Abstract
Background
Enhanced HIV surveillance using demographic, behavioral, and biologic data from national surveys can provide information to evaluate and respond to HIV epidemics efficiently.
Methods
From October 2012 to February 2013, we conducted a 2-stage cluster sampling survey of persons aged 18 months to 64 years in 9 geographic regions in Kenya. Participants answered questionnaires and provided blood for HIV testing. We estimated HIV prevalence, HIV incidence, described trends in HIV prevalence over the past 5 years, and identified factors associated with HIV infection. This analysis was restricted to persons aged 15–64 years.
Results
HIV prevalence was 5.6% [95% confidence interval (CI): 4.9 to 6.3] in 2012, a significant decrease from 2007, when HIV prevalence, excluding the North Eastern region, was 7.2% (95% CI: 6.6 to 7.9). HIV incidence was 0.5% (95% CI: 0.2 to 0.9) in 2012. Among women, factors associated with undiagnosed HIV infection included being aged 35–39 years, divorced or separated, from urban residences and Nyanza region, self-perceiving a moderate risk of HIV infection, condom use with the last partner in the previous 12 months, and reporting 4 or more lifetime number of partners. Among men, widowhood, condom use with the last partner in the previous 12 months, and lack of circumcision were associated with undiagnosed HIV infection.
Conclusions
HIV prevalence has declined in Kenya since 2007. With improved access to treatment, HIV prevalence has become more challenging to interpret without data on new infections and mortality. Correlates of undiagnosed HIV infection provide important information on where to prioritize prevention interventions to reduce transmission of HIV in the broader population.
Keywords: HIV, prevalence, incidence, surveillance, Kenya
INTRODUCTION
HIV continues to be a major public health challenge in sub-Saharan Africa, where an estimated 22 million people are living with HIV.1 In a population of 40 million in Kenya, 1.6 million people of all ages were living with HIV in 2012 and an estimated 98,000 of these had acquired HIV infection within the preceding year, making Kenya’s HIV epidemic the fourth largest worldwide.1,2 For this reason, Kenya has been regarded globally as a priority country in sub-Saharan Africa to reverse the spread of HIV in the region.
To implement effective HIV programs, nationally representative data that reflect the country’s current HIV epidemiology are required. Since 2003, HIV testing has been included in national household surveys, including the Kenya Demographic and Health Surveys (2003 and 2008–09) and the Kenya AIDS Indicator Survey (KAIS) in 2007.3–5 These surveys estimated that HIV prevalence in adults ranged from 6.3% to 7.4%. Data from these surveys have provided a clearer understanding of the magnitude, distribution, and trends in HIV infection, as well as coverage of HIV treatment and prevention interventions to inform policies and programs to address the epidemic.6
We conducted a second Kenya AIDS Indicator Survey (KAIS 2012) to estimate HIV incidence and prevalence, assess trends in HIV prevalence since 2007, and identify factors associated with HIV infection to inform programmatic and policy decisions to guide the national HIV response for the next five years in Kenya.
METHODS
KAIS 2012 was a cross-sectional household survey of persons aged 18 months to 64 years, conducted from October 2012 to February 2013. The methods of this survey are described in detail elsewhere.7 The survey was designed to provide representative estimates of HIV prevalence among adults and adolescents aged 15 to 64 years at the national and regional level for the urban and rural populace. Among children aged 18 months to 14 years, the survey was powered to provide estimates of HIV prevalence at the national level only. Because of regional insecurity at the time of the survey, the North Eastern region was not sampled. For the purposes of this article, we restricted our analyses to adults and adolescents aged 15 to 64 years.
Data Collection Procedures
Interviewers conducted face-to-face interviews with eligible participants. Interviews collected information on individual demographic and behavioral characteristics. Interview data were entered directly into tablet computers (Mirus Innovations, Mississauga, Ontario, Canada). Participants provided venous blood for HIV testing, which was performed at a central laboratory in Nairobi. If venous blood could not be collected, a finger prick was used to collect a dried capillary blood spot sample for HIV testing. Participants were informed that they would not receive the results of their laboratory tests but were offered home-based HIV testing and counseling services using the national HIV testing algorithm8 if they wished to learn their HIV status in the privacy of their homes.
Laboratory Methods
At the central laboratory, the same validated HIV testing algorithm that was used in KAIS 2007 was applied to KAIS 2012 blood samples. All specimens were initially screened with Vironostika HIV-1/2 UNIF II Plus O Enzyme Linked Immunoassay (bioMérieux, Marcy l’Etoile, France). Specimens that were reactive were then tested with the Murex HIV.1.2.O HIV Enzyme Immunoassay (DiaSorin, SpA, Saluggia, Italy) to confirm reactivity. Specimens with discrepant results were retested using the same algorithm. Twice discrepant results were resolved using polymerase chain reaction (Cobas Amplicor HIV-1 Monitor Test, version 1.5, Roche Molecular Diagnostics, Pleasanton, CA). HIV-positive dried blood spot specimens were tested for HIV RNA concentration using the Abbott M2000 Real-Time HIV-1 Assay (Abbott Laboratories, Abbott Park, IL) and recent HIV infection using the Limiting Antigen Avidity Enzyme Immunoassay (LAg-Avidity EIA) (Maxim Biomedical, Inc., Rockville, MD). Specimens with a normalized optical density value of 1.5 or lower on the LAg-Avidity EIA and (1) not virally suppressed (defined as HIV RNA concentration <1000 copies/mL) or (2) did not report use of antiretroviral therapy (ART) for their HIV infection were classified as indicative of recent infection. The estimated mean duration of recent infection for the assay was 130 days (95% confidence interval [CI] 118 to 142).
Data Management
We merged interview and laboratory data to produce a final survey data set for analysis. Survey data were weighted to correct for unequal probability of selection and adjusted for interview and blood nonresponse to produce estimates that were representative of the population from which the KAIS 2012 sample was drawn. All data were analyzed using SAS version 9.3 (SAS Institute, Cary, NC).
Data Analysis
We conducted univariate analyses and present frequencies and weighted proportions with 95% CI. Statistical significance for cross-tabulations was assessed using the Rao–Scott χ2 test. We assessed whether there were changes in HIV prevalence between KAIS 2007 and KAIS 2012 by age, sex, residence, and geographic region. A z-test was used to test for differences in proportions between the 2 surveys, and we considered a P value < 0.05 to be statistically significant.
Using the PROC SURVEYLOGISTIC procedure, we conducted bivariate and multivariate analyses to identify correlates of undiagnosed HIV infection among persons who had ever had sex and report results as odds ratios (OR), adjusted odds ratios (AOR), and 95% CI. We selected undiagnosed HIV infection as our main outcome of interest to identify subpopulations that were at the highest risk of acquiring and transmitting HIV infection. Predictor variables included the following: age, education, marital status, region, residence, household wealth, risk perception, condom use, number of sexual partners, lifetime history of high-risk behavior, including injecting drugs, anal sex, and transactional sex, symptoms of sexually transmitted infection (STI), self-reported circumcision among men, and circumcision status of male partners reported by women. Variables associated with undiagnosed HIV infection at P value <0.2 in bivariate analyses were tested in a multivariate model to identify factors that were independently associated with undiagnosed HIV infection. Variables that remained significantly associated with HIV infection at P value <0.05 were retained in the final model.
To estimate the number of adults and adolescents aged 15–64 years living with HIV and number with recently acquired HIV infection, we applied non-normalized survey weights to our HIV outcome variable. Non-normalized weights were based on the 2012 projected population data derived from the 2009 Kenya Population and Housing Census.2 Annualized HIV incidence was calculated using the World Health Organization’s recommended formula for estimating assay-based HIV incidence.9 The annual HIV transmission rate per 100 persons living with HIV was calculated by dividing the estimated HIV incidence by the estimated HIV prevalence and multiplying this value by 100.10
This study was approved by the Kenya Medical Research Institute Ethical Review Committee, the Institutional Review Board of the US Centers for Disease Control and Prevention, and the Committee on Human Research of the University of California, San Francisco.
RESULTS
Eligibility and Characteristics of Study Population
Of the 16,383 persons eligible for the survey, 13,720 (83.7%) consented to an interview. Among the 13,720 individuals in the interview sample, 11,626 (84.7%) provided a blood sample, representing the serologic sample from which HIV prevalence was estimated. Compared with individuals in the interview sample, significantly higher proportions of individuals in the serologic sample were from rural residences (64.1% compared with 56.4%, P = 0.003), from North Rift region (14.2% compared with 1.0%, P < 0.001), had ever been widowed (6.1% compared with 5.5%, P = 0.002), and were women who had been pregnant in the past (78.8% compared with 73.5%, P < 0.001), respectively (Table 1). In addition, compared with persons in the interview sample, significantly higher proportions of persons in the serologic sample reported being sexually active in the past 12 months (72.3% compared with 68.1%, P = 0.003), perceived that their risk of HIV infection was great (5.0% compared with 3.3%, P = 0.005), had received their last HIV test more than 12 months preceding the survey (45.1% compared with 38.1%, P < 0.001), and self-reported HIV-positive status based on their HIV testing history (4.1% compared with 2.1%, P < 0.001), respectively.
