Abstract
The processes for implementing effective programs at scale in low-income countries have not been well-documented in the peer-reviewed literature. This article describes the initial steps taken by one such program—the BRAC Manoshi Project, which now reaches a population of 6.9 million. The project has achieved notable increases in facility births and reductions in maternal and neonatal mortality. The focus of the paper is on the initial steps—community engagement, social mapping, and census taking. Community engagement began with (1) engaging local leaders, (2) creating Maternal, Neonatal, and Child Health Committees for populations of approximately 10,000 people, (3) responding to advice from the community, (4) social mapping of the community, and (5) census taking. Social mapping involved community members working with BRAC staff to map all important physical features that affect how the community carries out its daily functions—such as alleys, lanes and roads, schools, mosques, markets, pharmacies, health facilities, latrine sites, and ponds. As the social mapping progressed, it became possible to conduct household censuses with maps identifying every household and listing family members by household. Again, this was a process of collaboration between BRAC staff and community members. Thus, social mapping and census taking were also instrumental for advancing community engagement. These three processes—community engagement, social mapping, and census taking—can be valuable strategies for strengthening health programs in urban slum settings of low-income countries.
Keywords: Community health, Primary health care, Urban health, Slums, Maternal health, Neonatal health, Child health, Bangladesh
Introduction
Developing effective health systems for low-income populations in urban areas is a global priority. For the first time, a majority (54 %) of the world’s population is urban, as is 30 % of the population of low-income countries.1 By 2050, the percentage of the population of low-income countries living in urban areas is expected to reach 48 %.1
Along with rapid urbanization in low-income countries, urban poverty will also grow. In 2012, 863 million people were living in slums or informal settlements (characterized by housing that is non-durable or overcrowded, or that lacks access to improved water and sanitation or security against eviction).2 Almost half of urban residents in less-developed regions live in slums compared to 6 % in more-developed regions.3 The world’s total slum population is expected to reach 1 billion by 2020.4
In addition to coping with poor standards of living, slum dwellers face worse health conditions than their other urban counterparts, which Millennium Development Goal 7D acknowledges.5 Moreover, despite living in close proximity to health services, slum dwellers consistently utilize these services at disproportionately low rates.6–10
Just as slum residents face difficulties accessing services, so do programs have difficulty serving these populations. Many of these difficulties arise from characteristics unique to slums. Slum residents are often highly transient, lack formal addresses, and have numerous health problems arising from overcrowding, poor hygiene, extreme poverty, and hesitancy to seek medical care.11–14 Even governments that prioritize serving the poor often have difficulty creating programs that can effectively reach this highly mobile, dense, socio-culturally heterogeneous population.15–17 Furthermore, the authority of urban municipalities often overlaps with that of national ministries of health, leading to weak governmental health infrastructure and patient reliance on an uncoordinated, poorly regulated “mish-mash” of private and non-governmental organization (NGO) providers.
Health programs for urban slums need models of effective engagement with communities that make it possible to develop sustainable and globally replicable health services at scale. This paper describes the approach used by one large-scale health program to establish a working relationship with slum communities in Bangladesh that made it possible to scale up an effective program.
The BRAC Manoshi Project
BRAC (initially the Bangladesh Rural Advancement Committee, but now simply BRAC) is the largest NGO in the world in terms of population reached. Its intersectoral programs for alleviating poverty and empowering women now reach more than 138 million people in 12 different countries across Asia, Africa, and Haiti. It is also the largest national NGO program in the world: its Bangladesh program reaches 120 million people.18
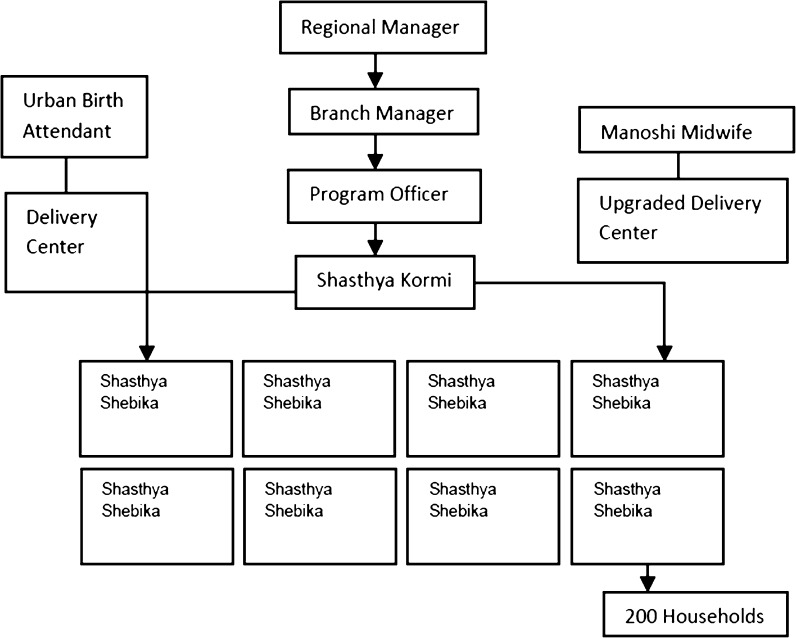
