Abstract
Background:
Several chemotherapeutic agents have been developed to prevent gingivitis and its progression into periodontitis. In this present study, the efficacy of ozonated oil and chlorhexidine gel was assessed and compared on plaque induced gingivitis.
Aim:
To evaluate the effect of ozonated oil on plaque induced gingivitis and to compare its efficacy with chlorhexidine gel.
Materials and Methods:
A total of 20 subjects, aged from 18 to 65 years, with plaque-induced gingivitis were selected from the outpatient Department of Periodontology, Government Dental College and Hospital, Aurangabad, for this study. They were divided randomly into the test or ozonated oil group (Group I) and the control or chlorhexidine gel group (Group II) with 10 subjects in each group. Subjects were randomly assigned to massage their gingiva thrice a day for 3 weeks with ozonated oil (test), and chlorhexidine gel (control). Plaque index and gingival index scores were recorded for the 20 subjects at baseline and after 3 weeks.
Results:
Ozonated oil (Group I) and chlorhexidine gel (Group II) groups showed statistically significant differences with respect to plaque index and gingival index, from the baseline to 3 weeks (P < 0.001 in both). But the difference between Group I and Group II, at the end of the study period, was not statistically significant with respect to the plaque index and gingival index.
Conclusions:
The ozonated oil and chlorhexidine gel, both can be used as an effective agent in maintaining and improving gingival health.
Keywords: Chlorhexidine gel, gingival massage, ozonated oil, plaque induced gingivitis
INTRODUCTION
Plaque-induced gingivitis is an inflammatory process, limited to the gingiva, resulting from bacteria located at the gingival margin. To prevent gingivitis and its progression to periodontitis, daily and effective supra-gingival plaque control methods are considered the most effective methods to regain and maintain dental and periodontal health.
Chlorhexidine is considered to be the “gold standard” agent for chemical plaque control methods, as it is a broad spectrum antiseptic. However, chlorhexidine is discouraged because of its unpleasant taste and undesirable side effects such as tooth staining.[1]
Ozone (O3), is found in nature, in the form of a gas in the stratosphere in a concentration of 1–10 ppm, being continually created from and destroyed into molecular O2. It is one of the most important gases in the stratosphere due to its ability to filter ultraviolet rays, which is critical for the maintenance of biological balance in the biosphere. The German Chemist Christian Friedrich Schonbein is considered to be the father of ozone therapy (1840). When he passed an electric discharge through water, a strange smell was produced, which he called ozone, from the Greek word ozein (odor). In dentistry, Dr. E.A. Fisch (1889–1966) was the first dentist to use ozonated water in his practice. Joachim Hansler, a German physicist, joined Hans Wolff, another German physician, to develop the first ozone generator for medical use. The main use of ozone in dentistry is relays on its antimicrobial properties. It is proved to be effective against both Gram-positive and Gram-negative bacteria, viruses and fungi.[2] In periodontology, it has been used for gingivitis, periodontits, peri-implantitis, surgical cuts, prophylaxis. Ozone can be used in various forms for treatment of periodontal disease: Ozonated water, ozonized oil, and gaseous ozone.[3]
In the present study, the effect of ozonated oil (test) and chlorhexidine gel (control) has been evaluated and compared on plaque induce gingivitis to improve the oral health through gingival massage based on the clinical parameters including plaque and gingival scores. In addition to the antimicrobial properties of the oil and gel, gingival massage can mechanically disrupt the biofilm on the teeth, disperses the agents throughout the gingiva, stimulates blood circulation to the gingival tissues, and strengthen its immune response. Furthermore, it is easy to perform, more acceptable and can have a better patient compliance.[4]
MATERIALS AND METHODS
The present study was conducted in the Department of Periodontology, Government Dental College and Hospital, Aurangabad.