TABLE 1.
Select Demographic, Behavioral, and Biologic Characteristics of Persons Aged 15–64 Years by Sample Type Kenya AIDS Indicator Survey 2012
| Interview Sample: Interviewed and Did Not Provide a Blood Sample (N = 2094)
|
Serologic Sample: Interviewed and Provided a Blood Sample (N = 11,626)
|
P* | |||
|---|---|---|---|---|---|
| Total
|
Total
|
||||
| Unweighted, N† | Weighted % (95% CI) | Unweighted, N† | Weighted % (95% CI) | ||
| Sociodemographic characteristics | |||||
| Sex | 0.208 | ||||
| Men | 930 | 50.3 (48.0 to 52.6) | 4836 | 48.7 (47.6 to 49.8) | |
| Women | 1164 | 49.7 (47.4 to 52.0) | 6790 | 51.3 (50.2 to 52.4) | |
| Age group, yrs | 0.007 | ||||
| 15–19 | 381 | 18.3 (16.1 to 20.5) | 1912 | 16.5 (15.5 to 17.5) | |
| 20–24 | 342 | 15.9 (14.3 to 17.6) | 1907 | 16.3 (15.4 to 17.3) | |
| 25–29 | 355 | 17.8 (15.9 to 19.7) | 1786 | 15.2 (14.3 to 16.1) | |
| 30–34 | 273 | 13.5 (11.8 to 15.2) | 1424 | 12.1 (11.4 to 12.9) | |
| 35–39 | 194 | 9.2 (7.8 to 10.7) | 1222 | 10.6 (10.0 to 11.3) | |
| 40–44 | 177 | 8.1 (6.7 to 9.5) | 985 | 8.6 (8.0 to 9.2) | |
| 45–49 | 134 | 6.1 (4.8 to 7.4) | 715 | 6.3 (5.8 to 6.8) | |
| 50–54 | 110 | 5.1 (4.0 to 6.3) | 735 | 6.3 (5.8 to 6.8) | |
| 55–59 | 74 | 3.4 (2.4 to 4.3) | 523 | 4.5 (4.0 to 5.0) | |
| 60–64 | 54 | 2.6 (1.8 to 3.5) | 417 | 3.6 (3.1 to 4.0) | |
| Highest educational attainment | 0.101 | ||||
| No primary education | 240 | 8.6 (6.5 to 10.8) | 1338 | 7.0 (5.8 to 8.3) | |
| Incomplete primary education | 172 | 7.1 (5.6 to 8.6) | 988 | 7.6 (6.7 to 8.6) | |
| Completed primary education | 622 | 30.4 (27.6 to 33.2) | 3694 | 32.6 (31.2 to 34.1) | |
| Completed secondary education or higher | 1060 | 53.9 (50.6 to 57.2) | 5606 | 52.7 (50.9 to 54.4) | |
| Region | <0.001 | ||||
| Nairobi | 431 | 17.5 (14.6 to 20.4) | 1314 | 9.8 (8.7 to 10.9) | |
| Central | 157 | 9.3 (5.9 to 12.6) | 1423 | 13.9 (12.2 to 15.6) | |
| Coast | 203 | 10.2 (7.4 to 13.1) | 1462 | 9.1 (7.7 to 10.5) | |
| Eastern North | 224 | 14.3 (11.0 to 17.6) | 1061 | 1.1 (0.9 to 1.4) | |
| Eastern South | 193 | 12.3 (8.8 to 15.8) | 1260 | 14.3 (12.6 to 16.0) | |
| North Rift | 159 | 1.0 (0.7 to 1.3) | 1031 | 14.2 (11.4 to 17.0) | |
| Nyanza | 204 | 14.3 (10.5 to 18.1) | 1631 | 14.7 (12.8 to 16.7) | |
| South Rift | 273 | 11.1 (8.6 to 13.6) | 1036 | 12.0 (9.9 to 14.0) | |
| Western | 250 | 10.1 (6.4 to 13.8) | 1408 | 10.8 (9.2 to 12.4) | |
| Residence | 0.003 | ||||
| Rural | 1137 | 56.4 (51.7 to 61.1) | 7501 | 64.1 (61.5 to 66.7) | |
| Urban | 957 | 43.6 (38.9 to 48.3) | 4125 | 35.9 (33.3 to 38.5) | |
| Wealth index | |||||
| Poorest | 416 | 18.2 (14.8 to 21.7) | 2434 | 19.4 (16.7 to 22.1) | |
| Second | 360 | 17.2 (14.7 to 19.8) | 2497 | 21.5 (19.5 to 23.4) | |
| Third | 357 | 18.4 (15.3 to 21.5) | 2318 | 20.1 (18.2 to 22.0) | |
| Fourth | 403 | 19.4 (16.2 to 22.7) | 2177 | 19.3 (17.1 to 21.4) | |
| Richest | 558 | 26.7 (22.2 to 31.1) | 2200 | 19.8 (17.1 to 22.5) | |
| Marital status | 0.002 | ||||
| Never married/never cohabited | 699 | 33.8 (31.2 to 36.5) | 3291 | 29.4 (28.1 to 30.8) | |
| Ever widowed | 137 | 5.3 (4.3 to 6.3) | 894 | 7.0 (6.4 to 7.6) | |
| Separated or divorced | 110 | 5.5 (4.3 to 6.7) | 739 | 6.1 (5.5 to 6.7) | |
| Currently married or cohabiting—polygamous | 113 | 5.0 (3.7 to 6.3) | 753 | 5.8 (5.0 to 6.5) | |
| Currently married or cohabiting—monogamous | 1029 | 50.3 (47.6 to 53.1) | 5945 | 51.7 (50.3 to 53.1) | |
| Behavioral indicators | |||||
| Ever had sexual intercourse | 0.029 | ||||
| No | 320 | 14.8 (12.8 to 16.8) | 1507 | 12.6 (11.7 to 13.6) | |
| Yes | 1766 | 85.2 (83.2 to 87.2) | 10,097 | 87.4 (86.4 to 88.3) | |
| Lifetime number of partners | <0.001 | ||||
| 1 | 611 | 31.9 (29.3 to 34.5) | 3263 | 28.9 (27.5 to 30.3) | |
| 2–3 | 597 | 33.6 (31.1 to 36.1) | 3575 | 35.3 (34.1 to 36.6) | |
| 4+ | 389 | 24.4 (21.9 to 26.9) | 2550 | 29.2 (27.8 to 30.6) | |
| Do not know | 159 | 10.1 (8.0 to 12.2) | 620 | 6.6 (5.6 to 7.5) | |
| Sexually active in the past 12 mo | 0.003 | ||||
| No | 687 | 31.9 (29.2 to 34.6) | 3420 | 27.7 (26.4 to 29.0) | |
| Yes | 1407 | 68.1 (65.4 to 70.8) | 8206 | 72.3 (71.0 to 73.6) | |
| No. partners in the past 12 mo | 0.657 | ||||
| 1 | 1241 | 89.0 (86.9 to 91.1) | 7290 | 88.5 (87.6 to 89.4) | |
| 2+ | 138 | 11.0 (8.9 to 13.1) | 830 | 11.5 (10.6 to 12.4) | |
| Used a condom with last partner in the past 12 mo‡ | 0.297 | ||||
| No | 1146 | 82.3 (79.7 to 84.9) | 6886 | 83.7 (82.6 to 84.8) | |
| Yes | 240 | 17.7 (15.1 to 20.3) | 1256 | 16.3 (15.2 to 17.4) | |
| HIV risk perception | 0.005 | ||||
| No risk | 866 | 46.4 (43.5 to 49.3) | 4213 | 42.1 (40.1 to 44.0) | |
| Low risk | 711 | 40.5 (37.3 to 43.8) | 4240 | 43.0 (40.9 to 45.1) | |
| Moderate risk | 169 | 9.8 (8.2 to 11.4) | 1023 | 10.0 (9.1 to 10.8) | |
| Great risk | 57 | 3.3 (2.3 to 4.2) | 457 | 5.0 (4.4 to 5.5) | |
| Most-at-risk behaviors | |||||
| Ever injected drugs for pleasure | 0.204 | ||||
| No | 2089 | 99.7 (99.4 to 100) | 11,595 | 99.9 (99.9 to 100) | |
| Yes | 5 | 0.3 (0.0 to 0.6) | 9 | 0.1 (0.0 to 0.1) | |
| Ever had anal sex | 0.262 | ||||
| No | 1744 | 98.6 (97.9 to 99.2) | 9897 | 98.1 (97.7 to 98.5) | |
| Yes | 22 | 1.4 (0.8 to 2.1) | 189 | 1.9 (1.5 to 2.3) | |
| Ever received money, gifts, or goods in exchange for sex | 0.945 | ||||
