Abstract
Background
Limited information is available about relatively contemporary trends in the incidence and hospital case-fatality rates (CFRs) of cardiogenic shock in patients hospitalized with acute myocardial infarction (AMI).The purpose of this population-based study was to describe decade long trends (2001-2011) in the incidence and hospital CFRs for patients who developed cardiogenic shock during hospitalization for an AMI.
Methods and Results
The study population consisted of 5,686 residents of central MA hospitalized with AMI at all 11 medical centers in the Worcester, MA, metropolitan area during six biennial periods between 2001 and 2011, who did not have cardiogenic shock at the time of hospital presentation. On average, 3.7% of these patients developed cardiogenic shock during their acute hospitalization with nonsignificant and inconsistent trends noted over time in both crude (3.7% in 2001/2003; 4.5% in 2005/2007; 2.7% in 2009/2011; p=0.19) and multivariable adjusted analyses. The overall in-hospital CFR for patients who developed cardiogenic shock was 41.4 %. The crude and multivariable adjusted odds of dying after cardiogenic shock declined during the most recent study years (47.1% dying in 2001/2003, 42.0% dying in 2005/2007, and 28.6% dying in 2009/2011). Increases in the use of evidence-based cardiac medications and interventional procedures paralleled the increasing hospital survival trends.
Conclusions
We found suggestions of a decline in the death, but not incidence, rates of cardiogenic shock over time. These encouraging trends in hospital survival are likely due to advances in the early recognition and aggressive management of patients who develop cardiogenic shock.
Keywords: cardiogenic shock, acute myocardial infarction, population-based epidemiological study
Cardiogenic shock is a devastating complication of acute myocardial infarction (AMI) and remains the most common cause of mortality in patients hospitalized with AMI 1-4. Early and aggressive revascularization for cardiogenic shock in the setting of AMI, in conjunction with the use of mechanical approaches to counter left ventricular pump failure in cardiogenic shock, has been shown to improve the short-term survival of these high risk patients 4-6. However, these and other recent advances in the management of patients hospitalized with AMI do not appear to have had a uniformly positive impact on the prognosis of patients who develop cardiogenic shock, since nearly half of those who experience this clinical complication continue to die during their acute hospitalization 3, 4, 7, 8. A limited number of randomized trials and population-based studies have shown slight declines in the incidence and short- term mortality associated with cardiogenic shock during the past two decades 9-11, whereas other studies have failed to observe declines in either the frequency of cardiogenic shock complicating AMI or improvements in its short-term survival 12.
In several prior publications from our population-based coronary disease surveillance system, we have described trends in the incidence and in-hospital death rates associated with cardiogenic shock in residents of central Massachusetts who were hospitalized at all area medical centers with confirmed AMI 1-3. The purpose of the present study was to provide a relatively contemporary perspective into decade long trends (2001-2011) in the incidence and hospital case-fatality rates associated with cardiogenic shock developing during hospitalization for AMI from the more generalizable perspective of a community-wide investigation.
Methods
The study population consisted of residents of the Worcester, MA, metropolitan area hospitalized with a discharge diagnosis of AMI and related coronary disease rubrics at all 11 teaching and community hospitals in central Massachusetts during six biennial study years between 2001 and 2011. These years were selected due to the availability of federal funding support and design features of this investigation; we have carried out surveillance for AMI in the central MA population on an approximate biennial basis since the inception of this population-based investigation 13-17.
The details of this study have been previously published 13-17. In brief, potentially eligible patients who were hospitalized for acute coronary disease and related disease rubrics were identified through the review of computerized hospital databases of patients with International Classification of Disease discharge diagnoses consistent with the possible presence of AMI. The medical records of all potentially eligible patients, who had to be residents of central Massachusetts since this study is population-based, were reviewed in a standardized manner and the diagnosis of AMI was confirmed according to pre-established criteria that have been previously described 13-17.
Cardiogenic shock was defined as a systolic blood pressure of less than 80 mm Hg in the absence of hypovolemia and associated with cyanosis, cold extremities, changes in mental status, persistent oliguria, or congestive heart failure as recorded in hospital medical records 1-3. The definition of cardiogenic shock remained the same during all periods studied. This disorder was defined so that patients with classic signs and symptoms of this clinical syndrome would be included. Data on cardiac index or left ventricular ejection fraction findings were, however, not included as part of our working definition for cardiogenic shock in this study. Among the 5,782 patients with confirmed AMI during the years under study, 96 were excluded due to the presence of cardiogenic shock at the time of hospital presentation.
Information was abstracted from the hospital medical records of greater Worcester residents with independently validated AMI by trained nurse and physician reviewers. Information was collected with regards to patient's baseline demographic characteristics, medical history, clinical findings, and hospital management practices, including the use of cardiac medications and specialized cardiac diagnostic and interventional procedures as these therapies became available in clinical practice.
