Abstract
This article is one of ten reviews selected from the Annual Update in Intensive Care and Emergency medicine 2016. Other selected articles can be found online at http://www.biomedcentral.com/collections/annualupdate2016. Further information about the Annual Update in Intensive Care and Emergency Medicine is available from http://www.springer.com/series/8901.
Background
Over the last few decades, increasing attention has been given to understanding the pathophysiology, etiology, prognosis, and treatment of elevated intra‐abdominal pressure (IAP) in trauma, surgical, and medical patients. However, there is still a relatively poor understanding of intra‐abdominal volume (IAV) and the relationship between IAV and IAP (i.e., abdominal compliance [Cab]). According to the consensus definitions proposed by the World Society on Abdominal Compartment Syndrome (WSACS), Cab is defined as a measure of the ease of abdominal expansion, determined by the elasticity of the abdominal wall and diaphragm [1]. Cab should be expressed as the change in IAV per change in IAP (expressed in ml/mmHg). Cab is one of the most neglected parameters in critically ill patients, despite playing a key‐role in understanding the deleterious effects of unadapted IAV on IAP, organ‐organ interactions and end‐organ perfusion [2, 3]. Although there are some papers related to Cab in surgical patients, only a few papers have been published addressing this issue in critically ill patients [2–4].
Definitions
The abdominal compartment
The abdominal compartment is a technical masterpiece as this small human cavity houses 8.5 m of intestine. Analogous to the skull, the abdomen can be considered as a relatively closed box with an anchorage above (costal arch) and rigid (spine and pelvis) or partially flexible walls (abdominal wall and diaphragm) filled with solid organs and hollow viscera [2]. The size and/or volume of the abdomen may be affected by the varying location of the diaphragm, the shifting position of the costal arch, the contractions of the abdominal wall, and the contents contained within the intestines.
The abdominal wall
The abdominal wall represents the boundaries of the abdominal cavity between the xyphoid bone and costal margins cranially and the iliac and pubic bones of the pelvis caudally. Cab is mainly defined by the elasticity of the different muscle layers of the abdominal wall (anterior and lateral parts) and to a lesser extent the diaphragm muscle.
Intra‐abdominal pressure and abdominal hypertension
Intra‐abdominal pressure
The IAP is the steady‐state pressure concealed within the abdominal cavity. The reference standard for intermittent IAP measurements is via the bladder. IAP should be expressed in mmHg and measured at the end of exhalation in the supine position after ensuring that abdominal muscle contractions are absent and with the transducer zeroed at the level where the midaxillary line crosses the iliac crest [1].
Baseline IAP
Also called resting, starting, static or opening IAP during laparoscopy, the baseline IAP is the IAP obtained at normal resting conditions [2]. Normal IAP is considered as 5–7 mmHg in healthy individuals, and approximately 10 mmHg in critically ill adults [5].
Intra‐abdominal hypertension (IAH)
IAH is defined as a sustained or repeated pathological elevation in IAP ≥ 12 mmHg. IAH is graded as follows: Grade I, IAP 12–15 mmHg; Grade II, IAP 16–20 mmHg; Grade III, IAP 21–25 mmHg; and Grade IV, IAP > 25 mmHg [1].
Abdominal compartment syndrome (ACS)
ACS is defined as a sustained IAP > 20 mmHg (with or without an abdominal perfusion pressure [APP] < 60 mmHg) that is associated with new organ dysfunction/failure. In contrast to IAH, ACS is an all‐or‐nothing phenomenon [1].
Delta IAP
∆IAP is calculated as the difference between the end‐inspiratory (IAPei) and the end‐expiratory (IAPee) IAP value. The higher the ∆IAP, the lower the Cab.
Abdominal pressure variation (APV)
APV is calculated as the difference between the IAPei and the IAPee value, or ∆IAP, divided by the mean IAP and is expressed as a percentage. The higher the APV, the lower the Cab.
Intra‐abdominal volume
Baseline IAV
Also called resting, starting or static IAV, the baseline IAV is the IAV at baseline conditions without additional pathologic volume increase or Cab decrease, with corresponding baseline IAP. The baseline IAV in healthy individuals is around 13 l [2].
Abdominal distension
This is defined as a sagittal abdominal diameter (approximately at the level of the umbilicus) higher than the virtual line between the xiphoid and symphysis pubis.
Abdominal workspace
This is the additional IAV that can be added to the baseline IAV when IAP is limited to a certain pressure (e.g., 14 mmHg during laparoscopic surgery). The normal workspace during laparoscopy ranges between 3 and 6 l.
Maximal stretched volume
The maximal volume is calculated as the baseline IAV + the maximal workspace resulting in maximal stretch of the abdominal cavity (from ellipse to sphere on a transverse plane). The maximal stretched volume depends on baseline IAP and Cab.
Abdominal compliance
Abdominal compliance
Cab is defined as the ease with which abdominal expansion can occur, and is determined by the elasticity of the abdominal wall and diaphragm. Increased compliance indicates a loss of elastic recoil of the abdominal wall. Decreased compliance means that the same change in IAV will result in a greater change in IAP. It should be expressed as the change in IAV per change in IAP (ml/mmHg) [1]. Normal Cab is around 250 to 450 ml/mmHg.
Abdominal PV relationship
Importantly, Cab is measured differently than IAP, it is only a part of the total abdominal pressure‐volume (PV) relationship.
The relationship between IAV and IAP is curvilinear with an initial linear part followed by an exponential increase once a critical volume is reached (Fig. 1).
Fig. 1.