| No | 1699 | 96.2 (95.2 to 97.2) | 9613 | 96.2 (95.7 to 96.7) | |
| Yes | 67 | 3.8 (2.8 to 4.8) | 381 | 3.8 (3.3 to 4.3) | |
| Ever gave money, gifts, or goods in exchange for sex (men only) | 0.448 | ||||
| No | 664 | 83.8 (80.3 to 87.2) | 3385 | 82.2 (80.2 to 84.3) | |
| Yes | 121 | 16.2 (12.8 to 19.7) | 684 | 17.8 (15.7 to 19.8) | |
| Biologic indicators | |||||
| Reported STI symptoms in the past 12 mo | 0.001 | ||||
| No | 1703 | 96.4 (95.4 to 97.4) | 9484 | 94.2 (93.6 to 94.8) | |
| Yes | 63 | 3.6 (2.6 to 4.6) | 613 | 5.8 (5.2 to 6.4) | |
| Ever been tested for HIV | 0.895 | ||||
| No | 587 | 28.5 (26.2 to 30.8) | 3121 | 28.3 (26.7 to 30.0) | |
| Yes | 1484 | 71.5 (69.2 to 73.8) | 8463 | 71.7 (70.0 to 73.3) | |
| Been tested for HIV in the past 12 mo§ | <0.001 | ||||
| No | 562 | 38.1 (35.0 to 41.2) | 3778 | 45.1 (43.5 to 46.6) | |
| Yes | 905 | 61.9 (58.8 to 65.0) | 4625 | 54.9 (53.4 to 56.5) | |
| Self-reported HIV status§ | <0.001 | ||||
| HIV-positive | 29 | 2.1 (1.3 to 2.9) | 328 | 4.1 (3.4 to 4.8) | |
| HIV-negative | 1383 | 97.9 (97.1 to 98.7) | 7916 | 95.9 (95.2 to 96.6) | |
| Ever pregnant (women only) | <0.001 | ||||
| No | 299 | 26.5 (23.2 to 29.9) | 1338 | 21.2 (19.7 to 22.6) | |
| Yes | 799 | 73.5 (70.1 to 76.8) | 4939 | 78.8 (77.4 to 80.3) | |
| Currently pregnant (women only) | 0.685 | ||||
| No | 962 | 93.4 (91.7 to 95.1) | 5501 | 93.8 (93.0 to 94.6) | |
| Yes | 74 | 6.6 (4.9 to 8.3) | 365 | 6.2 (5.4 to 7.0) | |
| Circumcised (men only) | 0.687 | ||||
| No | 96 | 9.6 (7.1 to 12.1) | 441 | 9.1 (7.5 to 10.7) | |
| Yes | 834 | 90.4 (87.9 to 92.9) | 4395 | 90.9 (89.3 to 92.5) | |
| Male partner circumcised (women only) | 0.027 | ||||
| No | 406 | 34.0 (30.4 to 37.6) | 2008 | 29.9 (27.8 to 32.1) | |
| Yes | 758 | 66.0 (62.4 to 69.6) | 4782 | 70.1 (67.9 to 72.2) | |
P value based on Rao–Scott χ2 test. Statistically significant differences between are represented by P < 0.05.
Because of missing responses, totals vary between variables.
Among persons who reported being sexually active in the past 12 months.
Among persons who had ever been tested for HIV.
NA, not applicable.
Among the 11,626 participants in the serologic sample, 51.3% were women. The median age was 33 years (interquartile range, 25–43). Over half (52.7%) had completed secondary school education or higher. The majority (64.1%) resided in rural areas; 14.7% were from Nyanza, 14.3% from Eastern South, 14.2% from North Rift, 9.8% from Nairobi, and 1.1% from Eastern North regions. Over half (57.5%) were currently in married or cohabiting relationships.
Most (87.4%) reported having ever had sexual intercourse, and 72.3% reported sexual intercourse in the past 12 months. Among these, 11.5% reported 2 or more partners in the past 12 months. Eighty-five percent of participants reported no to low self-perceived risk of HIV infection. Anal sex was reported by 1.9%. Receiving money, gifts, and favors in exchange for sex was reported by 3.8%. In total, 17.8% of men reported ever giving money, gifts, or favors in exchange for sex. Symptoms of STI in the past 12 months, including genital sores and/or vaginal (women only), penile (men only), or anal discharge were reported by 5.8% (2.7% of men and 8.7% of women). Among women, 78.8% had ever been pregnant, and 6.2% were currently pregnant at the time of the survey. Ninety-one percent of men were circumcised, and 70.1% of women reported that their current male partner was circumcised.
HIV Prevalence and Incidence
HIV prevalence was 5.6% (95% CI: 4.9 to 6.3), and HIV incidence was 0.5% (95% CI: 0.2 to 0.9), corresponding to an annual HIV transmission rate of 8.9 per 100 HIV-infected persons. Regional differences in HIV prevalence were observed with the highest HIV prevalence noted in Nyanza region (15.1%, 95% CI: 11.4 to 18.8) and lowest in Eastern North region (2.1%, 95% CI: 1.0 to 3.2) (Table 2). Women had significantly higher HIV prevalence than men (6.9% vs. 4.4%; P < 0.0001). HIV prevalence increased with age, peaking at age 35–39 years among women (12.3%, 95% CI: 9.4 to 15.2) and age 45–54 years among men (7.2%, 95% CI: 4.9 to 9.6) (data not shown). HIV prevalence was highest among persons who had been widowed (20.0%, 95% CI: 16.2 to 23.7), separated or divorced (10.9%, 95% CI: 8.4 to 13.4), or were married or cohabiting in a polygamous relationship (9.7%, 95% CI: 6.4 to 13.1).
TABLE 2.
Weighted HIV Prevalence by Demographic, Behavioral, and Biological Indicators, Persons Aged 15–64 Years, Kenya AIDS Indicator Survey 2012
| Select Characteristics | Unweighted, N | HIV-positive (Unweighted, n*) | Weighted HIV Prevalence % (95% CI) |
|---|---|---|---|
| Total | 11,626 | 648 | 5.6 (4.9 to 6.3) |
| Sex | |||
| Men | 4836 | 193 | 4.4 (3.6 to 5.2) |
| Women | 6790 | 455 | 6.9 (6.0 to 7.7) |
| Age group, yrs | |||
| 15–19 | 1912 | 17 | 1.0 (0.5 to 1.6) |
| 20–24 | 1907 | 58 | 3.1 (2.2 to 4.0) |
| 25–29 | 1786 | 112 | 6.3 (4.8 to 7.7) |
| 30–34 | 1424 | 97 | 6.6 (5.2 to 8.0) |
| 35–39 | 1222 | 108 | 8.7 (6.7 to 10.7) |
| 40–44 | 985 | 90 | 9.3 (7.1 to 11.6) |
| 45–49 | 715 | 66 | 9.8 (7.1 to 12.5) |
| 50–54 | 735 | 60 | 8.4 (6.3 to 10.5) |
| 55–59 | 523 | 24 | 4.4 (2.4 to 6.4) |
| 60–64 | 417 | 16 | 4.0 (2.0 to 6.1) |
| Highest educational attainment | |||
| No primary education | 1338 | 44 | 3.6 (2.4 to 4.8) |
