Abstract
Psychiatric staff are faced with multiple forms of hostility, aggression, and assault at work, collectively referred to as workplace violence, which typically is activated by patients but can also come from coworkers and supervisors. Whether workplace violence adversely affects staff well-being may be related not only to its presence, but also to an individual’s stress reactivity. At a large public psychiatric hospital, an online survey was completed by 323 clinical care staff, of whom 69.5% had experienced physical assault in the previous 12 months. Staff well-being (depression, anger, and physical health) and staff safety concerns were adversely affected by conflicts with other staff members and by individual reactivity to social conflict and to assault. To improve staff well-being, in addition to safety protocols, interventions should target staff relationships, personal health maintenance practices, and individual coping skills for dealing with adverse workplace experiences.
Keywords: assault, conflict, psychiatric staff, and well-being
The creation of a therapeutic environment is an essential goal for psychiatric inpatient settings. Interpersonal antagonism in the form of discord, hostility, aggression, and assault are common occurrences on psychiatric hospital wards, and impair the development of a treatment-conducive milieu (Arnetz & Arnetz, 2001). They also produce adversities for staff well-being, detracting from patient care. Numerous studies have documented that psychiatric staff are at high risk for workplace violence, including physical assault and verbal aggression by patients, visitors, supervisors, and coworkers (Cornaggia, Beghi, Pavone, & Barale, 2011; Flannery, Wyshak, & Flannery, 2014; Gerberich et al., 2004; McKenna, Smith, Poole, & Coverdale, 2003). According to a national survey conducted by the U.S. Department of Justice (Harrell, 2011), the average annual rate of nonfatal workplace violence between 2005 and 2009 was 5.1 incidents per 1,000 employees across occupational categories, whereas mental health workers experienced a rate of 20.5 incidents per 1,000 employees. Among staff in three public mental hospitals in California, a Service Employees International Union (2011) survey (N = 294) found that 68% reported being assaulted while at work, the most common forms of assault being hit, pushed, and spit upon. High rates of assault have serious consequences for staff well-being in terms of physical health, mental health, and perceptions of safety (Croker & Cummings, 1995; Ito, Eisen, Sederer, Yamada, & Tachimori, 2001; Lanza, 1983; Wykes & Whittington, 1998). However, staff can be differentially reactive to these stressors, and their reactivity may bear on the severity of the consequences.
The occurrence of assault and conflicts with patients in psychiatric settings continue to receive considerable research and practice attention, but interpersonal conflict with coworkers and supervisors, which can also impair one’s personal and professional functioning, has typically not been considered. Most previous research has not concurrently investigated multiple sources of antagonism, and whether their effects might be moderated by individual difference factors remains largely unexamined. How staff perceive conflict and strive to cope with it may be important for how they are affected by it. Staff are likely to appraise conflict with patients differently than they appraise conflict with coworkers and supervisors, seeing it as part of a patient’s pathology rather than as a true interpersonal conflict. Individual differences in sensitivity or reactivity to workplace conflict and assault hypothetically bear on how staff are affected by those experiences.
The current study was designed to assess how multiple sources of workplace stress (patient assault, high-conflict aspects of patient care, and interstaff conflict) are related to staff well-being (physical health, mental health, and perceptions of safety), and to determine whether individual stress reactivity moderates that relationship.
Patient Assault
Patient physical assault against staff, which ranges in outcome from unsuccessful attempts or minor injury to severe injury or even death (Yassi, 1994), is disturbingly prevalent in psychiatric settings. An international review of violence toward nurses by Spector, Zhou, & Che (2014) found that 55% of nurses in psychiatric settings experienced physical assault and that psychiatric settings had a higher rate of violence than any other health care setting. It is generally accepted that assault records data are underestimates, because staff may under-report harassment or assault due to fear of being perceived as less competent or being blamed (Lion, Synder, & Merrill, 1981), peer pressure not to report assault based on the gender of the person assaulted (Lanza, Kayne, Hicks, & Milner, 1991), or a lack of desire to deal with excessive paperwork (Lion et al., 1981). Staff who are assaulted tend to be younger (under 30 years old), less experienced, less educated, provide more direct care, spend more time with patients, receive lower pay, and possess low levels of qualifications (Cunningham, Connor, Miller, & Melloni, 2003; Flannery, LeVitre, Rego, & Walker, 2011). The present study will control for years of experience and direct care staff roles.
Workplace Social Conflict
Assault is the most serious safety concern in psychiatric settings, but it is not the only form of interpersonal conflict. Research has shown that 73% of nurses experience at least one incident of verbal aggression by patients per year (Spector et al., 2014), and verbal aggression accounts for an estimated 75% of patient-to-staff aggressive incidents (Jonker, Goossens, Steenhuis, & Oud, 2008). Many studies have identified coworkers and supervisors as a common source of verbal antagonism and bullying (e.g., McKenna et al., 2003; Paterson, McComish, & Aiken, 1997). In a large sample study of Minnesota nurses, approximately 33% of non-physical incidents were perpetrated by supervisors, physicians, visitors, and other employees (Gerberich et al., 2004). Cumulatively, these rates of workplace conflict and assault indicate that psychiatric staff must function in multi-faceted stressful environments. How staff are affected by these aversive physical and social experiences is an important issue.
Adverse Outcomes of Workplace Conflict and Assault
Psychological and Emotional Consequences
Direct care staff can feel tormented, helpless, unsettled, and humiliated by assault and verbal antagonism on their hospital units (Hellzen, Asplund, Sandman, & Norberg, 2004). The most commonly reported emotional consequences of assault and verbal aggression are shock, frustration, anger, fear, anxiety, stress, and irritability (Gerberich et al., 2004; Needham, Abderhalden, Halfens, Fischer, & Dassen, 2005). Similar to individuals who have experienced other traumatic events, psychiatric unit staff who have been assaulted by patients are at increased risk of developing posttraumatic stress disorder (Caldwell, 1992; Richter & Berger, 2006) and major depression (Lenehan & Turner, 1984). Interstaff aggression has also been noted to have adverse emotional effects in multiple studies (Hegney, Plank, & Parker, 2003; Henderson, 2003; McKenna et al., 2003), and nonphysical aggression by colleagues may be more distressing than that by patients (Farrell, 1999).
Physical Health
Patient assaults are the leading cause of physical injury in psychiatric hospitals in the United States (Love & Hunter, 1996). After an injury, there can be persistent pain, headaches, and muscle tension (Gerberich et al., 2004; Levin, Hewitt, & Misner, 1998), plus psychological distress. Verbal aggression from patients and conflict with other staff members represent daily challenges that activate a generalized stress response. Numerous studies have demonstrated that workplace stressors are associated with adverse health outcomes, such as development of cardiovascular disease (e.g., Eller et al., 2009; Karasek, Baker, Marxer, & Theorell, 1981).
Perceptions of Workplace Safety
Workplace violence impairs staff perceptions of safety. A chronic sense of decreased safety due to exposure to assault may lead to altered health behaviors and long-term effects on physical and emotional health. Job performance can also be adversely affected by feelings of insecurity; staff who feel unsafe at work may engage in behaviors that impair therapeutic rapport, such as avoidance, passivity, and inconsistent or harsh enforcement of ward rules (Alexander & Bowers, 2004; Needham et al., 2005). Conflict with other staff can also erode perceptions of safety. Because staff members must work together to prevent and manage patient assault and verbal aggression, conflict with other employees may erode one’s trust that coworkers will provide support in management of a violent incident, leading staff to feel less safe.
Hospitals, as organizations, suffer when staff safety is jeopardized. The occurrence of violence in mental health facilities has direct costs for medical care, litigation, worker’s compensation benefits, paid leave, and substitute staffing. Additionally, there are indirect costs related to low morale, recruitment and retention difficulties, service interruption, compromised public relations, impaired job performance, and the cultivation of a negative therapeutic environment (Cunningham et al., 2003; Farrell & Cubit, 2005; Hunter & Carmel, 1992; Jackson, Clare, & Mannix, 2002; Rossberg, Melle, Opjordsmoen, & Friis, 2008).
