Abstract
Background:
Laparoscopic cholecystectomy (LC) has been a standard operation and replaced the open cholecystectomy (OC) rapidly because the technique resulted in less pain, smaller incision, and faster recovery. This study was to evaluate the value of blunt dissection in preventing bile duct injury (BDI) in laparoscopic cholecystectomy (LC).
Methods:
From 2003 to 2015, LC was performed on 21,497 patients, 7470 males and 14,027 females, age 50.3 years (14–84 years). The Calot's triangle was bluntly dissected and each duct in Calot's triangle was identified before transecting the cystic duct.
Results:
Two hundred and thirty-nine patients (1.1%) were converted to open procedures. The postoperative hospital stay was 2.1 (0–158) days, and cases (46%) had hospitalization days of 1 day or less, and 92.8% had hospitalization days of 3 days or less; BDI was occurred in 20 cases (0.09%) including 6 cases of common BDI, 2 cases of common hepatic duct injury, 1 case of right hepatic duct injury, 1 case of accessory right hepatic duct, 1 case of aberrant BDI 1 case of biliary stricture, 1 case of biliary duct perforation, 3 cases of hemobilia, and 4 cases of bile leakage.
Conclusion:
Exposing Calot's triangle by blunt dissection in laparoscopic cholecystectomy could prevent intraoperative BDI.
Keywords: Bile Duct Injury, Blunt Dissection, Laparoscopic Cholecystectomy
INTRODUCTION
Laparoscopic cholecystectomy (LC) has been a standard operation and replaced the open cholecystectomy (OC) rapidly because the technique resulted in less pain, smaller incision, and faster recovery. From 1987, in which year Mouret performed the first LC, the new technique developed fast.[1] Despite the benefits of LC, there is still concern about some severe complications of this technique, especially bile duct injury (BDI). In order to reduce BDI, surgeons must expose Calot's triangle clearly without a sense of touch in LC. Now, there are two techniques universally used in LC. One is energized dissection, such as electric coagulation, monopolar electrosurgery, and ultrasonic scalpel. The other one is cold dissection, including sharp dissection, and blunt dissection.
Based on some reports of multicenter, large-sample trial studies, the rate of BDI in LC was 0.10–0.42%[2] around the world. Our center firstly used blunt dissection by flushing and aspiration to expose Calot's triangle and had a satisfactory result. From 2003 to 2015, LC was performed on 21,497 patients in 12 years. The Calot's triangle was exposed by blunt dissection routinely before transecting the cystic duct. Above all cases, BDI was diagnosed in 20 patients (0.09%). In this study, we were to introduce the technique of blunt dissection and to show the BDI cases in our institution.
METHODS
Patient
From 2003 to 2015, 21,497 LCs were performed in Department of General Surgery, Sir Run Run Shaw Hospital of Zhejiang University. There were 7470 males and 14,027 females, aged 50.3 years (14–84 years). In all the cases, 19,343 patients were diagnosed as cholecystolithiasis, including 16,754 chronic cholecystolithiasis and 2589 acute cholecystolithiasis; 2154 patients were diagnosed as cholecystic polypus. Informed consent was not required because of the retrospective nature of this study.
Operation
The operations were performed under general anesthesia. The technique of blunt dissection with flushing and aspiration was used in each operation to expose Calot's triangle. Patients were placed in supine position and 4 entries (1 umbilical, 1 epigastric, and 2 in the right flank) were made. A Veress needle was inserted directly under the umbilicus to allow for the flow of carbon dioxide into the peritoneal cavity, and the pneumoperitoneum was established at 12–14 mmHg. The cystic artery and cystic duct were ligated with clips after the cystic duct, the common hepatic duct, and the common hepatic duct were identified [Figure 1].
Figure 1.