Data Analysis
Changes over time in patient's demographic and clinical characteristics and hospital treatment practices were examined using chi square tests for trends. Decade long trends in the hospital incidence and case-fatality rates (CFRs) of cardiogenic shock were assessed using similar analytic methods. For ease of analysis and interpretation, we aggregated the six individual study years into 3 two year periods, namely 2001/2003, 2005/2007, and 2009/2011. In addition, we examined trends in the hospital incidence and CFRs of this study population subdividing those hospitalized in the initial three of the six years under study (2001, 2003, and 2005) as compared with those hospitalized during the latter three periods under investigation (2007, 2009, and 2011). Logistic regression models were used to examine trends in the multivariable adjusted odds ratios for developing cardiogenic shock during the patient's index hospitalization, and their corresponding hospital CFRs during the period under study, while controlling for several potentially confounding demographic and clinical factors of prognostic importance. The variables controlled for in our regression models were included either because they differed between our respective comparison groups at a p value of <0.25 or because they had been previously shown to be possible risk or prognostic factors for cardiogenic shock.
Human subjects approval for this coronary disease surveillance project was obtained from the Committee for the Protection of Human Subjects in Research at the University of Massachusetts Medical School.
Results
Study Population Characteristics
A total of 5,686 patients were hospitalized with independently confirmed AMI at all 11 medical centers in central Massachusetts during six biennial periods between 2001 and 2011, who did not have cardiogenic shock at the time of hospital presentation. The mean age of this patient population was 69.9 years, 56.7% were men, 89.7% were Caucasian, and for 64.5% it was their first AMI.
Patients who were admitted for AMI during the most recent study years were more likely to be younger, Caucasian, and obese but were less likely to have do not resuscitate orders at the time of hospital admission and to be transported to area hospitals by ambulance, compared with those from earlier study years (Table 1). Patients admitted during the most recent years under study were more likely to have previously undergone a percutaneous coronary intervention (PCI) and had a greater prevalence of several chronic co-morbidities. Patients who were admitted to all central Massachusetts medical centers during recent years were less likely to have developed many of the complications examined during their index hospitalization, in comparison with those hospitalized during earlier study years (Table 1).
Table 1. Characteristics of Patients Hospitalized with Acute Myocardial Infarction.
| Total population | 2001/2003 | 2005/2007 | 2009/2011 | p value for trend | |
|---|---|---|---|---|---|
| Characteristic | (n=5,686) | (n=2,357) | (n=1,783) | (n=1,546) | |
| Age (mean, years) | 69.9 | 71.6 | 70.4 | 66.6 | <0.001 |
| Male (%) | 56.7 | 56.3 | 55.4 | 58.7 | 0.14 |
| Caucasian (%) | 89.7 | 88.0 | 90.9 | 92.1 | <0.001 |
| Body mass index (%) | |||||
| <25 kg/m2 | 32.7 | 34.5 | 32.3 | 30.9 | |
| 25-29.9 kg/m2 | 36.1 | 37.2 | 36.2 | 34.5 | |
| ≥30 kg/m2 | 31.2 | 28.3 | 31.5 | 34.6 | 0.004 |
| Do not resuscitate order (%) | 23.4 | 24.2 | 25.9 | 19.4 | <0.001 |
| Transported by ambulance (%) | 67.8 | 68.5 | 68.0 | 66.3 | <0.001 |
| Medical History (%) | |||||
| Angina | 14.5 | 22.3 | 12.5 | 4.9 | <0.001 |
| Diabetes | 34.8 | 32.5 | 35.4 | 37.5 | 0.005 |
| Heart failure | 23.6 | 24.0 | 25.7 | 20.7 | 0.002 |
| Hypertension | 73.9 | 70.9 | 75.8 | 76.3 | <0.001 |
| Stroke | 11.6 | 12.4 | 11.7 | 10.5 | 0.19 |
| Procedure history (%) | |||||
| PCI | 20.2 | 14.7 | 21.3 | 27.2 | <0.001 |
| CABG surgery | 13.6 | 12.5 | 13.8 | 14.9 | 0.10 |
| Presenting symptoms (%) | |||||
| Chest pain | 73.2 | 71.3 | 72.9 | 76.3 | <0.005 |
| Diaphoresis | 29.5 | 37.4 | 31.9 | 14.8 | <0.001 |
| Shortness of breath | 55.8 | 61.2 | 54.0 | 49.7 | <0.001 |
| Type of AMI (%) | |||||
| STEMI | 31.7 | 33.6 | 31.2 | 29.6 | <0.05 |
| Initial | 64.5 | 64.6 | 64.6 | 64.4 | 0.98 |
| Vital signs at hospital admission (mean) | |||||
| Systolic Blood pressure, mmHg | 141.7 | 143.0 | 142.0 | 139.3 | <0.001 |
| Diastolic blood pressure, mmHg | 77.3 | 77.3 | 77.0 | 77.5 | 0.75 |
| Heart rate, bpm | 86.0 | 86.8 | 85.8 | 84.8 | 0.02 |
| Laboratory findings at hospital admission (mean) | |||||
| Estimated GFR (1.73m2) (%) | 56.4 | 57.0 | 59.5 | 52.2 | <0.001 |
| Serum Cholesterol (mg/dl) | 170.8 | 178.9 | 166.7 | 167.1 | <0.001 |
| Serum glucose (mg/dl) | 170.8 | 172.9 | 168.8 | 169.9 | 0.22 |
| Complications experienced during hospital stay (%) | |||||
| Atrial fibrillation | 20.1 | 21.3 | 21.8 | 16.2 | <0.001 |
| Complete heart block | 1.5 | 2.3 | 1.3 | 0.5 | <0.001 |
| Heart failure | 36.5 | 39.0 | 39.2 | 29.6 | <0.001 |
| Stroke | 1.7 | 2.2 | 0.8 | 1.9 | <0.001 |
In examining differences in the baseline characteristics of patients who developed cardiogenic shock during their index hospitalization as compared with those who did not develop this serious complication (Table 2), patients who developed cardiogenic shock were significantly older, were more likely to have a do not resuscitate order in their hospital medical record, to have been transported to all central Massachusetts hospitals by ambulance, to have had diabetes previously diagnosed, were more likely to have developed a STEMI during their index hospitalization, had appreciably lower blood pressure, serum cholesterol, and estimated glomerular filtration rate findings, but higher heart rate and serum glucose values at admission, and were more likely to have developed each of the major clinical complications examined, with the exception of stroke, and died during their acute hospitalization.