Stress Reactivity to Assault and Conflict
How staff are affected by aggression and assault may be a product of individual differences in their reactivity to these stressors. Stress reactivity refers to a person’s psycho-physiological activation in response to stressors, as the same stressor can have profoundly different effects on individuals (Cacioppo et al., 1998). Stress reactivity may reflect a person’s ability to cope with particular demands or may reflect their sensitization to particular stressors. It is conceptualized as the disposition of a person to respond to stressors with stress reactions that range from immediate to enduring (Federenko et al., 2006; Limm et al., 2010). Stress reactivity is often measured through physiological markers such as salivary cortisol, heart rate, blood pressure, and plasma catcholamine (Cacioppo et al., 1998). Since physiological measurement of stress responses is beyond the capacity of most studies in organizational settings, researchers have begun to use self-report measures (Limm et al., 2010).
Only a few studies have examined stress reactivity in relationship to workplace conflicts and assault. Ilies, Johnson, Judge, and Keeney (2011) indexed reactivity to conflict by the personality trait of agreeableness and found it to have a moderating influence on whether workplace interpersonal conflict was related to negative affect. In the presence of conflict, individuals who reported higher levels of agreeableness were more likely to experience negative affect than those who were less agreeable. Kelly, Subica, Fulginiti, Brekke, and Novaco (2015), with a slightly larger sample overlapping that of the present study, found that patient-on-staff assault was associated with social conflict, but that relationship was moderated by stress reactivity in a curious way. Staff at the highest risk for patient assault were those who were frequently exposed to conflict but were also less reactive to conflict. Cumulatively, these findings suggest that there may be a complex relationship between conflict, assault, and stress reactivity that bears on staff psychological and physical well-being in psychiatric settings.
The Current Study
Many studies have examined psychiatric staff well-being as a function of patient assault, conflicts with patients, and intrastaff conflicts (Needham et al., 2005), but not the concurrent effects of these variables as they coexist in the workplace. Review articles (e.g., Jackson et al. 2002) that have discussed interactive influences, largely focus on nursing staff. For example, the fine interactional model presented by Whittington and Richter (2005) deals with patient-staff interaction but does not address how staff-staff interaction might bear on patient-staff interaction. The concept of individual reactivity, which has been explored in the areas of interpersonal relationships and coping, has only recently been applied to the study of workplace violence (Kelly et al., 2015).
The present study involves ward, clinical, and supervisory staff at a large public psychiatric hospital. It examines the inter-relationships between patient assaults, conflicts with patients, conflicts with other staff, and individual stress reactivity in association with staff well-being. The aims of this study were: (a) to examine how staff well-being (physical health and mental health) and safety perceptions are associated with workplace violence and conflict, and (b) to test whether individual stress reactivity moderates those associations. We hypothesize that staff who are highly reactive to stressors are more likely to report symptoms of strain when faced with high frequencies of physical assault and interpersonal conflicts. We control for personal and workplace factors that bear on our outcomes, namely gender, years of experience, staff role (ward, clinical, and supervisory), and health habits.
Method
Procedures
All clinical staff (N = 1,794) at a large public mental hospital in California were invited to participate in an hour-long online survey about their background, occupational stressors, strains resultant from stressors, and management of occupational stressors. This study was approved by the institutional review board of [Blinded for Review].
Participants
The survey link was opened by 488 individuals (27%). Of those, 14 did not agree to participate, and 19 agreed but did not answer any questions. Another 127 individuals did not answer questions related to their well-being and were not included in the final analyses. Therefore, the final sample consisted of 323 staff (66% of those who saw the survey). This response rate is considerably higher than that of a survey on workplace violence conducted across all four state mental hospitals by a union organization (SEIU, 2011)
Measures
Demographic and background information
Participants reported their gender and race (see Table 1). Gender was coded dichotomously (0 = male, 1 = female). Race was a categorical variable and used descriptively.
Table 1.
Background Characteristics of Sample and Total Hospital Staff
| Sample
|
Total Hospital
|
|||
|---|---|---|---|---|
| Variables | % | N | % | N |
| Gender | 322 | 2824 | ||
| Male | 32.6% | 105 | 40.3% | 1137 |
| Female | 67.2% | 217 | 59.7% | 1687 |
| Race/Ethnicity | 322 | 2824 | ||
| White | 37.8% | 122 | 31.9% | 900 |
| Black | 20.4% | 66 | 23.2% | 654 |
| Asian | 11.1% | 36 | 21.2% | 599 |
| Hispanic | 20.4% | 66 | 20.2% | 571 |
| Other | 10.2% | 32 | 3.5% | 100 |
| Position | 323 | 1794 | ||
| Psychiatric technician | 40.9% | 132 | 39.7% | 712 |
| Senior psychiatric technician | 5.9% | 19 | 4.1% | 74 |
| Registered nurse | 19.2% | 62 | 22.7% | 408 |
| Unit supervisor | 0.9% | 3 | 1.6% | 29 |
| Rehabilitation therapist | 7.7% | 25 | 4.5% | 81 |
| Psychologist | 8.4% | 27 | 1.9% | 34 |
| Social worker | 7.4% | 24 | 5.5% | 99 |
| Psychiatrist | 2.8% | 9 | 5.2% | 93 |
| Administrative supervisors | 2.2% | 7 | 1.7% | 31 |
| Clinical supervisors | 1.5% | 5 | 3.3% | 60 |
| Other | 3.1% | 10 | 9.6% | 173 |
Note. Data for total hospital staff were provided by the office of the hospital’s Executive Director. Sample characteristics are presented alongside those for total hospital staff.
Work histories
Participants identified their current position and length of work experience (in years) in the current hospital. Because the amount of time spent in direct care with patients is a risk factor for assault, positions were recoded into groups according to the amount of time spent on the unit: ward staff (psychiatric technicians, senior psychiatric technicians, unit supervisors, registered nurses), clinical care staff (rehabilitation therapists, psychologists, social workers, and psychiatrists), and supervisory staff (administrative supervisors, clinical supervisors).
Health habits
Participants were asked five questions about their beneficial and detrimental health behaviors drawn from the 1981 National Health Leisure Time Survey (Wilsnack, Klassen, & Wilsnack, 1984). Beneficial health behaviors include the frequency of vigorous exercise (heart rate above 130 beats per minute: 1 = never to 8 = daily) and a general self-estimate of healthy eating habits (1= not healthy at all to 5 = very healthy). Detrimental health behaviors included the frequency and quantity of alcohol consumption (e.g., “How often do you drink any kind of alcoholic beverage (i.e., beer, wine, or liquor)?” Respondents who reported alcohol use were asked, “About how many drinks, on average, would you have on a typical day when you drank?” A drink was defined as a 4 oz glass of wine, a 12 oz beer, or 1 oz of liquor. Reports of alcohol use were extrapolated to assess the total number of drinks per month. A count of caffeinated beverages consumed daily was also included.
Beneficial health behaviors were reverse coded. All items were z scored and summed to create a composite score of health habits, with higher scores indicating poorer health habits. Health habits were included as a study measure, since infrequent exercise, poor diet, and consumption of alcohol are all associated with greater stress responses (Crews & Lander, 1987; Jakuli et al. 2007).
Predictor Variables
Intrastaff conflict
Using a three-item subscale of the Psychiatric Nurses Stress Inventory (Sullivan, 1993), respondents rated domains of social conflict with other staff members (difficulty working with particular nurses on the ward, disagreements concerning the treatment of a patient, and conflicts with management). Participants rated the frequency of each stressor during the previous 6 months (1 = never to 5 = very often). Higher scores indicated more conflict with coworkers. The reliability of this scale was good (α = .75).
Physical assault experiences
Participants rated how frequently they were physically assaulted during the previous year based on an eight-item measure written for this study, including: (a) spit at; (b) touched or grabbed aggressively; (c) kissed, fondled, or had a patient sexually expose themselves; (d) pushed or knocked down; (e) kicked, punched, bit, or slapped; (f) hit on the head; (g) had object thrown at them; and (h) other. A 4-point Likert scale was used (0 = never, 1 = one or two times, 2 = three to five times, 3 = 6 or more times), and a scaled mean was calculated for inclusion in analyses.
