Abstract
Objective:
The World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) is a disability scale included in Section 3 of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as a possible replacement for the Global Assessment of Functioning Scale (GAF). To assist Canadian psychiatrists with interpretation of the scale, we have conducted a descriptive analysis using data from the 2012 Canadian Community Health Survey–Mental Health component (CCHS-MH).
Methods:
The 2012 CCHS-MH was a cross-sectional survey of the Canadian community (n = 23,757). The survey included an abbreviated 12-item version of the WHODAS 2.0. Mental disorder diagnoses were assessed for schizophrenia, other psychosis, major depressive episode (MDE), generalized anxiety disorder (GAD), bipolar I disorder, substance abuse/dependence, and alcohol abuse/dependence.
Results:
Mean scores ranged from 14.2 (95% CI, 14.1 to 14.3) for the overall community population to 23.1 (95% CI, 19.5 to 26.7) for those with schizophrenia, with higher scores indicating greater disability. Furthermore, the difference in scores between those with lifetime and past-month episodes suggests that the scale is sensitive to changes occurring during the course of these disorders; for example, scores varied from 23.6 (95% CI, 22.2 to 25.1) for past-month MDE to 14.4 (95% CI, 14.2 to 14.7) in the lifetime MDE group without a past-year episode.
Conclusion:
This analysis suggests that the WHODAS 2.0 may be a suitable replacement for the GAF. As a disability measure, even though it is not a mental health–specific instrument, the 12-item WHODAS 2.0 appears to be sensitive to the impact of mental disorders and to changes over the time course of a mental disorder. However, the clinical utility of this measure requires additional assessment.
Keywords: mental disorders, disability, World Health Organization Disability Assessment Schedule 2.0, WHODAS, descriptive statistics, disability evaluation, population characteristics, psychiatric epidemiology
Abstract
Objectif:
Le WHODAS 2.0 est une échelle d’invalidité incluse dans le chapitre 3 du DSM-5 comme remplacement possible de l’Échelle d’évaluation globale du fonctionnement (GAF). Pour aider les psychiatres canadiens à interpréter l’échelle, nous avons mené une analyse descriptive à l’aide des données de l’Enquête sur la santé dans les collectivités canadiennes - Santé mentale (ESCC – SM) de 2012.
Méthodes:
L’ESCC - SM de 2012 était une enquête transversale menée dans les collectivités canadiennes (n = 23 757). L’enquête comprenait une version abrégée en 12 items de WHODAS 2.0. Les diagnostics de trouble mental ont été évalués pour la schizophrénie, d’autres psychoses, l’épisode de dépression majeure (EDM), le trouble d’anxiété généralisée (TAG), le trouble bipolaire I, le trouble lié à l’abus/dépendance de substances, et abus/dépendance d’alcool.
Résultats:
Les scores moyens s’échelonnaient de 14,2 (IC à 95% 14,1 à 14,3) pour la population générale des collectivités, à 23,1 (IC à 95% 19,5 à 26,7) pour les personnes souffrant de schizophrénie, les scores élevés indiquant une plus grande invalidité. En outre, la différence de scores entre ceux ayant des épisodes de durée de vie et ceux ayant des épisodes du mois précédent suggère que l’échelle est sensible aux changements qui surviennent durant le cours de ces maladies; par exemple, les scores variaient de 23,6 (IC à 95% 22,2 à 25,1) pour les EDM du mois précédent à 14,4 (IC à 95% 14,2 à 14,7) dans le groupe des EDM de durée de vie sans épisode l’année précédente.
Conclusion:
Cette analyse suggère que le WHODAS 2.0 puisse être un remplacement approprié de la GAF. Comme mesure d’invalidité, même si ce n’est pas un instrument spécifique de santé mentale, le WHODAS 2.0 en 12 items semble être sensible à l’impact des troubles mentaux, et aux changements qui surviennent au cours d’un trouble mental. Cependant, l’utilité clinique de cette mesure nécessite une évaluation additionnelle.