Table 2. Characteristics of Patients With Acute Myocardial Infarction According to Whether They Developed Cardiogenic Shock During Hospitalization.
| In-Hospital Shock (+) | No Shock (-) | ||
|---|---|---|---|
| Characteristic | (n=210) % | (n=5,476) % | P Value % |
| Demographics | |||
| Age (mean, yrs) | 73.2 | 69.8 | <0.001 |
| Male (%) | 54.3 | 56.8 | 0.48 |
| Caucasian (%) | 89.8 | 89.7 | 0.94 |
| Body mass index >30 (%) | 25.6 | 31.4 | 0.23 |
| Do not resuscitate order (%) | 35.7 | 22.9 | <0.001 |
| Transported by ambulance (%) | 77.6 | 67.7 | <0.01 |
| Medical History (%) | |||
| Angina | 15.2 | 14.4 | 0.75 |
| Diabetes | 41.9 | 34.5 | <0.05 |
| Heart failure | 26.2 | 23.5 | 0.38 |
| Hypertension | 76.2 | 73.8 | 0.44 |
| Stroke | 8.1 | 11.8 | 0.09 |
| Procedure History (%) | |||
| PCI | 23.3 | 20.1 | 0.25 |
| CABG surgery | 14.8 | 13.5 | 0.61 |
| Presenting Symptoms (%) | |||
| Chest pain | 69.1 | 73.3 | 0.18 |
| Diaphoresis | 27.6 | 29.6 | 0.54 |
| Shortness of breath | 61.9 | 55.6 | 0.07 |
| Type of AMI | |||
| STEMI (%) | 56.2 | 30.8 | <0.001 |
| Initial MI | 61.4 | 64.7 | 0.34 |
| Vital signs at hospital admission (mean) | |||
| Systolic blood pressure (mmHg) | 123.3 | 142.4 | <0.001 |
| Diastolic blood pressure (mmHg) | 69.9 | 77.5 | <0.001 |
| Heart rate (bpm) | 89.4 | 85.8 | <0.05 |
| Laboratory findings at hospital admission (mean) | |||
| Glucose (mg/dl) | 198.5 | 169.8 | <0.001 |
| Estimated GFR (%) | 50.0 | 56.6 | <0.001 |
| Cholesterol (mg/dl) | 155.3 | 171.3 | <0.001 |
| Complications experienced during hospital stay (%) | |||
| Atrial fibrillation | 46.2 | 19.1 | <0.001 |
| Complete heart block | 4.8 | 1.4 | <0.01 |
| Heart failure | 81.4 | 34.9 | <0.001 |
| Stroke | 2.4 | 1.6 | 0.44 |
| Died | 41.4 | 7.3 | <0.001 |
Hospital treatment practices
There were considerable increases over time in the proportion of hospitalized patients who received evidence-based cardiac medications and therapeutic interventions during their index hospitalization (Table 3). Patients hospitalized during the most recent years under study were more likely to have been prescribed all evidence-based cardiac medications, including aspirin, ACE inhibitors/ARBs, beta blockers, and lipid lowering agents, but were less likely to have received calcium channel blockers. These patients were also significantly more likely to have undergone cardiac catheterization and/or a PCI (Table 3).
Table 3. Hospital management practices in patients hospitalized with acute myocardial infarction.