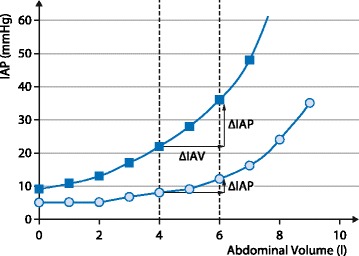
Pressure‐volume curve in the abdominal compartment. Abdominal pressure‐volume curves in a patient with low abdominal compliance (squares) and normal compliance (circles). At a baseline IAV of 4 l, the same 2 l increase in IAV will only lead to a small increase in IAP (5 mmHg) in a patient with good abdominal compliance versus a high increase in IAP (15 mmHg) in the case of a stiff abdominal wall and diaphragm. The compliance is 133 ml/mmHg [2000/(37 − 22)] versus 400 ml/mmHg [2000/(12 − 7)] for the same change in IAV from 4 to 6 l. Adapted from [2] with permission
Pathophysiology
Accommodation of the abdominal cavity
In contrast to the intracranial compartment that is confined within a rigid bony structure, the abdominal compartment can change shape during increasing IAV. During the initial phase of increasing IAV (e.g., laparoscopic insufflation), IAP only rises minimally (linear ‘reshaping phase’ from spherical to circular shape). This is followed by a ‘stretching phase’ of the rectus abdominis muscle (curvilinear phase) and finally, when further IAV is added, only small increases in IAV will result in dramatic increase in IAP (exponential ‘pressurization phase’) (Fig. 2) [6, 7]. During the stretching phase, the shape of the abdomen will change from elliptical to spherical. This change in shape is mainly due to an increase in the antero‐posterior diameter and a decrease in the transverse diameter (transverse plane) of the internal abdominal perimeter [8–12].
Fig. 2.
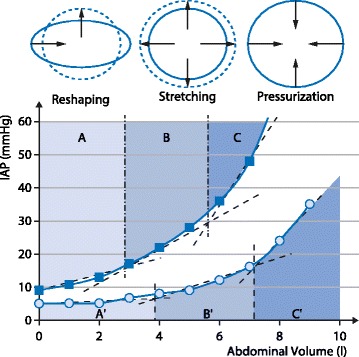
Accommodation of the abdominal cavity. Schematic representation of different phases during increasing intraabdominal volume (IAV) in two patients undergoing laparoscopy (CO2‐insufflation). Shaded areas represent the reshaping phase (light blue – A and A’), the stretching phase (medium blue – B and B’) and the pressurization phase (dark blue – C and C’). The apostrophe (’) indicates the patient with good abdominal compliance. In the patient with poor compliance, the reshaping phase went from an IAV of 0 to 2.8 l (vs 0 to 3.8 l when compliance was normal), the stretching phase from IAV of 2.8 to 5.6 l (vs 3.8 to 7.2 l) and the pressurization phase from > 5.6 l vs 7.2 l in the patient with normal compliance. Adapted from [2] with permission
Predictors for stretching and reshaping capacity
Factors determining the reshaping properties of the abdominal wall and diaphragm are not well understood but the mechanical properties are related to Cab. The stretching capacity is influenced by body anthropomorphy (weight, height, body mass index [BMI]), age, sex and visceral versus subcutaneous fat distribution [11]. Comorbidities like chronic obstructive lung disease (COPD) with emphysema (flatting of diaphragm), fluid overload (tissue and interstitial edema) or burn injury (with circular eschars) all have negative effects on stretching capacity. Android obesity usually results in increased visceral fat and a sphere‐like baseline shape of the abdominal cavity with poor stretching capacity, whereas gynoid obesity presents with more subcutaneous fat for the same BMI or abdominal perimeter (Fig. 3). In gynoid obesity, the internal abdominal perimeter is elliptical. Patients with an ellipse‐shaped internal perimeter have a much greater stretching capacity (and thus very good Cab).
Fig. 3.
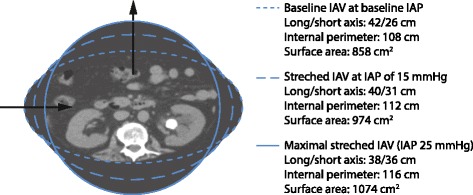
Evolution of internal abdominal cavity perimeter during increase in volume. In case of gynoid obesity, the internal abdominal perimeter is shaped as an ellipse. Patients with an ellipse‐shaped internal perimeter have a huge stretching capacity (and thus very good abdominal compliance); this is illustrated with the progression of the shape from ellipse (dotted line) at baseline to a sphere (solid line) at very high intra-abdominal pressures (IAP) obtained during laparoscopy. The arrows show the centripetal movement of the lateral edges of the ellipse and a centrifugal movement of the cranio‐caudal edges. During increase in intra-abdominal volume (IAV) from baseline to stretched and maximal stretched IAV, the difference between the long and short axes of the ellipse decreases, while the internal perimeter and surface area increase. At maximal stretch, the external and internal abdominal perimeter are equal. Patients with android obesity do not have this reshaping and stretching capability. Adapted from [2] with permission
Abdominal pressure-volume relationship
A linear abdominal PV relationship has been described previously. However, this was mainly in studies where the observed IAP values were < 15 mmHg. During laparoscopy with limitation of insufflation pressures at 12 to 15 mmHg, the IAV did not reach a critical point at which an exponential increase in IAP occured [13]. As discussed above, the initial phase of the PV curve may indeed be linear (as observed during laparoscopy) but the remaining part is curvilinear or rather exponential [13–15]. Because of this exponential relationship, it is important to know both the shape and the position on the curve, as the actual position will determine the corresponding Cab. In patients with IAH a small increase in IAV may push them into ACS (especially if Cab is low) and, vice versa, in patients with ACS a small decrease in IAV (with paracentesis) may result in a dramatic improvement in IAP.
Measurement
Intra‐abdominal pressure
Because of the fluid‐like nature of the abdomen, following Pascal’s law, the IAP can be measured in nearly every part of it. Rectal, uterine, inferior vena cava, bladder and gastric pressure measurements have all been described [16]. The use of direct intraperitoneal pressure measurement cannot be advocated in patients because of the complication risks, such as bleeding or infection. Bladder pressure measurements have been forwarded as the gold standard with the technique suggested in the WSACS consensus guidelines [1].
