Summary
Background
Wandering spleen is a rare condition which if uncorrected, can result in torsion and infarction. Clinical presentation of a wandering spleen can vary from asymptomatic abdominal mass to acute abdominal pain. Radiological investigations play a pivotal role in diagnosis as the clinical diagnosis is usually impossible.
Case Report
We present a case of wandering spleen with torsion and complete infarction that occurred in a 32-year-old multiparous female. The diagnosis was established preoperatively on colour Doppler and CT of the abdomen with subsequent confirmation on surgery.
Conclusions
Wandering spleen is a rare clinical condition which can present as acute abdomen. An increased awareness of this entity together with the timely use of ultrasound and CT of the abdomen can play an important role in preoperative diagnosis and surgical management.
MeSH Keywords: Abdomen, Acute; Splenectomy; Splenic Infarction; Wandering Spleen
Background
Wandering spleen is an uncommon clinical entity that results from abnormal laxity or absence of the supporting ligaments. Symptoms depend on the degree of torsion and range from chronic abdominal pain in mild torsion to acute pain in severe torsion and infarction. Accurate clinical diagnosis is difficult because of the rarity of the condition and non-specific symptoms. Radiological evaluation includes usage of ultrasound, Doppler, abdominal CT or MRI depending upon availability or preference. Cases of wandering spleen with torsion and complete infarction are seldom reported. We describe the Doppler and CT findings in a case of wandering spleen which had undergone complete infarction secondary to torsion. Knowledge of this rare entity and its radiological findings can prove crucial in making a correct preoperative diagnosis.
Case Report
A 32-year-old female patient presented in the emergency department with a 2–3-day history of intense pain on the left side of the abdomen along with low-grade fever. She gave a history of similar episodes of abdominal pain in the past but those were of less severe intensity. On admission she had a blood pressure of 110/70 mm Hg; pulse rate of 110 beats/min and body temperature of 38.3 degree Celsius. A vague mass was palpable in the left mid and lower abdomen. Routine blood tests were normal except for elevated white blood counts at 18×109/L. She was taken up for urgent ultrasound which revealed absence of spleen in its normal location in the left upper abdomen. A heterogeneous hypoechoic capsulated mass with size and shape resembling that of the spleen was seen in the left mid and lower abdomen. It showed absence of internal vascularity on colour Doppler imaging (Figure 1). Based on ultrasound findings, a diagnosis of wandering spleen with possible torsion was sustained. A CT of the abdomen performed preoperatively on the next day, confirmed the ultrasound diagnosis. The surview CT image revealed the absence of the splenic shadow in the left upper abdomen and its replacement by bowel gases. A vague soft tissue opacity was noticed in the left mid abdomen which represented the abnormally located spleen (Figure 2). Non-contrast images showed the typical findings of an abnormally located spleen, with a hyperdense splenic pedicle (Figure 3). On post-contrast images there was a lack of parenchymal enhancement in the spleen (Figures 4, 5). On surgery, the spleen appeared congested and infracted, and total splenectomy was performed. The post-operative recovery of the patient was uneventful and she was discharged after 2 weeks.
Figure 1.

Transverse Doppler image showing heterogeneously hypoechoic echotexture of the spleen with no internal vascularity.
Figure 2.
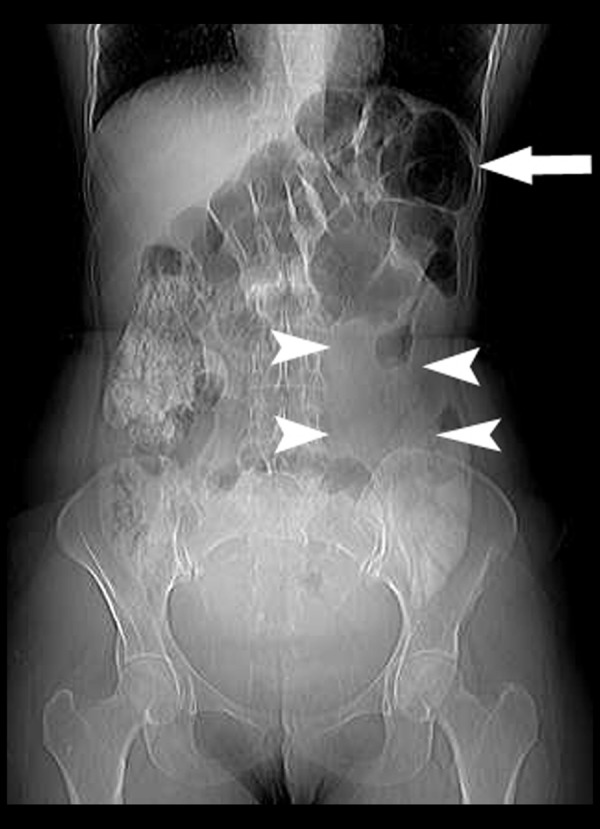
CT surview image showing absence of the splenic shadow in the left upper abdomen (arrow) and a vague soft tissue opacity in the left mid abdomen (arrowheads).
