Abstract
Background:
Hamstring (HS) autograft and bone-patellar tendon-bone allograft are the most common choice for reconstruction of anterior cruciate ligament (ACL). There was a little report about the clinical outcome and difference of arthroscopic ACL reconstruction using allograft and autograft. This study aimed to compare the clinical outcome of autograft and allograft reconstruction for ACL tears.
Methods:
A total of 106 patients who underwent surgery because of ACL tear were included in this study. The patients were randomly divided into two groups, including 53 patients in each group. The patients in group I underwent standard ACL reconstruction with HS tendon autografts, while others in group II underwent reconstruction with bone-patellar tendon-bone allograft. All the patients were followed up and analyzed; the mean follow-up was 81 months (range: 28–86 months). Clinical outcomes were evaluated using the International Knee Documentation Committee (IKDC), Lysholm scores, physical instability tests, and patient satisfaction questionnaires. The complication rates of both groups were compared. Tibial and femoral tunnel widening were assessed using lateral and anteroposterior radiographs.
Results:
At the end of follow-up, no significant differences were found between the groups in terms of IKDC, Lysholm scores, physical instability tests, patient satisfaction questionnaires, and incidences of arthrofibrosis. Tibial and femoral tunnel widening was less in the HS tendon autografts. This difference was more significant on the tibial side.
Conclusions:
In the repair of ACL tears, allograft reconstruction is as effective as the autograft reconstruction, but the allograft can lead to more tunnel widening evidently in the tibial tunnel, particularly.
Keywords: Allograft, Anterior Cruciate Ligament, Autograft, Reconstruction
INTRODUCTION
Tear of the anterior cruciate ligament (ACL) tear is a very common injury, with its frequency ranging from 11% to 33% in different series.[1] Reconstruction of ACL tears is one of the most common procedures performed by orthopedic surgeons. Despite the high frequency of this procedure, there is considerable variability in the grafts chosen for ACL reconstruction. The available autograft choices include a central third bone-patellar tendon-bone (BTB) graft, a semitendinosus-gracilis graft from the hamstring (HS), or a quadriceps tendon graft. A number of allograft choices are available, including Achilles tendon, BTB, anterior or posterior tibial tendon, HS, and quadriceps tendon. All the choices can be divided into autograft and allograft, it is still unknown which is better, the ideal graft should have rapid incorporation, low failure rates, a high degree of safety, low donor site morbidity, wide availability, and low cost. Unfortunately, no such graft exists. By now there is no affirmative data about the difference between autograft and allograft reconstruction for ACL tears. For this reason, we chose to analyze which is better in autograft and allograft choice for ACL reconstruction from 2002 to 2011.
Our hypothesis is that the clinical outcome of allograft is as favorable as the reconstruction with HS tendon autograft, and potential complications are not more common than that of autograft. We aimed to compare the clinical outcome and complications of autograft and allograft reconstruction.
METHODS
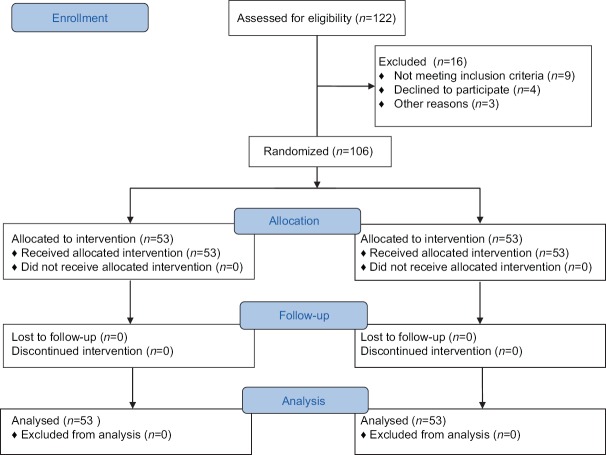
This study was performed between May 2002 and June 2011, the study protocol was approved by the Regional Ethics Committee (Qilu Hospital of Shandong University) and all patients signed an informed consent and conducted in accordance with the Declaration of Helsinki. A CONSORT diagram is provided for reference [Figure 1]. One hundred and twenty-two patients were diagnosed with ACL tear by physical examination and magnetic resonance imaging, other inclusion criteria were normal alignment, normal contralateral knee, and willingness to join the rehabilitation program. Nine patients with arthrosis, grade 3–4 chondral damage, rotatory instability, and history of previous knee surgery or fracture around the knee were excluded. Seven patients were excluded from the study because of other reasons. After informed consents were obtained, 106 patients were randomized into two groups using computer-generated randomized numbers which were put in sealed opaque envelopes. In order to provide standardization, all applications were performed by a single physician specialized in the field. Autograft reconstruction group is reconstructed with HS autograft and allograft group with bone-patellar tendon-bone