Intra‐abdominal volume
The abdominal volume is more difficult to measure. However, it can be estimated by anthropomorphic indices and imaging techniques. Anthropomorphic‐based indices for estimation of IAV have been described in obesity [17]. However, BMI does not correlate with Cab but does correlate with IAP at the resting volume. This only applies in healthy individuals and sometimes in critically ill patients. The external abdominal perimeter (or circumference), although often used in the past, correlates reasonably with IAV, but poorly with IAP [18]. Changes in external abdominal perimeter over time on the other hand may correlate well with changes in IAP [18]. Another useful parameter is the waist‐to‐hip ratio. The waist is the smallest horizontal girth between the rib cage and iliac crest and the hip is the largest horizontal girth between waist and thigh. The waist‐to‐hip ratio correlates with IAP in men only [17]. A promising index is the abdominal volume index (AVI). A formula developed for calculating AVI estimates the overall abdominal volume between the symphysis pubis and the xiphoid process. This measure theoretically includes intra‐abdominal fat and adipose volumes, with the waist and the hip dimensions. Although this index is superior to BMI, waist‐to‐hip ratio, and waist circumference, it has not yet been correlated to IAP [19]. Recently, techniques for estimating abdominal volume via three‐dimensional (3D) ultrasound, water‐suppressed breath hold magnetic resonance imaging (MRI), and computed tomography (CT) have been described. These techniques have not yet gained entrance to the intensive care unit (ICU). Although 3D ultrasound cannot measure IAV in toto, it estimates the volumes of separate intra‐abdominal organs. MRI and CT techniques calculate the visceral and subcutaneous fat volume or thus the volume of the adipose tissue. Quantitative CT analysis assessing volume, density and weight of abdominal organs may be a promising tool for the future [9, 10, 20, 21].
Abdominal compliance
Qualitative measurement of abdominal wall tension during palpation
The grade of indentation at the site where the downward force is applied can be measured during palpation of the abdomen. Palpation examines intra‐abdominal tension, passive and active muscle tension. However, it is not able to quantify Cab properly nor has it been validated in the clinical setting. The use of an abdominal tensiometer has also been described; however, this technique is only in its infancy [22].
PV relationship during laparoscopy with CO2 pneumoperitoneum
It has been observed that the compliance of the abdominal cavity decreases when additional volume is added [23]. The linear abdominal PV curve changed to a rather exponential shape when a pressure of 15 mmHg was achieved by insufflation of CO2 [13, 14]. In studies, the initial Cab at the beginning of the CO2 inflation varied between 333 and 400 ml/mmHg and at higher IAV (with corresponding IAP > 15 mmHg), the Cab decreased to 60 and 90 ml/mmHg [3]. Similar relationships have been described with addition or removal of gastric contents [3].
PV relationship during drainage or addition of abdominal free fluid
Measurements of Cab have been performed in humans by IAP assessment with at least two corresponding IAV values by addition of abdominal fluid during peritoneal dialysis or by drainage of intra‐abdominal fluid (ascites in liver cirrhosis, peripancreatic fluid or pseudocyst, serous fluid collections in trauma or burns) [2–4].
Interactions between different compartments
Polycompartment model
Being linked and bound by the diaphragm, the thoracic and abdominal compartments cannot be treated in isolation. Applied airway pressure (Paw) by mechanical ventilation will be transmitted to the lungs, pleural (Ppl) and abdominal spaces (IAP). In a simplified model, the lung and thorax are in series and coupled to the diaphragm and abdomen in series. Changes in IAP are paralleled by changes in Ppl. Changes in thoracic compliance will be reflected by changes in abdominal compliance and vice versa; as a consequence, increased IAP will result in reduced chest wall compliance. The interactions between different compartments have been referred to as the polycompartment model and syndrome [24, 25]. For example, transmission of airway pressures to the abdomen results from interactions between the thoracic and abdominal compartment and the percentage of pressure transmission is called the thoraco‐abdominal index (TAI) of transmission. This occurs in patients receiving positive pressure ventilation, application of positive end‐expiratory pressure (PEEP), presence of intrinsic or auto‐PEEP or a tension pneumothorax. Conversely, transmission of pressure from the abdomen to the thorax is called the abdomino‐thoracic index (ATI) and occurs in any physiologic (pregnancy) or pathologic condition associated with increased IAP; the ATI ranges from 20 to 80 % and is on average 50 % [26, 27]. The effects of increased IAP on end‐organ function are numerous: neurologic, respiratory, cardiovascular and renal adverse effects have all been described in patients with IAH and ACS. Increased IAP leads to diminished venous return, necessitating more fluid loading, causing mesenteric vein compression and venous hypertension, finally triggering a vicious cycle.
Estimation of abdominal compliance during low flow pressure volume loop
Cab can be estimated by analysis of the dynamic changes caused by mechanical ventilation on IAP. During a low flow PV loop to determine the best PEEP, one can observe the change in mean IAP. The compliance obtained by this maneuver can be calculated as follows:
with ∆VT the insufflated tidal volume and ∆IAP the difference between meanIAP at the end and start of the PV loop.
Estimation of abdominal compliance during mechanical ventilation
Whilst looking at the effects of tidal volume excursions on IAP and by calculating the difference between IAPei and IAPee, one can also obtain an idea of Cab [28]:
The higher the respiratory excursions seen in a continuous IAP tracing, the lower the Cab (for the same tidal volume). Alternatively, the higher the IAP, the higher the ∆IAP or the lower the Cab.
Calculation of abdominal pressure variation
As discussed previously, the higher the APV for any given IAP, the lower the Cab and vice versa, the lower the Cab, the higher the APV; hence APV can be used as a non‐invasive and continuous estimation of Cab.
Respiratory abdominal variation test (RAVT)
A final non‐invasive method for estimation of Cab can be done by performing a respiratory abdominal variation test (RAVT) (Fig. 4). The Cab obtained with RAVT correlates with the Cab obtained from ∆IAP during mechanical ventilation; increasing tidal volume increases IAPei while increasing PEEP increases IAPee.
Fig. 4.