A randomized controlled clinical trial was performed. A total of 20 subjects were enrolled for this study based on the following inclusion and exclusion criteria:
Inclusion criteria
Subjects with plaque-induced gingivitis
Age range of 18–65 years old
Subjects exhibited no evidence of clinical attachment loss
Ready to give consent.
Exclusion criteria
Use of antibiotics in the past 3–4 weeks
History of dental treatment/use of mouthwash
Patient with acute necrotizing ulcerative gingivitis, acute herpetic gingivostomatitis, allergic gingivitis, gingivitis associated with skin diseases, gingivitis associated with endocrine-metabolic disturbances, gingivitis associated with hematologic-immunologic disturbances, gingival enlargement associated with medications, gingival tumors were excluded
Individuals with known systemic disease
Pregnant or lactating women.
Diagnosis of plaque induce gingivitis was performed by the clinical assessment which was based on plaque index (Turesky-Gilmore-Glickman modification of Quigely Hein Index, 1970)[5] and gingival index (Loe and Silness, 1963).[6]
The plaque index and gingival index scores were recorded in each individual at baseline (pre) and after 3 weeks (post). A total of 20 subjects with almost equal baseline mean scores were chosen for the study. A simple random sampling was carried out using a lottery method. Group I (study group-ozonated oil) and Group II (control group-chlorhexidine gel) included 10 subjects each. Group I had four males and six females. Group II had six males and four females.
The Study group (Group I) was advised to massage their gingiva with 1 ml of ozonated oil [Figure 1]. The oil base used in ozonated oil, was consist of 60% sesame oil, 30% sunflower oil, 5% castor oil and tuvarak oil each. The control group (Group II) was advised to massage their gingiva with 1 ml of 1% chlorhexidine digluconate gel [Figure 2]. All the subjects were advised to massage their gingiva by using the index finger thoroughly around all teeth in circular motions for 10 min, thrice a day, for 3 weeks. Patients were instructed not to eat or drink for at least 1/2 h after the gingival massage. No specific instructions on other oral hygiene practices (tooth brushing, flossing) were given in order to eliminate the bias which could have arrived because of modifying their oral hygiene practices.
Figure 1.

Ozonated oil
Figure 2.
Chlorhexidine gel
The pre- and post-values of the plaque and gingival index scores within the same group were compared using a paired t-test. The comparison of the pre- and post-values between the two groups was performed using an unpaired t-test. The statistical analysis was performed using GraphPad software, (Inc.7825 Fay Avenue, Suite 230La Jolla, CA 92037 USA).
RESULTS
The pre and post values of plaque index score and gingival index score showed a statistically significant difference in Group I and Group II (P < 0.001).
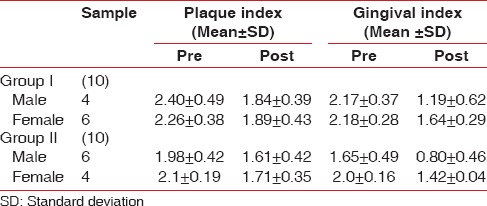
Table 1 shows a comparison of pre and post values of the plaque index scores and gingival index scores, between the study (Group I) and the control group (Group II). There was no statistically significant difference in both the scores indicating that the pre and post mean values of both the groups were almost the same. Table 2 shows that the effect of ozonated oil and chlorhexidine gel was same in males and females belonging to same groups.
Table 1.
A comparison of the pre- and post- values of plaque index and gingival index scores between Group I and Group II
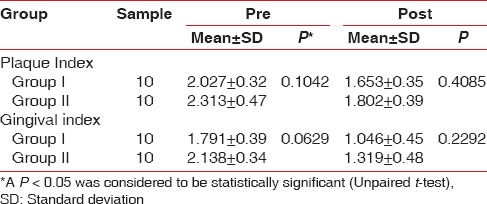
Table 2.