allograft. In order to reduce the immunogenicity of allograft, the allograft is presoaked with dexamethasone and gentamicin for at least 30 min. The first group was composed of 53 patients (28 males, 25 females; mean age 31 years; and range, 19–51 years). The second group consisted of 53 patients (26 males, 27 females; mean age 28 years; and range, 18–36 years). The patients underwent surgery no earlier than 1 week after the ACL tear. At this time, patients were placed into rehabilitation with the purpose of achieving painless and near-complete range of motion (ROM). In both groups, femoral fixation was performed with a cross-pin system (DePuy Mitek, Inc., USA) and tibial fixation with a screw. Patients were rehabilitated within the same program for 4–6 months. In the early postoperative period, they were instructed to use crutches and braces. Sports activities were permitted on an average of 12–16 months later. Clinical outcomes of both groups were compared using International Knee Documentation Committee (IKDC) and Lysholm scores, ROM, Lachman, pivot shift tests, and patient satisfaction. Femoral and tibial tunnel widening was assessed by comparing lateral and AP radiographs taken in the early postoperative and at the last follow-up. Femur and tibial tunnel width at the widest point and at 1 cm from aperture of the tunnels were measured by a radiologist and corrected for magnification. Differences between the early postoperative and the last follow-up were recorded.
Figure 1.
Flow diagram of the CONSORT diagram.
Statistical analysis
Full analysis set was analyzed and included all randomized patients. Data are expressed as a mean ± standard deviation or mean (95% confidence interval) as noted. The sample size of each group was determined beforehand using statistical power analysis. Sample sizes of 53 patients in each group were calculated to yield more than 0.80 statistical power, and the study groups were arranged accordingly. The independent sample t-test, Fisher exact and Chi-square tests were used as statistical analyses. A P < 0.05 was considered statically significant.
RESULTS
Mean follow-up was 81 months (range, 28–86 months). Mean time from trauma to ACL reconstruction was 1.4 months (range, 1–3 months) in the autograft group and 1.5 months (range, 1–3 months) in the allograft group. There was no significant difference between the groups in terms of improvement of IKDC (P = 0.90) and Lysholm scores (P = 0.94). All the patients in both groups had firm end points, and there was no significant difference between the two groups in terms of final follow-up Lachman and postoperative pivot-shift (P = 0.5, P = 0.5) There was no significant difference between the two groups in terms of ROM, patient satisfaction, and mean quadriceps circumference differences between the two groups (P > 0.05) [Table 1]. Tibial and femoral tunnel widening was lower in the autograft group (P = 0.001, P = 0.03 respectively). This difference was more significant on the tibial side (P = 0.001) [Table 2]. Forty-seven patients in the autograft group were satisfied, 5 patients were nearly satisfied, and one was unsatisfied. Forty-six patients in the allograft group were satisfied, and 7 patients were nearly satisfied (P > 0.05).
Table 1.
Assessment of stability, quadriceps circumferences, ROM, and knee function in both groups (group I and group II)
| Characteristics | n | Mean ± SD | Range | n | Mean ± SD | Range | P |
|---|---|---|---|---|---|---|---|
| Preoperative Lachman | |||||||
| Grade 2 | 4 | 5 | |||||
| Grade 3 | 49 | 48 | |||||
| Final follow-up Lachman | |||||||
| – | 46 | 47 | 0.5 | ||||
| Grade 1 | 7 | 6 | |||||
| Preoperative pivot-shift | |||||||
| Grade 1 | 7 | 6 | |||||
| Grade 2 | 46 | 44 | |||||
| Grade 3 | 0 | 3 | |||||
| Final follow-up pivot-shift | |||||||
| – | 42 | 40 | 0.5 | ||||
| Grade 1 | 11 | 13 | |||||
| Preoperative quadriceps circumference (feet) | 2.6 | 0.8–5.0 | 2.6 | 1–4 | >0.5 | ||
| Postoperative quadriceps circumference (feet) | 1.0 | 0.4–2.0 | 2.0 | 1.0–3.5 | |||
| ROM (°) | 136.0 ± 4.5 | 136 ± 43 | >0.5 | ||||
| Preoperative IKDC score | (I) 67.3 ± 2.5 | 61–78 | (II) 66.1 ± 3.5 | 60–74 | >0.5 | ||
| Postoperative IKDC score | (I) 87.8 ± 1.6 | 82–90 | (II) 85.6 ± 2.9 | 81–91 | |||
| Preoperative Lysholm score | (I) 71.9 ± 4.2 | 69–84 | (II) 71.0 ± 3.6 | 66–83 | >0.5 | ||
| Postoperative Lysholm score | (I) 85.2 ± 3.1 | 80–95 | (II) 86.8 ± 2.6 | 81–90 |
SD: Standard deviation; IKDC: International Knee Documentation Committee; ROM: Range of motion. The P values of Final follow-up Lachman and Final follow-up pivot-shift stand for improvement ratio.