A significant portion of the global burden of disease is attributable to mental disorders and their resulting disability,1 and functioning is an important element of psychiatric diagnosis.2 The World Health Organization (WHO) recognizes the overlapping, but distinct, nature of medical diagnoses and their accompanying functional limitations (i.e., disability).3
Given the importance of valid and reliable measures of disability, the WHO developed the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) as a standardized measure of disability across cultures and health conditions. The WHODAS 2.0 is based on the WHO International Classification of Functioning, Disability and Health biopsychosocial model of disability.3 As defined by the WHO, disability is “the interaction between individuals with a health condition and personal and environmental factors,”4 and it encompasses impairments, activity limitations, and participation restrictions.1 The reliability and validity of the WHODAS 2.0 have been established through field studies in multiple countries using subjects aged 18 years and older and including those with mental, emotional, alcohol, and/or drug use problems.5 In clinical studies, the WHODAS 2.0 has been shown to be sensitive to changes in patients’ functioning, such as pre- and postintervention.5 Further psychometric property testing is ongoing for the 12-item WHODAS 2.0. It has been found to have strong internal consistency, as well as convergent and discriminatory validity in major depressive episode (MDE).6 Its reliability and validity have also been demonstrated in Huntington disease.7 Unlike the Global Assessment of Functioning Scale (GAF), which asked raters to incorporate only the effects of mental disorders in their scoring, the WHODAS 2.0 is a general functional measure, reflecting the WHO philosophy that functional limitations are distinct from clinical diagnoses.3,4,8
The full 36-item version of the WHODAS 2.0 was developed by selecting items based on the item-response theory (IRT) psychometric technique.5 It requires 20 minutes to administer and allows users to obtain scores for 6 domains of functioning.3 In comparison, the short 12-item version uses a subset of the original questions, including 2 from each domain of function, and accounts for 81% of the variance in 36-item version.5 The 12-item version requires only 5 minutes to administer and has been used in several population-level surveys to date.3 The WHODAS 2.0 is in the public domain and is free to use.3
In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the GAF has been removed and the 36-item WHODAS 2.0, a possible GAF replacement, is included in Section 3 as an “emerging measure.”8 Despite its strengths as a psychometric tool, the widespread adoption of the WHODAS 2.0 faces several hurdles. Clinically, it lacks the interpretability and imbued meaning of the GAF, which has been employed in the domains of medicine, law, and insurance.2 There is a need to identify meaningful severity thresholds and normative values for WHODAS 2.0 disability scores across sociodemographic characteristics and in the context of different mental disorders.2,9 Routine outcomes assessment is increasingly being used to monitor the effectiveness of services, and the WHODAS 2.0 may able to play a role in this. On the other hand, the WHODAS 2.0 is a formal scale and may be less convenient to clinicians than the GAF. A GAF could be assigned after a routine assessment, without need of additional forms or other materials. To be useful, the WHODAS 2.0 needs to reflect the impact of mental disorders, be sensitive to change over time, and be acceptable to clinicians in busy clinical settings.
The objectives of this project were to describe WHODAS 2.0 scores in the general Canadian community population and in those with selected mental disorders. A second objective was to describe the pattern of scores in relation to the timing of illness occurrence for major depressive disorder (MDD). To assess whether the WHODAS 2.0 reflected clinical characteristics of MDD, patterns of item endorsement for Canadians experiencing an MDE in the past 12 months were examined. This study did not seek to decisively assess the utility of the scale, since this depends on its acceptability to clinicians, which could not be assessed in this study.
Methods
Canadian Community Health Survey–Mental Health Component
The 2012 Canadian Community Health Survey–Mental Health component (CCHS-MH) was a cross-sectional national survey of the Canadian household population. Data collection occurred from January to December 2012, with a population representative sample and a response rate of 69%. Interviews were completed preferentially in person and over the phone as required (13% of all interviews) by trained interviewers using computer-assisted interviewing.10 The survey excluded those living in the 3 territories, on aboriginal reserves or settlements, in institutions, or those working full-time in the military; these exclusions accounted for <3% of the Canadian population.8 More information on the methods is available elsewhere.10
Diagnosing Mental Disorders with the CCHS-MH
The CCHS-MH includes chronic health condition screening to document professionally diagnosed self-reported health conditions and also includes validated Composite International Diagnostic Interview (CIDI) modules to diagnose past-year and lifetime episodes of certain mental disorders.11 Schizophrenia and other psychosis diagnoses were determined using self-report of professional diagnoses.