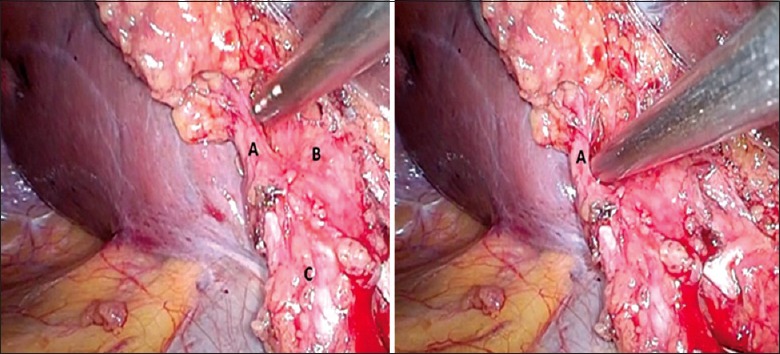
Exposure of Calot's triangle by blunt dissection with flushing and aspiration. The main equipment of the technique is laparoscopic suction and irrigation tubes. In the picture, we identified the cystic duct (A), the common hepatic duct (B) and the common hepatic duct (C).
Prophylactic antibiotics were used in all operated patients (half an hour before surgery, intravenously). In cases of conversion from LC to OC, the preferred incision was a subcostal incision.
Laparoscopic cholecystitis grading
As inflammation around the gallbladder, the laparoscopic cholecystitis grading (LCG) was classified into four grades (G0–G3) [Table 1].[3]
Table 1.
Laparoscopic cholecystitis grading
| Grade | Description |
|---|---|
| 0 | Mild adhesion without inflammation of the gallbladder |
| 1 | Inflammatory fibrous adhesion without acute inflammation |
| 2 | Severe inflammatory thickening of the gallbladder with mild adhesion |
| 3 | Lack of visualization of the gallbladder due to close inflammatory adhesion |
Type of bile duct injury
The Strasberg classification[4] was used to describe the type of BDI (based on surgical and cholangiographic findings) and the Dindo-Clavien classification[5] was used to stratify the severity of complications [Tables 2 and 3].
Table 2.
Type of bile duct injury
| Type | Description |
|---|---|
| A | Cystic duct leaks or leakage from aberrant |
| B | An injury of aberrant right duct |
| C | A bile leak from a major aberrant right duct without an injured common duct |
| D | A lateral injury to the extrahepatic common duct |
| E | Bile duct strictures El – E5 |
| E1 | A circumferential injury to the common duct >2 cm from the bifurcation |
| E2 | A circumferential injury to the common duct <2 cm from the bifurcation |
| E3 | A circumferential injury to the common duct at the bifurcation |
| E4 | An injury proximal to the bifurcation involving both main right and left hepatic ducts |
| E5 | A combined injury to the common duct and a major aberrant right hepatic duct |
Table 3.
The Dindo-Clavien classification
| Type | Description |
|---|---|
| Grade 1 | Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, and radiological interventions |
| Grade 2 | Requiring pharmacological treatment with drugs other than such allowed for Grade 1 complications. Blood transfusions and total parenteral nutrition are also included |
| Grade 3 | Requiring surgical, endoscopic, or radiological intervention |
| Grade 3a: | Intervention not under general anesthesia |
| Grade 3b: | Intervention under general anesthesia |
| Grade 4 | Life-threatening complication (including CNS complications) requiring IC/ICU management |
| Grade 4a: | Single organ dysfunction (including dialysis) |
| Grade 4b: | Multiorgan dysfunction |
| Grade 5 | Death of patient |
CNS: Central nervous system; IC: Intermediate care; ICU: Intensive care unit.
Data of patients
Patient demographics include age and gender; operation time, rate of conversion, surgeon; the hospitalization days, complications, and types and treatments of BDI.
RESULTS
During the 12-year study period, 21,497 LCs were performed by blunt dissection with flushing and aspiration, operation time 45 (range: 20–300 minutes) minutes, average bleeding 14 ml. Mean hospitalization days were 2.1 days, and about 46% had hospitalization days of 1 day or less. 92.8% had hospitalization days of 3 days or less. Two hundred and thirty-nine cases had conversion because of severe adhesion, carcinoma of the gallbladder, gallbladder-intestine fistula, and BDI. Twenty patients had diagnosis of BDI, representing an incidence of 0.09%. In 11 cases (55%), the diagnosis was performed during the surgical procedure. The other 9 patients were diagnosed BDI after the operation.
