doi: 10.1001/jama.297.4.407.
Giachello AL, Arrom JO, Davis M, Sayad JV, Ramirez D, Nandi C, et al. Reducing diabetes health disparities through community-based participatory action research: The Chicago Southeast Diabetes Community Action Coalition. Public Health Rep. 2003;118:309–323. doi: 10.1016/S0033-3549(04)50255-8.
Krieger J, Allen C, Cheadle A, Ciske S, Schier JK, Senturia K, et al. Using community-based participatory research to address social determinants of health: Lessons learned from Seattle Partners for Healthy Communities. Health Educ Behav. 2002;29:361–382. doi: 10.1177/109019810202900307.
Davis MM, Aromaa S, McGinnis P, et al. Strengthening foundations: A process model to mobilize rural community health coalitions and academicians in research partnerships.
McGinnis P, Przybilla J. Community Health Improvement Partnership: A rural community health development process [updated 1999; cited 2010 Jun 8]. Available from: http://www.ohsu.edu/research/orprn/resources/community.html
McGinnis PB, Hunsberger M, Davis M, Smith J, Beamer BA, Hastings DD. Transitioning from CHIP to CHIRP: Blending community health development with community-based participatory research. Fam Community Health. 2010;33:228–237. doi: 10.1097/FCH.0b013e3181e4bc8e.
Samaritan Health Services. Community Health Improvement Partnerships: Lincoln County, East Linn County [updated 2012; cited 2012 Nov 20]. Available from: http://www.sam-health.org/communitysupport/communitycollaborations/Pages/communityhealthimprovementpartnerships.aspx
Fehren O. Who organises the community? The university as an intermediary actor. Gateways: International Journal of Community Research and Engagement. 2010;3:104–119.
Children First for Oregon . Status of Oregon’s children county data book, 2010. Portland: Author; 2010.
United States Census Bureau. State & county quickfacts [cited 2012 Aug 1]. Available from: http://quickfacts.census.gov/qfd/index.html
WorkSource Oregon. Unemployment rate chart [cited 2012 Aug 1]. Available from: http://www.qualityinfo.org/olmisj/OlmisZine?zineid=00000011
Share Our Strength. Cooking matters: No kid hungry [cited 2012 Aug 1]. Available from: http://cookingmatters.org
Israel B, Schulz AJ, Parker EA, Becker AB, Allen AJ, III , Guzman JR. Crucial issues in developing and following community based participatory research principles. In: Minkler M, Wallerstein N, editors. Community-based participatory research for health. San Francisco: Jossey-Bass; 2003.
Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173.
Academic/Community Research Partnerships Symposium [updated 2011; cited 2012 Aug 15]. Available from: http://www.ohsu.edu/xd/outreach/oregon-rural-health/hospitals/chip/creed-symposium.cfm
Schardt C, Adams MB, Owens T, Keitz S, Fontelo p. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7:16. doi: 10.1186/1472-6947-7-16.
Borkan J. Immersion/crystallization. In: Crabtree BF, Miller WL, editors. doing qualitative research. 2nd ed. Thousand Oaks (CA): Sage; 1999. pp. 179–194.
Israel BA, Krieger J, Vlahov D, Ciske S, Foley M, Fortin P, et al. Challenges and facilitating factors in sustaining community-based participatory research partnerships: Lessons learned from the Detroit, New York City and Seattle Urban Research Centers. J Urban Health. 2006;83:1022–1040. doi: 10.1007/s11524-006-9110-1.
Israel BA, Parker EA, Rowe Z, Salvatore A, Minkler M, López J, et al. Community-based participatory research: Lessons learned from the Centers for Children’s Environmental Health and Disease Prevention Research. Environ Health Perspect. 2005;113:1463–1471. doi: 10.1289/ehp.7675.
Israel BA, Eng E, Schultz AJ, Parker EA, editors. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2005.
Minkler M, Wallerstein N. Community-based participatory research for health: From process to outcomes. San Francisco: Jossey-Bass; 2008.
Allen ML, Culhane-Pera K, Call KT, Pergament S. Partners in research: Curricula to prepare community and faculty for CBPR partnerships [updated 2011; cited 2012 Nov19]. Available from: http://www.healthdisparities.umn.edu/news/training/home.html
Rocky Mountain Prevention Research Center. Workshops/custom training: Community-based participatory research [updated 2012; cited 2012 Nov 19]. Available from: http://www.ucdenver.edu/academics/colleges/PublicHealth/research/centers/RMPRC/training/Pages/CBPR.aspx
Freeman ER, Brugge D, Bennett-Bradley WM, Levy JI, Carrasco ER. Challenges of conducting community-based participatory research in Boston’s neighborhoods to reduce disparities in asthma. J Urban Health. 2006;83:1013–1021. doi: 10.1007/s11524-006-9111-0.
Shoultz J, Oneha MF, Magnussen L, Hla MM, Brees-Saunders Z, Cruz MD, et al. Finding solutions to challenges faced in community-based participatory research between academic and community organizations. J Interprof Care. 2006;20:133–144. doi: 10.1080/13561820600577576.
Lazarus S, Duran B, Caldwell L. Public health research and action: Reflections on challenges and possibilities of community-based participatory research. In: Maddock J, editor. public health: Social and behavioral health. New York: InTech; 2012. pp. 309–324.
Jagosh J, Macaulay AC, Pluye P, Salsberg J, Bush PL, Henderson J, et al. Uncovering the benefits of participatory research: Implications of a realist review for health research and practice. Milbank Q. 2012;90:311–346. doi: 10.1111/j.1468-0009.2012.00665.x.
Buchanan DR, Miller FG, Wallerstein N. Ethical issues in community-based participatory research: Balancing rigorous research with community participation in community intervention studies. Prog Community Health Partnersh. 2007;1:153–160. doi: 10.1353/cpr.2007.0006.
Contributor Information
Julia Young-Lorion, Lincoln County Community Health Improvement Partnership; Center for Health Research and Quality, Samaritan Health Services.
Melinda M. Davis, Oregon Rural Practice-based Research Network, Oregon Health & Science University; Department of Family Medicine, Oregon Health & Science University.
Nancy Kirks, East Linn Community Health Improvement Partnership.
Anna Hsu, School of Biological and Population Health Sciences, Oregon State University.
Susan Aromaa, Oregon Clinical and Translational Research Institute, Oregon Health & Science University.