The CIDI was used to determine diagnoses of MDE, generalized anxiety disorder (GAD), bipolar I disorder, substance abuse/dependence, and alcohol abuse/dependence. Among those with a past-year episode of mental disorder, subjects also were asked whether the period of dysfunction occurred in the past month. Bipolar I disorder was diagnosed if a subject had lifetime bipolar disorder (with ≥1 episode of mania) and either a manic or depressive episode in the reference time period. Thus, for these CIDI-diagnosed mental disorders, it was possible to divide subjects into mutually exclusive groups depending on whether they had an episode in the past month, past 12 months, or lifetime.
A group of “healthy” Canadians was identified that had no CIDI mental disorder diagnosis and did not endorse any mental, physical, or unknown chronic condition. This group may include some people with mental disorders not covered by the CIDI and also those with unreported chronic conditions. Because the coverage of mental disorders was limited, assessment of comorbidity could have been inaccurate. Therefore, patterns of comorbidity were not assessed in the analysis.
Scoring the WHODAS 2.0
The 12-item WHODAS 2.0 contains 12 Likert-style scale questions with possible responses ranging from “none” to an “extreme” amount of difficulty with an area of function in the past 30 days. Whereas it is possible to compute responses to the WHODAS 2.0 algorithmically using IRT weighting,5 this analysis presents results obtained using the “simple scoring” method to compute WHODAS scores.5 The WHODAS manual states that simple scoring is sufficient to “describe the degree of functional limitations,” due to the one-dimensional structure and high internal consistency of the scale.3 The DSM-5 advocates the simple scoring method in clinical practice to generate a “total general disability score” due to its greater practicality.8 In this analysis, correlation between IRT and simple scoring methods of the 12-item WHODAS 2.0 was very strong (Spearman’s ρ = 0.999, P < 0.001).
Simple scores are obtained by summing the values attributed to each answer, wherein “none” = 1, “mild” = 2, “moderate” = 3, “severe” = 4, and “extreme” = 5. Possible scores for the 12-item WHODAS 2.0 range from 12 to 60; a score of 12 indicates that for all items, endorsement was “none.” As directed in the WHODAS manual, imputation from the mean score was used for individuals missing 1 of 12 answers on the 12-item WHODAS 2.0.3 Individuals missing more than 1 WHODAS answer were not included in the analysis.
WHODAS 2.0 frames of reference
The WHODAS 2.0 seeks information on the difficulties subjects experience due to “any short or long lasting health condition related to diseases or illnesses, injuries, mental or emotional problems and problems with alcohol or drugs” (p. 130).12 For this analysis, respondents who answered “not applicable” for the questions on difficulty with joining community activities or day-to-day work/school activities were recoded to “none,” under the assumption that these responses indicated a lack of impairment.
Statistical Analysis
The analysis consists of descriptive statistics conducted in Stata, version 13.13 Replicate bootstrapped weights provided by Statistics Canada were used to ensure representation of the Canadian community household-dwelling population, accounting for unequal selection probabilities and clustering arising from the sampling design. However, score percentiles were performed using analytic weights due to limitations with the bootstrapping weighting technique.
Results
The CCHS-MH collected 25,113 valid interviews.10 In this analysis, 1267 subjects were excluded as being <18 years old, and 89 were excluded for having >1 missing answer on the 12-item WHODAS 2.0 and/or providing no information on chronic health conditions or CIDI modules. The CCHS-MH sample included 23,757 respondents (Table 1). Of the subjects, 9.8% (95% CI, 9.2% to 10.4%) were found to have an existing selected mental disorder, which included those with a self-reported diagnosis of schizophrenia and/or other psychosis or CIDI diagnosis of past 12-month MDE, GAD, bipolar I disorder, substance abuse/dependence, and/or alcohol abuse/dependence.
Table 1.