The BRAC Manoshi Project, started in 2007, provides community-based maternal, neonatal, and child health care for 6.9 million urban slum dwellers in Bangladesh. Services are provided by a dual cadre of community health workers (CHWs)—Shasthya Shebikas (SSs) and their supervisors, Shasthya Kormis (SKs)—as well as urban birth attendants (UBAs) who work in BRAC delivery centers in the slums. One SS is responsible for approximately 200 households, each of which she visits monthly. She provides health education, treatment for common illnesses, and referrals for complex cases. She promotes family planning and asks about possible pregnancy. She notifies her supervising SK of any new pregnancies, and the SK provides home-based prenatal care. In addition to providing home-based prenatal care, SKs visit every home once every 3 months and update the census information for the home. SSs and SKs are supported by three levels of supervision (Fig. 1).
FIG. 1.
Organizational structure of the BRAC Manoshi Project.
The BRAC Manoshi Project reaches women living in the slums at a low cost and with minimal infrastructure. Most BRAC delivery centers are two-room concrete former homes with no special equipment. The project’s other main “infrastructure” is social—(1) community engagement and support, and (2) the attitudes, knowledge and practices of the mothers in community and their families.
At the project’s inception, the service area had high maternal and neonatal mortality—a maternal mortality ratio (MMR) of 294 per 100,000 live births and a neonatal mortality rate (NMR) of 43 per 1000 live births.19 Most women (86 %) delivered at home; only a quarter received antenatal and postnatal care.14 Six years into the project, 87 % of women delivered at a facility; the MMR and NMR declined by 56 and 60 %, respectively.20
These outcomes are superior to national trends. Nationally, the MMR and NMR have declined by 40 and 14 %, respectively, over 9 years.20,21 Even though the national MMR in 2010 had fallen to 194 per 100,000, it remained higher than the BRAC Manoshi Project service area MMR of 130.22 In 2011, 71 % of newborns were delivered at home nationally compared to only 13 % in the Manoshi Project area after project implementation.21
Relevance as a Model Program for Urban Slum Health
Overall, the BRAC Manoshi Project demonstrates impressive results with respect to expanding access to care as well as reducing mortality (Table 1). Notably, the reverse is usually true: slum populations have worse health than the country as a whole. As the poor around the world shift from rural villages to urban slums, the achievements of the BRAC Manoshi Project have significant policy implications, as it is one of the world’s few successful and sustainable large-scale community-based urban slum health projects.
TABLE 1.
Maternal and neonatal health indicators in the BRAC Manoshi Project area versus Bangladesh overall
| Percentage of deliveries performed in facilities, including in Birth Huts (year) | Maternal mortality ratio (maternal deaths per 100,000 live births) (year) | Neonatal mortality rate (neonatal deaths per 1,000 live births) (year) | ||||
|---|---|---|---|---|---|---|
| Bangladesh | Manoshi Project Area | Bangladesh | Manoshi Project Area | Bangladesh | Manoshi Project Area | |
| Baseline | 15 % (2007) | 16 % (2008) | 322 (2001) | 294 (2008) | 37 (2007) | 43 (2008) |
| Endline | 29 % (2011) | 87 % (2013) | 194 (2010) | 130 (2013) | 32 (2011) | 17 (2013) |
Sources: 1–5
1. NIPORT, Mitra and Associates, Macro International. Bangladesh Demographic and Health Survey 2007. Dhaka, Bangladesh and Calverton, Maryland: National Institution of Population and Research Training, Mitra and Associates, and Macro International, 2009
2. NIPORT, Mitra and Associates, ICF International. Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh, Dhaka, Bangladesh, Calverton, MD: National Institute of Population Research and Training, Mitra and Associates, ORC Macro; 2013
3. ORC Macro, ICDDR B. Bangladesh Maternal Health Services and Maternal Mortality Survey 2001. . Calverton, MD and Dhaka, Bangladesh: ORC Macro and ICDDR, B, 2003
4. Manoshi Project. Manoshi Internal Data Report, 2012. Dhaka, Bangladesh: BRAC, 2013
5. Manoshi Project. Manoshi Internal Data Report, 2013. Dhaka, Bangladesh: BRAC, 2014
Although prior evidence exists that community-based maternal, neonatal, and child health programs improve health,23–26 most programs have been rural and have had a more vertical focus,25–29 with limited published information on their implementation strategies. Two successful, comprehensive rural programs that have detailed their implementation strategies are the Rwandan national CHW program,30,31 and the home-based neonatal care program of SEARCH in central India.32 Thus, the BRAC Manoshi Project’s methods in community engagement, social mapping, and census taking provide important lessons for improving maternal, neonatal, and child health in urban slum health projects at scale.