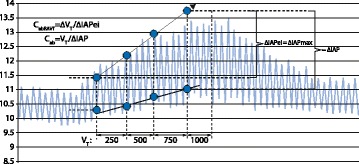
Estimation of abdominal compliance (Cab) during the respiratory abdominal variation test (RAVT) in intermittent positive pressure ventilation (IPPV)‐mode. The graph shows the smoothed average of a continuous intra-abdominal pressure (IAP) tracing (CiMON, Pulsion Medical System, Munich, Germany) obtained during the RAVT in IPPV mode. The tidal volume (VT) was increased stepwise from 250 to 1000 ml with increments of 250 ml. At each VT, the following parameters were recorded: end‐expiratory IAP (IAPee), end‐inspiratory IAP (IAPei), IAP and ∆IAP. With increasing VT mainly the IAPei increases whereas IAPee remains relatively unchanged. During the RAVT, the diaphragm is displaced caudally and an additional volume is added to the abdominal cavity. The ∆IAV is probably correlated to the ∆VT observed between the start and the end of the RAVT (= 750 ml). The slope of the curve connecting the IAPei at each VT can be used to estimate the Cab. The CabRAVT in the sample shown can be calculated as follows: CabRAVT = ∆VT/∆IAPei = 750/(13.6 − 11.5) = 357.1 ml/mmHg and this correlates well with the CabVT:CabVT = VT/∆IAP = 1000/(13.6 − 11) = 384.6 ml/mmHg. Adapted from [3] with permission
Prognostic and predictive factors related to abdominal compliance
Theoretically, Cab allows prediction of complications during laparoscopy and mechanical ventilation, identification of patients who would benefit from delayed abdominal closure, those in whom to monitor IAP, and those at risk during prone ventilation, etc. … Therefore, prediction of poor or high Cab can be clinically important.
Conditions associated with decreased abdominal compliance
Aside from risk factors for IAH, patients should also be screened for risk factors for decreased Cab. These are listed in Table 1 and can be divided into those related to body habitus and anthropomorphy; those related to comorbidities and/or increased non‐compressible IAV; and those related to the abdominal wall and diaphragm [3].
Table 1.
Factors associated with decreased abdominal compliance. Adapted from [2] with permission
| 1) Related to anthropomorphy and demographics | |
| - Android composition (sphere, apple shape) | |
| - Increased visceral fat | |
| - Waist‐to‐hip ratio > 1 | |
| - Short stature | |
| - Male sex | |
| - Young age (increased elastic recoil) | |
| - Obesity (weight, BMI) | |
| 2) Related to comorbidities and/or increased non‐compressible intra‐abdominal volume (IAV) | |
| - Fluid overload | |
| - Abdominal fluid collections, pseudocyst, abscess | |
| - Sepsis, burns, trauma and bleeding (coagulopathy) | |
| - Bowels filled with fluid | |
| - Stomach filled with fluid | |
| - Tense ascites | |
| - Hepatomegaly | |
| - Splenomegaly | |
| 3) Related to abdominal wall and diaphragm | |
| - Interstitial and anasarca edema (skin, abdominal wall) | |
| - Abdominal burn eschars (circular) | |
| - Thoracic burn eschars (circular) | |
| - Tight closure after abdominal surgery | |
| - Abdominal Velcro belt or adhesive drapes | |
| - Prone positioning | |
| - Head‐of‐bed > 45° | |
| - Umbilical hernia repair | |
| - Muscle contractions (pain) | |
| - Body builders (‘6‐pack’) | |
| - Pneumoperitoneum | |
| - Pneumatic anti‐shock garments | |
| - Abdominal wall bleeding | |
| - Rectus sheath hematoma | |
| - Correction of large hernias | |
| - Gastroschisis | |
| - Omphalocele | |
| - Mechanical ventilation (positive pressure) | |
| - Fighting with the ventilator | |
| - Use of accessory muscles | |
| - Use of positive end‐expiratory pressure (PEEP) | |
| - Presence of auto‐PEEP (tension pneumothorax) | |
| - Chronic obstructive pulmonary disease (COPD) emphysema (diaphragm flattening) | |
| - Basal pleuropneumonia |
Morbidly obese patients have a higher baseline IAP around 12–14 mmHg, and this is mainly related to the presence of central obesity [17, 29–32]. Morbidly obese patients with an android (mainly visceral and sphere shaped) fat distribution have a limited reserve to accommodate excess IAV than those patients who, for a similar BMI or abdominal perimeter, have a gynoid (mainly subcutaneous and ellipse shaped) fat distribution [17, 29]. On the other hand, subcutaneous fat accumulation may have a negative effect on the elastic properties of the abdominal wall, although the thin muscle layer may have a beneficial effect. Therefore, it is not possible to predict Cab in obese patients; in general Cab is decreased because of the increased baseline IAV.
Conditions associated with increased abdominal compliance
These are listed in Table 2 and can be divided into those related to body habitus and anthropomorphy; those related to absence of comorbidities and/or increased compressible IAV; and those related to abdominal wall and diaphragm. Chronic conditions will have higher Cab for the same change in IAV as illustrated in Fig. 5.
Table 2.
Factors associated with increased abdominal compliance. Adapted from [2] with permission
| 1) Related to anthropomorphy and demographics | |
| - Gynoid composition (ellipse, pear‐shaped) | |
| - Waist‐to‐hip ratio < 0.8 | |
| - Peripheral obesity | |
| - Preferentially subcutaneous fat | |
| - Height (tall stature) | |
| - Old age (loss of elastic recoil) | |
| - Female sex | |
| - Lean and slim body | |
| - Normal BMI | |
| 2) Related to absence of comorbidities and/or increased compressible intra‐abdominal volume (IAV) | |
| - Absence of deadly triad: normothermia, normal pH, normal coagulation | |
| - Bowels filled with air | |
| - Stomach filled with air | |
| - Absence of fluid overload (second or third space fluid accumulation) | |
| 3) Related to abdominal wall and diaphragm | |
| - Previous pregnancy | |
| - Previous laparoscopy | |
| - Previous abdominal surgery | |
| - Abdominal wall lift | |
| - Weight loss | |
| - Chronic intra‐abdominal hypertension (IAH) | |
| - Umbilical hernia (before repair) | |
| - Burn escharotomy (thorax and/or abdomen) | |
| - Avoidance of tight closure | |
| - Open abdomen with temporary abdominal closure | |
| - Beach chair positioning | |
| - Sedation and analgesia | |
| - Muscle relaxation | |
| - Bronchodilation | |
| - Lung protective ventilation | |
| - Pre‐stretching of fascia (cirrhosis with ascites, peritoneal dialysis when fluid is drained from abdomen) |
Fig. 5.