| Total | 2001/2003 | 2005/2007 | 2009/2011 | p value for trend | |
|---|---|---|---|---|---|
| Hospital Medications (%) | |||||
| ACE inhibitors/ARBs | 69.5 | 66.5 | 73.8 | 69.2 | <0.001 |
| Aspirin | 93.3 | 90.2 | 95.3 | 95.6 | <0.001 |
| Beta blockers | 91.6 | 87.9 | 95.1 | 93.3 | <0.001 |
| Calcium channel blockers | 23.2 | 26.2 | 21.7 | 20.31 | <0.001 |
| Lipid lowering medications | 76.7 | 66.1 | 78.8 | 90.6 | <0.001 |
| Thrombolytics | 3.3 | 7.1 | 0.9 | 0.4 | <0.001 |
| Hospital procedures (%) | |||||
| Cardiac catheterization | 61.7 | 53.1 | 66.7 | 69.0 | <0.001 |
| Coronary artery bypass graft surgery | 6.4 | 7.0 | 5.7 | 6.4 | 0.22 |
| Intra-aortic balloon counterpulsation | 5.3 | 5.0 | 6.7 | 4.2 | <0.005 |
| PCI | 43.5 | 35.0 | 49.3 | 49.7 | <0.001 |
Incidence Rates of Cardiogenic Shock
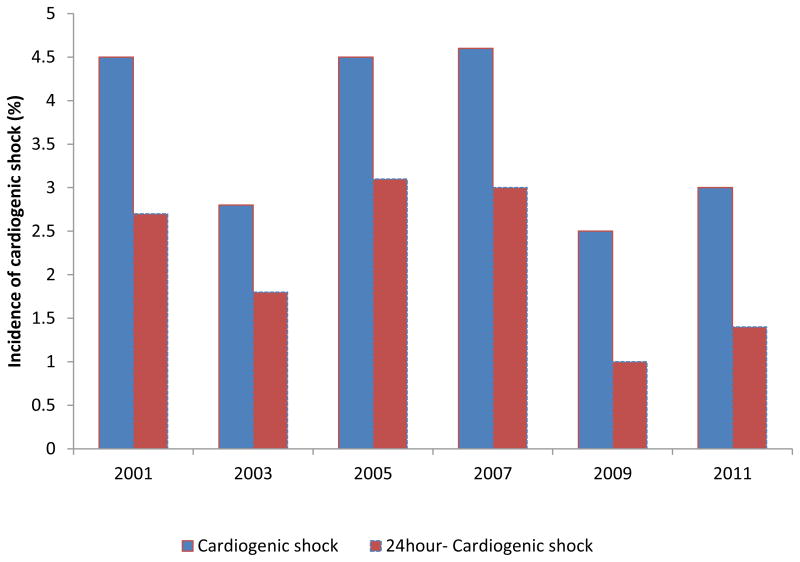
Among the 5,686 patients hospitalized with confirmed AMI during the years under study, a total of 210 (3.7%) developed cardiogenic shock after hospital admission. The crude incidence rates of in-hospital cardiogenic shock declined during the six individual years under study, albeit in an inconsistent, bimodal, and varying manner, from 4.5% in 2001 to 3.0% in 2011, with a nadir at 2.5% in 2009 (Figure 1; p for trend = 0.12). Similar nonsignificant trends were observed when we analyzed trends in the hospital incidence rates of cardiogenic shock between 2001/03 (incidence rate =3.7%), 2005/07 (4.5%), and 2009/11 (2.7%) (p = 0.19).
Figure 1. Trends in the incidence rates of cardiogenic shock in patients hospitalized with acute myocardial infarction.
A multivariable adjusted regression analysis was performed to examine the odds of developing cardiogenic shock during hospitalization for AMI while controlling for several factors of prognostic importance. The results of this analysis also did not demonstrate a decline in the multivariable adjusted odds of developing shock during the most recent years under study after controlling for several demographic and clinical factors that may have affected the risk of developing cardiogenic shock (Table 4).
Table 4.
Crude and multivariable adjusted odds ratios (OR) for developing cardiogenic shock in patients hospitalized with acute myocardial infarction
| Study Years | Crude frequency (%) | Adjusted OR (95% CI)* | Adjusted OR (95% CI )** |
|---|---|---|---|
| 2001/2003 | 3.7 | 1.0 | 1.0 |
| 2005/2007 | 4.5 | 1.27 (0.93, 1.73) | 1.42 (1.02, 1.98) |
| 2009/2011 | 2.7 | 0.76 (0.52, 1.11) | 1.03 (0.69, 1.55) |
adjusted for age and sex
adjusted for age, sex, medical history, history of cardiac procedures, type of presenting AMI, in-hospital complications, and hospital length of stay
When we examined possible changes in the hospital development of cardiogenic shock during the first half of the six years under study (2001, 2003, and 2005; n=3,250) compared with those who were hospitalized during the latter three years under investigation, namely 2007, 2009, and 2011 (n=2,436), there was a nonsignificant decline in the hospital incidence rates of cardiogenic shock from 3.9% during the early years under study to 3.4% during the three most recent study years (p=0.32). When we simultaneously adjusted for several demographic and clinical factors that could have affected the likelihood of developing cardiogenic shock, we failed to final evidence of a decline in the multivariable adjusted odds of developing cardiogenic shock during the latter three of the six years under study compared with the first three years under investigation (adjusted OR = 1.10; 95% CI = 0.81, 1.49).
Since the prompt initiation of evidence-based medications and aggressive coronary interventions for patients hospitalized with AMI could potentially prevent the development of early clinical complications, such as cardiogenic shock, we also examined trends in the frequency of cardiogenic shock during the initial 24 hours of admission for AMI. The results of this analysis showed a marked, but varying, decline in the frequency of cardiogenic shock during the initial 24 hours after hospitalization, declining from a peak of 2.7% in 2001 to a low of 1.4% in 2011 (Figure 1).