Methods
We conducted a literature search of the published and gray literature for background information on (1) methods used to establish community health programs and (2) the success of these programs in both rural and urban settings. Search terms used individually and collectively were as follows: community mapping, health equity, community asset mapping, community census, maternal health services, community census, maternal health system, and community-based, impact-oriented.
One of us (LM) then conducted semi-structured interviews in January 2013 with six BRAC employees who were involved in the initial stages of the BRAC Manoshi Project. These interviews focused on the methods used during implementation and on the staff members’ perspectives on the advantages and disadvantages of each. One of these interviews was with a staff member who also works predominately with BRAC’s rural maternal, neonatal, and child health programs. This interview gave us insight into some key differences between rural and urban programs. Upon completion, we examined the interview content for themes. Additionally, we examined existing internal documents (census forms, social maps, and working briefs) and participated in a site visit to the Korail slum of Dhaka to corroborate the information gained from interviews. On the site visit, we met with a Branch Manager, a Program Organizer, a SK, and women enrolled in the project. Informal conversations with them further informed our analysis. This work was deemed “Not Human Subjects Research” by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Results
Community Engagement
Community engagement began with BRAC Manoshi staff meeting with local community leaders and representatives of the city council (elected local government bodies of the city corporations), and forming Maternal, Neonatal, and Child Health (MNCH) Committees (described further below) with them based on discussions with them. The community health workers were initially selected through BRAC’s other local platforms, such as micro-credit groups and parents’ groups for BRAC’s Education Programme. Gradually, BRAC was able to build trust with local leaders and community members as these activities continued, as social mapping and census taking progressed, and as cyclical feedback from the community led to stronger community engagement (Table 2). Although the effort was led by BRAC, over time, more initiative has come from the community. For example, women actively referred other women to use BRAC/Manoshi services, members of the MNCH Committees became more active (including monitoring of program activities and carrying out social autopsies on all maternal deaths and selected neonatal deaths), and as women’s groups developed their own funds to help pay for the expenses of women who required hospitalization for delivery complications.
TABLE 2.
Community engagement methods used by the BRAC Manoshi Project
| Approach | Timeline | Benefit |
|---|---|---|
| Timely initiation of services | As soon as possible | Trust building with the community when services begin, without too much delay or assessment |
| Formation of Maternal, Neonatal, and Child Health (MNCH) Committees | Ongoing (bimonthly meetings) | Forum for community feedback |
| Local leader buy-in | ||
| Open communication | ||
| Establishment of legitimacy of the program with community members | ||
| Mass marketing | Several months prior to and after program implementation | Preparation of clients for program initiation |
| Receptiveness of prime clients to program services | ||
| Social mapping and census taking | First month of program | Familiarization of clients with program workers |
| Trust building | ||
| Genuine responsiveness to community feedback | Ongoing | Establishment of trust between the program and the community |
| Adaptation of services to meet community needs | ||
| Incorporation of local resources | At outset, revised as needed | Provision of culturally acceptable care |
To build trust, BRAC initiated the service provision quickly, with the plan to adjust program focus later as needed. Local slum dwellers noted they had encountered numerous pilot programs that suddenly stopped service provision. This pattern had created suspicion among community members. As one BRAC staff member noted, “They wanted to understand why we are here. Everybody comes, talks, but does nothing.”
Thus, to gain trust, BRAC found it important to first prove to the community that BRAC was serious about scaling their pilot program. Once the community members experienced benefits from the program, they became more willing to engage.
After service initiation, BRAC focused on creating Maternal, Neonatal, and Child Health (MNCH) Committees for defined geographic areas of approximately 10,000 people. Each committee consists of 9–11 local leaders from multiple sectors such as government, education, business, and religion. These committees provided indispensable guidance and legitimacy for the project from the perspective of the community. One BRAC staff member noted, “A good quality MNCH committee [is essential] because this committee helped us select surveyors, some [of whom] actually became Shasta Kormis.” These Committees knew which individuals would be acceptable to the community as surveyors for mapping and census taking. The Committees met bimonthly, with BRAC staff in attendance. During these meetings, BRAC updated the community about activities and progress, and the Committee gave feedback about problems. More recently, MNCH Committees have taken the responsibility of carrying out social autopsies of all maternal deaths and selected neonatal deaths that occur in their jurisdiction as well as reviewing the outcomes of births and referrals of women with obstetrical complications. This engages the community in real issues of program operations and approaches to program strengthening.