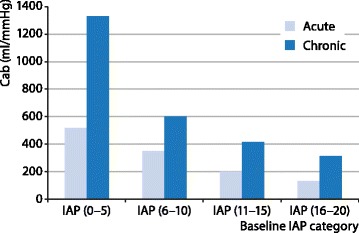
Abdominal compliance (Cab) in relation to baseline intra-abdominal pressure (IAP). Bar graph showing mean values of Cab (ml/mmHg) per baseline IAP category (mmHg) in acute (light blue bars) and chronic (dark blue bars) conditions. Acute conditions are laparoscopy and evacuation of ascites, collections or hematomas in acutely ill patients, whereas chronic condition refers to peritoneal dialysis. Adapted from [3] with permission
Previous stretching of the abdominal fascia increases Cab. This can be explained by a gradual prestretching of the internal abdominal cavity perimeter during acute or progressive increased IAV (as is the case during laparoscopy, with pregnancy, peritoneal dialysis, cirrhotic ascites) [7–9, 33, 34], which leads to increased reshaping capacity. Prestretching or overdistension may indeed result in tissue damage and fibrosis of the abdominal wall structure with lengthened muscle fibers and diminished elastic retraction capacity. History of a previous laparotomy may lead to scarring of the abdominal wall, which in combination with adhesions may cause decreased elasticity [33]. The Cab may be decreased or increased and the effect of previous laparotomy on baseline IAV and IAP is unpredictable. The use of external bandages (drapings, Velcro belt, etc.) or tight surgical closure causes a mechanical limitation; these should be avoided in high‐risk patients and IAP should be measured during their use. In case of capillary leak, fluid overload and fluid collections, IAV and IAP will both increase while reshaping capacity and wall compliance will decrease.
Treatment
How to decrease baseline IAP?
In simple terms, in order to reduce IAP, either (additional) IAV has to be removed intra-luminally or intra‐abdominally (e.g., weight loss, fluid removal via dialysis, ascites drainage, gastric suctioning, evacuation of abscess or hematoma, etc.), or the Cab has to be improved by increasing the internal abdominal cavity perimeter and surface area (pre‐stretching, open abdomen treatment) [35, 36]. Weight loss and the resulting decrease in BMI will decrease IAP [37].
How to reduce IAV?
The evacuation of intra‐luminal and intra‐abdominal contents can be done, for example, via placement of a nasogastric tube with suctioning with or without gastroprokinetics (cisapride, metoclopramide or erythromycin). Paracentesis with evacuation of ascites and the placement of a rectal tube in conjunction with enemas and colonoprokinetics (prostygmin) may also reduce IAV [38]. Colonic pseudo‐obstruction or Ogilvie’s syndrome may be treated with endoscopic decompression of large bowel or a surgical colostomy or ileostomy together with colonoprokinetics. When in doubt, imaging should be performed and ultrasound or CT guided drainage should be attempted in case of hematoma, abscess, fluid collections, etc. The correction of capillary leak and avoiding a positive fluid balance will eventually lead to a decreased IAV by decreasing organ and bowel edema [39]. This can be achieved with (hypertonic) albumin in combination with diuretics (furosemide), correction of capillary leak (antibiotics, source control, …), the use of colloids instead of crystalloids and eventually dialysis or continuous veno‐venous hemofiltration (CVVH) with ultrafiltration [40]. Targeted APP with the use of vasopressors will reduce venocongestion and this will lower IAV (in analogy to the effect of norepinephrine on intracranial pressure and cerebral perfusion pressure) and dobutamine (but not dopamine) will improve splanchnic perfusion. Ascorbinic acid has been associated with a reduced incidence of secondary ACS in burn patients, although its routine use has yet to be validated.
How to improve Cab?
Improvement in Cab should be performed in a stepwise approach as suggested by the WSACS consensus recommendations [1, 3].
First step: ensure adequate sedation and analgesia
Fentanyl should not be used as it may increase abdominal muscle tone while dexmedetomedine has superior effects over propofol. Thoracic epidural anesthesia has been shown to reduce IAP via an increase in Cab [41].
Second step: remove constrictive bandages and eschars
Any tight abdominal closure, like a Velcro belt to prevent incisional hernia in a patient with abdominal hypertension and end‐organ dysfunction, should be removed immediately. Likewise, escharotomies (abdominal but also thoracic) will increase Cab while sternotomy will increase not only thoracic wall compliance but also Cab [42–44]. Placing a chest tube in case of a tension pneumothorax or pleural effusion will also increase Cab.
Third step: avoid prone and head of bed > 30° and consider reverse Trendelenburg position
Body positioning, such as the Trendelenburg position, may lower bladder pressure; however, it may also compromise respiratory function [29]. The use of head‐of‐bed elevation > 30° may on the other hand increase bladder pressure and the head‐of‐bed 45° position will increase IAP by 5 to 15 mmHg [29]. Therefore, in patients with respiratory insufficiency who are mechanically ventilated, the anti‐Trendelenburg position may be best to allow lung recruitment, oxygenation and ventilation [16]. During prone positioning there is merit in unloading the abdomen (abdominal suspension) as this will result in a decrease in chest wall compliance, while the effect of gravity will improve Cab and decrease IAP. During laparoscopy, body position can also help to optimize the laparoscopic workspace IAV. The Trendelenburg position with head‐of‐bed at 20° provides the optimal workspace in lower abdominal laparoscopic surgery, while during upper abdominal laparoscopic surgery in obese patients, the beach‐chair position (flexing the legs in reverse Trendelenburg) is optimal [45]. Laparoscopic insufflation pressures should at all times be limited to 15 mmHg. Higher working pressures cannot be routinely recommended in obese patients with high baseline IAP and in morbidly obese patients, open surgery seems the best option because of the high complication risk associated with pneumoperitoneum [31].