Sociodemographic Characteristics of Canadian Community Health Survey Population (Weighted), Age ≥18 (N = 23,757).
| Variable | Measures (95% CI) |
|---|---|
| Age (y) | |
| Mean | 47.1 (47.0-47.3) |
| Range | 18-102 |
| Percentiles | |
| 25th | 33 |
| 50th | 47 |
| 75th | 60 |
| Sex (%) | |
| Male | 49.1 (49.0-49.3) |
| Female | 50.9 (50.7-51.0) |
| Education (%) | |
| Up to high school | 18.0 (17.2-18.8) |
| More than high school | 82.0 (81.2-82.8) |
| Marital status (%) | |
| Married/common law | 63.2 (62.2-64.2) |
| Single (never married) | 23.3 (22.5-24.1) |
| Widowed/separated/divorced | 13.5 (12.9-14.2) |
| Estimated household income (%) | |
| <$15,000 | 4.5 (4.1-5.0) |
| $15,000-$39,999 | 21.8 (20.9-22.6) |
| $40,000-$64,999 | 24.0 (23.1-24.9) |
| $65,000-$89,999 | 16.3 (15.4-17.1) |
| ≥$90,000 | 33.4 (32.2-34.6) |
Canadian Community Population
The mean score on the 12-item WHODAS 2.0 was 14.2 (95% CI, 14.1 to 14.3). The Canadian community population modal score was 12, and the proportion responding “none” to all items was 59.2% (95% CI, 58.1% to 60.3%). The 25th, 50th (median), and 75th percentiles for mean scores were 12, 12, and 14, respectively.
Mean item scores in the community population were highest for “walking a long distance” (1.39; 95% CI, 1.37 to 1.41), “standing long periods” (1.34; 95% CI, 1.32 to 1.35), “affected emotionally” (1.33; 95% CI, 1.31 to 1.34), and “household responsibilities” (1.26; 95% CI, 1.24 to 1.27). Response rate was >99.6% for all questions.
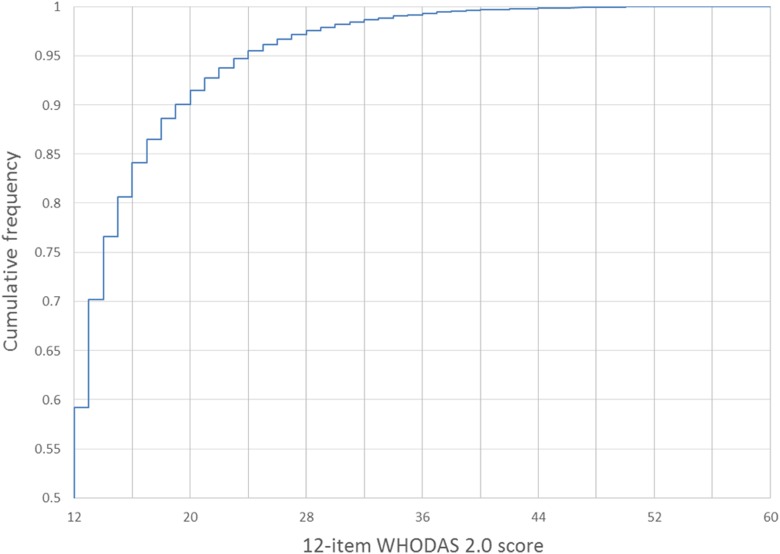
The population percentiles of scores are shown on a cumulative distribution of 12-item WHODAS 2.0 scores for the Canadian population (Figure 1). A score of 16 roughly corresponds to the 80th population percentile and a score of 20 to the 90th.
Figure 1.
The distribution of the 12-item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) scores in the community population, allowing for the imputation of the population percentiles of scores.
Selected Mental Disorders
Mean 12-item WHODAS 2.0 scores in subjects with current mental disorders ranged from 15.2 (95% CI, 14.7 to 15.7) in those with alcohol use disorders to 23.1 (95% CI, 19.5 to 26.7) in those with schizophrenia. Of those with a current mental disorder other than the substance use disorders, it is notable that mean (and median) 12-item WHODAS 2.0 scores for those with schizophrenia, GAD, and bipolar I disorder are in the top 10% of the population in terms of disability (Table 2). In healthy subjects, 80% (95% CI, 79% to 82%) did not endorse any items (“none” for all), but less than one-fifth of subjects with schizophrenia, other psychosis, MDD, GAD, and bipolar I disorder had no disability on any items, including only 4% (95% CI, 0% to 8%) of those with bipolar I disorder. Among those with current mental disorder, 48.9% (95% CI, 47.7% to 50.1%) of subjects with mental disorder(s) have an identified comorbid physical disorder(s).