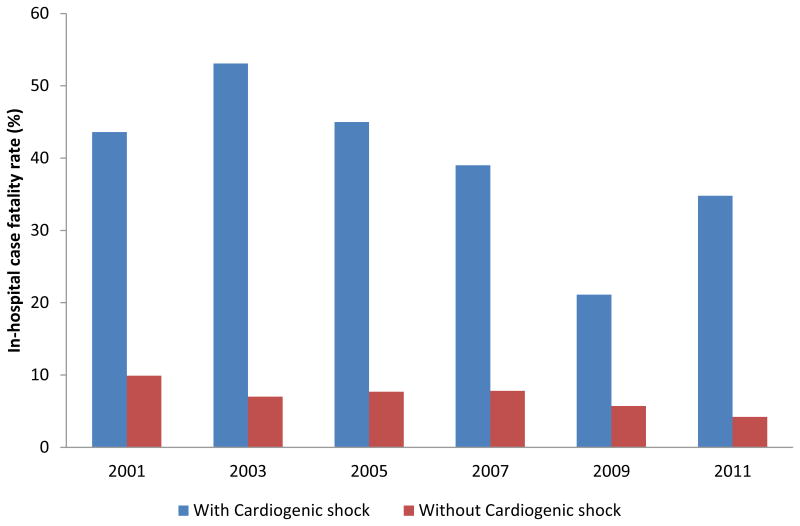
Hospital case-fatality rates
Patients who developed cardiogenic shock were at significantly greater risk for dying during their acute hospitalization compared with those who did not develop shock (41.3 % vs. 7.3 %) (p<0.001).The crude biennial hospital death rates associated with cardiogenic shock showed a non-significant decline over time from 43.6 % in 2001 to 34.8 % in 2011 (p for trend =0.31); the death rates for AMI patients who did not develop cardiogenic shock also showed a marked decline over time from 9.9% in 2001 to 4.2% in 2011 (Figure 2).
Figure 2. Trends in hospital case-fatality rates (CFRs) among patients hospitalized with acute myocardial infarction according to the presence of cardiogenic shock.
A multivariable adjusted logistic regression analysis was performed to examine trends in the odds of dying from cardiogenic shock after adjusting for several potentially confounding variables of prognostic importance (Table 5). These analyses demonstrated a significant and consistent decline in the multivariable adjusted odds of dying after cardiogenic shock during the years under study. When we carried out a similar analysis comparing patients hospitalized during the latter half of our study (2007-2011) compared with those hospitalized during the initial three years (2001-2005; referent period), we also found evidence of a multivariable adjusted decline in the odds of dying from cardiogenic shock (adjusted OR = 0.35; 95% CI = 0.16, 0.75).
Table 5. Crude and multivariable adjusted odds ratios (OR) of dying in the hospital for patients with cardiogenic shock complicating acute myocardial infarction.
| Study Years | Crude Hospital Case Fatality Rate (%) | Adjusted OR (95% CI)* | Adjusted OR (95% CI )** |
|---|---|---|---|
| 2001/2003 | 47.1 | 1.0 | 1.0 |
| 2005/2007 | 42.0 | 0.71 (0.37, 1.35) | 0.57 (0.26, 1.25) |
| 2009/2011 | 28.6 | 0.40 (0.17, 0.92) | 0.22 (0.08, 0.63) |
adjusted for age and sex
adjusted for age, sex, medical history, history of cardiac procedures, type of presenting AMI, in-hospital complications, and hospital length of stay
When we also controlled for the receipt of several evidence-based cardiac medications and in-hospital cardiac catheterization, PCI, and CABG surgery, there remained a significant decline in the multivariable adjusted odds of dying from cardiogenic shock during the most recent years under study (2005/2007: adjusted OR=1.02; 95% CI =0.37, 2.81; 2009/2011: adjusted OR=0.12; 95% CI= 0.03,0.54) compared with the referent years of 2001/03.
Discussion
The results of this population-based observational study suggest that the frequency of cardiogenic shock complicating AMI has not declined during the decade long period under study whereas the hospital death rates associated with the in-hospital development of cardiogenic shock have declined during recent years among residents of central Massachusetts hospitalized at all 11 medical centers in this large urban metropolitan area with AMI.
Patient's risk profile and hospital management practices for AMI
Multiple studies have established the implications of patient's risk profile in terms of the risk of developing and dying from cardiogenic shock in the setting of AMI 1-3, 7. For example, older patients and those with various cardiac comorbidities are known to be at particularly high risk for developing cardiogenic shock after AMI 4, 18. Our analyses showed that the population of patients hospitalized with AMI changed significantly over time with regards to many demographic and clinical factors, patterns which were necessary to adjust for in examining decade long trends in the incidence and hospital CFRs associated with cardiogenic shock. Furthermore, we presented differences in the characteristics of patients who developed, as compared with those who did not develop, cardiogenic shock during the years under study, finding differences between these two groups in a variety of demographic, medical history, clinical, and physiologic factors.
It has been repeatedly shown in previous studies that the early initiation of evidence-based medical therapies and coronary re-perfusion/ re-vascularization strategies during AMI positively influences patient's hospital course and short-term outcomes 4, 6, 19-21. The ACC/AHA guidelines for the management of AMI stress the importance of initiation of evidence-based cardiac medications and diagnostic/therapeutic cardiac procedures for optimal outcomes in patients hospitalized with AMI 20-23. Our observation of increased utilization of effective medical therapies and invasive coronary diagnostic and interventional procedures during the years under study likely contributed to the encouraging declines we observed in the short-term death rates associated with cardiogenic shock in the present study. One needs to be careful in deriving any causal inferences from these observations, however, due to the potential for confounding by treatment indication in non-randomized studies, such as ours, and that several additional confounding factors may have contributed to improved outcomes associated with different treatment practices that were not specifically examined in the context of our study.
Frequency of Cardiogenic Shock Complicating AMI
Unlike previous studies which had examined the magnitude of cardiogenic shock complicating AMI irrespective of its timing, and had noted incidence rates ranging from 5-7% during the past several decades 7, 12, 24, 25, our study examined the patterns of cardiogenic shock developing during hospitalization for AMI between 2001 and 2011, finding that nearly 4% of patients with AMI developed cardiogenic shock over this period.