Fourth step: lose weight and avoid fluid overload
Similar to weight loss, avoiding a positive cumulative fluid balance and obtaining a negative fluid balance with the use of diuretics in combination or not with hypertonic solutions (albumin 20 %) [40, 46] will decrease interstitial edema of the abdominal wall and increase Cab. Fluid resuscitation should be guided by volumetric (and not barometric) preload indicators and, if central venous pressure (CVP) is used, transmural pressures should be calculated:
In case diuretics do not have a sufficient effect, renal replacement therapy with hemodialysis or CVVH can be used [1, 3].
Fifth step: use neuromuscular blockers
Theoretically, the use of neuromuscular blockade should not only lower baseline IAP but also improve Cab [1, 3]. However, some studies showed no additional increase in Cab after full block of abdominal muscle contractions (guided by train of four) [7].
Sixth step: less invasive surgery
Recently a less invasive percutaneous endoscopic abdominal wall component separation (EACS) technique has been described [47]. With this technique, the abdominal capacity (maximal stretched volume) increased by 1 l while IAP decreased from 15.9 ± 2.1 to 11 ± 1.5 mmHg (p < 0.001) [47]. Another alternative for midline laparotomy is subcutaneous linea alba fasciotomy (SLAF), which seems a promising approach especially in secondary IAH and ACS [48].
When all the above listed treatment options fail to provide a sufficient decrease in IAP and IAV, the only definite solution is to perform a decompressive laparotomy that will assist with IAP, IAV and Cab [49].
Conclusion
Cab is a measure of the ease of abdominal expansion, determined by the elasticity of the abdominal wall and diaphragm. It is expressed as the change in IAV per change in IAP (ml/mmHg). The Cab baseline in ‘resting conditions’ is determined by the baseline IAP and IAV, the external and internal abdominal cavity perimeter and surface area and shape, the additional and maximal stretched volume, the presence of predisposing conditions and comorbidities as well as tissue properties of the fascia, abdominal wall and diaphragm. As such, Cab should be viewed separately from the abdominal wall and diaphragm compliance with its own specific elastic properties. Cab can be estimated based on demographic and anthropomorphic data and can be assessed by PV relationship analysis of the observed changes in IAP (mirroring induced changes in IAV). The abdominal PV relationship is believed to be linear up to pressures of 12–15 mmHg and increases exponentially thereafter. Cab can also be estimated non‐invasively by examining the interactions between pressure variations in the thorax and abdominal compartment during positive pressure ventilation. Cab is one of the most neglected parameters in critically ill patients, although it plays a key‐role in understanding organ‐organ interactions and the deleterious effects of unadapted IAV on IAP and end‐organ perfusion. A large overlap exists between the treatment of patients with IAH and those with low Cab, but when we identify the latter, we should potentially be able to anticipate and select the most appropriate medical or surgical treatment to avoid complications related to IAH or ACS.
Declarations
Open access publication of this article was funded by the corresponding author.
Footnotes
Competing interests
Dr Manu Malbrain is member of the Executive Committee of the World Society of the Abdominal Compartment (WSACS) and current Treasurer; he is member of the medical advisory board of Pulsion Medical Systems (Maquet Getinge group). The other authors have no possible conflicts of interest related to the content of this paper.
Authors’ contributions
All authors read and approved the final manuscript.
Contributor Information
Manu L. N. G. Malbrain, Email: manu.malbrain@skynet.be
Yannick Peeters, Email: yannickpeeters@hotmail.com.
Robert Wise, Email: robertwise@webafrica.org.za.
References
- 1.Kirkpatrick AW, Roberts DJ, De Waele J, et al. Intra-abdominal hypertension and the abdominal compartment syndrome: updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013;39:1190–1206. doi: 10.1007/s00134-013-2906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malbrain MLNG, Roberts DJ, De Laet I. The role of abdominal compliance, the neglected parameter in critically ill patients – a consensus review of 16. Part 1: Definitions and pathophysiology. Anaesthesiol Intensive Ther. 2014;46:392–405. doi: 10.5603/AIT.2014.0062. [DOI] [PubMed] [Google Scholar]
- 3.Malbrain MLNG, De Laet I, De Waele J. The role of abdominal compliance, the neglected parameter in critically ill patients – a consensus review of 16. Part 2: Measurement techniques and management recommendations. Anaesthesiol Intensive Ther. 2014;46:406–432. doi: 10.5603/AIT.2014.0063. [DOI] [PubMed] [Google Scholar]
- 4.Blaser AR, Bjorck M, De Keulenaer B, Regli A. Abdominal compliance: a bench-to-bedside review. J Trauma Acute Care Surg. 2015;78:1044–1053. doi: 10.1097/TA.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 5.Malbrain ML, Chiumello D, Pelosi P, et al. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med. 2005;33:315–322. doi: 10.1097/01.CCM.0000153408.09806.1B. [DOI] [PubMed] [Google Scholar]