Prior to project implementation, BRAC provided information about the project through mass media channels accessible to slum dwellers. In Bangladesh, most market shops have small TVs, which are popular to watch. BRAC ran paid project advertisements, which familiarized slum dwellers with both the BRAC logo and message. Consequently, people were more receptive to the program at its inception.
BRAC found that incorporating traditional practices into project services further increased community engagement. For instance, traditional birth attendants (TBAs) are women lacking formal training but with much experience attending deliveries. They are an integral part of birthing in Bangladesh. BRAC decided to incorporate them into the project as trained UBAs instead of trying to remove them, which might have caused community resistance. BRAC has found that women are more comfortable utilizing its services when UBAs with whom they are already familiar provide care.
Both social mapping and census taking are a means of community engagement, valuable in its own right but also a means to obtain important programming information. Through these processes, the communities became familiar with the project and experienced BRAC’s commitment to understanding their needs. BRAC found that having key community leaders intermittently present alongside the surveyors further increased acceptance of the social mapping and census-taking activities.
Despite all these efforts, BRAC found that uptake of services was low at the outset. Instead of being discouraged, BRAC used a cyclical process of feedback to encourage community engagement. Through continued conversations with the community and establishing relationships with the families, slum dwellers observed that the program was committed to responding to their feedback and to providing quality services. Ultimately, service uptake increased substantially over time.
Social Mapping
BRAC staff consistently emphasized that the key aspects of social mapping were training staff, using a systematic method, identifying community resources, and involving the community when possible (Table 3). BRAC’s mapping team consisted of several levels of staff: surveyors, who were carefully selected by community members, along with BRAC Program Officers and Branch Managers. Aside from their supervisory roles, personnel at both levels were closely involved in the social-mapping and census-taking processes. Monitoring and evaluation staff oversaw the entire process.
TABLE 3.
Methods in social mapping used by the BRAC Manoshi Project
| Approach | Timeline | Benefit |
|---|---|---|
| Training of surveyors, Program Officers, Branch Managers to carry out social mapping | At outset | Consistent and high-quality mapping procedures |
| Key informant identification | Beginning of mapping | Provides early guidance on slum layout and key features |
| Household list creation | Beginning of mapping | Familiarizes staff with slum layout |
| Ensures no households are missing from the map | ||
| Decisions on level of detail and household representation on map | Beginning of mapping | Maximizes visual utility of map |
| Standardize data collection | Ensures no households are missing from the map | |
| Mapping of houses and other facilities in a systematic manner | After above steps are complete | Facilitates the planning of services to be as accessible as possible |
| Consultation with households to verify map accuracy | After draft of map is complete | Community engagement |
| Enhanced accuracy |
Social mapping of the slum community included mapping homes as well as community structures such as roads, schools, mosques, markets, pharmacies, health facilities, latrines, and ponds—any important community structures or physical feature that may impact the community’s daily functions. Special symbols were used to represent these facilities and landmarks in a clear manner on the map.
Program staff found key informants, who provided a basic overview of the layout of the slum, special landmarks, and its boundaries. However, because Bangladeshi slums have large populations, key informants did not know every household. As a result, before mapping, staff first created a household list by going briefly from house to house, enumerating each household, and writing down the household number on the outside of the house after obtaining consent. They also wrote down on a register the name of the head of household and the number of individuals in the household. This list was important for two reasons. It created an accurate account of who exactly lived in the slum, and it gave the staff an overview of the layout of the slum.
At this point, mapping began. BRAC staff started at the northwest corner of the slum, following a written protocol, which helped avoid missing houses. This process later helped SSs, SKs, and residents learn their house numbers. Even though residents memorized their house number over time, BRAC felt that it is important to keep this information readily visible to all so that when changes in house occupants and program staff occurred, the information would be preserved. Visibly marking houses also made monitoring and evaluation efforts easier. For household-based maps, BRAC assigned every household its own number. Commonly, different families live within the same house; each was assigned a specific letter (e.g., 10/a, 10/b, etc.). This system allowed flexibility as families moved.