The majority of previously published studies 1, 2, 8, 26, including the findings from multinational randomized trials such as the Global Utilization of Steptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO-I, 1990-1993) and the follow up study (GUSTO-III, 1995-1997) had observed relatively stable trends in the frequency of this devastating complication over the past few decades, despite significant advances in the medical management of patients hospitalized with AMI. In contrast, a limited number of international studies 10, 11, including three nationwide French registries conducted 5 years apart, observed declining trends in the incidence rates of cardiogenic shock over time (6.9% in 1995; 5.7% in 2005). There was a non-uniform decline in the incidence rates of cardiogenic shock observed in the GRACE registry from 2000 to 2005 among patients with both ST and non-ST segment elevation AMI 9.
Very few studies have, however, examined trends in the incidence rates of cardiogenic shock and its timing 10, 27-29. The AMIS plus population-based registry study of more than 23,500 adults hospitalized with an acute coronary syndrome in medical centers throughout Switzerland examined trends in the incidence and treatment of cardiogenic shock between 1997 and 2006. The study investigators observed a significant decline in the frequency of cardiogenic shock developing during hospitalization for AMI (10.6% in 1997; 2.7% in 2006). On the other hand, the rates of cardiogenic shock present at the time of hospital admission remained constant at 2.3% during the years under study 11.
Our study demonstrated that the frequency of cardiogenic shock developing during hospitalization for AMI declined in an inconsistent and somewhat bimodal manner during the decade long period under study; these nonsignificant trends remained after controlling for a variety of other demographic and clinical factors that could have affected the development of cardiogenic shock.
In a secondary analysis, we examined trends in the timing of cardiogenic shock during the first 24 hours after hospital admission, since previous studies had shown that those with early onset shock had different outcomes compared to those with late onset shock 27-30. For example, the Multicenter Investigation of Limitation of Infarct Size (MILIS) study in the 1990's noted that nearly half of patients with an acute coronary syndrome, without shock on admission, developed cardiogenic shock within 24 hours of hospitalization 28; in the Danish Trandolapril Cardiac Evaluation (TRACE) study, approximately 3 in every 5 patients who developed cardiogenic shock developed this complication within 48 hours after the onset of AMI 27. These frequency estimates were comparable to our rates as well where 60% of patients who developed cardiogenic shock did so within the initial 24 hours of hospital admission.
Hospital death rates
Patients who developed cardiogenic shock in the present study were at nearly 6 fold greater risk for dying during their index hospitalization than patients who did not develop shock. While the crude in-hospital death rates associated with cardiogenic shock decreased over time, these encouraging trends were further enhanced after controlling for several factors of prognostic importance among patients hospitalized with AMI during the most recent years under study.
Our observed declines in the hospital death rates associated with cardiogenic shock were comparable to declines in short-term mortality reported in other studies including the National Registry of Myocardial Infarction (60.3% hospital death rate in 1995; 47.9% in 2004), the Swiss AMIS plus study (hospital CFR declined from 62.8% in 1997 to 47.7% in 2006) and several French national registries 10, 11, 24.
The improving survival rates associated with cardiogenic shock during the most recent years under study, especially after adjusting for several potentially confounding variables of prognostic importance, are likely explained by advances in the medical management of patients who develop cardiogenic shock, including the more extensive use of evidence-based supportive therapies such as positive inotropic agents and IABP 27, as well as the more optimal treatment of all patients hospitalized with AMI. Our findings are also consistent with the results of the SHOCK trial which demonstrated the benefits of early revascularization in patients with AMI who develop cardiogenic shock in reducing short and long-term mortality 6, 31. In a recent analysis of data from the Nationwide Inpatient Sample from 2002-2011, patients with an AMI who were managed invasively experienced a significantly lower odds of dying in the hospital following cardiogenic shock than those managed conservatively, with these benefits also extended to elderly patients 32. Furthermore, there were even broader implications of the enhanced medical management of patients hospitalized with AMI as there was also a marked decline observed in the hospital death rates of patients who did not develop cardiogenic shock during the years under study.
Study Strengths and Limitations
The current study was carried out in a well-defined metropolitan area with socio-demographic characteristics similar to the U.S. population as a whole. Despite the population-based design utilized, the absolute number of patients with cardiogenic shock remained relatively small compared with data from large national registries or multi-center randomized trials. Since our study included patients with AMI admitted to all hospitals in central Massachusetts that differed in their resources, individual clinician expertise, and treatment protocols, we were unable to examine the impact of these and additional related factors on our principal study endpoints. Our study does, however, provide a more ‘real world’ perspective about the magnitude and outcomes of cardiogenic shock in patients presenting to the hospital with AMI.
Conclusions
Despite encouraging declines in the death rates associated with cardiogenic shock in patients hospitalized with AMI, cardiogenic shock continues to be a serious complication of AMI with a high death rate but one that is potentially preventable and treatable with early and aggressive identification of high risk patients and effective medical management. Future studies remain needed to evaluate the efficacy of existing strategies for the prevention and management of cardiogenic shock during hospitalization for AMI and the development of protocols to ensure the optimal utilization of effective treatment strategies.
What is Known.