| Incomplete primary education | 988 | 46 | 5.0 (3.2 to 6.7) |
| Completed primary education | 3694 | 223 | 6.0 (4.9 to 7.0) |
| Completed secondary education or higher | 5606 | 335 | 5.8 (4.9 to 6.7) |
| Region | |||
| Nairobi | 1314 | 67 | 4.9 (3.7 to 6.1) |
| Central | 1423 | 60 | 3.8 (2.7 to 4.9) |
| Coast | 1462 | 66 | 4.3 (3.0 to 5.6) |
| Eastern North | 1061 | 29 | 2.1 (1.0 to 3.2) |
| Eastern South | 1260 | 46 | 3.9 (2.4 to 5.3) |
| Nyanza | 1631 | 242 | 15.1 (11.4 to 18.8) |
| North Rift | 1036 | 37 | 3.1 (2.0 to 4.2) |
| South Rift | 1031 | 42 | 4.3 (2.7 to 5.8) |
| Western | 1408 | 59 | 4.7 (3.0 to 6.5) |
| Residence | |||
| Rural | 7501 | 373 | 5.1 (4.3 to 5.9) |
| Urban | 4125 | 275 | 6.5 (5.4 to 7.7) |
| Wealth index | |||
| Poorest | 2434 | 97 | 4.2 (2.9 to 5.4) |
| Second | 2497 | 153 | 6.5 (4.9 to 8.1) |
| Third | 2318 | 137 | 6.0 (4.6 to 7.4) |
| Fourth | 2177 | 159 | 6.8 (5.3 to 8.3) |
| Richest | 2200 | 102 | 4.6 (3.7 to 5.6) |
| Marital status | |||
| Never married/never cohabited | 3291 | 58 | 1.8 (1.3 to 2.3) |
| Ever widowed | 894 | 165 | 20.0 (16.2 to 23.7) |
| Separated or divorced | 739 | 83 | 10.9 (8.4 to 13.4) |
| Currently married or cohabiting—polygamous | 753 | 68 | 9.7 (6.4 to 13.1) |
| Currently married or cohabiting—monogamous | 5945 | 274 | 4.8 (4.0 to 5.7) |
| Behavioral indicators | |||
| Ever had sexual intercourse | |||
| No | 1507 | 10 | 0.9 (0.3 to 1.6) |
| Yes | 10,097 | 636 | 6.3 (5.5 to 7.1) |
| Lifetime number of partners | |||
| 1 | 3263 | 128 | 3.8 (3.0 to 4.6) |
| 2–3 | 3575 | 236 | 6.1 (5.1 to 7.1) |
| 4+ | 2550 | 208 | 8.2 (6.8 to 9.6) |
| Do not know | 620 | 62 | 10.6 (7.6 to 13.7) |
| Sexually active in the past 12 mo | |||
| No | 3420 | 175 | 5.2 (4.3 to 6.0) |
| Yes | 8206 | 473 | 5.8 (5.0 to 6.7) |
| No. partners in the past 12 mo† | |||
| 1 | 7290 | 403 | 5.6 (4.7 to 6.5) |
| 2+ | 830 | 65 | 7.4 (5.3 to 9.4) |
| Used a condom with last partner in the past 12 mo† | |||
| No | 6886 | 291 | 4.2 (3.5 to 4.9) |
| Yes | 1256 | 179 | 14.0 (11.1 to 17.0) |
| HIV risk perception | |||
| No risk | 4213 | 89 | 2.1 (1.6 to 2.7) |
| Low risk | 4240 | 151 | 3.5 (2.8 to 4.2) |
| Moderate risk | 1023 | 59 | 5.4 (3.9 to 6.9) |
| Great risk | 457 | 41 | 9.2 (6.2 to 12.2) |
| Most-at-risk behaviors | |||
| Ever injected drugs for pleasure | |||
| No | 11,617 | 647 | 5.6 (4.9 to 6.3) |
| Yes | 9 | 1 | ‡ |
| Ever had anal sex | |||
| No | 9908 | 621 | 6.3 (5.5 to 7.0) |
| Yes | 189 | 15 | 8.9 (4.6 to 13.1) |
| Ever received money, gifts, or goods in exchange for sex | |||
| No | 9716 | 600 | 6.2 (5.4 to 7.0) |
| Yes | 381 | 36 | 9.5 (6.1 to 12.8) |
| Ever gave money, gifts, or goods in exchange for sex (men only) | |||
| No | 3415 | 141 | 4.5 (3.5 to 5.5) |
| Yes | 684 | 48 | 6.9 (4.7 to 9.1) |
| Biologic indicators | |||
| Reported STI symptoms in the past 12 mo | |||
| No | 9484 | 562 | 5.9 (5.2 to 6.7) |
| Yes | 613 | 74 | 12.5 (9.0 to 16.0) |
| Ever been tested for HIV | |||
| No | 3121 | 72 | 2.5 (1.9 to 3.2) |
| Yes | 8463 | 574 | 6.9 (6.0 to 7.7) |
| Circumcised (men only) | |||
| No | 441 | 70 | 16.5 (12.7 to 20.2) |
| Yes | 4395 | 123 | 3.1 (2.5 to 3.8) |
| Male partner circumcised (women only) | |||
| No | 2008 | 210 | 10.9 (9.1 to 12.7) |
| Yes | 4782 | 245 | 5.2 (4.4 to 6.0) |
Because of missing responses, totals may vary between variables.
Among persons who reported being sexually active in the past 12 months.
Estimate suppressed due to small sample size (N<25 observations).
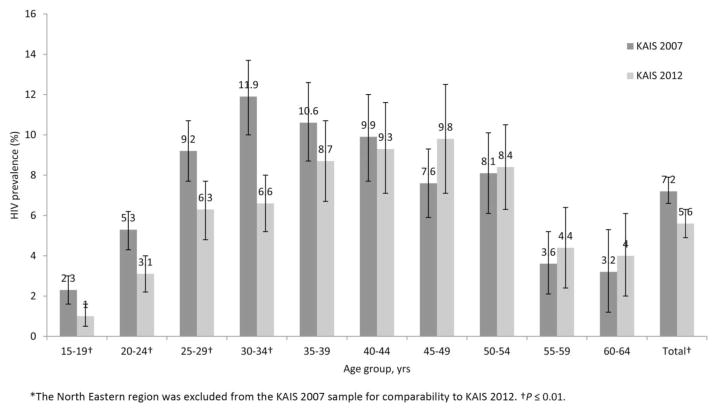
Trends in HIV Prevalence, 2007–2012
HIV prevalence declined significantly from 7.2% (excluding North Eastern region) in 2007 to 5.6% in 2012 (P = 0.002; Fig. 1). Significant declines were observed for both men (5.5% in 2007 to 4.4% in 2012; P = 0.0310) and women (8.5% in 2007; 6.9% in 2012; P = 0.006) (data not shown). We observed differential changes in HIV prevalence across age groups. In 2007, HIV prevalence peaked among persons aged 30–34 years (11.9%; 95% CI: 10.0 to 13.5), while in 2012, HIV prevalence peaked among persons aged 45–49 years (9.8%, 95% CI: 7.1 to 12.5). HIV prevalence declined significantly for persons who were aged 15–34 years in 2007 and 2012 (P ≤ 0.010) but remained unchanged among persons aged 35 years and older in the same time period.
FIGURE 1.
Trends in HIV prevalence among persons aged 15–64 years by age group, KAIS 2007* and KAIS 2012.
In Table 3, we describe trends in HIV prevalence between 2007 and 2012 for select age groups by sex, geographic location, and residence. Among persons aged 15–24 years, we observed significant declines in HIV prevalence for women (5.6% in 2007 to 3.0% in 2012; P < 0.001) but not for men (1.0% in 2007 to 1.1% in 2012; P = 0.864). For women aged 15–24 years, significant declines in HIV prevalence were observed among those residing in Nairobi (5.8% in 2007 to 1.8% in 2012; P = 0.038), Coast (5.7% in 2007 to 2.0% in 2012; P = 0.026), and Eastern (4.3%, in 2007 to 0.6% in 2012; P = 0.001) regions and those residing in rural areas (5.7% in 2007 to 2.8% in 2012; P < 0.001). Among men aged 15–24 years, significant declines in HIV prevalence were observed among those residing in Coast region (4.5% to 0.5%; P = 0.041) and rural areas (1.4% to 0.4%; P = 0.012).
TABLE 3.