A comparison of plaque index and gingival index scores in males and females
DISCUSSION
Plaque-induced gingivitis is the common form of periodontal disease, results from interactions of the immune system and existing biofilm. The classification of gingival diseases relies on the presence of dental plaque and factors that modify the inflammatory status of gingiva. The modification of plaque-induced gingivitis can occur by local or systemic factors. Local factors include tooth anatomic factors, dental restorations and appliances, root fractures and cervical root resorption, whereas, systemic factors involve the endocrine system, hematologic diseases, drugs, or malnutrition.[7]
Chlorhexidine has emerged as an important oral antiseptic agent and is used as an adjunct to periodontal therapy. It is a broad spectrum antiseptic with antimicrobial effects on Gram-positive as well as Gram-negative bacteria, some viruses, and fungi.[8] However, due to the undesirable effects such as brownish discoloration of teeth, some restorative materials, the dorsum of tongue and taste disturbance, after prolonged use, several alternatives to chlorhexidine have been investigated.[9]
Ozone gas is considered to be an oral antiseptic agent because it is a stronger antimicrobial agent. It kills bacteria, fungi, and viruses and does not induce microbial resistance. Application of ozone in dentistry is based on physical and chemical properties such as antimicrobial action, immunostimulatory action, antihypoxic, biosynthetic, and detoxicating effect.[10] Ozone gas is not recommended for intra-oral use, for safety concern.[11] Ozone gas dissolved in water and oils were and are still commonly used in different fields of dentistry.[12,13,14] Ozonated oils are obtained from the chemical reaction between ozone and unsaturated fatty acids of vegetable oils.[15,16,17,18] They are gaining importance due to its excellent curative results, simple application, long-term effects, and nontoxic nature. Ozone therapy should be contraindicated in pregnancy, glucose-6-phosphate-dehydrogenase deficiency, hyperthyroidism, severe anemia, severe myasthenia, and active hemorrhage.[19]
In the present study, route of administration of ozonated oil and chlorhexidine gel is through gingival massage by which the antiseptic agent disperses throughout the gingiva and gingival margin and it stimulates circulation within gingival tissues, which allows the immune system to fight against the infection.
Besides the valuable properties of ozone gas dissolved in oil, the possible mechanism of action of oil therapy alone could be that the viscosity of the oil probably inhibits bacterial adhesion and plaque co-aggregation. Other possible mechanisms might be that the saponification or the “soap making” process that occurs as a result of alkali hydrolysis of fat, that is, when oils are acted upon by salivary alkalis such as bicarbonates, the soap making process is initiated. Soaps are known to be good cleansing agents because they are effective emulsifiers. Emulsification greatly enhances the surface area of the oil, thereby increasing its cleansing action.[20]
One of the main quantitative methods developed for determining the quality of ozonated oil is peroxide value (Ip). The IP is the number that expresses in milliequivalents of active oxygen the quantity of peroxide contained in 1000 g of the substance (British Pharmacopoeia, 2012). IP is an indicator of how much active oxygen could be released: The higher IP, the stronger antimicrobial effectiveness of ozonated oil. With the IP of 1500 mmol-equiv/kg in ozonated oil was used in this trial.