Patient-staff conflicts
Using eight items derived from the Psychiatric Nurses Stress Inventory (Sullivan, 1993), participants estimated the frequency with which they experience patient care demands that are high conflict. Patient-staff conflicts were based in 3 domains: (a) antagonism or challenging by patients (patients swearing or yelling at staff member, patients who tried to intimidate staff member, difficult or demanding patients); (b) containment or restraint procedures (physically restraining a patient, unscheduled medication of a patient, placing a patient in seclusion); and (c) working with high risk patients (dealing with potentially suicidal patients, continuous observation of patients on a one-to-one basis). Staff members rated the frequency of each activity on a 5-point scale (1 = never to 5 = very often). Higher scores indicated more frequent conflict with patients and the scale demonstrated excellent reliability (α = .89).
Social conflict stress reactivity
A 5-item social conflict subscale of the Perceived Stress Reactivity scale was used (Schulz, Jansen, & Schlotz, 2005). Each item has two components: a description of a potentially stressful social situation and three response options (e.g., (a) When I argue with other people, (1) I usually calm down quickly, (2) I usually stay upset for some time, or (3) it usually takes me a long time until I calm down (b) When I have conflicts with others not immediately resolved, (1) I generally shrug it off, (2) it usually affects me a little, or (3) it usually affects me a lot; (c) When I am wrongly criticized by others, (1) (3) in general, I am hardly annoyed at all (2) I am annoyed for just a short time, or, (3) I am normally annoyed for a long time).. Higher scores indicate a more intense and prolonged degree of upset. In prior research, high total stress reactivity scores have been associated with depressive symptoms and sleep disturbances (Schlotz, Yim, Zoccola, Jansen, & Schulz, 2011). In the current study, the reliability of the subscale (α = .72) was similar to that found in a previous study with a U.S. population (α = .71; Schlotz et al., 2011).
Assault reactivity
Participants rated 2 items on a 5-point scale about their reactions to assault. First, participants rated how stressful it was for them when a patient made an unsuccessful attempt to assault them. Secondly, they rated their distress when assaulted (0 = not stressful to 4 = overwhelming). If individuals were not assaulted and no one had attempted to assault them, they could select ‘not applicable’. Individuals who were not assaulted and selected ‘not applicable’ were coded as having a ‘not stressful‘ reaction, unless they reported distress related to an attempted assault. An average assault reactivity score was calculated. The reliability of reactions to assault was good (α = .86).
Outcome Measures
Safety perceptions
Participants estimated how unsafe they feel at work using two items. First, they were asked about how unsafe they feel generally at work. Responses ranged from 1 = very safe to 5 = very unsafe. Secondly, they were asked to rate whether the hospital’s current safety procedures are effective at protecting the safety of staff members on a 4-point scale (1 = well protected to 4 = unprotected). These items, which were on different scales, were transformed into z scores and averaged to compose a safety index (α = .71). Higher scores indicated greater concerns about safety.
Physical health symptoms
A 12-item subscale from the Hopkins Symptom Checklist (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974) was used to estimate the number of health issues among staff members. Participants rated the frequency of perceptions of bodily dysfunction during the previous month (1 = not at all to 4 = extremely often). Complaints ranged from cardiovascular (heart or chest pain) and respiratory (difficulty breathing) to other symptoms related to stress (lower back pain). Reliability of this measure in prior research was good (α = .87; N = 1,435 anxious and depressed outpatients and controls; Derogatis et al., 1974), and it was also good in the present study (α = .85). Scores on this scale are average item scores, higher scores indicated poorer health.
Depression symptoms
The General Health Questionnaire-12 is a self-report measure that assesses depressed mood, lack of positive affect, somatic symptoms, and interpersonal difficulties (Goldberg & Williams, 1988). The presence of depressive symptoms includes six negative items (e.g., feeling unhappy or depressed) and six positive items (e.g., ability to face problems). Each item is rated on a 4-point scale, conveying the frequency of each endorsed item during the previous few weeks (0 = much less than usual to 3 = more so than usual). Item scores were averaged and used as a continuous variable in analyses. In the current study, this measure demonstrated good reliability (α = .76).
Anger
Participants rated the frequency that they felt angry or irritable on a 4-point scale (1 = not at all to 4 = extremely often) using an item written for this study. The use of a single item was done to obviate participant misgivings about reporting anger in the workplace, as it is typically seen as an inappropriate emotion for staff in this context.
Statistical Analyses
All data were inspected for normality of distributions and z-score transformations were used when appropriate. Correlation, t-tests, one-way analyses of variance, and chi-square analyses were also completed. To analyze the predictive factors of perceived safety and staff well-being, hierarchical linear regressions were completed in three steps. In the first step, personal and workplace factors that generally affect staff well-being were entered as a covariate block (gender, years of experience, position, and healthy habits). In the second step, aggression and assault factors and staff reactions to these experiences were included (intrastaff conflict, patient-on-staff conflict, social conflict reactivity, and patient-on-staff assault frequency and severity). In the final step, interactions of the frequency of conflict and assault and reactions to conflict and assault were tested. Tests of variance inflation factor and tolerance indicated that multicollinearity was not an issue for the regression models.
Results
Sample
The composition of the final study sample is presented in Table 1 and was similar to the overall hospital staff, though it was slightly over-representative of Caucasians and females. There were no gender differences across position groups (χ2 (2, 311) = 3.11, p = .19) or years of experience (t (312) = .65, p = .52).
Workplace Aggression and Assault
To determine the scope of workplace conflict, assault, and concerns about safety and the status of psychiatric staff we examined: (a) the prevalence of workplace assault and conflict; (b) the intercorrelations of assault, conflict, and reactions to assault and conflict; and (c) the intercorrelations of safety and well-being. The means, standard deviations, ranges, and correlations of workplace violence and outcome variables are presented in Table 2.
Table 2.
Descriptives and Correlations of Study Variables
| Variable Name | M | SD | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Years employed in hospital | 10.36 | 7.55 | (0.10–37.00) | ||||||||||
| 2. Health habits index | 0.00 | 0.57 | (−1.26–2.11) | .08 | |||||||||
| 3. Patient-staff conflict | 3.08 | 0.95 | (1.00–5.00) | −.13 | .04 | ||||||||
| 4. Patient assault frequency | 0.37 | 0.46 | (0.00–2.75) | −.03 | −.07 | .54** | |||||||
| 5. Intrastaff social conflict | 2.56 | 1.00 | (1.00–5.00) | −.03 | .12 | .38** | .22** | ||||||
| 6. Reactivity to assault | 1.87 | 1.57 | (0.00–4.00) | .00 | −.07 | .52** | .51** | .21** | |||||
| 7. Reactivity to social conflict | 1.94 | 1.80 | (1.00–3.00) | .04 | .09 | −.05 | −.18** | .20** | .07 | ||||
| 8. Depression symptoms | 1.45 | 0.35 | (0.00–2.69) | .18* | .19** | −.03 | −.01 | .15* | .06 | .25** | |||
| 9. Angry/Irritable | 1.97 | 0.71 | (1.00–4.00) | .06 | .20** | .14 | .02 | .27** | .08 | .40** | .36** | ||
| 10. Physical health symptoms | 1.59 | 0.43 | (1.00–3.42) | .11 | .12 | .24** | .15* | .27** | .18** | .24** | .31** | .46** | |
| 11. Safety z score | −0.02 | 0.89 | (−2.97–1.67) | .05 | .05 | .40** | .33** | .31** | .31** | .21** | .07 | .21** | .27** |
Note. M = Mean. SD = Standard Deviation.
p < .01.
p <.001.
Health habits = a z-scored index of diet, exercise, alcohol and caffeine consumption. Patient-staff conflict = modified items from Psychiatric Nurses Stress Inventory. Patient assault frequency = scaled frequency of assault index created for this study. Intrastaff social conflict = modified items from Psychiatric Nurses Stress Inventory. Assault reactivity = two items of distress severity due to assault incidents. Reactivity to social conflict = subscale from Perceived Stress Reactivity Scale. Depression symptoms = General Health Questionnaire-12. Angry/Irritable = one item frequency of feeling angry/irritable. Physical health symptoms = subscale from Hopkins Symptom Checklist. Safety = a z-scored two-item scale with higher scores indicating less safety.