While conducting the survey, the surveyor simultaneously drew the map, including house and family numbers, clearly on a piece of paper with a pencil. BRAC staff emphasized that these drawings had to occur in real time. Otherwise, important details would have been lost if surveyors had attempted to draw the map later from memory. Each surveyor and team carried a copy of the map symbols with them to facilitate standardization as they mapped. After drawing each section of the map, surveyors consulted with residents to ensure no households were missed. As slums are large, each team of surveyors mapped its own section. Program Officers and Branch Managers then compiled all maps, with the input of the surveyors, to make a final master map. Staff compared the household listing to the social map to make sure they matched. If not, staff returned to the area to resolve any discrepancies.
Census Taking
A strong training system and consistent supportive oversight were two main areas BRAC staff identified as key to the success of census taking during the initial stages of project implementation (Table 4). The staff members who conducted the census were the same as those who did the social mapping: surveyors, Program Officers, and Branch Managers. The surveyors, who went house to house to conduct the census, were selected by the MNCH Committees. In areas where BRAC had pre-existing CHWs who were literate, the project recruited them as surveyors. This approach was beneficial since these CHWs and the communities were already familiar with each other.
TABLE 4.
Methods in census taking used by the BRAC Manoshi Project
| Approach | Timeline | Benefit |
|---|---|---|
| Selection of census takers with the assistance of the MNCH Committee | At outset | Utilization of existing CHW resources |
| Collaboration with MNCH Committee to promote community engagement | ||
| Training of census takers, Program Officers, and Branch Managers | At outset | Standardization of information collected |
| Conduct of census | Over a 1–2 month time period | Specification of program population (age and sex, household location, as well as other socio-demographic household information) |
| Assistance with needs assessment and allocation of program resources | ||
| Baseline data for monitoring and evaluation | ||
| Monitoring of census-taking process | During census taking | Quality assurance |
Surveyor qualifications included literacy and the ability to correctly fill out forms. A sub-set of surveyors who did a particularly good job were offered a position as a SK. The incentive for surveying was 5 taka (0.06 US dollars) per household survey, with a maximum of 25 households daily.
BRAC conducted a 2-day training for surveyors. First, though, BRAC conducted a 1-day training for the Program Officers, Branch Managers, and senior management.
During the training, Program Officers first explained the nature of and reason for the census to the surveyors. Next, they ensured the surveyors could both record the information and compile data correctly. Surveyors practiced these skills in the field and then reviewed the experience in the classroom to learn from their errors and experience. After completing their training, surveyors were assigned to a geographic area and given a schedule with an expected date for completion. The Branch Manager for the project and the Program Officer from the Monitoring Unit of the project supervised the survey activities. Program Officers compiled the data.
The information collected in the household census focused on demographic and economic information. Questions included the number of births and deaths in the previous year, number of people in the family who are in the target population (children younger than 5 years of age, pregnant women, lactating women, married couples, newly married couples, and women of reproductive age), and economic status of the family (“ultra poor” <5000 taka or 64 US dollars of family income per month, “poor” 5–10,000 taka or 64–128 US dollars per month, and “not poor” >10,000 taka or 128 US dollars per month).
BRAC monitored data collection during the census process. The Program Officers from the Monitoring Unit randomly selected 5 % of households to re-survey as well as at least three households per surveyor. Additionally, the Branch Manager monitored 5 % of the 5 % of households that the Program Officer monitored. If they uncovered problems with the collected information, they discussed these discrepancies with the surveyors and their supervisors.
Maintaining confidentially during census taking was essential to the success of the process. Pregnancy status and economic status were the most sensitive for the slum populations. For this information, it was important to assure households that it would remain confidential.
Discussion
The BRAC Manoshi Project used community engagement, social mapping, and census taking as initial steps in creating an effective maternal, neonatal, and child health project with strong local ownership and long-term sustainability. These effective methods should be considered for all urban slum health programs that seek to achieve impact through community-based programming.
Benefits of Community Engagement, Social Mapping, and Census Taking in Slum Communities
One important benefit of community engagement is enhanced communication, which improves project functioning. One of many examples is cited here. Through community engagement with MNCH Committees, BRAC found that many women desired a higher-level health worker than a UBA at delivery centers.33,34 The MNCH Committees also expressed their dissatisfaction with high rates of hospital referral, which were necessary because UBAs were not trained to handle complications.35 In response, BRAC piloted upgraded delivery centers (BRAC Maternity Centers), staffed by trained midwives who could handle more complicated cases. Unlike at the BRAC Delivery Centers manned by UBAs where the services are free, BRAC Maternity Centers charge a small fee for services and are designed to be sustainable with locally generated resources. Although still in the pilot stage, these centers are already quite popular, reflecting that responding to community feedback can contribute to project quality improvements.