Previous observational studies have shown that the incidence of cardiogenic shock complicating acute myocardial infarction (AMI), and the associated mortality, remain high, despite improvements in the overall in-hospital prognosis associated with AMI.
A few recent international studies have, however, found improving short-term survival trends for cardiogenic shock, especially for shock developing during hospitalization for AMI compared with those presenting with shock at the time of hospital admission.
What the Study Adds.
The frequency of cardiogenic shock that developed during hospitalization remained relatively unchanged during the decade long period under study (2001-2011) among individuals hospitalized for AMI at all 11 metropolitan Worcester, Massachusetts, medical centers.
The crude and adjusted odds of surviving shock developing during hospitalization for AMI improved during recent study years in this cohort.
Increasing utilization of evidence- based cardiac medications and coronary reperfusion/ revascularization strategies during hospitalization for AMI parallel the declines in death risks.
Acknowledgments
We wish to express our appreciation to all persons involved in the review of data for this project during the years under study. This study was made possible through the cooperation of the administration, medical records, and cardiology departments of participating Worcester metropolitan area hospitals.
Sources of Funding: Grant support for this project was provided by the National Heart, Lung, and Blood Institute (RO1 HL35434). Dr. McManus' effort was funded by NIH grant KL2RR031981 and Drs. McManus, Gore, and Goldberg's effort was supported in part by funding from the National Heart, Lung and Blood Institute U01HL105268.
Footnotes
Disclosures: None.
References
- 1.Goldberg RJ, Gore JM, Alpert JS, Osganian V, de Groot J, Bade J, Chen Z, Frid D, Dalen JE. Cardiogenic shock after acute myocardial infarction. Incidence and mortality from a community-wide perspective, 1975 to 1988. N Engl J Med. 1991;325:1117–22. doi: 10.1056/NEJM199110173251601. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM. Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med. 1999;340:1162–8. doi: 10.1056/NEJM199904153401504. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective. Circulation. 2009;119:1211–9. doi: 10.1161/CIRCULATIONAHA.108.814947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reynolds HR, Hochman JS. Cardiogenic shock: current concepts and improving outcomes. Circulation. 2008;117:686–97. doi: 10.1161/CIRCULATIONAHA.106.613596. [DOI] [PubMed] [Google Scholar]
- 5.Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, Talley JD, Buller CE, Jacobs AK, Slater JN, Col J, McKinlay SM, LeJemtel TH. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock. N Engl J Med. 1999;341:625–34. doi: 10.1056/NEJM199908263410901. [DOI] [PubMed] [Google Scholar]
- 6.Hochman JS, Sleeper LA, Webb JG, Dzavik V, Buller CE, Aylward P, Col J, White HD, Investigators S. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295:2511–5. doi: 10.1001/jama.295.21.2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldberg RJ, Gore JM, Thompson CA, Gurwitz JH. Recent magnitude of and temporal trends (1994-1997) in the incidence and hospital death rates of cardiogenic shock complicating acute myocardial infarction: the second national registry of myocardial infarction. Am Heart J. 2001;141:65–72. doi: 10.1067/mhj.2001.111405. [DOI] [PubMed] [Google Scholar]
- 8.Fang J, Mensah GA, Alderman MH, Croft JB. Trends in acute myocardial infarction complicated by cardiogenic shock, 1979-2003, United States. Am Heart J. 2006;152:1035–41. doi: 10.1016/j.ahj.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 9.Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA, Jr, Granger CB, Flather MD, Budaj A, Quill A, Gore JM, Investigators G. Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007;297:1892–900. doi: 10.1001/jama.297.17.1892. [DOI] [PubMed] [Google Scholar]
- 10.Aissaoui N, Puymirat E, Tabone X, Charbonnier B, Schiele F, Lefevre T, Durand E, Blanchard D, Simon T, Cambou JP, Danchin N. Improved outcome of cardiogenic shock at the acute stage of myocardial infarction: a report from the USIK 1995, USIC 2000, and FAST-MI French nationwide registries. Eur Heart J. 2012;33:2535–43. doi: 10.1093/eurheartj/ehs264. [DOI] [PubMed] [Google Scholar]
- 11.Jeger RV, Radovanovic D, Hunziker PR, Pfisterer ME, Stauffer JC, Erne P, Urban P, Investigators APR. Ten-year trends in the incidence and treatment of cardiogenic shock. Ann Intern Med. 2008;149:618–26. doi: 10.7326/0003-4819-149-9-200811040-00005. [DOI] [PubMed] [Google Scholar]
- 12.Menon V, Hochman JS, Stebbins A, Pfisterer M, Col J, Anderson RD, Hasdai D, Holmes DR, Bates ER, Topol EJ, Califf RM, Ohman EM. Lack of progress in cardiogenic shock: lessons from the GUSTO trials. Eur Heart J. 2000;21:1928–36. doi: 10.1053/euhj.2000.2240. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–9. [PubMed] [Google Scholar]