Patient verbal aggression was common, with 98% of participants reporting any verbal aggression from patients, although only 34% reported verbal aggression from patients as occurring often or very often. Ward staff reported more conflict with patients (M = 3.36, SD = .89) than clinical staff (M = 2.47, SD = .70, Games-Howell post hoc tests p <.001) but neither ward staff (p = .10) or clinical staff (p = .81) differed significantly from supervisory staff (M = 2.66, SD = 1.04; F(2,307) = 34.63, p <.001). Staff conflict was also common, with 94.2% reporting social conflict with other staff. There were no gender differences in the frequency of conflict with patients (t (318) = 1.50, p = .14) or with other staff (t (318) = −.57, p = .57). Ward staff reported slightly more conflict with other staff (M = 2.65, SD = 1.05) than did clinical staff (M = 2.35, SD = .84; Games-Howell post hoc test p = .03). Neither ward staff nor clinical staff differed from supervisory staff (M = 2.56, SD = .99) in conflicts with co-workers.
During the previous 12 months, 69.8% of staff reported at least one physical assault incident. Assaults varied in severity. The most frequent type of incident was having a patient attempt to kiss or fondle a staff member or expose themselves (43.2%), and the least frequent, but very serious, occurrence was being hit in the head (13.9%). Male staff were assaulted (scaled M = .45, SD = .52) slightly more often than female staff (scaled M = .33, SD = .42; t (320) = 2.17, p = .03). Ward staff were assaulted (scaled M = .48, SD = .51) more often than clinical (scaled M = .15, SD = .18; Games-Howell post hoc test, p <.001) or supervisory staff (scaled M = .17, SD = .24; Games-Howell post hoc test p = .002; F(2,309) = 19.31, p <.001). The measures of conflict and assault with patients were moderately correlated (r = .54) and conflict with patients was more strongly related to intrastaff conflict (r = .38) than assault (r = .22).
Reactivity to social conflict and reactivity to assault
Reactivity to social conflict was normally distributed (M = 1.94, SD = 1.80), and about a third of participants reported at least moderate difficulty letting go of conflict. Staff position groups did not differ in their reactivity to conflict (F [2, 308] = 1.05, p = .35), but there was a small difference by gender, as female staff (M = 1.98, SD = .43) reported higher reactivity to social conflict than did males (M = 1.87, SD = .41; t (319) = −2.19, p = .03).
Some staff were deeply affected by assault incidents, even if an assault attempt was not successful; 24.6% reported being stressed or overwhelmed by assault. On average, staff reported only occasional use of patient containment, but 78.3% had used patient containment procedures (medication, restraints, or solitary confinement) during the previous 6 months. For reactivity to assault (F [2,307] = 14.30, p < .001) ward staff reported higher assault reactivity (M = 2.19, SD = 1.50) than did clinical (M = 1.22, SD = 1.53; Scheffe post-hoc tests p < .001) or supervisory staff (M = 1.04, SD = 1.42; p = .04). There were no differences in assault reactivity between clinical and supervisory staff or between males and females. The correlation between reactivity to social conflict and reactivity to assault was not significant, which suggests that these are distinct constructs.
Perceptions of Safety
Staff reported high concern about their safety, as 44.6% of staff reported feeling ‘unsafe’ or ‘very unsafe’ at work. Moreover, 90.1% of respondents thought that staff could be more protected or are unprotected while at work. As can be seen in Table 2, safety perceptions were modestly correlated with reactivity to assault and reactivity to social conflict.
Workplace Violence and Safety
Hierarchical linear regressions were performed in three steps with perceived safety and each measure of well-being. Results are presented in Table 3.
Table 3.
Hierarchical Linear Regressions of Staff Well-Being Indices as Associated with Workplace Conflict and Assault
| Model | Variables | Safety
|
Depression
|
Angry/Irritable
|
Physical Health
|
||||
|---|---|---|---|---|---|---|---|---|---|
| β | p | β | p | β | p | β | p | ||
| Step 1 | |||||||||
| Gender | .05 | .338 | .12 | .033 | .02 | .771 | .19 | .001 | |
| Experience | .03 | .561 | .18 | .003 | .07 | .226 | .10 | .103 | |
| Clinical staffa | −.26 | .000 | .00 | .947 | .02 | .729 | −.14 | .014 | |
| Supervisorsa | −.11 | .064 | −.02 | .699 | −.05 | .364 | −.07 | .255 | |
| Health habits | .06 | .291 | .20 | .000 | .22 | .000 | .15 | .007 | |
| Step 2 | |||||||||
| Gender | .06 | .278 | .09 | .098 | −.05 | .361 | .18 | .001 | |
| Experience | .09 | .108 | .16 | .006 | .09 | .087 | .13 | .023 | |
| Clinical staffa | −.11 | .052 | −.01 | .814 | .06 | .317 | −.05 | .373 | |
| Supervisorsa | −.07 | .158 | −.03 | .618 | −.06 | .265 | −.05 | .369 | |
| Health habits | .03 | .566 | .18 | .002 | .14 | .008 | .12 | .032 | |
| Patient conflict frequency | .19 | .007 | −.12 | .106 | .11 | .141 | .13 | .068 | |
| Patient assault frequency | .15 | .016 | .04 | .567 | −.01 | .847 | .03 | .615 | |
| Intrastaff conflict frequency | .15 | .007 | .12 | .058 | .18 | .001 | .14 | .022 | |
| Reactivity to social conflict | .20 | .000 | .18 | .002 | .34 | .000 | .16 | .005 | |
| Reactivity to assault | .06 | .334 | .09 | .177 | .02 | .721 | .06 | .368 | |
| Step 3 | |||||||||
| Gender | .05 | .321 | .10 | .077 | −.05 | .350 | .18 | .001 | |
| Experience | .08 | .150 | .17 | .003 | .11 | .054 | .13 | .020 | |
| Clinical staffa | −.11 | .046 | .00 | .981 | .06 | .296 | −.06 | .363 | |
| Supervisorsa | −.07 | .206 | −.01 | .822 | −.06 | .237 | −.06 | .318 | |
| Health habits | −.08 | .106 | .18 | .001 | .15 | .004 | .12 | .029 | |
| Patient conflict frequency | .18 | .009 | −.14 | .063 | .10 | .141 | .15 | .047 | |
| Patient assault frequency | .12 | .167 | .19 | .028 | .10 | .216 | .05 | .529 | |
| Intrastaff conflict frequency | .14 | .013 | .11 | .072 | .20 | .001 | .14 | .019 | |
| Reactivity to social conflict | .09 | .000 | .17 | .002 | .34 | .000 | .17 | .003 | |
| Reactivity to assault | .20 | .201 | .02 | .811 | −.06 | .410 | .04 | .610 | |
| Patient conflict x conflict reactivity | −.05 | .388 | .00 | .998 | .03 | .608 | .08 | .152 | |
| Assault frequency x assault reactivity | .05 | .414 | −.17 | .018 | −.17 | .012 | −.03 | .661 | |
| Staff conflict x conflict reactivity | .05 | .384 | .12 | .048 | −.10 | .065 | −.11 | .069 | |
Note: Criterion measures are: Safety = Z score of two-item scale with higher scores indicating less safety. Depression = General Health Questionnaire-12. Angry/Irritable = frequency of feeling angry/irritable on a 4 point scale. Physical Health = Hopkins Symptom Checklist. Gender is coded 1 = men, 2 = female.
Comparison group is ward staff.
Health habits = a z-scored index of diet, exercise, alcohol and caffeine consumption. Staff conflict with patients = Modified items from Psychiatric Nurses Stress Inventory. Patient assault = Scaled frequency of assault index created for this study. Intrastaff conflict = Modified items from Psychiatric Nurses Stress Inventory. Reaction intensity to assault = Two items of distress severity in response to assault incidents. Reactivity to social conflicts = subscale from Perceived Stress Reactivity Scale. In step 3, the coefficients are bolded only if the interaction terms are significant, which means the full block of variables should be interpreted.