- 6.Mulier JP, Dillemans B, Heremans L. Determinants of the abdominal pressure volume relation in non ACS patients. Acta Clin Belg Suppl. 2007;62:289. [Google Scholar]
- 7.Mulier J, Dillemans B, Crombach M, Missant C, Sels A. On the abdominal pressure volume relationship. Internet J Anesthesiol. 2008;21:1. [Google Scholar]
- 8.Song C, Alijani A, Frank T, Hanna GB, Cuschieri A. Mechanical properties of the human abdominal wall measured in vivo during insufflation for laparoscopic surgery. Surg Endosc. 2006;20:987–990. doi: 10.1007/s00464-005-0676-6. [DOI] [PubMed] [Google Scholar]
- 9.Vlot J, Wijnen R, Stolker RJ, Bax KN. Optimizing working space in laparoscopy: CT measurement of the effect of pre-stretching of the abdominal wall in a porcine model. Surg Endosc. 2014;28:841–846. doi: 10.1007/s00464-013-3229-4. [DOI] [PubMed] [Google Scholar]
- 10.Accarino A, Perez F, Azpiroz F, Quiroga S, Malagelada JR. Abdominal distention results from caudo-ventral redistribution of contents. Gastroenterology. 2009;136:1544–1551. doi: 10.1053/j.gastro.2009.01.067. [DOI] [PubMed] [Google Scholar]
- 11.Mulier JP, Coenegrachts K, Van de Moortele K. CT analysis of the elastic deformation and elongation of the abdominal wall during colon insufflation for virtual coloscopy. Eur J Anesth. 2008;25(S44):42 (abst). doi: 10.1097/00003643-200805001-00132. [DOI] [Google Scholar]
- 12.Villoria A, Azpiroz F, Soldevilla A, Perez F, Malagelada JR. Abdominal accommodation: a coordinated adaptation of the abdominal wall to its content. Am J Gastroenterol. 2008;103:2807–2815. doi: 10.1111/j.1572-0241.2008.02141.x. [DOI] [PubMed] [Google Scholar]
- 13.Abu-Rafea B, Vilos GA, Vilos AG, Hollett-Caines J, Al-Omran M. Effect of body habitus and parity on insufflated CO2 volume at various intraabdominal pressures during laparoscopic access in women. J Minim Invasive Gynecol. 2006;13:205–210. doi: 10.1016/j.jmig.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 14.McDougall EM, Figenshau RS, Clayman RV, Monk TG, Smith DS. Laparoscopic pneumoperitoneum: impact of body habitus. J Laparoendosc Surg. 1994;4:385–391. doi: 10.1089/lps.1994.4.385. [DOI] [PubMed] [Google Scholar]
- 15.Fischbach M, Terzic J, Laugel V, Escande B, Dangelser C, Helmstetter A. Measurement of hydrostatic intraperitoneal pressure: a useful tool for the improvement of dialysis dose prescription. Pediatr Nephrol. 2003;18:976–980. doi: 10.1007/s00467-003-1199-9. [DOI] [PubMed] [Google Scholar]
- 16.Malbrain ML. Different techniques to measure intra-abdominal pressure (IAP): time for a critical re-appraisal. Intensive Care Med. 2004;30:357–371. doi: 10.1007/s00134-003-2107-2. [DOI] [PubMed] [Google Scholar]
- 17.Sugerman H, Windsor A, Bessos M, Wolfe L. Intra-abdominal pressure, sagittal abdominal diameter and obesity comorbidity. J Intern Med. 1997;241:71–79. doi: 10.1046/j.1365-2796.1997.89104000.x. [DOI] [PubMed] [Google Scholar]
- 18.Malbrain ML, De Laet I, Van Regenmortel N, Schoonheydt K, Dits H. Can the abdominal perimeter be used as an accurate estimation of intra-abdominal pressure? Crit Care Med. 2009;37:316–319. doi: 10.1097/CCM.0b013e318192678e. [DOI] [PubMed] [Google Scholar]
- 19.Guerrero-Romero F, Rodriguez-Moran M. Abdominal volume index. An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. 2003;34:428–432. doi: 10.1016/S0188-4409(03)00073-0. [DOI] [PubMed] [Google Scholar]
- 20.Kirkpatrick AW, Colistro R, Laupland KB, et al. Renal arterial resistive index response to intraabdominal hypertension in a porcine model. Crit Care Med. 2007;35:207–213. doi: 10.1097/01.CCM.0000249824.48222.B7. [DOI] [PubMed] [Google Scholar]
- 21.Forstemann T, Trzewik J, Holste J, et al. Forces and deformations of the abdominal wall – a mechanical and geometrical approach to the linea alba. J Biomech. 2011;44:600–606. doi: 10.1016/j.jbiomech.2010.11.021. [DOI] [PubMed] [Google Scholar]
- 22.van Ramshorst GH, Salih M, Hop WC, et al. Noninvasive assessment of intra-abdominal pressure by measurement of abdominal wall tension. J Surg Res. 2011;171:240–244. doi: 10.1016/j.jss.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 23.Gilroy RJ, Jr, Lavietes MH, Loring SH, Mangura BT. Mead J (1985) Respiratory mechanical effects of abdominal distension. J Appl Physiol. 1985;58:1997–2003. doi: 10.1152/jappl.1985.58.6.1997. [DOI] [PubMed] [Google Scholar]
- 24.Malbrain ML, Wilmer A. The polycompartment syndrome: towards an understanding of the interactions between different compartments! Intensive Care Med. 2007;33:1869–1872. doi: 10.1007/s00134-007-0843-4. [DOI] [PubMed] [Google Scholar]
- 25.Malbrain MLNG, Roberts DJ, Sugrue M, et al. The polycompartment syndrome: a concise state-of-the-art review. Anaesthesiol Intensive Ther. 2014;46:433–450. doi: 10.5603/AIT.2014.0064. [DOI] [PubMed] [Google Scholar]
- 26.Wauters J, Wilmer A, Valenza F. Abdomino-thoracic transmission during ACS: facts and figures. Acta Clin Belg Suppl. 2007;62:200–205. doi: 10.1179/acb.2007.62.s1.026. [DOI] [PubMed] [Google Scholar]
- 27.Wauters J, Claus P, Brosens N, et al. Relationship between abdominal pressure, pulmonary compliance, and cardiac preload in a porcine model. Crit Care Res Pract. 2012;2012:763181. doi: 10.1155/2012/763181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sturini E, Saporito A, Sugrue M, Parr MJ, Bishop G, Braschi A. Respiratory variation of intra-abdominal pressure: indirect indicator of abdominal compliance? Intensive Care Med. 2008;34:1632–1637. doi: 10.1007/s00134-008-1155-z. [DOI] [PubMed] [Google Scholar]