Patients of bile duct injury
Twenty patients were diagnosed BDI, 14 males and 6 females. Three patients were acute cholecystolithiasis, and 17 patients were chronic cholecystolithiasis. Based on the LCG, there were 8 G1, 7 G2, and 5 G3. The operating surgeon was a senior HPB staff in 17 cases (85%), an HPB surgery fellow in 2 cases (10%), and a general surgery resident in 1 case (5%). The BDIs in these 20 cases were as follows: 6 cases of common BDI (4 cases of lateral injury and 2 circumferential injury), 2 of common hepatic duct injury, 1 of right hepatic duct injury, 1 of accessory right hepatic duct, 1 of aberrant BDI, 1 of biliary stricture, 1 of biliary duct perforation, 3 of hemobilia, and 4 of bile leakage. One case of right hepatic duct injury and 1 case of common hepatic duct injury were caused by thermal damage of electric coagulation. According to Strasberg-Bismuth Classification of BDI, there were 4 type A (20%), 1 type B (5%), 1 type C (5%), 10 type D (50%), and 1 type E2 (5%). The other 3 cases suffered in bile duct bleeding [Table 4].
Table 4.
Operative data and overall perioperative outcomes in patients with BDI after LC
| Patient Number | LCG | Time | Type of BDI | Convert | Surgeon level | Management | Complication | Hospital stay (days) | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Grade 2 | Selective | Right hepatic duct | Yes | Senior | Primary closure + T-tube | II | 28 | Recovery |
| 2 | Grade 2 | Selective | Aberrant bile duct | Yes | Senior | Primary closure | II | 7 | Recovery |
| 3 | Grade 3 | Selective | Partial CBD | No | Senior | Primary closure + T-tube | II | 21 | Recovery |
| 4 | Grade 1 | Selective | Partial CBD | Yes | Senior | Primary closure + T-tube | II | 23 | Recovery |
| 5 | Grade 1 | Selective | Partial CBD | Yes | Senior | Primary closure + T-tube | II | 30 | Recovery |
| 6 | Grade 3 | Selective | Partial CBD | Yes | Senior | Primary closure + T-tube | II | 7 | Recovery |
| 7 | Grade 3 | Emergency | Complete CBD | Yes | Fellow | RYH | II | 8 | Recovery |
| 8 | Grade 2 | Selective | Complete CBD | Yes | Senior | RYH | II | 17 | Recovery |
| 9 | Grade 1 | Selective | CBD perforation | No, SS | Senior | SS to RYH | IVb | 158 | Recovery |
| 10 | Grade 1 | Emergency | CBD stricture | No | Fellow | Conservative treatment | II | 5 | Recovery |
| 11 | Grade 3 | Emergency | Partial CHD | Yes | Senior | Primary closure + T-tube | II | 8 | Recovery |
| 12 | Grade 3 | Selective | Partial CHD | Yes | Senior | Primary closure + T-tube | II | 14 | Recovery |
| 13 | Grade 2 | Selective | Right hepatic duct | Yes | Senior | Primary closure + T-tube | II | 8 | Recovery |
| 14 | Grade 1 | Selective | Bile leakage | No, SS | Senior | SS to lavage and drainage | IIIb | 26 | Recovery |
| 15 | Grade 2 | Selective | Bile leakage | No | Senior | Conservative treatment | IIIa | 15 | Recovery |
| 16 | Grade 1 | Selective | Bile leakage | No | Resident | Conservative treatment | IIIa | 7 | Recovery |
| 17 | Grade 1 | Selective | Bile leakage | No | Senior | Conservative treatment | IIIa | 14 | Recovery |
| 18 | Grade 1 | Selective | Bile duct bleeding | No | Senior | Conservative treatment | IIIa | 9 | Recovery |
| 19 | Grade 2 | Selective | Bile duct bleeding | No | Senior | Conservative treatment | IIIa | 7 | Recovery |
| 20 | Grade 2 | Selective | Bile duct bleeding | No | Senior | Conservative treatment | IIIa | 8 | Recovery |
CHD: Common hepatic duct; CBD: Common bile duct; BDI: Bile duct injury; LCG: Laparoscopic cholecystitis grading; LC: Laparoscopic cholecystectomy; SS: Secondary surgery; RYH: Roux-en-Y hepaticojejunostomy.