For the perceived safety criterion, in the first step, the covariate block of personal factors (gender, health habits, and years of experience) and position (ward/clinical staff, ward/supervisory staff) accounted for 6.4% of the variance. Specifically, staff stationed on the ward (i.e., psychiatric technicians and nurses) felt less safe than did clinical staff. In the second step, after indexes of conflict and assault were added, the ward/clinical position contrast was reduced to a trend level. Staff experiences of higher levels of patient conflict, patient assault, intrastaff conflict, and reactivity to social conflict were all significantly associated with staff feeling unsafe (model adjusted R2 = 24.0%). Notably, the patient variables and the staff variables had comparable associations with safety. None of the interaction terms in the final step were significantly related to safety concerns.
Staff Well-Being and Workplace Violence
Staff well-being was evaluated in terms of mental health and physical health. Depression and anger were moderately correlated (see Table 2), as were depression and physical health, but depression was not correlated with perceived safety. Anger had a robust association with physical health. Safety had smaller but significant correlations with anger and physical health.
Depression
Participants’ depression ratings were comparable to those found among employees in a similar setting (Hardy, Shapiro, Haynes, & Rick, 1999). Participants reported feeling positive emotions more often (M = 2.89, SD = 0.33) than negative emotions (M = 1.79, SD = 0.57).
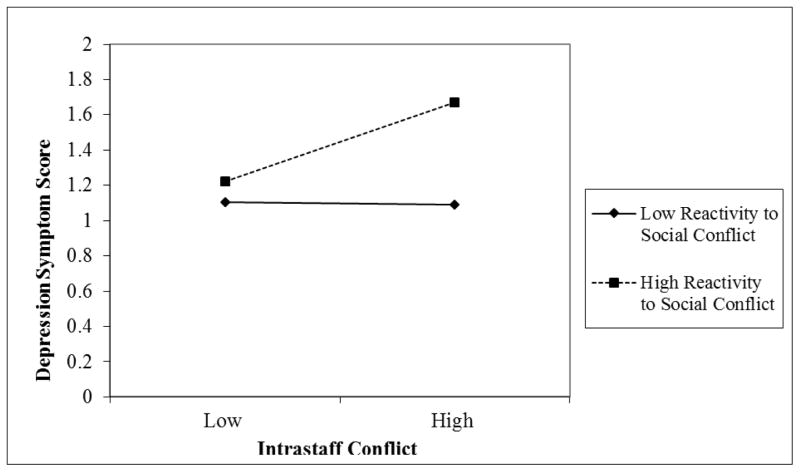
More experienced staff, those with more unhealthy habits, and female staff reported more depression symptoms (first step, model adjusted R2 = 6.4%). After the addition of conflict and assault factors in the second step (model adjusted R2 = 11.2%), intrastaff conflict and being more reactive to social conflict were also significantly associated with greater depression symptoms, but gender was no longer significant. In the final step, the interaction of staff conflict and reactivity to social conflict was significant (model adjusted R2 = 13.7%). As presented in Figure 1, reactivity to conflict was unrelated to depression scores among individuals experiencing low levels of conflict. However, among staff experiencing high levels of conflict, those who were more reactive reported higher depression, but those who were less reactive had depression scores comparable to those experiencing low levels of conflict.
Figure 1.
Depression and Staff Conflict Frequency as Moderated by Social Conflict Reactivity
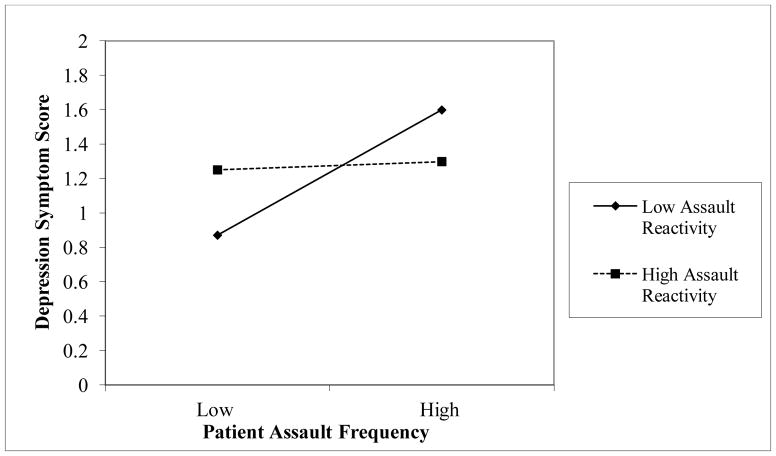
The interaction between patient care conflict and social stress reactivity was significant (see Figure 2). The depression scores of those who reported stronger reactivity to assault was unaffected by the frequency of assault. However, among those low in reactivity to assault, depression scores were higher if they were assaulted more frequently than if they were assaulted less often. Staff who were not reactive to assault and were infrequently assaulted had the best overall mental health.
Figure 2.
Depression and Patient Assault Frequency as Moderated by Assault Reactivity
Anger
Having more unhealthy habits was associated with anger in the first step (model adjusted R2 = 3.8%); gender, years of experience, and staff position were not significant. In the second step, intrastaff conflict and reactivity to social conflict were associated with more frequent anger (model adjusted R2 = 21.0%). In the final step, reactivity to assault moderated the associations between assault and anger (model adjusted R2 = 22.5%). Similar to the interaction in Figure 2 for depression, anger was unrelated to frequency of assault among those who were highly reactive to assault. Conversely, among those with low reactivity to assault, the frequency of assault and anger were positively associated.
Physical health
Staff reported few physical health symptoms. The most common health complaints were having low energy, headaches, back pain, and muscle soreness. More serious health problems were reported with less frequency, these being numbness or tingling, hot and cold spells, difficulty breathing, and dizziness. The number of physical health symptoms was most strongly correlated (r = .46) with anger. In the hierarchical regression, on the first step, women, those with poorer health habits, and ward staff reported higher symptoms scores than did clinical staff (model adjusted R2 = 6.7%). After the inclusion of the conflict and assault factors in the second step, women and those with poorer health habits remained at higher risk for symptoms. Having more work experience became significantly related to symptomology, but the contrast between ward and clinical staff was no longer significant. Poorer physical health was significantly related to more frequent intrastaff conflict and to being more reactive to social conflict (model adjusted R2 = 15.1%). None of the interactions tested were significant in the third step.
Finally, as hospitals may need to recognize employees needing assistance, an exploratory analysis was conducted.. Scores on each of the safety and well-being indices were partitioned into quartiles and we examined the overlap of those who scored in the top quartile on all indices. Eight percent of the sample scored in highest quartile on all four outcomes, and another 13.3% in the top quartile on three or more. Overall, about a fifth of staff are struggling and could potentially benefit from intervention.
Discussion
The performance of psychiatric staff is linked to their psychological functioning (Packard & Motowidlo, 1987; Stewart, Ricci, Chee, & Morganstein, 2003). To ensure that high-quality care is delivered to patients, the wellness of care providers must be optimized, and therefore given concerted attention. As exposure to social conflict and assault are known to compromises staff well-being, we added self-reported stress reactivity to these adversities in our examination – one of the few studies to do so. Our results suggest that, although assault may be traumatic, everyday stressors of patient conflict and intrastaff conflict also have importance for staff well-being. Overall, intrastaff conflict had consistent adverse associations with psychological distress and with physical health symptoms. Importantly, stress reactivity played an important role in staff well-being, as their reactivity to social conflict had the strongest association with all outcomes.
Social Conflict
Intrastaff conflict and reactivity to social conflict were associated with all adverse outcomes in this study. Conflict between staff adversely affected the well-being and perceived safety of employees, and the presence of conflict between patients and staff adversely impacted safety. Because prior research has suggested that the presence of social conflict is more influential than the presence of positive workplace relationships (Calabrese, 2000), only variables of adverse workplace experiences were included in this study. Intrastaff conflict and reactivity to social conflict had independent, direct associations with safety concerns, anger, and physical health. Regarding mental health, reactivity to social conflict moderated the impact of intrastaff conflict (as seen in Figure 1). As expected, those who are highly reactive to conflict and experienced conflict frequently, had the poorest mental health. This could indicate a personality trait of emotionality or, a lack of psychological hardiness or resilience. Those who were less reactive to conflict were not adversely affected by its presence.