Table 2.
Tunnel widening in autograft and allograft groups
| Items | Tibia | Femur | ||
|---|---|---|---|---|
| Allograft | Autograft | Allograft | Autograft | |
| Postoperative | 7.12 ± 0.40 | 7.48 ± 0.31 | 7.46 ± 0.41 | 7.42 ± 0.31 |
| Follow-up | 7.80 ± 0.40 | 7.61 ± 0.22 | 7.64 ± 0.35 | 7.51 ± 0.42 |
| Difference in widening | P = 0.001 | P = 0.03 | ||
DISCUSSION
The bone-patellar tendon-bone (BPTB) and HS tendon autografts are the most common grafts in ACL reconstructions. More surgeons choose HS tendon autografts as their first choice. Some studies suggested that a harvest of the central third of the patellar tendon might have associated donor site morbidities, such as patellofemoral osteoarthritis, patellar tendon shortening, loss of terminal extension, and patellofemoral pain.[2] There has been an increase in the popularity of HS tendons as autografts for ACL reconstructions, but it also cannot completely avoid harvest site morbidity. So surgeons begin to use allograft to reconstruct the torn ACL. The potential advantages of allograft placement include autograft benefits without donor site morbidity.[3,4,5] Debates over graft selection are likely to persist with the presence of autograft harvest site morbidity.
Our study showed that patients undergoing allograft reconstruction can obtain satisfactory clinical effect as the autograft and allograft ACL reconstruction found only one statistically significant difference in outcome measures, tunnel widening was found to be significantly less in autograft reconstruction. For all other negative outcome measures including positive Lachman test, positive pivot-shift test, IKDC grade C or D, and graft failure proportions were larger for allograft than for autograft, but after statistical analysis, the differences were not significant. The rate of ligament rupture after primary reconstruction is higher in the allograft group, but the difference is not statistical, we think that the reason that the allograft group has higher risk of ACL graft failure is that allograft reconstruction patients have a quicker postoperative rehabilitation course and diminished pain compared to patients with autografts, it may lead the allograft reconstruction patients to return to high level of activity earlier than the latter and before sufficient biological healing of the graft, which may place allograft reconstruction patients at a higher risk of retear. Gobbi and Foster TE et al compared the biological incorporation and mechanical properties of allografts and autografts in a sheep model. The result showed that autografts incorporated more quickly than allograft at 6 and 12 weeks, but the difference decreasing at 52 weeks and disappeared at 72 weeks.[6,7,8,9] Perhaps, this is another reason that the allograft group has a higher risk of ACL graft failure in the early stage after the reconstruction. So we suggest that allograft reconstruction patients should receive more conservative rehabilitation than autograft reconstruction patients.
In spite of obvious progress of research on ACL reconstruction, none of graft or reconstruction technique can duplicate the complex structure of ACL. Grafts used at present are all tendons and histological different from normal ACL. Surgeons usually choose grafts for ACL reconstructions according to their experience, preference, and tissue availability. In general, the majority of orthopedic surgeons feels that allograft tissues are safe for use, more than 86% of the American Orthopedic Society for Sports Medicine members stating that they use allograft.[1,9] The overall incidence of suspected allograft infection was 0.014% during a 2-year time period.[10,11] The allograft can be a safe choice for tear of the ACL if the allograft receives standard and strict procedure before it is used by surgeons.
One of the contributions of our study is examining the effect of autograft and allograft reconstruction on tunnel widening. In this study, tunnel widening was found to be significantly less in autograft reconstruction. Tunnel widening is a complication of ACL reconstruction surgery; it is the result of biological and biomechanical events.[12,13] The main reason for the biological events is the presence of synovial fluid with elevated concentration of cytokines and inflammatory agents. Allograft reconstruction can lead to more synovial fluid in the joint cavity,[14] the fluid is propagated (synovial bathing) through the tunnels, bathing the graft-bone interface with inflammatory enzymes which induce calcitonin to cause widening of the tunnels. Junkin and Johnson hypothesized that remnant ACL prevents the tunnel widening by decreasing leakage of synovial fluid. Similarly, tunnel widening was found to be significantly less in the autograft group in our study. Synovial bathing can be more prominent on the tibial side, due to gravity.[8] The results of this study support this hypothesis.