Like community engagement, social mapping provides benefits that improve program functioning. Knowing the location of people, roads, and facilities in the slum allowed BRAC to place delivery centers at central locations to minimize walking distances. Of particular importance was locating birthing centers in areas that do not require women to cross bridges and that provide ready access to transport for referral of patients with complications. Local cultural beliefs as well as practical realities lead women to fear crossing bridges, particularly at night, and to deliver close to home.36,37
Census taking also provides many benefits to project functioning. It provides accurate information about the service population and this, in turn, enables the project to allocate financial and human resources appropriately. For example, the project also used this population data to calculate how many SSs, SKs, and UBAs it needed and where it would need them.
Both census taking and social mapping are powerful tools in and of themselves for community engagement.38 They provide the opportunity to visit families in their homes and to speak to gatekeepers such as the head of household and older women as well as the women of reproductive age, thereby giving families a chance to learn about the project. BRAC has found that having the opportunity for men and older women to meet with Manoshi staff when they come by for the census can be the first step toward building community support for the program.
Community engagement, social mapping, and census taking have all enabled BRAC to better advocate for the slum populations with the government and donors, to better plan project activities, and to build community support.
Challenges of Community Engagement, Social Mapping, and Census Taking in Slum Communities
These methods are not without their challenges, however. Slum populations are highly transient; migration within the slum, to other slums, and back to home villages are common. BRAC staff estimate that, within a given year, 20–40 % of a given slum’s population relocates. Furthermore, slums are often located on public property or occupied private property, making it impossible for slum dwellers to own their houses and discouraging long-term residence.
Social mapping is challenging not only because of migration of inhabitants but also because of the constant remolding of slums in response to recurrent flooding, new construction, and intermittent demolition. Thus, a map created one day will not necessarily be accurate the next.
Generally speaking, the processes of community engagement, social mapping, and census taking are not commonly undertaken at the outset of most health programs in urban slum communities. The pioneering experience of the BRAC Manoshi Project with these processes can aid other emerging programs. A field guide is now available that describes these processes in greater detail.39
The first steps taken by the BRAC Manoshi Project have led to an increasingly sustainable large-scale program that continues to provide services to an urban population in Bangladesh of 6.9 million people as of 2014, including 1.8 million women of reproductive age and 191,631 newly pregnant women. The program continues to grow and expand to smaller city corporations and urban municipalities. A social enterprise model is emerging that will enable the program to be self-sustaining but will not compromise its social impact. As residents gain trust in the services and their high quality of care, they are more willing to pay for services provided by the Project and less likely to for services provided by drug sellers and local independent practitioners (whose fees are often substantially higher than those of the Project). In addition, new services are slowly being added to the program in pilot sites that can generate profits to help sustain the overall program, including eye care services and care of chronic diseases. However, steps are being taken to ensure that the poorest members of the population will be able to receive free services. BRAC is committed to sustaining these services and is, in addition, introducing and expanding its other programs into the service area, including women’s savings groups/microfinance, primary schools, adolescent development programs, as well as programs for community empowerment, human rights, and gender diversity.
Conclusion
As the world’s population becomes increasingly urbanized, finding new and effective ways to build low-cost, high-quality health systems for low-income populations is essential. The processes of social engagement, social mapping, and census taking can provide a foundation for an effective program. The skills and experience that BRAC has developed obtained can benefit other programs serving the expanding urban slum populations of the world. BRAC’s methods of community engagement, social mapping, and census taking are practical and feasible. They provide an excellent starting point.
Acknowledgments
We thank the people of slum communities in Bangladesh and the staff of the BRAC Manoshi Project for their assistance in gathering the information used for this article. We also thank the Lipitz Public Health Policy Fund for its support of Dr. Marcil’s participation in this study. The Bill & Melinda Gates Foundation provided funding from 2007 to 2011 for the BRAC Manoshi Project.
Abbreviations
- BRAC
Formerly Bangladesh Rural Advancement Committee
- CHWs
Community health workers
- NGO
Non-governmental organization
- SSs
Shasthya Shebikas
- SKs
Shasthya Kormis
- UBAs
Urban birth attendants
References
- 1.UN. World Urbanization Prospects: the 2014 Revision, (ST/ESA/SER.A/366). 2015. Available at http://esa.un.org/unpd/wup/FinalReport/WUP2014-Report.pdf. Accessed Dec 20 2015.
- 2.United Nations. The Millennium Development Goals Report 2014. 2014. Available at http://www.un.org/millenniumgoals/2014%20MDG%20report/MDG%202014%20English%20web.pdf. Accessed Dec 20 2015.