Singla et al.[21] conducted a study, where chlorhexidine gel, olive oil, sesame oil, and coconut oil was used for gingival massage and concluded that these oils and chlorhexidine gel can be used as valuable preventive agents in maintaining and improving oral health status. Nagayoshi et al.[22] tested the efficacy of three different concentrations of ozone water (0.5, 2, and 4 mg/ml in distilled water) on the time-dependent inactivation of cariogenic, periodontopathogenic and endodontopathogenic microbes (Streptococcus, Porphyromonas gingivalis and endodontalis, Actinomyces actinomycetemcomitans, Candida albicans) in culture and in biofilms and confirm that ozonated water was highly effective in killing of both Gram-positive and Gram-negative micro-organisms. Depending on the dosage, the oral microbes were inactivated after 10 s. Huth et al., in 2007,[23] established a condition under which aqueous ozone exerts inhibitory effects on the nuclear factor-kappa B system, suggesting that it has an anti-inflammatory capacity. A study conducted by Kshitish and Laxman,[24] found higher percentage of reduction in plaque index (12%), gingival index (29%) and bleeding index (26%) using ozone irrigation as compared to chlorhexidine. Patel et al.,[25] found that the adjunctive use of the ozonated olive oil with scaling and root planning resulted in a significant improvement of clinical parameters as well as microbiological parameters over the time and in comparison to the control groups. The ozonated olive oil as monotherapy also showed a significant improvement in clinical parameters as well as microbiological parameters over the time without any documented side effects. However, there was a significant increase in dentinal hypersensitivity following ozonated olive oil as an adjunct to scaling and root planning therapy. Montevecchi et al.[26] found that ozonated oil is a more effective antiseptic than chlorhexidine digluconate and povidone-iodine against S. aureus and the periodontal pathogen P. gingivalis.
Based on all the studies mentioned above and considering the properties of ozone and chlorhexidine, we evaluated and compared the role of ozonated oil and chlorhexidine gel on plaque induced gingivitis in the present study.
Limitation
The groups were unsupervised in the application of therapy; compliance with the requirement to invest 10 min, 3 times a day for 3 weeks was difficult in few patients. Since this study has shown positive results, it can be used as an exploratory study and further research can be carried out on a larger sample. In addition, the lack of significance between the groups could be due to the smaller sample size. The reassessment was performed after 3 weeks based upon the previously conducted similar studies;[27,28,29] longer periods of follow-up can be considered in further research. Due to the possible mechanism of action of oil therapy as mentioned above, in addition to the antimicrobial properties of the oils, they would have a beneficial role in decreasing the plaque and gingivitis. The role of mechanical disruption of the biofilm due to gingival massage may be as relevant as ozonated oils or chlorhexidine gel. Hence, to verify such hypothesis, a group of gingival massaging without any product could be included in the further research.
CONCLUSIONS
Gingival massage with ozonated oils can be used as an effective alternative to gingival massage with chlorhexidine gel against plaque induced gingivitis.
Financial support and sponsorship
Ozone Forum of India and ICPA Health Product Ltd.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jones CG. Chlorhexidine: Is it still the gold standard? Periodontol 2000. 1997;15:55–62. doi: 10.1111/j.1600-0757.1997.tb00105.x. [DOI] [PubMed] [Google Scholar]
- 2.Gupta M, Abhishek Ozone: An emerging prospect in dentistry. Indian J Dent Sci. 2012;1:47–50. [Google Scholar]
- 3.Gupta G, Mansi B. Ozone therapy in periodontics. J Med Life. 2012;5:59–67. [PMC free article] [PubMed] [Google Scholar]
- 4.Hirschfeld I. Gingival massage. J Am Dent Assoc. 1951;43:290–304. doi: 10.14219/jada.archive.1951.0208. [DOI] [PubMed] [Google Scholar]