In this study, the relationship of social conflict reactivity with well-being was straightforward. However, a previous study with an overlapping sample (Kelly et al., 2015) found that being less reactive to social conflict was associated with higher assault frequency. Previously, we speculated that this could indicate a lack of sensitivity to social cues or, alternatively, that these individuals were more likely to intervene in high conflict situations. Although highly reactive staff may be at lower risk for physical assault, reactivity to social conflict may have costs for their well-being. In the measure used in this study, highly reactive individuals report becoming highly upset and remaining so for prolonged periods when faced with conflict, whereas less reactive people indicate that they are unaffected or can “shrug off” conflict. The later might be thought to be similar to the concept of resilience. However, measures of resilience capture domains related to personal strength, adaptability and capacity for recovery that are not captured by the reactivity measure used in the present study (e.g., Conner & Davidson, 2003). In this context, the value of reactivity is ambiguous, as high reactivity may reflect being more sensitive to cues of interpersonal distress and perhaps patient needs but, may also confer vulnerability to distress. Further research is needed to elucidate the meaning of social conflict reactivity in a psychiatric setting.
Reactivity to social conflict did not differ across staff positions, nor was it correlated with years of experience, although female staff reported slightly more reactivity (gender was not significantly different across positions or years of experience). The presence of staff conflict was positively correlated with problematic patient behaviors, which suggests a feedback loop between intrastaff conflict and patient-staff conflict/assault that increases risk.
Patient Assault
Seventy percent of study participants reported having been assaulted during the previous year, comparable to what was found in three public California mental hospitals (SEIU, 2011). Experiencing patient assault was associated with feeling unsafe at work. A staff member’s reactivity to assault (independent of assault exposure) was not significantly related to his or her safety concerns or to physical health symptoms, which was not in accord with our hypothesis.
Patient assault was associated with anger and depression but, surprisingly, conflict with patients was not. Anger and depression may here be symptoms of a trauma response. Anger and depression were also related to intrastaff conflict. Assault may increase discord among staff or impair staff’s mental health and consequently make it more difficult for those impaired to work well with other staff.
The relationship between assault experiences and mental health (depression and anger) was complex, as it was moderated by the severity of individuals’ reactivity to assault. For those who were highly reactive to assault, depression and anger did not vary by assault frequency. However, among participants who were low in reactivity to assault, those having more frequent assault experiences reported more depression and anger than did those with fewer assault incidents (see Figure 2). These findings suggest that staff who report “low reactivity” to assault may, in many cases, be suppressing their stress reactions to being assaulted, for which there may be hidden mental health costs. Alternatively, some who are frequently assaulted may have difficulty recognizing their adverse reactions to assault, despite being more symptomatic or failing to connect their symptoms to assault experiences, or be a learned helplessness response to repeated assaults. Staff who report low reactivity to assault may be unaware of their distress, may be suppressing their distress, or may be providing socially desirable reports. Hospital managers might then be mindful that some staff members may suppress their reactivity to assault or be unaware of it, and thus may refrain from seeking support when assaulted. Future studies might explore whether these low assault reactivity findings are due to suppression or to poor self-monitoring.
Importance of Self-care
Although health habits were not the main focus of this study, they were significantly related to mental and physical health of staff. Staff who had poorer overall health maintenance habits in terms diet, exercise, alcohol, and caffeine consumption also had poorer well-being. Hospital management should find ways to encourage healthier lifestyles among their staff, perhaps offering programming that supports exercise individually or as a group, ensuring that healthier food is offered in cafeterias, encouraging staff to reduce high levels of alcohol and caffeine consumption, and providing holistic health care consultation. Investment in the health of staff could improve their well-being, as well as having indirect effects on morale and staff cohesion.
Limitations
This study was cross-sectional, therefore, inferences about whether conflict and assault cause the development of psychopathology, physical health problems, or safety concerns are limited. It is important to note that the directionality of the impact of stress reactivity and the experience of stressors in association with strain cannot be determined from a cross-sectional study, as stress responses change over time and are dependent on multiple, contextual variables. It is also unclear whether the timing of the assault experiences affected reports of well-being. Temporal distance from assault relative to participation in this study was not measured, and timing may have bearing on reports of well-being. A longitudinal study could more adequately investigate these issues. It is also important to consider potential confounders that could influence an individual’s stress reactivity. In this study we attempted to estimate the impact of engagement in self-care (health habits) that could diminish the magnitude of their stress responses, but future studies could include other important factors, such as social support.
Respondents were recruited from a single hospital in California, thus limiting the generalizability of results. However, the facility is a large long term care state hospital and may be representative of such institutions. The data from study participants may have been subject to sampling bias, as staff who elected to participate may be those most sensitized to assault experiences. Alternatively, those participating may have been motivated to underreport their issues with conflict and assault, so as to maintain a positive self-concept (Bem, 1967; French, Rogers, &, Cobb, 1974) and their self-image as effective mental health professionals. Further, on selection bias, staff who are unable to tolerate assault do not remain long in mental health institutions with high risk for assault and move to lower-risk settings. A single item was used to assess the presence of anger and future studies should use a more extensive measure. Lastly, only self-report data were collected. Future studies should include objective measures of patient assault and indicators of employee functioning, such as absenteeism and turnover.
Suggestions and Conclusions
Staff who remain in long term care hospitals or in acute psychiatric settings surely have some expectation of assault, perhaps even viewing it as inevitable (Chambers, 1998; Paterson, Leadbetter, & Bowie, 1999; Postner & Randell, 1993), but that sense of inevitability does not diminish their potential harm or the importance of developing protocols that improve safety. Hospital executive staff have long known that staff may not accurately report distress related to assault so as to deny being affected by something that is culturally considered part of the job, or as a way of coping in the desire to return to work (Chambers, 1998; Lanza, 1983; Lion et al., 1981; Needham et al., 2005). Therefore, supervisors need to monitor both the direct victims of assault and the unit as a whole, since witnessing an assault can also lead to trauma responses and contribute to perceptions that the workplace is unsafe.
In the present study, 45% reported feeling unsafe at work, and 90% thought that they could be more protected while at work. These findings are indicative of a general concern across psychiatric settings and the quest to improve safety protocols (Cornaggia et al., 2011; Mckenna et al., 2003; Whittington & Wykes, 1992; Wykes & Whittington, 1998). Despite most staff reporting resilience regarding their personal assaults, these findings suggest that there are serious concerns about safety within this setting and that require policy and procedural changes that will affect hospital operations.
Our study findings call attention to factors in the unit environment underlying both patient violence and staff conflict. A major function of management is to maintain a safe, civil environment. Patient and staff conflict are less likely to exist in a setting characterized by strong leadership, effective staffing practices, a culture of cohesiveness, and effective communication and structure (Bowers, 2009; Farrell, 1999). In such settings, assault (Farrell & Cubit, 2005) and intrastaff conflict (Dellasega, 2009) can be minimized. Although most hospitals have extensive safety protocols to protect against patient assault, intrastaff relationships are integral to successfully implementing safety protocols. Our results suggest that in the context of dealing with staff safety, intrastaff relationships have high relevance for staff well-being. To be sure, adequate training and support should be provided both to prevent and address assaultive incidents and to communicate that staff are valued (Nolan, Dallender, Soares, Thomsen, & Arnetz, 1999). Management should also strive to identify impaired interpersonal relationships, promote team building, offer plentiful support, provide education on conflict resolution, and create a collegial culture (Hamrin, Iennaco, & Olsen, 2009; Hutton, 2006; Whittington & Wykes, 1992).
Acknowledgments
We would like to thank Patton State Hospital for their participation. This study would not have been possible without the input and support of Carlos Luna, George Christison, Cindy Barrett, and the entire executive staff. Fellowship support was provided by the Clinical Translational Science Institute at the University of California, Los Angeles and the Los Angeles County Department of Mental Health. Erin Kelly’s contribution to this project was partially supported by grant UL1TR000124 from the National Center for Research Resources of the National Institutes of Health.