Figure 3.

Axial non-contrast CT of the abdomen showing a whorled splenic pedicle with a hyperdense vessel (arrow).
Figure 4.

Axial contrast-enhanced CT image showing the lack of parenchymal enhancement in the spleen (arrows).
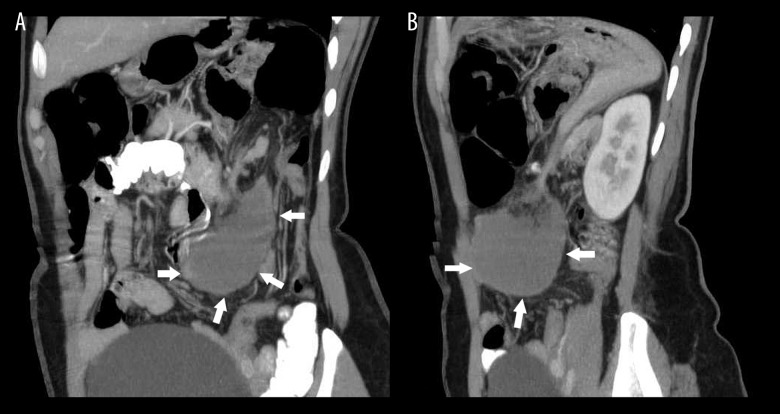
Figure 5.
Oblique coronal (A) and sagittal MPR image (B) of contrast-enhanced CT showing the abnormal location of the spleen with no parenchymal enhancement (arrows).
Discussion
Wandering spleen is not encountered frequently and accounts for less than 0.5% of splenectomies [1]. It implies migration of the spleen from its fixed position in the left upper abdomen and occurs mainly in children or women aged 20–40 years [2,3]. Normally, the spleen is anchored in its anatomical position by the gastrosplenic and splenorenal ligaments. In children, congenital maldevelopment of the fixating ligaments can result in a long splenic vascular pedicle and an abnormally mobile spleen [4]. The acquired aetiological factors of wandering spleen are associated with multiparity which causes laxity of the anchoring ligaments due to hormonal effects of pregnancy and abdominal wall weakness [5]. Besides multiparity, this condition may also be seen with other conditions like lymphoma, chronic myeloid leukemia, malaria that cause splenomegaly.
Clinical manifestations of wandering spleen are varied. In cases of wandering spleen without torsion, the patients may be entirely asymptomatic and the condition comes to light due to an incidentally noticed mobile abdominal or pelvic mass. Torsion is a known complication of wandering spleen and the symptoms and signs of torsion depend on the degree of torsion. Mild torsion presents with chronic pain of the abdomen because of splenic congestion while moderate degree of torsion manifests as severe intermittent pain of the abdomen because of periods of torsion and detorsion [5]. Severe torsion results in splenic infarction and presents as acute abdomen [4,5]. In our case the patient gave a history of chronic relapsing remitting pain of the abdomen prior to the acute abdomen which, according to our speculations, was due to periods of moderate torsion and detorsion.