- 29.De Keulenaer BL, De Waele JJ, Powell B, Malbrain ML. What is normal intra-abdominal pressure and how is it affected by positioning, body mass and positive end-expiratory pressure? Intensive Care Med. 2009;35:969–976. doi: 10.1007/s00134-009-1445-0. [DOI] [PubMed] [Google Scholar]
- 30.Lambert DM, Marceau S, Forse RA. Intra-abdominal pressure in the morbidly obese. Obes Surg. 2005;15:1225–1232. doi: 10.1381/096089205774512546. [DOI] [PubMed] [Google Scholar]
- 31.Nguyen NT, Wolfe BM. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241:219–226. doi: 10.1097/01.sla.0000151791.93571.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugerman HJ. Increased intra-abdominal pressure in obesity. Int J Obes Relat Metab Disord. 1998;22:1138. doi: 10.1038/sj.ijo.0800757. [DOI] [PubMed] [Google Scholar]
- 33.Verbeke K, Casier I, Van Acker B, Dillemans B, Mulier J. Impact of laparoscopy on the abdominal compliance is determined by the duration of the pneumoperitoneum the number of gravidity and the existence of a previous laparoscopy or laparotomy. Eur J Anesth. 2010;27:29–30. doi: 10.1097/00003643-201006121-00093. [DOI] [Google Scholar]
- 34.Becker V, Schmid RM, Umgelter A. Comparison of a new device for the continuous intra-gastric measurement of intra-abdominal pressure (CiMon) with direct intra-peritoneal measurements in cirrhotic patients during paracentesis. Intensive Care Med. 2009;35:948–952. doi: 10.1007/s00134-009-1451-2. [DOI] [PubMed] [Google Scholar]
- 35.Cheatham ML, Malbrain ML, Kirkpatrick A, et al. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med. 2007;33:951–962. doi: 10.1007/s00134-007-0592-4. [DOI] [PubMed] [Google Scholar]
- 36.De Laet I, Malbrain ML. ICU management of the patient with intra-abdominal hypertension: what to do, when and to whom? Acta Clin Belg. 2007;62(Suppl):190–199. doi: 10.1179/acb.2007.62.s1.025. [DOI] [PubMed] [Google Scholar]
- 37.Sugerman H, Windsor A, Bessos M, Kellum J, Reines H, DeMaria E. Effects of surgically induced weight loss on urinary bladder pressure, sagittal abdominal diameter and obesity co-morbidity. Int J Obes Relat Metab Disord. 1998;22:230–235. doi: 10.1038/sj.ijo.0800574. [DOI] [PubMed] [Google Scholar]
- 38.Cheatham ML, Safcsak K. Percutaneous catheter decompression in the treatment of elevated intraabdominal pressure. Chest. 2011;140:1428–1435. doi: 10.1378/chest.10-2789. [DOI] [PubMed] [Google Scholar]
- 39.Cordemans C, De Laet I, Van Regenmortel N, et al. Fluid management in critically ill patients: the role of extravascular lung water, abdominal hypertension, capillary leak and fluid balance. Ann Intensive Care. 2012;2(Suppl 1):S1. doi: 10.1186/2110-5820-2-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cordemans C, De Laet I, Van Regenmortel N, et al. Aiming for a negative fluid balance in patients with acute lung injury and increased intra-abdominal pressure: a pilot study looking at the effects of PAL-treatment. Ann Intensive Care. 2012;2(Suppl 1):15. doi: 10.1186/2110-5820-2-S1-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hakobyan RV, Mkhoyan GG. Epidural analgesia decreases intraabdominal pressure in postoperative patients with primary intra-abdominal hypertension. Acta Clin Belg. 2008;63:86–92. doi: 10.1179/acb.2008.63.2.005. [DOI] [PubMed] [Google Scholar]
- 42.Tsoutsos D, Rodopoulou S, Keramidas E, Lagios M, Stamatopoulos K, Ioannovich J. Early escharotomy as a measure to reduce intraabdominal hypertension in full-thickness burns of the thoracic and abdominal area. World J Surg. 2003;27:1323–1328. doi: 10.1007/s00268-003-6962-3. [DOI] [PubMed] [Google Scholar]
- 43.Oda J, Ueyama M, Yamashita K, et al. Effects of escharotomy as abdominal decompression on cardiopulmonary function and visceral perfusion in abdominal compartment syndrome with burn patients. J Trauma. 2005;59:369–374. doi: 10.1097/01.ta.0000174917.90514.4a. [DOI] [PubMed] [Google Scholar]
- 44.Bloomfield GL, Ridings PC, Blocher CR, Marmarou A, Sugerman HJ. A proposed relationship between increased intra-abdominal, intrathoracic, and intracranial pressure. Crit Care Med. 1997;25:496–503. doi: 10.1097/00003246-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 45.Mulier JP, Dillemans B, Van Cauwenberge S. Impact of the patient’s body position on the intraabdominal workspace during laparoscopic surgery. Surg Endosc. 2010;24:1398–1402. doi: 10.1007/s00464-009-0785-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malbrain ML, Marik PE, Witters I, et al. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. 2014;46:361–380. doi: 10.5603/AIT.2014.0060. [DOI] [PubMed] [Google Scholar]
- 47.Voss M, Pinheiro J, Reynolds J, et al. Endoscopic components separation for abdominal compartment syndrome. Am J Surg. 2003;186:158–163. doi: 10.1016/S0002-9610(03)00171-5. [DOI] [PubMed] [Google Scholar]
- 48.Leppaniemi A, Hienonen P, Mentula P, Kemppainen E. Subcutaneous linea alba fasciotomy, does it really work? Am Surg. 2011;77:99–102. [PubMed] [Google Scholar]
- 49.De Waele JJ, Hoste EA, Malbrain ML. Decompressive laparotomy for abdominal compartment syndrome – a critical analysis. Crit Care. 2006;10:R51. doi: 10.1186/cc4870. [DOI] [PMC free article] [PubMed] [Google Scholar]