Table 2.
Mean 12-Item World Health Organization Disability Assessment Schedule 2.0 Scores and Percentiles in Community Population and in Those with a Current Mental Disorder.
| Weighted Score Percentile | ||||||
|---|---|---|---|---|---|---|
| Disorder Group | Mean Score (95% CI) | 25th | 50th | 75th | 90th | 95th |
| Community population | 14.2 (14.1-14.3) | 12 | 12 | 14 | 19 | 24 |
| Depression | 20.4 (19.6-21.1) | 14 | 18 | 25 | 33 | 38 |
| Generalized anxiety disorder | 22.4 (21.2-23.6) | 15 | 21 | 27 | 35 | 41 |
| Bipolar I | 22.0 (20.0-24.0) | 16 | 21 | 27 | 33 | 33 |
| Schizophrenia | 23.1 (19.5-26.7) | 14 | 25 | 28 | 35 | 47 |
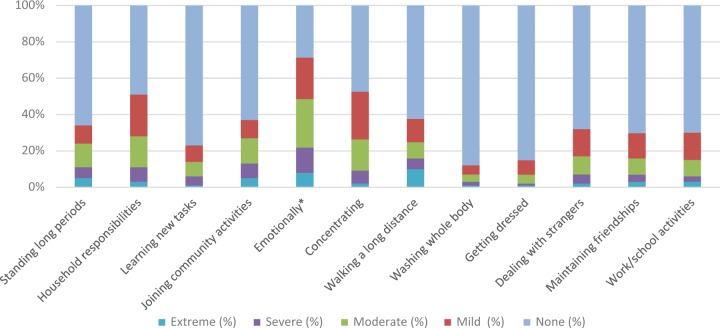
In subjects with an MDE in the past 12 months, severity by item is visualized in Figure 2. More than 50% of respondents have at least mild difficulty with household responsibilities and concentration and are emotionally affected by their health condition(s). While self-care (washing and dressing oneself) is not highly endorsed, >30% of respondents have at least mild difficulty walking long distances and standing for long periods. The endorsement of mobility symptoms is likely due mostly to comorbid physical conditions.
Figure 2.
The proportion of respondents with past 12-month major depressive episode (MDE) reporting “none,” “mild,” “moderate,” “severe,” and “extreme” as the amount of difficulty for each item. *The wording of this item refers to the magnitude of being emotionally affected rather than amount of difficulty.
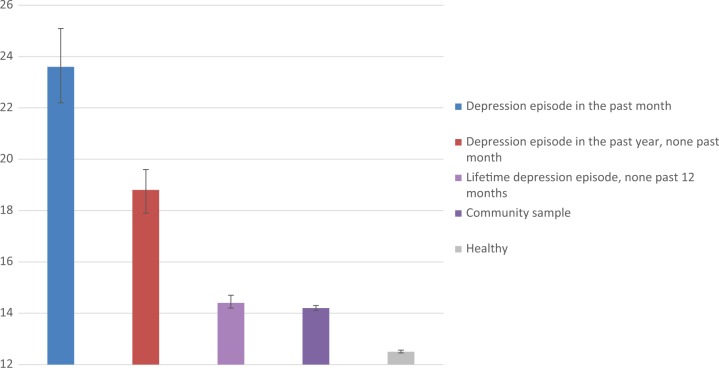
The disability endorsed by subjects who have or have experienced a MDE shows a strong trend towards decreased disability with time since last episode (Figure 3). Mean 12-item WHODAS 2.0 scores decrease from a peak of 23.6 (95% CI, 22.2 to 25.1) in those experiencing past-month MDE to 14.4 (95% CI, 14.2 to 14.7) in those with a lifetime episode. Whereas those with lifetime MDE have higher disability scores than healthy subjects, these are still very similar to those in the community population.
Figure 3.
In addition, the mean World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) score for all subjects with a past-year depression episode is 20.4 (95% CI, 19.6 to 21.1).