A number of radiological investigations like plain film radiography, grayscale ultrasound, Doppler sonography, CT scan or MRI of the abdomen have been used in diagnostic evaluation of wandering spleen with torsion. The findings on plain radiograph include nonvisualization of the splenic shadow in the left upper abdomen and its replacement by a gas-filled loop, a large central abdominal mass or left-flank mass [6]. On gray scale ultrasound the spleen is absent from its position in the left upper abdomen and instead a capsulated mass is visualized in the abdomen or pelvis [7]. It shows a heterogenous, and predominantly hypoechoic echotexture with reduced or absent intraparenchymal and/or splenic hilar flow on color Doppler imaging [8]. The CT findings include whorled appearance of the splenic pedicle which may or may not be accompanied by twisting of the pancreatic tail [9]. On non-contrast sections the spleen shows lower density values than the hepatic parenchyma and a hyperdensity may be identifiable in the splenic pedicle representing a thrombosed splenic vein [7]. The spleen may also be enlarged (due to accompanying congestion) with minimal or no post-contrast enhancement of the parenchyma suggesting infarction [7,8]. MRI can be used as an alternative to CT and it can identify infarcts on both T1- and T2-weighted images. Loss of signal void of the splenic pedicle vessels suggests thrombosis. Our case showed typical grayscale ultrasound, Doppler and CT findings of wandering spleen with torsion and complete infarction. The findings were confirmed during surgery and subsequent histopathological examination.
The surgical treatment options of wandering spleen depend on its viability. If the spleen is viable, either open or laproscopic splenopexy may be offered. If however the spleen is infracted, a partial subtotal resection or splenectomy is considered [10]. The patient should be offered vaccination against capsulated pathogens like pnemococcus, H influenzae and meningococcus.
Conclusions
Wandering spleen should be considered in the differential diagnosis of acute abdomen. A high index of suspicion and increased awareness of this rare condition coupled with the use of radiological modalities like Doppler and CT of the abdomen are very crucial in making an accurate and timely diagnosis.
Footnotes
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Lam Y, Yuen KK, Chong LC. Acute torsion of a wandering spleen. Hong Kong Med J. 2012;18:160–62. [PubMed] [Google Scholar]
- 2.Gayer G, Zissin R, Apter S, et al. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001;74:767–72. doi: 10.1259/bjr.74.884.740767. [DOI] [PubMed] [Google Scholar]
- 3.Alimoglu O, Sahin M, Akdag M. Torsion of a wandering spleen presenting with acute abdomen: a case report. Acta Chir Belg. 2004;104:221–23. doi: 10.1080/00015458.2004.11679541. [DOI] [PubMed] [Google Scholar]
- 4.Chawla S, Boal DK, Dillon PW, et al. Splenic torsion. Radiographics. 2003;23:305–8. doi: 10.1148/rg.232025110. [DOI] [PubMed] [Google Scholar]
- 5.Yakan S, Telciler KE, Denecli AG. Acute torsion of a wandering spleen causing acute abdomen. Hong Kong J Emerg Med. 2011;18:34–36. [Google Scholar]
- 6.Gordon DH, Burrell MI, Levin DC, et al. Wandering spleen: the radiological and clinical spectrum. Radiology. 1977;125:39–46. doi: 10.1148/125.1.39. [DOI] [PubMed] [Google Scholar]
- 7.Chu J, Li Z, Luo B, et al. Wandering spleen with torsion and complete infarction. Acta Radiol. 2011;52:911–13. doi: 10.1258/ar.2011.100504. [DOI] [PubMed] [Google Scholar]
- 8.Nemeck AA, Miller FH, Fitzgerald SW. Acute torsion of a wandering spleen: Diagnosis by CT and Duplex Doppler and color flow sonography. Am J Roentgenol. 1991;157:307–9. doi: 10.2214/ajr.157.2.1853811. [DOI] [PubMed] [Google Scholar]
- 9.Swischuk LE, Williams JB, John SD. Torsion of wandering spleen: the whorled appearance of the splenic pedicle on CT. Pediatr Radiol. 1993;23:476–77. doi: 10.1007/BF02012458. [DOI] [PubMed] [Google Scholar]
- 10.Cohen MS, Soper NJ, Underwood RA, et al. Laparoscopic splenopexy for wandering (pelvic) spleen. Surg Laparosc Endosc. 1998;8:286–90. [PubMed] [Google Scholar]