Management and repair
The LCs were converted to open in 10 cases (50%). Laparoscopic BDI repair was performed in 1 patient (5%). Two cases were diagnosed BDI after operations and received second surgeries. Seven cases were diagnosed BDI after operations and had conservative treatment. Above the 20 cases, 17 cases (85%) were selective operations (8 cases [47%] were converted to repair BDI, 2 cases received second surgeries) and 3 cases were emergency operations (2 cases [67%] were converted to repair BDI).
Ten cases were converted to open surgery (6 cases of common BDI, 2 of common hepatic duct injury, 1 of right hepatic duct injury, and 1 of accessory right hepatic duct). The most common procedure performed was a primary closure in 8 with T-tube placement, and 2 Roux-en-Y hepaticojejunostomies (2 with a circumferential injury of the common bile duct). In 1 case (aberrant BDI), the injury was repaired laparoscopically.
Nine cases were diagnosed after operations. Two cases (1 biliary duct perforation and 1 bile leakage) received the second surgery: 1 case of biliary duct perforation was performed Roux-en-Y hepaticojejunostomy and stayed in Intensive Care Unit (ICU) for more than 2 weeks; 1 case of bile leakage was performed peritoneal lavage and drainage. One patient had jaundice after surgery and was diagnosed biliary stricture by magnetic resonance cholangiopancreatography. This patient received conservative treatment and achieved remission of symptoms in 1 week. The other 6 cases (3 bile duct bleeding and 3 bile leakage) also had conservative treatment with ultrasound guided percutaneous puncture catheter drainage and achieved remission of symptoms [Tables 4 and 5].
Table 5.
Type of BDI, repair, and overall results
| Characteristics | Results, n (%) |
|---|---|
| Type of injury | |
| A | 4 (20) |
| B | 1 (5) |
| C | 1 (5) |
| D | 10 (50) |
| E2 | 1 (5) |
| Artery injury | 3 (15) |
| Type of repair | |
| Primary closure | 9 (45) |
| Second surgery | 2 (10) |
| RYH | 2 (10) |
| Conservative treatment | 7 (35) |
| Complications | |
| II | 12 (60) |
| IIIa | 6 (30) |
| IIIb | 1 (5) |
| IVb | 1 (5) |
| Hospitalization (days) | |
| Mean | 21 |
| Range | 5–158 |
| Mortality | 0 (0) |
| Follow-up | 0 (0) |
BDI: Bile duct injury. RYH: Roux-en-Y hepaticojejunostomy.
Outcomes
The outcomes of BDI managed are summarized in Tables 1 and 2. There was no death in 20 cases, and all the patients recovered well. Twelve cases (60%) were grade II and 6 cases (30%) of leakage or bleeding required ultrasound guided percutaneous puncture catheter drainage (grade IIIa). Common bile duct perforation with bile leakage developed in 1 case (IV b), which received the second surgery to do Roux-en-Y hepaticojejunostomies and stayed in ICU for more than 1 month because of multiorgan dysfunction. The other one had a bile leakage with severe infection and received the second surgery to lavage and drainage (IIIb). Mean hospitalization days was 21 days (range: 5–158 days), and all the patients were fully recovered.