Discussion
Face Validity of Results
Our intent was to provide a context for 12-item WHODAS 2.0 results in the Canadian community population and in Canadians with mental disorders to enhance the interpretability of the WHODAS 2.0 for both clinicians and researchers. The uptake of the WHODAS 2.0 in clinical practice will likely determine whether it transitions from Section 3 to Section 2 of the manual. It is important to note that several key results regarding disability in mental disorders and its measurement on the WHODAS 2.0 are supported by previous literature. It has already been determined that those with mental disorders have much higher mean 12-item WHODAS 2.0 scores than the general population.14 Furthermore, the finding that subjects with schizophrenia endorsed the highest mean disability is consistent with the recent establishments of global disability weights for the Global Burden of Diseases Project, in which out of 220 possible negative health states, the highest disability weight was attributed to acute schizophrenia.15
An interesting finding is that the level of disability associated with GAD was very high. It is notable that in analyses excluding comorbidities, GAD has been found to produce equivalent levels of impairment as MDD.16–18 However, lifetime comorbid mental disorder in GAD has been reported as high as 90.4%.19 As this analysis seeks to provide information applicable to the community population, subjects with comorbid psychiatric diagnoses were not excluded. The high mean disability scores reported by subjects with GAD may thus be affected by the notably high prevalence of comorbid conditions in GAD patients.16,18,20,21 These high ratings may also reflect the philosophical approach of the WHODAS 2.0. Whereas previous concepts of disability tended to focus on impairments (such as impaired cognition), the WHODAS 2.0 incorporates concepts such as activities and participation in society, previous neglect of which may have underestimated the impact of GAD.
Regarding the severity by item profiles for MDD and other mental disorders, items with more severe endorsement included being emotionally affected, concentration difficulties, and difficulties with household responsibilities. In developing the WHODAS 2.0, it was also found that subjects with mental problems or addictions issues had higher scores in the domains of “cognitive activities” (includes concentration and learning items) and “getting along” (includes maintaining a friendship and dealing with people you do not know) than a comparison group with physical disorders.5 These findings, and those of the CCHS-MH, confirm that that pattern of item endorsement reflects the expected impact of mental disorders.
As these are cross-sectional population data, the endorsement of non–mental health–related items, such as difficulty standing and walking, is probably reflective of the general health status of people with MDD, which includes many comorbid chronic conditions. However, concerns have been raised with the face validity of the WHODAS 2.0 due to possible disproportionate endorsement of these mobility items in subjects with borderline personality disorder,22 leaving this an area for further investigation. Unfortunately, personality disorders were not assessed in the CCHS-MH.
In subjects with lifetime MDE but no episode in the past year, the finding that disability scores returned to the level of those in the general community is supported by a previous observation that endorsed impairment on the WHODAS items decreased with time since last MDE and that those who did not have a MDE in the past year did not have elevated scores on WHODAS items.23 This provides support for the idea that the WHODAS 2.0 may be useful in tracking the recovery of function in patients with mental disorders, a purpose for which the previous GAF scale was widely used.
Interpretation of the WHODAS 2.0
To facilitate the interpretation of respondents’ answers, the frames of reference of the WHODAS 2.0 require respondents to focus on “degree of difficulty due to health conditions in the past 30 days … as the respondent usually does the activity. Items not experienced in the past 30 days are not rated” (p. 38).3 However, this interpretation may lead to idiosyncrasies with scoring. For example, those with a disabling health condition who are able to perform work with considerable difficulty will answer “extreme” on the WHODAS 2.0, while those who are completely unable to work may have their answers coded into the survey as “not applicable.”9 One study chose to modify the WHODAS 2.0 by adding the option “you didn’t perform this task” and then providing follow-up questions to code subjects as having none or the highest level of difficulty.24 The WHODAS manual suggests that for those who answer “not applicable,” interviewers should probe to determine the reason for this response (e.g., “Can you tell me why this question does not apply to you?” (p. 69)).3 It would be beneficial to standardize this type of clarifying question in future WHODAS 2.0 survey applications. However, the practicality of interviewer exploration in real-world psychiatric practice is questionable. An advantage of the GAF over the WHODAS was that a clinician could conveniently record the GAF score based on the global assessment of information gathered during the interview and other sources. If use of the WHODAS involves modifications to clinical practice, its wider uptake may be hampered.