- 14.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–9. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, Dalen JE. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–8. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 16.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975-2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Incidence and case fatality rates of acute myocardial infarction (1975-1984): the Worcester Heart Attack Study. Am Heart J. 1988;115:761–7. doi: 10.1016/0002-8703(88)90876-9. [DOI] [PubMed] [Google Scholar]
- 18.Lindholm MG, Boesgaard S, Torp-Pedersen C, Kober L group Trs. Diabetes mellitus and cardiogenic shock in acute myocardial infarction. Eur J Heart Fail. 2005;7:834–9. doi: 10.1016/j.ejheart.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 19.Lindholm MG, Aldershvile J, Sundgreen C, Jorgensen E, Saunamaki K, Boesgaard S. Effect of early revascularisation in cardiogenic shock complicating acute myocardial infarction. A single center experience. Eur J Heart Fail. 2003;5:73–9. doi: 10.1016/s1388-9842(02)00112-5. [DOI] [PubMed] [Google Scholar]
- 20.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso JE, Tracy CM, Woo YJ, Zhao DX, Force CAT. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:529–55. doi: 10.1161/CIR.0b013e3182742c84. [DOI] [PubMed] [Google Scholar]
- 21.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Jr, Ganiats TG, Holmes DR, Jr, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ Members AATF. AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;2014;130:2354–94. doi: 10.1161/CIR.0000000000000133. [DOI] [PubMed] [Google Scholar]
- 22.Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, Rapaport E, Riegel B, Russell RO, Smith EE, 3rd, Weaver WD, Gibbons RJ, Alpert JS, Eagle KA, Gardner TJ, Garson A, Jr, Gregoratos G, Smith SC., Jr 1999 update: ACC/AHA Guidelines for the Management of Patients With Acute Myocardial Infarction: Executive Summary and Recommendations: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) Circulation. 1999;100:1016–30. doi: 10.1161/01.cir.100.9.1016. [DOI] [PubMed] [Google Scholar]
- 23.Krumholz HM, Anderson JL, Bachelder BL, Fesmire FM, Fihn SD, Foody JM, Ho PM, Kosiborod MN, Masoudi FA, Nallamothu BK. American College of Cardiology/American Heart Association Task Force on Performance M, American Academy of Family P, American College of Emergency P, American Association of C, Pulmonary R, Society for Cardiovascular A, Interventions and Society of Hospital M. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST-elevation and non-ST-elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. 2008;118:2596–648. doi: 10.1161/CIRCULATIONAHA.108.191099. [DOI] [PubMed] [Google Scholar]
- 24.Babaev A, Frederick PD, Pasta DJ, Every N, Sichrovsky T, Hochman JS, Investigators N. Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA. 2005;294:448–54. doi: 10.1001/jama.294.4.448. [DOI] [PubMed] [Google Scholar]
- 25.Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, Jain D, Gotsis W, Ahmed A, Frishman WH, Fonarow GC. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc. 2014;3:e000590. doi: 10.1161/JAHA.113.000590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abdel-Qadir HM, Ivanov J, Austin PC, Tu JV, Dzavik V. Temporal trends in cardiogenic shock treatment and outcomes among ontario patients with myocardial infarction between 1992 and 2008. Circ Cardiovasc Qual Outcomes. 2011;4:440–7. doi: 10.1161/CIRCOUTCOMES.110.959262. [DOI] [PubMed] [Google Scholar]
- 27.Lindholm MG, Kober L, Boesgaard S, Torp-Pedersen C, Aldershvile J Trandolapril Cardiac Evaluation study g. Cardiogenic shock complicating acute myocardial infarction; prognostic impact of early and late shock development. Eur Heart J. 2003;24:258–65. doi: 10.1016/s0195-668x(02)00429-3. [DOI] [PubMed] [Google Scholar]
- 28.Hands ME, Rutherford JD, Muller JE, Davies G, Stone PH, Parker C, Braunwald E. The in-hospital development of cardiogenic shock after myocardial infarction: incidence, predictors of occurrence, outcome and prognostic factors. The MILIS Study Group. J Am Coll Cardiol. 1989;14:40–6. doi: 10.1016/0735-1097(89)90051-x. discussion 47-8. [DOI] [PubMed] [Google Scholar]
- 29.Webb JG, Sleeper LA, Buller CE, Boland J, Palazzo A, Buller E, White HD, Hochman JS. Implications of the timing of onset of cardiogenic shock after acute myocardial infarction: a report from the SHOCK Trial Registry. SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK? J Am Coll Cardiol. 2000;36:1084–90. doi: 10.1016/s0735-1097(00)00876-7. [DOI] [PubMed] [Google Scholar]
- 30.Holmes DR, Jr, Bates ER, Kleiman NS, Sadowski Z, Horgan JH, Morris DC, Califf RM, Berger PB, Topol EJ. Contemporary reperfusion therapy for cardiogenic shock: the GUSTO-I trial experience. The GUSTO-I Investigators. Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries. J Am Coll Cardiol. 1995;26:668–74. doi: 10.1016/0735-1097(95)00215-p. [DOI] [PubMed] [Google Scholar]
- 31.Menon V, Fincke R. Cardiogenic shock: a summary of the randomized SHOCK trial. Congest Heart Fail. 2003;9:35–9. doi: 10.1111/j.1751-7133.2003.tb00020.x. [DOI] [PubMed] [Google Scholar]
- 32.Bangalore S, Gupta N, Guo Y, Lala A, Balsam L, Roswell RO, Reyentovich A, Hochman JS. Outcomes with invasive vs conservative management of cardiogenic shock complicating acute myocardial infarction. Am J Med. 2015;128:601–8. doi: 10.1016/j.amjmed.2014.12.009. [DOI] [PubMed] [Google Scholar]