DISCUSSION
BDI is the most severe complication in LC. According to a report, the rate of BDI in LC was 0.10–0.42%,[3] and common BDI and common hepatic duct injury were the most common types, ranged from 61.0% to 77.5%.[6,7,8] Before the adoption of this technique, 14,302 cases of laparoscopic cholecystectomies were performed in our institute by the conventional procedure and the occurrence rate of biliary injury was 0.37%[9] which was significant higher than that reported in the current study (P < 0.05, chi-square analysis), but we did not use this comparison to approve the advantage of the current procedure because of the potential impact of the learning curve. We reviewed large-series reports of LC, which had more than 10,000 cases on PubMed [Table 6]. The occurrence rate of biliary injury in our series is lower than that in these reports that might account for the potential advantage of this procedure. According to these reports, causes of BDI include: (1) severe adhesion, it is difficult to expose Calot's triangle clearly; (2) abnormal anatomy of bile duct; (3) improper operation, such as thermal injury by electric coagulation, monopolar electrosurgery, and ultrasonic scalpel, bile duct stricture caused by clips; (4) surgeons are not trained well.[10,11]
Table 6.
Literatures of LC
| Year | Author | Patients (n) | BDI incidence (%) |
|---|---|---|---|
| 1993 | Deziel et al.[18] | 77,604 | 0.60 |
| 1998 | Vecchio et al.[19] | 114,005 | 0.49 |
| 2005 | Wang et al.[9] | 14,302 | 0.37 |
| 2006 | Waage and Nilsson[20] | 152,776 | 0.40 |
| 2010 | Zha et al.[21] | 13,000 | 0.28 |
| 2011 | Harboe et al.[10] | 20,307 | 0.20 |
| 2013 | Pekolj et al.[22] | 10,123 | 0.18 |
| 2013 | Grbas et al.[2] | 10,317 | 0.24 |
| 2013 | Fullum et al.[23] | 377,424 | 0.30 |
BDI: Bile duct injury; LC: Laparoscopic cholecystectomy.
Agarwal et al.[12] showed an RCT study in 2014, the use of energetic dissection in LC, like electric coagulation and ultrasonic scalpel, was associated with higher risk of complication. McKinley et al.[13] reported that the rate of BDI in surgeon’s first LC was 1.7%, but in one's 50th LC the rate reduced to 0.17%. So in LCs, experienced and well-trained surgeons are very important. Besides, the most important measure to avoid BDI was exposing the Calot's triangle clearly.[14] In conclusion, our center firstly used blunt dissection by flushing and aspiration to expose the Calot's triangle. The technique has two advantages: (1) blunt dissection, which can avoid thermal injury by using energetic dissection and reduce injury by sharp dissection; (2) the equipment is cheap, simple, and easy for young surgeons to learn. Surgeons use laparoscopic suction and irrigation tubes to flush and aspirate the Calot's triangle repeatedly. We collected data of 12-year LCs in our institution. Total 21,497 LCs were performed by blunt dissection with flushing and aspiration. Two hundred and thirty-nine cases (1.1%) were converted to open, 20 cases (0.09%) were BDI and 11 cases of BDI (55%) were diagnosed in operations. Compared with other institution around the world (over 10,000 LCs), we had a significantly lower incidence of BDI in LCs [Table 6]. In the 20 cases, there were 17 senior surgeons, 2 fellows, and 1 resident. Above all, we found that the rate of BDI and converted using our blunt dissection were both less than other large sample trial studies around the world. According to the analysis of surgeons, 85% cases were performed by senior surgeons and only 15% cases were performed by junior surgeons. It proved that this technique was easy for young surgeons to learn and control. So we believed that the technique of blunt dissection with flushing and aspiration is the best and easiest solution for surgeons to expose the Calot's triangle and reduce the incidence of BDI.