Footnotes
The content is solely the responsibility of the author and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
References
- Alexander J, Bowers L. Acute psychiatric ward rules: A review of the literature. Journal of Psychiatric and Mental Health Nursing. 2004;11:623–631. doi: 10.1111/j.1365-2850.2004.00770.x. [DOI] [PubMed] [Google Scholar]
- Arnetz JE, Arnetz BB. Violence towards health care staff and possible effects on the quality of patient care. Social Science & Medicine. 2001;52:417–427. doi: 10.1016/S0277-9536(00)00146-5. [DOI] [PubMed] [Google Scholar]
- Bem DJ. Self-perception: An alternative interpretation of cognitive dissonance phenomena. Psychological Review. 1967;74:183–200. doi: 10.1037/h0024835. [DOI] [PubMed] [Google Scholar]
- Bowers L. Association between staff factors and levels of conflict and containment on acute psychiatric wards in England. Psychiatric Services. 2009;60:231–239. doi: 10.1176/appi.ps.60.2.231. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG, Malarkey WB, Kiecolt-Glaser JK, Sheridan JF, Poehlmann KM, Glaser R. Autonomic, neuroendocrine, and immune responses to psychological stress: The reactivity hypothesisa. Annals of the New York Academy of Sciences. 1998;840(1):664–673. doi: 10.1111/j.1749-6632.1998.tb09605.x. [DOI] [PubMed] [Google Scholar]
- Calabrese KR. Interpersonal conflict and sarcasm in the workplace. Genetic, Social, and General Psychology Monographs. 2000;126:459–494. [PubMed] [Google Scholar]
- Caldwell MF. Incidence of PTSD among staff victims of patient violence. Hospital & Community Psychiatry. 1992;43:838–839. doi: 10.1176/ps.43.8.838. [DOI] [PubMed] [Google Scholar]
- Chambers N. ‘We have to put up with it—don’t we?’ The experience of being the registered nurse on duty, managing a violent incident involving an elderly patient: A phenomenological study. Journal of Advanced Nursing. 1998;27:429–436. doi: 10.1046/j.1365-2648.1998.00542.x. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression & Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Cornaggia CM, Beghi M, Pavone F, Barale F. Aggression in psychiatry wards: A systematic review. Psychiatry Research. 2011;189:10–20. doi: 10.1016/j.psychres.2010.12.024. [DOI] [PubMed] [Google Scholar]
- Crews DJ, Landers DM. A meta-analytic review of aerobic fitness and reactivity to psychosocial stressors. Medicine & Science in Sports & Exercise. 1987 [PubMed] [Google Scholar]
- Croker K, Cummings AL. Nurses’ reactions to physical assault by their patients. Canadian Journal of Nursing Research. 1995;27:81–93. [PubMed] [Google Scholar]
- Cunningham J, Connor DF, Miller K, Melloni RH., Jr Staff survey results and characteristics that predict assault and injury to personnel working in mental health facilities. Aggressive Behavior. 2003;29:31–40. doi: 10.1002/ab.10027. [DOI] [Google Scholar]
- Dellasega CA. Bullying among nurses. American Journal of Nursing. 2009;109:52–58. doi: 10.1097/01.NAJ.0000344039.11651.08. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Eller NH, Netterstrøm B, Gyntelberg F, Kristensen TS, Nielsen F, Steptoe A, Theorell T. Work-related psychosocial factors and the development of ischemic heart disease: A systematic review. Cardiology in Review. 2009;17:83–97. doi: 10.1097/CRD.0b013e318198c8e9. [DOI] [PubMed] [Google Scholar]
- Farrell GA. Aggression in clinical settings: Nurses’ views—A follow-up study. Journal of Advanced Nursing. 1999;29:532–541. doi: 10.1046/j.1365-2648.1999.00920.x. [DOI] [PubMed] [Google Scholar]
- Farrell G, Cubit K. Nurses under threat: A comparison of content of 28 aggression management programs. International Journal of Mental Health Nursing. 2005;14:44–53. doi: 10.1111/j.1440-0979.2005.00354.x. [DOI] [PubMed] [Google Scholar]
- Federenko IS, Schlotz W, Kirschbaum C, Bartels M, Hellhammer DH, Wust S. The heritability of perceived stress. Psychological Medicine. 2006;36:375–385. doi: 10.1017/S0033291705006616. [DOI] [PubMed] [Google Scholar]
- French JRP, Jr, Rodgers WL, Cobb S. Adjustment as person-environment fit. In: Coelho GV, Hamburg DA, Adams JE, editors. Coping and adaptation. New York, NY: Basic Books; 1974. pp. 316–333. [Google Scholar]
- Flannery RB, Jr, LeVitre V, Rego S, Walker AP. Characteristics of staff victims of psychiatric patient assaults: 20-year analysis of the Assaulted Staff Action Program. Psychiatric Quarterly. 2011;82:11–21. doi: 10.1007/s11126-010-9153-z. [DOI] [PubMed] [Google Scholar]
- Flannery RB, Jr, Wyshak G, Flannery GJ. Characteristics of international staff victims of psychiatric patient assaults: Review of published findings, 2000–2012. Psychiatric Quarterly. 2014 doi: 10.1007/s11126-014-9314-6. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Gerberich SG, Church TR, McGovern PM, Hansen HE, Nachreiner NM, Geisser MS, Watt GD. An epidemiological study of the magnitude and consequences of work related violence: The Minnesota Nurses’ Study. Occupational & Environmental Medicine. 2004;61:495–503. doi: 10.1136/oem.2003.007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg DP, Williams P. A user’s guide to the General Health Questionnaire. Windsor, United Kingdom: NFER-Nelson; 1988. [Google Scholar]
- Hamrin V, Iennaco J, Olsen D. A review of ecological factors affecting inpatient psychiatric unit violence: Implications for relational and unit cultural improvements. Issues in Mental Health Nursing. 2009;30:214–226. doi: 10.1080/01612840802701083. [DOI] [PubMed] [Google Scholar]
- Hardy GE, Shapiro DA, Haynes CE, Rick JE. Validation of the General Health Questionnaire-12: Using a sample of employees from England’s health care services. Psychological Assessment. 1999;11:159–165. doi: 10.1037/1040-3590.11.2.159. [DOI] [Google Scholar]
- Harrell E. Workplace Violence, 1993–2009: National Crime Victimization Survey and the Census of Fatal Occupational Injuries. US Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2011. Retrieved from http://www.bjs.gov/content/pub/pdf/wv09.pdf. [Google Scholar]
- Hegney D, Plank A, Parker V. Workplace violence in nursing in Queensland, Australia: A self-reported study. International Journal of Nursing Practice. 2003;9:261–268. doi: 10.1046/j.1440-172X.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- Hellzen O, Asplund K, Sandman PO, Norberg A. The meaning of caring as described by nurses caring for a person who acts provokingly: An interview study. Scandinavian Journal of Caring Sciences. 2004;18:3–11. doi: 10.1111/j.1471-6712.2004.00256.x. [DOI] [PubMed] [Google Scholar]
- Henderson AD. Nurses and workplace violence: Nurses’ experiences of verbal and physical abuse at work. Nursing Leadership. 2003;16(4):82–98. doi: 10.12927/cjnl.2003.16263. [DOI] [PubMed] [Google Scholar]
- Hunter M, Carmel H. The cost of staff injuries from inpatient violence. Hospital & Community Psychiatry. 1992;43:586–590. doi: 10.1176/ps.43.6.586. [DOI] [PubMed] [Google Scholar]
- Hutton SA. Workplace incivility: State of the science. Journal of Nursing Administration. 2006;36:22–27. doi: 10.1097/00005110-200601000-00006. [DOI] [PubMed] [Google Scholar]
- Ilies R, Johnson MD, Judge TA, Keeney J. A within-individual study of interpersonal conflict as a work stressor: Dispositional and situational moderators. Journal of Organizational Behavior. 2011;32:44–64. doi: 10.1002/job.677. [DOI] [Google Scholar]
- Ito H, Eisen SV, Sederer LI, Yamada O, Tachimori H. Factors affecting psychiatric nurses’ intention to leave their current job. Psychiatric Services. 2001;52:232–234. doi: 10.1176/appi.ps.52.2.232. [DOI] [PubMed] [Google Scholar]