Trends in HIV Prevalence by Region, Residence, and Age Group, KAIS 2007 and KAIS 2012
| Persons Aged 15–24 Years
|
Persons Aged 25–34 Years
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Men
|
Women
|
Men
|
Women
|
|||||
| KAIS 2007* % (95% CI) |
KAIS 2012 % (95% CI) |
KAIS 2007* % (95% CI) |
KAIS 2012 % (95% CI) |
KAIS 2007* % (95% CI) |
KAIS 2012 % (95% CI) |
KAIS 2007* % (95% CI) |
KAIS 2012 % (95% CI) |
|
| Total | 1.0 (0.9 to 1.9) | 1.1 (0.5 to 1.8) | 5.6 (4.6 to 6.6) | 3.0 (2.2 to 3.8)† | 8.1 (6.5 to 9.7) | 5.4 (3.9 to 6.8)‡ | 12.0 (10.3 to 13.7) | 7.3 (6.0 to 8.7)† |
| Region* | ||||||||
| Nairobi | 0.5 (0 to 1.4) | 2.2 (0 to 4.6) | 5.8 (2.2 to 9.3) | 1.8 (0.4 to 3.2)‡ | 7.0 (2.7 to 11.3) | 2.8 (0.6 to 5.1) | 14.0 (10.3 to 17.7) | 6.6 (3.8 to 9.5)‡ |
| Central | 0.9 (0 to 2.0) | 0.9 (0 to 2.7) | 1.7 (0.5 to 2.9) | 1.0 (0 to 2.5) | 4.5 (0.3 to 8.7) | 2.0 (0 to 4.3) | 7.7 (3.5 to 11.9) | 4.5 (2.2 to 6.9) |
| Coast | 4.5 (0.9 to 8.2) | 0.5 (0 to 1.5)‡ | 5.7 (3.2 to 8.2) | 2.0 (0 to 4.1)‡ | 7.1 (3.2 to 11.1) | 0.6 (0 to 1.9)‡ | 11.6 (6.9 to 16.4) | 4.1 (1.9 to 6.3)‡ |
| Eastern | 0.6 (0 to 1.4) | 1.1 (0 to 3.2) | 4.3 (2.2 to 6.3) | 0.6 (0 to 1.6)† | 3.0 (0 to 6.2) | 2.1 (0 to 4.7) | 8.9 (5.4 to 12.5) | 5.5 (3.0 to 7.9) |
| Nyanza | 1.6 (0.4 to 2.8) | 2.0 (0.2 to 3.8) | 13.2 (9.6 to 16.9) | 10.0 (6.3 to 13.6) | 21.1 (14.9 to 27.3) | 22.4 (13.8 to 31.0) | 24.5 (19.7 to 29.3) | 22.9 (15.1 to 30.7) |
| Rift Valley | 1.1 (0 to 2.3) | 0.6 (0 to 1.7) | 2.9 (1.3 to 4.6) | 2.1 (0.7 to 3.4) | 8.6 (5.5 to 11.7) | 4.9 (2.1 to 7.7) | 11.2 (6.9 to 15.5) | 4.0 (2.0 to 6.1)‡ |
| Western | 2.8 (0.9 to 4.7) | 0.9 (0 to 2.3) | 4.3 (2.0 to 6.5) | 2.2 (0.3 to 4.2) | 7.8 (2.3 to 13.2) | 4.9 (0.6 to 9.2) | 6.9 (3.5 to 10.2) | 6.0 (2.8 to 9.1) |
| Residence | ||||||||
| Rural | 1.4 (0.8 to 2.0) | 0.4 (0 to 0.9)‡ | 5.7 (4.5 to 6.9) | 2.8 (1.7 to 3.8)† | 8.0 (6.2 to 9.8) | 4.9 (2.7 to 7.1)‡ | 11.4 (9.6 to 13.2) | 6.3 (4.7 to 8.0)† |
| Urban | 1.3 (0.3 to 2.3) | 2.3 (0.8 to 3.9) | 5.4 (3.3 to 7.4) | 3.3 (2.0 to 4.6) | 8.5 (5.3 to 11.7) | 5.8 (3.9 to 7.7) | 13.5 (9.7 to 17.3) | 8.7 (6.4 to 11.1)‡ |
| Persons Aged 35+ Years
|
||||
|---|---|---|---|---|
| Men
|
Women
|
|||
| KAIS 2007* % (95% CI) |
KAIS 2012 % (95% CI) |
KAIS 2007* % (95% CI) |
KAIS 2012 % (95% CI) |
|
| Total | 7.3 (6.2 to 8.4) | 6.4 (5.1 to 7.6) | 8.6 (7.3 to 9.8) | 9.3 (8.3 to 11.3) |
| Region* | ||||
| Nairobi | 12.6 (5.9 to 19.2) | 6.2 (3.2 to 9.2) | 13.8 (6.7 to 20.9) | 11.6 (7.0 to 16.2) |
| Central | 4.4 (2.0 to 6.8) | 2.5 (0.5 to 4.5) | 3.1 (1.8 to 4.4) | 8.4 (5.5 to 11.4)‡ |
| Coast | 6.7 (4.1 to 9.2) | 5.6 (2.5 to 8.7) | 10.6 (7.8 to 13.4) | 11.6 (7.1 to 16.2) |
| Eastern | 3.8 (2.0 to 5.7) | 3.0 (1.0 to 5.0) | 5.9 (2.7 to 9.0) | 8.6 (4.6 to 12.5) |
| Nyanza | 19.0 (14.2 to 23.9) | 19.3 (12.9 to 25.8) | 16.9 (13.7 to 20.1) | 17.0 (11.4 to 22.7) |
| Rift Valley | 5.2 (3.4 to 7.1) | 4.5 (2.2 to 6.9) | 8.0 (4.9 to 11.0) | 6.6 (3.8 to 9.4) |
| Western | 4.5 (2.0 to 7.0) | 5.3 (2.2 to 8.4) | 6.9 (3.9 to 9.9) | 8.6 (4.5 to 12.8) |
| Residence | ||||
| Rural | 7.0 (5.9 to 8.2) | 6.1 (4.6 to 7.5) | 7.7 (6.6 to 8.9) | 8.6 (6.8 to 10.3) |
| Urban | 8.3 (5.1 to 11.5) | 6.9 (4.4 to 9.4) | 12.7 (7.7 to 17.7) | 13.1 (10.1 to 16.2) |
The North Eastern region was excluded from the KAIS 2007 sample for comparability to KAIS 2012.
Z-test statistic used to compare KAIS 2007 and KAIS 2012 prevalence estimate: P < 0.001.
Z-test statistic used to compare KAIS 2007 and KAIS 2012 prevalence estimate: 0.001 ≤ P < 0.05.
Among persons aged 25–34 years, we observed declining HIV prevalence among men (8.1% in 2007 to 5.4% in 2012; P = 0.013) and women (12.0% in 2007 to 7.3% in 2012; P < 0.001). Among women aged 25–34 years, significant declines were observed among those residing in Nairobi (14.0% to 6.6%; P = 0.002), Coast (11.6% to 4.1%; P = 0.005), and Rift Valley (11.2% to 4.0%; P = 0.003) regions and those residing in both rural (11.4% to 6.3%; P < 0.001) and urban (13.5% to 8.7%; P = 0.036) areas in 2007 and 2012, respectively. Among men aged 25–34 years, significant declines were observed in Coast region (7.1% in 2007 to 0.6% in 2012; P = 0.002) and among persons residing in rural areas (8.0% in 2007 to 4.9% in 2012; P = 0.033). Among persons aged 35 years and older, no changes in HIV prevalence were observed across sex and urban/rural residences between 2007 and 2012. HIV prevalence, however, increased significantly among women residing in Central region, from 3.1% in 2007 to 8.4% 2012 (P = 0.001).
Factors Associated With Undiagnosed HIV Infection
Of the 10,097 persons who had ever had sex, 6.3% (95% CI: 5.3 to 7.1) were HIV infected (Table 2); 52.2% (95% CI: 46.5 to 57.8) of these had undiagnosed HIV infection (data not shown). We compared individuals with undiagnosed HIV infection with those who were HIV uninfected to assess factors associated with undiagnosed HIV infection. Among men, factors that were independently associated with increased odds of undiagnosed HIV infection were widowhood (AOR: 8.1, 95% CI: 1.9 to 34.6, P = 0.005) and using a condom with the last sexual partner in the past year (AOR: 3.3, 95% CI: 1.8 to 6.2, P < 0.001) (Table 4). In contrast, men who were circumcised had significantly lower odds of undiagnosed HIV infection (AOR: 0.3, 95% CI: 0.1 to 0.5, P < 0.001). Among women, higher odds of undiagnosed HIV infection were associated with being aged 34–39 years (AOR: 4.5, 95% CI: 1.1 to 18.3, P = 0.037), separated or divorced (AOR: 2.3, 95% CI: 1.1 to 5.0, P = 0.033), residence in Nyanza region (AOR: 2.9, 95% CI: 1.4 to 6.0, P = 0.004), living in urban areas (AOR: 1.8, 95% CI: 1.1 to 2.7, P = 0.012), having a moderate self-perceived risk of HIV infection (AOR: 2.1, 95% CI: 1.3 to 3.5, P = 0.002), using a condom with the last sexual partner in the past year (AOR: 2.3, 95% CI: 1.2 to 4.2, P < 0.009), and reporting ≥ 4 lifetime number of sexual partners (AOR: 1.9, 95% CI: 1.1 to 3.4, P = 0.026).
TABLE 4.