- 3.UN-Habitat. The Challenge of Slums: Global Report on Human Settlements 2003. 2003. http://www.unhabitat.org.jo/pdf/GRHS.2003.pdf. Accessed Dec 20 2015.
- 4.UN. Population Distribution, Urbanization, Internal Migration and Development: an International Perspective. 2011. Available at http://www.un.org/esa/population/publications/PopDistribUrbanization/PopulationDistributionUrbanization.pdf. Accessed Dec 20 2015.
- 5.UN. End Poverty: Millennium Development Goals and Beyond 2015. Goal 7. Environmental Sustainability 2014. Available at http://www.un.org/millenniumgoals/environ.shtml. Accessed Dec 20 2015.
- 6.Prakash R, Kumar A. Urban poverty and utilization of maternal and child health care services in India. J Biosoc Sci. 2013;45(4):433–49. doi: 10.1017/S0021932012000831. [DOI] [PubMed] [Google Scholar]
- 7.Yuan B, Qian X, Thomsen S. Disadvantaged populations in maternal health in China who and why? Global Health Action. 2013;6:19542. doi: 10.3402/gha.v6i0.19542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vasquez F, Paraje G, Estay M. Income-related inequality in health and health care utilization in Chile, 2000–2009. Rev Panam Salud Publica. 2013;33(2):98–106. doi: 10.1590/S1020-49892013000200004. [DOI] [PubMed] [Google Scholar]
- 9.Zhao Q, Huang ZJ, Yang S, Pan J, Smith B, Xu B. The utilization of antenatal care among rural-to-urban migrant women in Shanghai: a hospital-based cross-sectional study. BMC Public Health. 2012;12:1012. doi: 10.1186/1471-2458-12-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zyaambo C, Siziya S, Fylkesnes K. Health status and socio-economic factors associated with health facility utilization in rural and urban areas in Zambia. BMC Health Serv Res. 2012;12:389. doi: 10.1186/1472-6963-12-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emina J, Beguy D, Zulu EM, et al. Monitoring of health and demographic outcomes in poor urban settlements: evidence from the Nairobi Urban Health and Demographic Surveillance System. J Urban Health: Bull New York Acad Med. 2011;88(Suppl 2):S200–18. doi: 10.1007/s11524-011-9594-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Islam MM, Azad KM. Rural–urban migration and child survival in urban Bangladesh: are the urban migrants and poor disadvantaged? J Biosoc Sci. 2008;40(1):83–96. doi: 10.1017/S0021932007002271. [DOI] [PubMed] [Google Scholar]
- 13.Hazarika I. Women’s reproductive health in slum populations in India: evidence from NFHS-3. J Urban Health: Bull New York Acad Med. 2010;87(2):264–77. doi: 10.1007/s11524-009-9421-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moran AC, Choudhury N, Uz Zaman Khan N, et al. Newborn care practices among slum dwellers in Dhaka, Bangladesh: a quantitative and qualitative exploratory study. BMC Pregnancy Childbirth. 2009;9:54. doi: 10.1186/1471-2393-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khatun F, Rasheed S, Moran AC, et al. Causes of neonatal and maternal deaths in Dhaka slums: implications for service delivery. BMC Public Health. 2012;12:84. doi: 10.1186/1471-2458-12-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.More NS, Bapat U, Das S, et al. Community mobilization in Mumbai slums to improve perinatal care and outcomes: a cluster randomized controlled trial. PLoS Med. 2012;9(7) doi: 10.1371/journal.pmed.1001257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zulu EM, Beguy D, Ezeh AC, et al. Overview of migration, poverty and health dynamics in Nairobi City’s slum settlements. J Urban Health: Bull New York Acad Med. 2011;88(Suppl 2):S185–99. doi: 10.1007/s11524-011-9595-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.BRAC. BRAC Annual Report, 2014. 2014. Available at http://www.brac.net/sites/default/files/ar2014/BRAC-annual-report-14.pdf. Accessed Dec 20 2015.
- 19.Manoshi Project . Manoshi Internal Data Report, 2012. Dhaka, Bangladesh: BRAC; 2013. [Google Scholar]
- 20.Manoshi Project . Manoshi Internal Data Report, 2013. Dhaka, Bangladesh: BRAC; 2014. [Google Scholar]
- 21.National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. Bangladesh Demographic and Health Survey 2014: Key Indicators. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT, Mitra and Associates, and ICF International; 2015.