The main equipment of the technique is laparoscopic suction and irrigation tubes. It has three advantages: (1) laparoscopic suction and irrigation tubes are blunt tools and have a high safety in dissection; (2) it is easy for surgeons to control and it can flush and aspirate repeatedly to keep operation field clear without changing equipment frequently; and (3) laparoscopic suction and irrigation tubes are cheap and available equipments, it can reduce the cost of operations.[15]
The technique of blunt dissection by flushing and aspiration to expose the Calot's triangle is safe and simple. Detailed operation procedures: First step is open a hole in the anterior sheath over the Calot's triangle wall by dissecting forceps, then using laparoscopic suction and irrigation tubes to flush and aspirate the Calot's triangle repeatedly through the anterior sheath hole until we see the cystic duct clearly. Second step is flushing and aspiration in a direction parallel to the cystic duct, from its length down toward the junction of the cystic duct, common bile duct, and common hepatic duct until exposing the bile duct clearly. Third, in order to expose the cystic artery and abnormal anatomy, we can use the same way to flush and aspirate the tissue in the Calot's triangle and identify all the location of main arteries and bile ducts. If the Calot's triangle cannot be dissected clearly with severe adhesion, in our experience, we cannot cut-off the arteries and bile ducts blindly, and we can use intraoperative cholangiography to locate bile ducts. So we believe that blunt dissection by flushing and aspiration is an effective solution to expose bile ducts and arteries, especially abnormal anatomy.
Besides, based on our experience, there were some notices for prevention of BDI: (1) Check carefully before operations and evaluate the abnormal anatomy; (2) Do not cut-off the ducts before the main bile ducts are not clear; (3) Reduce the use of energetic dissection; (4) Intraoperative cholangiography can show the bile ducts clearly and prevent BDI, but now many experts considered that it is unnecessary for surgeons to perform intraoperative cholangiography in all the LCs.[16,17]
In conclusion, avoiding BDI is a major issue for surgeons in LC. Blunt dissection by flushing and aspiration to expose Calot's triangle, and results proved it to be a valuable method to avoid BDI.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Mouret P. How I developed laparoscopic cholecystectomy. Ann Acad Med Singapore. 1996;25:744–7. [PubMed] [Google Scholar]
- 2.Grbas H, Kunisek L, Zelic M, Petrosic N, Cepic I, Pirjavec A, et al. Outcome evaluation of 10,317 laparoscopic cholecystectomies: A 17-year experience at a single center. Hepatogastroenterology. 2013;60:1873–6. [PubMed] [Google Scholar]
- 3.Hakamada K, Narumi S, Toyoki Y, Nara M, Oohashi M, Miura T, et al. Intraoperative ultrasound as an educational guide for laparoscopic biliary surgery. World J Gastroenterol. 2008;14:2370–6. doi: 10.3748/wjg.14.2370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–25. [PubMed] [Google Scholar]
- 5.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Way LW, Stewart L, Gantert W, Liu K, Lee CM, Whang K, et al. Causes and prevention of laparoscopic bile duct injuries: Analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–9. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Olsen D. Bile duct injuries during laparoscopic cholecystectomy. Surg Endosc. 1997;11:133–8. doi: 10.1007/s004649900315. [DOI] [PubMed] [Google Scholar]
- 8.McKinley SK, Brunt LM, Schwaitzberg SD. Prevention of bile duct injury: The case for incorporating educational theories of expertise. Surg Endosc. 2014;28:3385–91. doi: 10.1007/s00464-014-3605-8. [DOI] [PubMed] [Google Scholar]