Factors Associated With Undiagnosed HIV Infection by Sex, Ever Sexually Active Persons Aged 15–64 Years, KAIS 2012
| Men (N = 4026)
|
Women (N = 5767)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P | AOR (95% CI) | P | OR (95% CI) | P | AOR (95% CI) | P | |
| Sociodemographic characteristics | ||||||||
| Age group, years | ||||||||
| 15–19 | 1.0 | — | 1.0 | — | 1.0 | — | 1.0 | — |
| 20–24 | 3.0 (0.6 to 15.6) | 0.202 | 1.6 (0.3 to 9.3) | 0.621 | 3.4 (1.0 to 11.2) | 0.046 | 2.6 (0.7 to 9.5) | 0.149 |
| 25–29 | 7.0 (1.4 to 33.6) | 0.016 | 4.1 (0.7 to 24.3) | 0.120 | 4.4 (1.4 to 14.1) | 0.013 | 3.6 (1.0 to 13.7) | 0.057 |
| 30–34 | 8.0 (1.7 to 36.8) | 0.008 | 3.4 (0.5 to 23.1) | 0.206 | 3.3 (1.0 to 11.0) | 0.057 | 3.3 (0.8 to 14.0) | 0.099 |
| 35–39 | 5.2 (1.2 to 22.2) | 0.028 | 2.2 (0.3 to 17.5) | 0.452 | 4.9 (1.5 to 16.2) | 0.010 | 4.5 (1.1 to 18.3) | 0.037 |
| 40–44 | 8.7 (1.8 to 41.3) | 0.007 | 4.8 (0.7 to 32.5) | 0.111 | 3.7 (1.1 to 12.0) | 0.032 | 2.8 (0.7 to 11.2) | 0.135 |
| 45–49 | 11.5 (2.4 to 54.0) | 0.002 | 5.2 (0.8 to 36.1) | 0.092 | 4.4 (1.2 to 16.0) | 0.024 | 3.3 (0.7 to 15.6) | 0.129 |
| 50–54 | 7.0 (1.5 to 33.9) | 0.015 | 3.3 (0.5 to 22.8) | 0.223 | 3.3 (0.9 to 11.8) | 0.073 | 3.3 (0.8 to 14.4) | 0.107 |
| 55–59 | 5.8 (1.0 to 32.3) | 0.046 | 2.0 (0.3 to 15.7) | 0.512 | 1.8 (0.5 to 7.0) | 0.408 | 1.8 (0.4 to 9.0) | 0.478 |
| 60–64 | 3.9 (0.7 to 21.1) | 0.109 | 1.1 (0.1 to 17.0) | 0.922 | 0.7 (0.1 to 4.2) | 0.718 | 0.7 (0.1 to 5.6) | 0.761 |
| Highest educational attainment | ||||||||
| No primary education | 1.0 | — | * | * | 1.0 | — | 1.0 | — |
| Incomplete primary education | 1.1 (0.3 to 3.5) | 0.934 | * | * | 1.6 (0.7 to 3.7) | 0.268 | 2.1 (0.9 to 4.6) | 0.068 |
| Completed primary education | 1.4 (0.5 to 3.7) | 0.523 | * | * | 2.1 (1.2 to 3.8) | 0.013 | 1.6 (0.6 to 4.3) | 0.313 |
| Completed secondary education or higher | 1.1 (0.5 to 2.8) | 0.764 | * | * | 1.9 (1.0 to 3.3) | 0.035 | 1.7 (0.8 to 3.6) | 0.205 |
| Region | ||||||||
| Nairobi | 1.0 | — | 1.0 | — | 1.0 | — | 1.0 | — |
| Central | 0.3 (0.1 to 0.9) | 0.024 | 0.4 (0.1 to 1.1) | 0.072 | 1.1 (0.6 to 2.1) | 0.680 | 1.4 (0.7 to 2.8) | 0.400 |
| Coast | 0.5 (0.2 to 1.2) | 0.128 | 0.6 (0.2 to 1.7) | 0.321 | 1.4 (0.8 to 2.6) | 0.268 | 2.0 (1.0 to 4.1) | 0.061 |
| Eastern North | 0.3 (0.1 to 1.2) | 0.091 | 0.4 (0.1 to 1.8) | 0.251 | 0.6 (0.2 to 1.5) | 0.282 | 1.3 (0.4 to 3.8) | 0.666 |
| Eastern South | 0.6 (0.2 to 1.7) | 0.303 | 0.8 (0.3 to 2.4) | 0.667 | 1.0 (0.4 to 2.1) | 0.915 | 1.0 (0.4 to 2.4) | 0.933 |
| North Rift | 0.7 (0.3 to 1.7) | 0.402 | 0.7 (0.3 to 1.8) | 0.485 | 1.1 (0.5 to 2.2) | 0.878 | 1.0 (0.4 to 2.8) | 0.965 |
| Nyanza | 3.1 (1.6 to 6.0) | <0.001 | 2.1 (0.9 to 4.7) | 0.074 | 2.9 (1.6 to 5.0) | <0.001 | 2.9 (1.4 to 6.0) | 0.004 |
| South Rift | 0.6 (0.2 to 1.4) | 0.222 | 0.6 (0.2 to 2.1) | 0.448 | 0.6 (0.3 to 1.2) | 0.154 | 1.6 (0.7 to 3.6) | 0.219 |
| Western | 0.7 (0.3 to 1.6) | 0.393 | 0.6 (0.3 to 1.5) | 0.286 | 0.9 (0.5 to 1.7) | 0.770 | 1.6 (0.7 to 3.6) | 0.291 |
| Residence | ||||||||
| Rural | 1.0 | — | * | * | 1.0 | — | 1.0 | — |
| Urban | 1.2 (0.7 to 1.9) | 0.513 | * | * | 1.5 (1.1 to 2.1) | 0.014 | 1.8 (1.1 to 2.7) | 0.012 |
| Wealth index | ||||||||
| Poorest | 1.0 | — | * | * | 1.0 | — | 1.0 | — |
| Second | 1.7 (0.8 to 3.3) | 0.138 | * | * | 1.4 (0.9 to 2.4) | 0.153 | 1.0 (0.6 to 1.9) | 0.913 |
| Third | 1.3 (0.7 to 2.6) | 0.433 | * | * | 1.4 (0.8 to 2.5) | 0.243 | 1.3 (0.7 to 2.3) | 0.454 |
| Fourth | 1.6 (0.8 to 3.3) | 0.165 | * | * | 2.1 (1.2 to 3.6) | 0.009 | 1.4 (0.7 to 2.7) | 0.364 |
| Richest | 1.3 (0.6 to 2.8) | 0.435 | * | * | 1.4 (0.8 to 2.4) | 0.254 | 0.8 (0.4 to 1.8) | 0.599 |
| Marital status | ||||||||
| Never married/never cohabited | 1.0 | — | 1.0 | — | 1.0 | — | 1.0 | — |
| Ever widowed | 9.9 (4.2 to 23.0) | <0.001 | 8.1 (1.9 to 34.6) | 0.005 | 2.0 (1.1 to 3.7) | 0.022 | 2.2 (0.9 to 5.5) | 0.080 |
| Separated or divorced | 3.7 (1.4 to 9.8) | 0.008 | 2.5 (0.7 to 9.3) | 0.157 | 3.3 (1.9 to 5.8) | <0.001 | 2.3 (1.1 to 5.0) | 0.033 |
| Currently married or cohabiting—polygamous | 4.2 (1.6 to 11.4) | 0.004 | 1.3 (0.3 to 6.2) | 0.749 | 1.3 (0.7 to 2.5) | 0.383 | 1.0 (0.4 to 2.6) | 0.921 |
| Currently married or cohabiting—monogamous | 3.1 (1.6 to 6.0) | <0.001 | 2.8 (0.9 to 8.6) | 0.065 | 0.8 (0.5 to 1.4) | 0.410 | 0.8 (0.4 to 1.7) | 0.626 |
| Behavioral indicators | ||||||||
| Lifetime number of partners | ||||||||
| 1 | 1.0 | — | 1.0 | — | 1.0 | — | 1.0 | — |
| 2–3 | 2.2 (1.0 to 5.0) | 0.050 | 1.8 (0.6 to 5.4) | 0.263 | 1.9 (1.2 to 2.8) | 0.002 | 1.3 (0.8 to 1.9) | 0.261 |
| 4+ | 3.3 (1.4 to 8.1) | 0.008 | 2.3 (0.8 to 7.0) | 0.128 | 3.5 (2.2 to 5.5) | <0.001 | 1.9 (1.1 to 3.4) | 0.026 |
| Do not know | 5.9 (2.3 to 15.1) | <0.001 | 2.7 (0.7 to 10.1) | 0.135 | 2.3 (1.1 to 4.6) | 0.022 | 1.4 (0.6 to 3.3) | 0.390 |
| Used a condom with last partner in the past 12 mo | ||||||||
| No | 1.0 | — | 1.0 | — | 1.0 | — | 1.0 | — |
| Yes | 1.8 (1.1 to 2.9) | 0.013 | 3.3 (1.8 to 6.2) | <0.001 | 2.5 (1.7 to 3.8) | <0.001 | 2.3 (1.2 to 4.2) | 0.009 |
| Not sexual active in the past 12 mo | 0.7 (0.3 to 1.3) | 0.256 | 1.6 (0.6 to 4.0) | 0.332 | 1.8 (1.2 to 2.5) | 0.003 | 1.3 (0.7 to 2.5) | 0.340 |
| HIV risk perception | ||||||||
| No risk | 1.0 | — | 1.0 | — | 1.0 | — | 1.0 | — |
| Low risk | 1.6 (0.9 to 2.9) | 0.107 | 1.3 (0.7 to 2.3) | 0.444 | 1.3 (0.8 to 2.0) | 0.311 | 1.3 (0.8 to 2.1) | 0.249 |
| Moderate risk | 1.6 (0.7 to 3.8) | 0.235 | 0.8 (0.3 to 2.1) | 0.718 | 2.5 (1.5 to 4.1) | <0.001 | 2.1 (1.3 to 3.5) | 0.002 |
| Great risk | 3.3 (1.3 to 8.3) | 0.011 | 2.3 (0.8 to 6.6) | 0.122 | 2.1 (1.1 to 4.0) | 0.028 | 1.6 (0.8 to 3.2) | 0.192 |
| Most-at-risk behaviors | ||||||||
| Ever injected drugs for pleasure | ||||||||
| No | 1.0 | — | * | * | — | — | — | — |
| Yes | 3.5 (0.5 to 25.9) | 0.215 | * | * | — | — | — | — |
| Ever had anal sex | ||||||||
| No | 1.0 | — | * | * | 1.0 | — | 1.0 | — |
| Yes | 1.2 (0.4 to 3.6) | 0.759 | * | * | 2.3 (1.0 to 5.3) | 0.059 | 1.7 (0.6 to 4.6) | 0.281 |
| Ever received money, gifts, or goods in exchange for sex | ||||||||
| No | 1.0 | — | * | * | 1.0 | — | * | * |
| Yes | 1.4 (0.6 to 3.4) | 0.476 | * | * | 1.4 (0.7 to 2.9) | 0.340 | * | * |
| Ever gave money, gifts, or goods in exchange for sex (men only) | ||||||||
| No | 1.0 | — | * | * | — | — | — | — |
| Yes | 1.0 (0.6 to 1.7) | 0.986 | * | * | — | — | — | — |
| Biologic indicators | ||||||||
| STI symptoms in the past 12 mo | ||||||||
| No | 1.0 | — | 1.0 | — | 1.0 | — | * | * |
| Yes | 3.6 (1.7 to 7.6) | <0.001 | 1.6 (0.7 to 3.8) | 0.280 | 1.3 (0.7 to 2.4) | 0.386 | * | * |
| Ever been tested for HIV | ||||||||
| No | 1.0 | — | * | * | 1.0 | — | * | * |
| Yes | 1.1 (0.7 to 1.7) | 0.740 | * | * | 1.0 (0.6 to 1.5) | 0.876 | * | * |
| Male circumcision status (men only) | ||||||||
| No | 1.0 | — | 1.0 | — | — | — | — | — |
| Yes | 0.1 (0.1 to 0.2) | <0.001 | 0.3 (0.1 to 0.5) | <0.001 | — | — | — | — |
| Male partner circumcised (women only) | ||||||||
| No | — | — | — | — | 1.0 | — | 1.0 | — |
| Yes | — | — | — | — | 0.4 (0.3 to 0.6) | <0.001 | 0.7 (0.4 to 1.1) | 0.106 |
Indicates variable not retained in final multivariate model.