A major shift in thinking will be required if there is to be a switch from the GAF to the WHODAS 2.0 to measure functional impairment in those with mental disorders. The GAF confounds mental disorder symptoms with resulting disability, while excluding environmental context.1,2,9 In comparison, the WHODAS 2.0 separates diagnoses (mental, physical, or both) from disability, while specifically incorporating environmental context to evaluate disability in relation to the biopsychosocial model.2,5
WHODAS 2.0 in the Context of the DSM-5
In addition to the simple sum “total disability” score, the DSM-5 suggests that clinicians may divide scores by the number of items answered, generating an average general disability score that is comparable to the initial Likert scale of response options (1= none, 2 = mild, etc.).8 This technique is endorsed as “reliable, easy to use … clinically useful” (p. 746)8; however, our analysis draws the validity of this approach into question. The mean 12-item WHODAS 2.0 score for those with a depressive episode in the past month is 23.6 and is in the 94th population percentile; dividing this by 12 produces an average disability of ∼2, or “mild.” This seems inconsistent with mean score in this group identifying those in the top 6% of the population in terms of disability. As the 12-item WHODAS 2.0 explains 81% of the variance on the 36-item version, this undervaluing of disability scores would likely occur on the long version as well. It does not seem reasonable to characterize the dramatic impact of MDD as mild just because of the average item score.
While the 36-item WHODAS 2.0 was chosen for inclusion in the DSM-5, a major limitation of its utility is a current lack of normative data with the simple scoring procedure.2 The shorter, 12-item version may be more clinically useful at present. It requires 5 minutes rather than 20 to complete,5 and we now provide normative Canadian population values for its use with simple scoring as well as values for Canadian household residents with mental disorders. Valid measures of overall disability in those with mental disorders may also be used in prioritizing limited resources and in determining urgency of care,24 but the ability of the WHODAS 2.0 to fulfill this role in Canadian psychiatry remains undetermined.
Conclusions
This study assists with meaningful interpretation of the 12-item WHODAS 2.0 by providing normative data for the Canadian community population and for those with specific mental disorders. This analysis provides details on disability severity by area of function and over the time course of a disorder. This information is expected to have implications clinically and in further mental health research should the DSM-5 Section 3 recommendation for its use be implemented. Due to the significant comorbidity burden in the psychiatric population, further work will focus on clarifying the relationship between comorbid mental and physical disorders and disability, as well as characterizing those with mental disorders scoring in the upper limits of the spectrum of disability.
Clinical Implications
Compared with the general population, the WHODAS 2.0 scores of people with mental disorders are dramatically worse, indicating that the scale is sensitive to the impact of mental disorders.
Canadians with mental disorders are shown to endorse items on the WHODAS 2.0 in patterns consistent with their conditions, providing some evidence of construct validity.
The expected course of overall disability, progressing from acute mental disorder episodes to remission, appears to be reflected in WHODAS 2.0 ratings.
Limitations of the Study
The ability of this study to inform DSM-5 Section 3 recommendations is limited, as the 12-item, not 36-item, WHODAS 2.0 was used.
An analysis of WHODAS 2.0 scores incorporating comorbidities and sociodemographic stratification is needed since comorbidity is the norm in clinical settings.
The mental health diagnoses were derived using a fully structured diagnostic interview or for psychotic disorders by self-report, rather than by a semistructured interview conducted by a health professional.
Acknowledgement
This article was presented as a poster presentation at the Canadian Mental Health Association Nationwide Conference, Calgary, Alberta, Canada, October 24, 2014. The authors thank Dr. Charlie Victorino and Rebecca Williams at the Prairie Regional RDC for providing general support. Scott Patten is a Senior Health Scholar with Alberta Innovates–Health Solutions.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Kirsten Sjonnesen would like to acknowledge the financial support of Alberta Innovates–Health Solutions (summer studentship grant 201300818). The analysis was conducted at Prairie Regional RDC, which is part of the Canadian Research Data Centre Network (CRDCN). The services and activities provided by the CRDCN are made possible by the financial or in-kind support of the Social Sciences and Humanities Research Council of Canada, the Canadian Institutes of Health Research, the Canadian Foundation for Innovation, Statistics Canada, and participating universities whose support is gratefully acknowledged. The views expressed in this article do not necessarily represent the CRDCN’s or that of its partners.