- Jackson D, Clare J, Mannix J. Who would want to be a nurse? Violence in the workplace—A factor in recruitment and retention. Journal of Nursing Management. 2002;10:13–20. doi: 10.1046/j.0966-0429.2001.00262.x. [DOI] [PubMed] [Google Scholar]
- Jakulj F, Zernicke K, Bacon SL, van Wielingen LE, Key BL, West SG, Campbell TS. A high-fat meal increases cardiovascular reactivity to psychological stress in healthy young adults. The Journal of nutrition. 2007;137(4):935–939. doi: 10.1093/jn/137.4.935. [DOI] [PubMed] [Google Scholar]
- Jonker EJ, Goossens PJJ, Steenhuis HM, Oud NE. Patient aggression in clinical psychiatry: Perceptions of mental health nurses. Journal of Psychiatric and Mental Health Nursing. 2008;15:492–499. doi: 10.1111/j.1365-2850.2008.01261.x. [DOI] [PubMed] [Google Scholar]
- Karasek R, Baker D, Marxer F, Theorell T. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. American Journal of Public Health. 1981;71:694–705. doi: 10.2105/ajph.71.7.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly EL, Subica AM, Fulginiti A, Brekke JS, Novaco RW. A cross-sectional survey of factors related to inpatient assault of staff in a forensic psychiatric hospital. Journal of advanced nursing. 2015;71:1110–1122. doi: 10.1111/jan.12609. [DOI] [PubMed] [Google Scholar]
- Lanza ML. The reactions of nursing staff to physical assault by a patient. Hospital & Community Psychiatry. 1983;34:44–47. doi: 10.1176/ps.34.1.44. [DOI] [PubMed] [Google Scholar]
- Lanza ML, Kayne HL, Hicks C, Milner J. Nursing staff characteristics related to patient assault. Issues in Mental Health Nursing. 1991;12:253–265. doi: 10.3109/01612849109040519. [DOI] [PubMed] [Google Scholar]
- Lenehan GP, Turner JT. Treatment of staff victims of violence. In: Turner JT, editor. Violence in a medical care setting: A survival guide. Rockville, MD: Aspen Systems; 1984. pp. 251–260. [Google Scholar]
- Levin PF, Hewitt JB, Misner ST. Insights of nurses about assault in hospital-based emergency departments. Image: The Journal of Nursing Scholarship. 1998;30:249–254. doi: 10.1111/j.1547-5069.1998.tb01300.x. [DOI] [PubMed] [Google Scholar]
- Limm H, Angerer P, Heinmueller M, Marten-Mittag B, Nater UM, Guendel H. Self-perceived stress reactivity is an indicator of psychosocial impairment at the workplace. BMC public health. 2010;10(1):252. doi: 10.1186/1471-2458-10-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lion JR, Snyder W, Merrill GL. Underreporting of assaults on staff in a state hospital. Hospital & Community Psychiatry. 1981;32:497–498. doi: 10.1176/ps.32.7.497. [DOI] [PubMed] [Google Scholar]
- Love CC, Hunter ME. Violence in public sector psychiatric hospitals: Benchmarking nursing staff injury rates. Journal of Psychosocial Nursing and Mental Health Services. 1996;34:30–34. doi: 10.3928/0279-3695-19960501-15. [DOI] [PubMed] [Google Scholar]
- McKenna BG, Smith NA, Poole SJ, Coverdale JH. Horizontal violence: Experiences of registered nurses in their first year of practice. Journal of Advanced Nursing. 2003;42:90–96. doi: 10.1046/j.1365-2648.2003.02583.x. [DOI] [PubMed] [Google Scholar]
- Needham I, Abderhalden C, Halfens RJG, Fischer JE, Dassen T. Non-somatic effects of patient aggression on nurses: A systematic review. Journal of Advanced Nursing. 2005;49:283–296. doi: 10.1111/j.1365-2648.2004.03286.x. [DOI] [PubMed] [Google Scholar]
- Nolan P, Dallender J, Soares J, Thomsen S, Arnetz B. Violence in mental health care: The experiences of mental health nurses and psychiatrists. Journal of Advanced Nursing. 1999;30:934–941. doi: 10.1046/j.1365-2648.1999.01163.x. [DOI] [PubMed] [Google Scholar]
- Packard JS, Motowidlo SJ. Subjective stress, job satisfaction, and job performance of hospital nurses. Research of Nursing & Health. 1987;10:253–261. doi: 10.1002/nur.4770100408. [DOI] [PubMed] [Google Scholar]
- Paterson B, Leadbetter D, Bowie V. Supporting nursing staff exposed to violence at work. International Journal of Nursing Studies. 1999;36:479–486. doi: 10.1016/S0020-7489(99)00046-2. [DOI] [PubMed] [Google Scholar]
- Paterson B, McComish A, Aitken I. Abuse and bullying. Nursing Management (Harrow) 1997;3(10):8–9. doi: 10.7748/nm.3.10.8.s12. [DOI] [PubMed] [Google Scholar]
- Postner EC, Randell BP. It comes with the territory? Journal of Child and Adolescent Psychiatric Nursing. 1993;6(3):3–4. doi: 10.1111/j.1744-6171.1993.tb00164.x. [DOI] [PubMed] [Google Scholar]
- Richter D, Berger K. Post-traumatic stress disorder following patient assaults among staff members of mental health hospitals: a prospective longitudinal study. BMC psychiatry. 2006;6(1):15. doi: 10.1186/1471-244X-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossberg JI, Melle I, Opjordsmoen S, Friis S. The relationship between staff members’ working conditions and patients’ perceptions of the treatment environment. International Journal of Social Psychiatry. 2008;54:437–446. doi: 10.1177/0020764008090689. [DOI] [PubMed] [Google Scholar]
- Schlotz W, Yim IS, Zoccola PM, Jansen L, Schulz P. The Perceived Stress Reactivity Scale: Measurement invariance, stability, and validity in three countries. Psychological Assessment. 2011;23:80–94. doi: 10.1037/a0021148. [DOI] [PubMed] [Google Scholar]
- Schulz P, Jansen LJ, Schlotz W. Stressreaktivtät: Theoretiches Konzept und Messung [Stress reactivity: Theoretical concept and measurement] Diagnostica. 2005;51:124–133. doi: 10.1026/0012-1924.51.3.124. [DOI] [Google Scholar]
- Service Employees International Union 1000. [November 21 2014];Violence in California’s mental health hospitals: Workers deserve stronger protection [White paper] 2011 Retrieved from: http://seiu1000.org/research/research_white%20paper_dmhviolence.pdf.
- Spector PE, Zhou ZE, Che XX. Nurse exposure to physical and nonphysical violence, bullying, and sexual harassment: A quantitative review. International Journal of Nursing Studies. 2014;51:72–84. doi: 10.1016/j.ijnurstu.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Stewart WF, Ricci JA, Chee E, Morganstein D. Lost productive work time costs from health conditions in the United States: Results from the American Productivity Audit. Journal of Occupational and Environmental Medicine. 2003;45:1234–1246. doi: 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- Sullivan PJ. Occupational stress in psychiatric nursing. Journal of Advanced Nursing. 1993;18:591–601. doi: 10.1046/j.1365-2648.1993.18040591.x. [DOI] [PubMed] [Google Scholar]
- Whittington R, Richter D. Interactional aspects of violent behaviour on acute psychiatric wards. Psychology, Crime & Law. 2005;11(4):377–388. [Google Scholar]
- Whittington R, Wykes T. Staff strain and social support in a psychiatric hospital following assault by a patient. Journal of Advanced Nursing. 1992;17:480–486. doi: 10.1111/j.1365-2648.1992.tb01933.x. [DOI] [PubMed] [Google Scholar]
- Wilsnack SC, Klassen AD, Wilsnack RW. Drinking and reproductive dysfunction among women in a 1981 national survey. Alcoholism: Clinical and Experimental Research. 1984;8:451–458. doi: 10.1111/j.1530-0277.1984.tb05700.x. [DOI] [PubMed] [Google Scholar]
- Wykes T, Whittington R. Prevalence and predictors of early traumatic stress reactions in assaulted psychiatric nurses. Journal of Forensic Psychiatry. 1998;9:643–658. doi: 10.1080/09585189808405379. [DOI] [Google Scholar]
- Yassi A. Assault and abuse of health care workers in a large teaching hospital. Canadian Medical Association Journal. 1994;151:1273–1279. [PMC free article] [PubMed] [Google Scholar]