Bolded results were statistically significant findings at P < 0.05 in the final multivariate model.
AOR, adjusted odds ratio; OR, odds ratio.
DISCUSSION
This population-based survey provides an update on the status of the HIV epidemic in Kenya. HIV prevalence was 5.6% and HIV incidence was 0.5% among persons aged 15–64 years. This represents approximately 1,192,000 million (95% CI: 1,037,000 to 1,347,000) adults and adolescents living with HIV in 2012, 106,000 (95% CI 32,000 to 180,000) of whom had recently acquired their HIV infection within the preceding year. These results broadly corroborate the 2012 estimates published by the Joint United Nations Programme on HIV/AIDS in 2013, which reported that the number of Kenyan adults and adolescents aged ≥15 years living with HIV/AIDS in 2012 was 1,400,000 (lower estimate: 1,400,000; upper estimate: 1,500,000), and the number of new infections was 85,000 (lower estimate: 80,000; upper estimate: 96,000).1 Based on our results, the annual HIV transmission rate was 8.9 per 100 persons living with HIV in 2012. In other words, 9% of all persons living with HIV in 2012 were transmitting to HIV-negative persons. In comparison, the annual transmission rate in the United States, where 16% of the HIV-infected population remains undiagnosed, was 4.1 per 100 HIV-infected persons in 2010.10
Our data confirm a significant decline in HIV prevalence from 7.2% (excluding North Eastern region) in 2007 to 5.6% in 2012, with similar declines noted across male and female sex. Based on mathematically modeled HIV incidence in 2007, our results also suggest that HIV incidence may have declined from 0.7% in 2007 to 0.5% in 2012, coinciding with similar declines in new HIV infections reported by at least 26 countries in Africa, Asia, and the Caribbean between 2001 and 2012.1,11 Declining incidence is also supported by the observation that HIV prevalence reduced significantly among younger persons aged 15–34 years between 2007 and 2012 but remained unchanged among older persons aged 35 years and above.
Among persons aged 15–34 years, we observed differential trends in HIV prevalence across geographic regions and sex, providing important epidemiologic evidence on sub-populations where substantial reductions in HIV infection may be occurring. Among women, declining prevalence was observed for women aged 15–34 years in Nairobi and Coast regions, women aged 15–24 years in Eastern region, and women aged 25–34 years in Rift Valley region. Among men, declining prevalence was observed among men aged 15–34 years in Coast region. Of concern, we found a significant increase in HIV prevalence among middle-aged and older women (aged ≥35 years) residing in Central region.
Reductions in HIV prevalence on a population level is possible if there are marked declines in new HIV infections or high rates of HIV-related death in a population. If substantial, both scenarios on their own could result in a diminished pool of infected people in the population. Over the past 5 years, Kenya has experienced substantial progress in linking HIV-infected persons into HIV care and placing those that require ART on treatment.12 Increased coverage of ART and high levels of viral suppression on ART have led to significant reductions in HIV mortality and HIV transmission risk, likely contributing to a possible decline in HIV incidence over the past 5 years.1,12 Still, over half of HIV-infected persons in the country remained undiagnosed by the year-end (2012), representing a major barrier to achieving even greater reductions in HIV transmission to eventually halt the spread of infection.13 A critical component to reversing this trend will be to accelerate ART coverage in the country by prioritizing HIV testing in settings that will yield greater numbers of HIV-infected persons, facilitating their immediate linkages into HIV care services, and treating them promptly.
Our findings provide important insight on groups with increased risk of transmitting HIV to sexual partners, highlighting opportunities for targeted HIV prevention. Markers of high-risk sexual behaviors, including multiple sexual partners and perceived risk of HIV infection were associated with higher odds of undiagnosed HIV infection. Surprisingly, we found that persons who used a condom with their last sexual partner in the past 12 months had higher odds of undiagnosed HIV infection. This positive association may be a reflection of reluctance or denial in admitting to unprotected sex. Alternatively, it could suggest that persons who choose to use condoms with their sexual partners may already know that they are at high risk of HIV infection despite lack of awareness of their HIV infection. The use of condoms in this group is an encouraging finding for HIV-positive prevention strategies but raises the question as to whether current condom use campaigns are effective in reaching the general population with messages on the important benefits of correct and consistent condom use for HIV prevention.
Widowhood has been previously described as a factor associated with HIV infection in Kenya and other countries in sub-Saharan Africa although the factors that place widowed men at higher risk of HIV infection are not clear-cut.14–18 Widowers whose spouses died of HIV disease may have been exposed to high viral load from their partners, which can occur during late-stage disease,17 but it is also possible that widowed men were sources of infection for their spouses who died from the disease. Studies have also demonstrated that widowers are more likely to engage in high-risk sexual behavior after the death of their spouse and contribute to new HIV infections in the population.15
In addition to widowhood, the link between HIV infection and divorce or separation in women sheds additional light on the vulnerability of women in the Kenyan HIV epidemic. Previous studies in sub-Saharan Africa have reported that the dissolution of marriage, through divorce or separation, is often the result of a female’s HIV status within the couple relationship. HIV-infected women in serodiscordant relationships are more likely to be separated or divorced than HIV-infected men in serodiscordant relationships, reinforcing the gender disparities that exist around sexual norms in the African context.18 Further exploration of the impact of serodiscordancy on marital outcomes and implications for the spread of HIV may help to understand how to appropriately strategize prevention, care, and treatment services for couples and formerly married individuals.
Male circumcision has been widely cited as a key pillar of HIV prevention that can significantly reduce new HIV infections in a population.19–21 Because of an aggressive national strategy on male circumcision, which was implemented in 2008, Kenya has observed substantial increases in male circumcision over the past 5 years, increasing from 85.0% in 2007 to 91.2% in 2012.11 Greatest increases were noted in the 4 priority regions for the national voluntary male medical circumcision program: Nairobi, Nyanza, Rift Valley, and Western regions.11 However, coverage in traditionally noncircumcising communities, where regional HIV prevalence is highest, still remains far below the national target of 80% of adult men.22 We found lower odds of HIV infection among circumcised men highlighting that the prevention benefits of this intervention will continue to play an important role in addressing the HIV epidemic in Kenya. Further scale-up of HIV prevention should aim for universal male circumcision accompanied with sexual risk reduction strategies for greater impact in the longer term.
Our results provided important information on geographic areas which require specialized attention for HIV prevention. Continued momentum is needed to address persistently high levels of HIV infection in Nyanza region. Moreover, the observed increases in HIV prevalence among middle-aged and older women in Central region, as well as elevated risk of HIV infection among women in urban residences, are areas which require more focused strategies.
Our study had several limitations. Because this study was cross-sectional in design, we were unable to infer directionality of associations, such as the associations between HIV infection and condom use with last sexual partner, widowhood among men, and divorce or separation among women. Behaviors, circumcision status, and symptoms of STI were self-reported, and associations observed may have been impacted by social desirability bias. Selection bias may have been introduced by decisions to exclude North Eastern region from the sampling frame because of security concerns. The North Eastern region, however, is relatively sparsely populated and had an HIV prevalence of only 0.8% in KAIS 2007,5 and we feel it is unlikely that excluding this region affected our results substantially. Differences in HIV prevalence between KAIS 2007 and KAIS 2012 could also reflect changes in composition of the sample between the two surveys. Compared with KAIS 2007, the sample in KAIS 2012 had significantly higher proportions of persons who were aged 25–34 years, never married or never cohabited, reported secondary education or higher and were from urban residences.7 The demographic, behavioral, and biological differences observed among KAIS 2012 participants in the interview and serologic sample may have also contributed to either an underestimation or overestimation of HIV prevalence in 2012, limiting our ability to accurately interpret trends in HIV prevalence.