The study has several limitations, although a standardized therapy protocol was prescribed postoperatively, the quality and consistency of the physical therapy might have varied at outside institutions. This can be a factor that affects the clinical outcomes. Furthermore, the follow-up time of the study is relatively short; so long-term follow-up should be done to further evaluate the clinical outcomes. And this can explain why the effect of allograft reconstruction in our study is much better than the result of some doctor's report. The antigen-recognizing phase perhaps needs longer time than our follow-up. If we continue the follow-up, the failed case is perhaps unavoidable. Finally, this is a single-surgeon study, and the results may not be generalized.
This study confirms that allograft reconstruction for ACL tears can obtain similar clinical effect with autograft by surgeons who have the adequate training and experience. A long-term follow-up would be required to confirm the conclusion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Pujol N, Queinnec S, Boisrenoult P, Maqdes A, Beaufils P. Anatomy of the anterior cruciate ligament related to hamstring tendon grafts. A cadaveric study. Knee. 2012;14:195–7. doi: 10.1016/j.knee.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Edgar CM, Zimmer S, Kakar S, Jones H, Schepsis AA. Prospective comparison of auto and allograft hamstring tendon constructs for ACL reconstruction. Clin Orthop Relat Res. 2008;466:2238–46. doi: 10.1007/s11999-008-0305-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ma Y, Ao YF, Yu JK. Pretensioning of soft tissue grafts in anterior cruciate ligament reconstruction. Orthopedics. 2015;38:582–7. doi: 10.3928/01477447-20150701-55. [DOI] [PubMed] [Google Scholar]
- 4.Carey JL, Dunn WR, Dahm DL, Zeger SL, Spindler KP. A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. J Bone Joint Surg Am. 2009;91:2242–50. doi: 10.2106/JBJS.I.00610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang SK, Egami DK, Shaieb MD, Kan DM, Richardson AB. Anterior cruciate ligament reconstruction: Allograft versus autograft. Arthroscopy. 2003;19:453–62. doi: 10.1053/jars.2003.50103. [DOI] [PubMed] [Google Scholar]
- 6.Foster TE, Wolfe BL, Ryan S, Silvestri L, Kaye EK. Does the graft source really matter in the outcome of patients undergoing anterior cruciate ligament reconstruction? An evaluation of autograft versus allograft reconstruction results: A systematic review. Am J Sports Med. 2010;38:189–99. doi: 10.1177/0363546509356530. [DOI] [PubMed] [Google Scholar]
- 7.Youm YS, Cho SD, Eo J, Lee KJ, Jung KH, Cha JR. 3D CT analysis of femoral and tibial tunnel positions after modified transtibial single bundle ACL reconstruction with varus and internal rotation of the tibia. Knee. 2012;26:00217–7. doi: 10.1016/j.knee.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 8.Ma Y, Ao YF, Yu JK, Dai LH, Shao ZX. Failed anterior cruciate ligament reconstruction: Analysis of factors leading to instability after primary surgery. CMJ. 2013;126:280–5. [PubMed] [Google Scholar]
- 9.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: A prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14:1021–8. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- 10.Krych AJ, Jackson JD, Hoskin TL, Dahm DL. A meta-analysis of patellar tendon autograft versus patellar tendon allograft in anterior cruciate ligament reconstruction. Arthroscopy. 2008;24:292–8. doi: 10.1016/j.arthro.2007.08.029. [DOI] [PubMed] [Google Scholar]
- 11.Kustos T, Bálint L, Than P, Bárdos T. Comparative study of autograft or allograft in primary anterior cruciate ligament reconstruction. Int Orthop. 2004;28:290–3. doi: 10.1007/s00264-004-0568-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poehling GG, Curl WW, Lee CA, Ginn TA, Rushing JT, Naughton MJ, et al. Analysis of outcomes of anterior cruciate ligament repair with 5-year follow-up: Allograft versus autograft. Arthroscopy. 2005;21:774–85. [Google Scholar]
- 13.Prodromos C, Joyce B, Shi K. A meta-analysis of stability of autografts compared to allografts after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15:851–6. doi: 10.1007/s00167-007-0328-6. [DOI] [PubMed] [Google Scholar]
- 14.Scheffler SU, Schmidt T, Gangéy I, Dustmann M, Unterhauser F, Weiler A. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: Delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy. 2008;24:448–58. doi: 10.1016/j.arthro.2007.10.011. [DOI] [PubMed] [Google Scholar]