References
- 1. Üstün TB, Kennedy C. What is “functional impairment”? Disentangling disability from clinical significance. World J Psychiatry. 2009;8(2):82–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gold LH. DSM-5 and the assessment of functioning: the World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0). J Am Acad Psychiatry Law. 2014;42(2):173–181. [PubMed] [Google Scholar]
- 3. Üstün TB, Kostanjsek N, Chatterji S, Rehm J, editors. Measuring health and disability: manual for WHO disability assessment schedule WHODAS 2.0. Malta: World Health Organization; 2010. [Google Scholar]
- 4. World Health Organization Media Centre. Fact sheet: Health and disability [Internet]. [cited 2014 August 18]. Available from: www.who.int/mediacentre/factsheets/fs352/en
- 5. Üstün TB, Chatterji S, Kostanjsek N, et al. Developing the World Health Organization Disability Assessment Schedule 2.0. Bull World Health Org. 2010;88(11):815–823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Luciano JV, Ayuso-Mateos JL, Fernandez A, et al. Psychometric properties of the twelve item World Health Organization Disability Assessment Schedule II (WHO-DAS II) in Spanish primary care patients with a first major depressive episode. J Affect Disord. 2010;121(1):52–58. [DOI] [PubMed] [Google Scholar]
- 7. Carlozzi NE, Kratz AL, Downing NR, et al. Validity of the 12-item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) in individuals with Huntington disease (HD). Qual Life Res. 2015;24(8):1963–1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA; ): American Psychiatric Publishing; 2013. [Google Scholar]
- 9. Konecky B, Meyer EC, Marx BP, et al. Using the WHODAS 2.0 to assess functional disability associated with DSM-5 mental disorders. Am J Psych. 2014;171(8):818–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Statistics Canada. Canadian Community Health Survey (CCHS)—mental health user guide: microdata files. Statistics Canada; 2013. [Google Scholar]
- 11. Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):83–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Statistics Canada. Canadian Community Health Survey (CCHS)—mental health questionnaire [specifications report]. Statistics Canada; 2011. [Google Scholar]
- 13. Stata [computer program]. Stata Statistical Software: Release 13. College Station (TX): StataCorp LP; 2013. [Google Scholar]
- 14. Andrews G, Kemp A, Sunderland M, et al. Normative data for the 12 item WHO Disability Assessment Schedule 2.0. PLoS One. 2009;4(12):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet. 2013;380(9859):2129–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychol Med. 2005;35(12):1747–1759. [DOI] [PubMed] [Google Scholar]
- 17. Hunt C, Slade T, Andrews G. Generalized anxiety disorder and major depressive disorder comorbidity in the National Survey of Mental Health and Well-Being. Depress Anxiety. 2004;20(1):23–31. [DOI] [PubMed] [Google Scholar]
- 18. Wittchen HU, Carter RM, Pfister H, et al. Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. Int Clin Psychopharmacol. 2000;15(6):319–328. [DOI] [PubMed] [Google Scholar]
- 19. Wittchen HU, Zhao S, Kessler RC, et al. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psych. 1994;51(5):355–364. [DOI] [PubMed] [Google Scholar]
- 20. Ballenger JC, Davidson JR, Lecrubier Y, et al. Consensus statement on generalized anxiety disorder from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry. 2001;62:53–58. [PubMed] [Google Scholar]
- 21. Bruce SE, Machan JT, Dyck I, et al. Infrequency of “pure” GAD: impact of psychiatric comorbidity on clinical course. Depress Anxiety. 2001;14(4):219–225. [DOI] [PubMed] [Google Scholar]
- 22. Ruocco AC, Lam J, McMain SF. Subjective cognitive complaints and functional disability in patients with borderline personality disorder and their nonaffected first-degree relatives. Can J Psychiatry. 2014;59(6):335–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–3105. [DOI] [PubMed] [Google Scholar]
- 24. Novak SP, Colpe LJ, Barker PR. Development of a brief mental health impairment scale using a nationally representative sample in the USA. Int J Methods Psychiatr Res. 2010;19(Suppl 1):49–60. [DOI] [PMC free article] [PubMed] [Google Scholar]