- 9.Wang XF, Li W, Cai XJ. Clinical study on primary repair for bile duct injury during laparoscopic cholecystectomy (in Chinese) Natl Med J China. 2005;85:916–8. [PubMed] [Google Scholar]
- 10.Harboe KM, Bardram L. The quality of cholecystectomy in Denmark: Outcome and risk factors for 20,307 patients from the national database. Surg Endosc. 2011;25:1630–41. doi: 10.1007/s00464-010-1453-8. [DOI] [PubMed] [Google Scholar]
- 11.Chuang KI, Corley D, Postlethwaite DA, Merchant M, Harris HW. Does increased experience with laparoscopic cholecystectomy yield more complex bile duct injuries? Am J Surg. 2012;203:480–7. doi: 10.1016/j.amjsurg.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 12.Agarwal BB, Agarwal N, Agarwal KA, Goyal K, Nanvati JD, Manish K, et al. Outcomes of laparoscopic cholecystectomy done with surgical energy versus done without surgical energy: A prospective-randomized control study. Surg Endosc. 2014;28:3059–67. doi: 10.1007/s00464-014-3579-6. [DOI] [PubMed] [Google Scholar]
- 13.McKinley SK, Brunt LM, Schwaitzberg SD. Prevention of bile duct injury: The case for incorporating educational theories of expertise. Surg Endosc. 2014;28:3385–91. doi: 10.1007/s00464-014-3605-8. [DOI] [PubMed] [Google Scholar]
- 14.Li LX, Ai KX, Bai YQ, Zhang P, Huang XY, Li YY. Strategies to decrease bile duct injuries during laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2014;24:770–6. doi: 10.1089/lap.2014.0225. [DOI] [PubMed] [Google Scholar]
- 15.Cai XJ, Gu XJ, Wang YF, Hong Y, Xiao L. Experience in laparoscopic cholecystectomy by exposing comm on hepatic duct using blunt dissection to prevent bile duct injury (in Chinese) Natl Med J China. 2007;87:1425–6. [PubMed] [Google Scholar]
- 16.Ammori MB, Al-Dabbagh AK. Laparoscopic cholecystectomy without intraoperative cholangiography. J Laparoendosc Adv Surg Tech A. 2012;22:146–51. doi: 10.1089/lap.2011.0401. [DOI] [PubMed] [Google Scholar]
- 17.Pesce A, Portale TR, Minutolo V, Scilletta R, Li Destri G, Puleo S. Bile duct injury during laparoscopic cholecystectomy without intraoperative cholangiography a retrospective study on 1100 selected patients. Dig Surg. 2012;29:310–4. doi: 10.1159/000341660. [DOI] [PubMed] [Google Scholar]
- 18.Deziel DJ, Millikan KW, Economou SG, Doolas A, Ko ST, Airan MC. Complications of laparoscopic cholecystectomy: A national survey of 4,292 hospitals and an analysis of 77,604 cases. Am J Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. [DOI] [PubMed] [Google Scholar]
- 19.Vecchio R, MacFadyen BV, Latteri S. Laparoscopic cholecystectomy: An analysis on 114,005 cases of United States series. Int Surg. 1998;83:215–9. [PubMed] [Google Scholar]
- 20.Waage A, Nilsson M. Iatrogenic bile duct injury: A population-based study of 152 776 cholecystectomies in the Swedish Inpatient Registry. Arch Surg. 2006;141:1207–13. doi: 10.1001/archsurg.141.12.1207. [DOI] [PubMed] [Google Scholar]
- 21.Zha Y, Chen XR, Luo D, Jin Y. The prevention of major bile duct injures in laparoscopic cholecystectomy: The experience with 13,000 patients in a single center. Surg Laparosc Endosc Percutan Tech. 2010;20:378–83. doi: 10.1097/SLE.0b013e3182008efb. [DOI] [PubMed] [Google Scholar]
- 22.Pekolj J, Alvarez FA, Palavecino M, Sánchez Clariá R, Mazza O, de Santibañes E. Intraoperative management and repair of bile duct injuries sustained during 10,123 laparoscopic cholecystectomies in a high-volume referral center. J Am Coll Surg. 2013;216:894–901. doi: 10.1016/j.jamcollsurg.2013.01.051. [DOI] [PubMed] [Google Scholar]
- 23.Fullum TM, Downing SR, Ortega G, Chang DC, Oyetunji TA, Van Kirk K, et al. Is laparoscopy a risk factor for bile duct injury during cholecystectomy? JSLS. 2013;17:365–70. doi: 10.4293/108680813X13654754535638. [DOI] [PMC free article] [PubMed] [Google Scholar]