Despite these limitations, KAIS 2012 was a large representative study whose primary findings were based on biological samples obtained during the survey. We believe that evidence of decreasing HIV prevalence to be encouraging yet underscores the need to establish routine and standardized surveillance methods to monitor trends in recently acquired HIV infections and HIV-related mortality for a clearer interpretation of the epidemiology of HIV in the country. Our data support that substantial interventions are needed to improve identification of HIV-infected persons to effectively reach those in need of ART for improved survival and continued reductions in transmission risks. Continued monitoring of the burden of HIV disease through enhanced surveillance and seeking to assess and respond to factors associated with undiagnosed HIV infection are central to an effective response to the HIV epidemic in Kenya.
Acknowledgments
Kenya AIDS Indicator Survey (KAIS) 2012 was supported by the National AIDS and STI Control Programme (NASCOP), Kenya National Bureau of Statistics (KNBS), National Public Health Laboratory Services (NPHLS), National AIDS Control Council (NACC), National Council for Population and Development (NCPD), Kenya Medical Research Institute (KEMRI), US Centers for Disease Control and Prevention (CDC/Kenya, CDC/Atlanta), United States Agency for International Development (USAID/Kenya), University of California, San Francisco (UCSF), Joint United Nations Team on HIV/AIDS, Japan International Cooperation Agency (JICA), Elizabeth Glaser Paediatric AIDS Foundation (EGPAF), Liverpool Voluntary Counselling and Testing (LVCT), African Medical and Research Foundation (AMREF), World Bank, and Global Fund. This publication was made possible by support from the US President’s Emergency Plan for AIDS Relief through cooperative agreements (PS001805, GH000069, and PS001814) from the US Centers for Disease Control and Prevention, Division of Global HIV/AIDS. This work was also funded in part by support from the Global Fund, World Bank, and the Joint United Nations Team for HIV/AIDS.
The authors thank the fieldworkers and supervisors for their excellent work during KAIS data collection and all the individuals who participated in this national survey. The authors also thank Timothy Kellogg for his statistical input; George Rutherford and Joy Mirjahangir for discussing and reviewing the article; Anthony Gichangi, John Bore, James Ng’ang’a, Ray Shiraishi, Eddas Bennett, and Paul Stupp for their input in weighting of the data set; and the KAIS Study Group for their contribution to the design of the survey and collection of the data set: Willis Akhwale, Sehin Birhanu, John Bore, Angela Broad, Robert Buluma, Thomas Gachuki, Jennifer Galbraith, Anthony Gichangi, Beth Gikonyo, Margaret Gitau, Joshua Gitonga, Mike Grasso, Malayah Harper, Andrew Imbwaga, Muthoni Junghae, William Maina, Nicolas Muraguri, Mutua Kakinyi, Samuel Mwangi Kamiru, Nicholas Owenje Kandege, Lucy Kanyara, Yasuyo Kawamura, Timothy Kellogg, George Kichamu, Andrea Kim, Lucy Kimondo, Davies Kimanga, Elija Kinyanjui, Stephen Kipkerich, Danson Kimutai Koske, Boniface O. K’Oyugi, Veronica Lee, Serenita Lewis, William Maina, Ernest Makokha, Agneta Mbithi, Joy Mirjahangir, Ibrahim Mohamed, Rex Mpazanje, Silas Mulwa, Nicolas Muraguri, Patrick Murithi, Lilly Muthoni, James Muttunga, Jane Mwangi, Mary Mwangi, Sophie Mwanyumba, Francis Ndichu, Anne Ng’ang’a, James Ng’ang’a, John Gitahi Ng’ang’a, Lucy Ng’ang’a, Carol Ngare, Bernadette Ng’eno, Inviolata Njeri, David Njogu, Bernard Obasi, Macdonald Obudho, Edwin Ochieng, Linus Odawo, Jacob Odhiambo, Caleb Ogada, Samuel Ogola, David Ojakaa, James Kwach Ojwang, George Okumu, Patricia Oluoch, Tom Oluoch, Kenneth Ochieng Omondi, Osborn Otieno, Yakubu Owolabi, Bharat Parekh, George Rutherford, Sandra Schwarcz, Shahnaaz Sharrif, Victor Ssempijja, Lydia Tabuke, Yuko Takenaka, Mamo Umuro, Brian Eugene Wakhutu, Wanjiru Waruiru, Celia Wandera, John Wanyungu, Anthony Waruru, Paul Waweru, Larry Westerman, and Kelly Winter.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention and the Government of Kenya.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) Global Report. UNAIDS Report on the Global AIDS Epidemic 2013. Geneva, Switzerland: UNAIDS; 2013. [Google Scholar]
- 2.Kenya National Bureau of Statistics (KNBS) 2009 Kenya Population and Housing Census: Volume 1C. Population Distribution by Age, Sex and Administrative Units. Nairobi, Kenya: KNBS; 2010. [Google Scholar]
- 3.Kenya National Bureau of Statistics (KNBS) and ICF Macro. Kenya Demographic and Health Survey 2008–09. Calverton, Maryland: KNBS and ICF MACRO; 2010. [Google Scholar]
- 4.Central Bureau of Statistics (CBS) Kenya Ministry of Health (MOH), and ORC Macro. Kenya Demographic and Health Survey 2003. Calverton, Maryland: CBS, MOH, and ORC Macro; 2004. [Google Scholar]
- 5.National AIDS and STI Control Programme (NASCOP) 2007 Kenya AIDS Indicator Survey Final Report. Nairobi, Kenya: NASCOP; 2009. [Accessed May 25, 2013]. Available at: http://www.nascop.or.ke/public_site/webroot/cache/article/file/KAIS Final Report.pdf. [Google Scholar]
- 6.Maina WK, Kim AA, Rutherford G, et al. Kenya AIDS indicator surveys 2007 and 2012: Implications for public health policies for HIV prevention and treatment. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S130–S137. doi: 10.1097/QAI.0000000000000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waruiru W, Kim AA, Kimanga DO, et al. The Kenya AIDS indicator survey 2012: rationale, methods, description of participants and response rates. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S3–S12. doi: 10.1097/QAI.0000000000000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National AIDS and STI Control Programme (NASCOP) National Guidelines for HIV Testing and Counseling in Kenya. 2. Nairobi, Kenya: NASCOP; 2010. Available at: http://www.nascop.or.ke. [Google Scholar]
- 9.World Health Organization (WHO) When and How to Use Assays for Recent Infection to Estimate HIV Incidence at a Population Level. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 10.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2011. [Accessed December 30, 2013];HIV Surveill Supplemental Rep. 2013 18 Available at: http://www.cdc.gov/hiv/library/reports/surveillance/. Published 2013. [Google Scholar]
- 11.Kim AA, Hallett T, Stover J, et al. Estimating HIV incidence among adults in Kenya and Uganda: a systematic comparison of multiple methods. PLoS One. 2011;6:e17535. doi: 10.1371/journal.pone.0017535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National AIDS and STI Control Programme (NASCOP) Kenya AIDS Indicator Survey 2012: Preliminary Report. Nairobi, Kenya: NASCOP; 2013. [Google Scholar]
- 13.Ng’ang’a A, Waruiru W, Ngare C, et al. The status of HIV testing and counselling in Kenya: results from a nationally representative population-based survey. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S27–S36. doi: 10.1097/QAI.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oluoch T, Mohammed I, Bunnell R, et al. Correlates of HIV infection among sexually active adults in Kenya: a national population-based survey. Open AIDS J. 2011;5:125–134. doi: 10.2174/1874613601105010125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lopman BA, Nyamukapa C, Hallett T, et al. Role of widows in the heterosexual transmission of HIV in Manicaland, Zimbabwe, 1998–2003. Sex Transm Infec. 2009;85(suppl 1):i41–48. doi: 10.1136/sti.2008.033043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mermin J, Musinguzi J, Opio A, et al. Risk factors for recent HIV infection in Uganda. JAMA. 2008;300:540–549. doi: 10.1001/jama.300.5.540. [DOI] [PubMed] [Google Scholar]
- 17.Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project study group. N Engl J Med. 2000;342:921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- 18.Porter L, Hao L, Bishai D, et al. HIV status and union dissolution in sub-Saharan Africa: the case of Rakai, Uganda. Demography. 2004;41:465–482. doi: 10.1353/dem.2004.0025. [DOI] [PubMed] [Google Scholar]
- 19.Auvert B, Taljaard D, Lagarde E, et al. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2:e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bailey R, Moses S, Parker C, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–656. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 21.Gray R, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–666. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 22.Galbraith J, Ochieng A, Mwalili S, et al. Status of voluntary medical male circumcision in Kenya: findings from two nationally-representative surveys in Kenya, 2007 and 2012. J Acquir Immune Defic Syndr. 2014;66(suppl 1):S37–S45. doi: 10.1097/QAI.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]