- 22.Streatfield P, Arifeen S. Bangladesh Maternal Mortality and Health Survey 2010. Dhaka, Bangladesh: icddr,b; 2010. [Google Scholar]
- 23.Quayyum Z, Khan MN, Quayyum T, Nasreen HE, Chowdhury M, Ensor T. “Can community level interventions have an impact on equity and utilization of maternal health care”—evidence from rural Bangladesh. Int J Equity Health. 2013;12:22. doi: 10.1186/1475-9276-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Darmstadt GL, Lee AC, Cousens S, et al. 60 Million non-facility births: who can deliver in community settings to reduce intrapartum-related deaths? Int J Gynaecol Obstet. 2009;107(Suppl 1):S89–112. doi: 10.1016/j.ijgo.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Littrell M, Moukam LV, Libite R, Youmba JC, Baugh G. Narrowing the treatment gap with equitable access: mid-term outcomes of a community case management program in Cameroon. Health Policy Plan. 2013;28(7):705–16. doi: 10.1093/heapol/czs110. [DOI] [PubMed] [Google Scholar]
- 26.le Roux IM, Tomlinson M, Harwood JM, et al. Outcomes of home visits for pregnant mothers and their infants: a cluster randomized controlled trial. AIDS. 2013;27(9):1461–71. doi: 10.1097/QAD.0b013e3283601b53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nsona H, Mtimuni A, Daelmans B, et al. Scaling up integrated community case management of childhood illness: update from Malawi. Am J Trop Med Hyg. 2012;87(5 Suppl):54–60. doi: 10.4269/ajtmh.2012.11-0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kisia J, Nelima F, Otieno DO, et al. Factors associated with utilization of community health workers in improving access to malaria treatment among children in Kenya. Malar J. 2012;11:248. doi: 10.1186/1475-2875-11-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith JM, Gubin R, Holston MM, Fullerton J, Prata N. Misoprostol for postpartum hemorrhage prevention at home birth: an integrative review of global implementation experience to date. BMC Pregnancy Childbirth. 2013;13:44. doi: 10.1186/1471-2393-13-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farmer PE, Nutt CT, Wagner CM, et al. Reduced premature mortality in Rwanda: lessons from success. BMJ. 2013;346:f65. doi: 10.1136/bmj.f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mugeni C, Levine AC, Munyaneza RM, et al. Nationwide implementation of integrated community case management of childhood illness in Rwanda. Global Health, Sci Pract. 2014;2(3):328–41. doi: 10.9745/GHSP-D-14-00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bang AT, Bang RA. Background of the field trial of home-based neonatal care in Gadchiroli, India. J Perinatol. 2005;25(Suppl 1):S3–10. doi: 10.1038/sj.jp.7211267. [DOI] [PubMed] [Google Scholar]
- 33.Mridha MK, Hossain A, Alam B, et al. The Perceptions of Community Groups to Improve MNCH in Urban Slums: an Exploratory Case Study of Korail Slum in Dhaka. Dhaka, Bangladesh: icddr,b and BRAC; 2009. [Google Scholar]
- 34.Ahmed SM, Hossain A, Khan MA, et al. Using formative research to develop MNCH programme in urban slums in Bangladesh: experiences from MANOSHI, BRAC. BMC Public Health. 2010;10:663. doi: 10.1186/1471-2458-10-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan M, Ahmed S. The “Birthing Hut” Facilities of Manoshi: a two-part paper exploring the inception and post-inception phases of urban delivery centers. Dhaka, Bangladesh: icddr,b and BRAC; 2009. [Google Scholar]
- 36.Banu M, Nahar S, Nasreen H. Assessing the MANOSHI Referral System: addressing delays in seeking emergency obstetric care in Dhaka’s slums. Dhaka, Bangladesh: icddr,b and BRAC; 2010. [Google Scholar]
- 37.Story WT, Burgard SA, Lori JR, Taleb F, Ali NA, Hoque DM. Husbands’ involvement in delivery care utilization in rural Bangladesh: a qualitative study. BMC Pregnancy Childbirth. 2012;12:28. doi: 10.1186/1471-2393-12-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aronson RE, Wallis AB, O’Campo PJ, Schafer P. Neighborhood mapping and evaluation: a methodology for participatory community health initiatives. Matern Child Health J. 2007;11(4):373–83. doi: 10.1007/s10995-007-0184-5. [DOI] [PubMed] [Google Scholar]
- 39.Roy T, Marcil L, Chowdhury R, Afsana K, Perry H. The BRAC Manoshi Approach to Initiating a Maternal, Neonatal and Child Health Project in Urban Slums with Social Mapping, Census Taking, and Community Engagement2014. Available at http://www.brac.net/sites/default/files/portals/Manoshi-book-v3-1.pdf. Accessed Dec 20 2015.