- 5.Kallar S, Pandit IK, Srivastava N, Gugnani N. Plaque removal efficacy of powered and manual toothbrushes under supervised and unsupervised conditions: A comparative clinical study. J Indian Soc Pedod Prev Dent. 2011;29:235–8. doi: 10.4103/0970-4388.85832. [DOI] [PubMed] [Google Scholar]
- 6.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 7.Mariotti A. Dental plaque-induced gingival diseases. Ann Periodontol. 1999;4:7–19. doi: 10.1902/annals.1999.4.1.7. [DOI] [PubMed] [Google Scholar]
- 8.Moshrefi A. Chlorhexidine. J West Soc Periodontol Periodontal Abstr. 2002;50:5–9. [PubMed] [Google Scholar]
- 9.Gagari E, Kabani S. Adverse effects of mouthwash use. A review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:432–9. doi: 10.1016/s1079-2104(05)80337-3. [DOI] [PubMed] [Google Scholar]
- 10.Srikanth A, Sathish M, Sri Harsha AV. Application of ozone in the treatment of periodontal disease. J Pharm Bioallied Sci. 2013;5(Suppl 1):S89–94. doi: 10.4103/0975-7406.113304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta G, Mansi B. Ozone therapy in periodontics. J Med Life. 2012;5:59–67. [PMC free article] [PubMed] [Google Scholar]
- 12.Ramzy MI, Gomaa HE, Mostafa MI, Zaki BM. Management of aggressive periodontitis using ozonized water. Egypt Med JNRC. 2005;6:229–45. [Google Scholar]
- 13.Katti SS, Chava VK. Effect of Ozonised water on chronic periodontitis – A clinical study. J Int Oral Health. 2013;5:79–84. [PMC free article] [PubMed] [Google Scholar]
- 14.Estrela C, Estrela CR, Decurcio DA, Hollanda AC, Silva JA. Antimicrobial efficacy of ozonated water, gaseous ozone, sodium hypochlorite and chlorhexidine in infected human root canals. Int Endod J. 2007;40:85–93. doi: 10.1111/j.1365-2591.2006.01185.x. [DOI] [PubMed] [Google Scholar]
- 15.Patel PV, Gujjari SK. The morphometrical and histopathological changes which were observed after topical ozone therapy on an exophytic fibrous gingival lesion: A case report. J Clin Diagn Res. 2013;7:1239–43. doi: 10.7860/JCDR/2013/4963.3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Travagli V, Zanardi I, Valacchi G, Bocci V. Ozone and ozonated oils in skin diseases: A review. Mediators Inflamm 2010. 2010 doi: 10.1155/2010/610418. 610418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Travagli V, Zanardi I, Bocci V. Topical applications of ozone and ozonated oils as anti-infective agents: An insight into the patent claims. Recent Pat Antiinfect Drug Discov. 2009;4:130–42. doi: 10.2174/157489109788490271. [DOI] [PubMed] [Google Scholar]
- 18.Azarpazhooh A, Limeback H. The application of ozone in dentistry: A systematic review of literature. J Dent. 2008;36:104–16. doi: 10.1016/j.jdent.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Makkar S, Makkar M. Ozone treating dental infection. Indian J Stomol. 2011;2:256–9. [Google Scholar]
- 20.Asokan S, Rathinasamy TK, Inbamani N, Menon T, Kumar SS, Emmadi P, et al. Mechanism of oil-pulling therapy – In vitro study. Indian J Dent Res. 2011;22:34–7. doi: 10.4103/0970-9290.79971. [DOI] [PubMed] [Google Scholar]
- 21.Singla N, Acharya S, Martena S, Singla R. Effect of oil gum massage therapy on common pathogenic oral microorganisms – A randomized controlled trial. J Indian Soc Periodontol. 2014;18:441–6. doi: 10.4103/0972-124X.138681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagayoshi M, Kitamura C, Fukuizumi T, Nishihara T, Terashita M. Antimicrobial effect of ozonated water on bacteria invading dentinal tubules. J Endod. 2004;30:778–81. doi: 10.1097/00004770-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Huth KC, Saugel B, Jakob FM, Cappello C, Quirling M, Paschos E, et al. Effect of aqueous ozone on the NF-kappaB system. J Dent Res. 2007;86:451–6. doi: 10.1177/154405910708600512. [DOI] [PubMed] [Google Scholar]
- 24.Kshitish D, Laxman VK. The use of ozonated water and 0.2% chlorhexidine in the treatment of periodontitis patients: A clinical and microbiologic study. Indian J Dent Res. 2010;21:341–8. doi: 10.4103/0970-9290.70796. [DOI] [PubMed] [Google Scholar]
- 25.Patel PV, Patel A, Kumar S, Holmes JC. Short-term effect of sub gingival application of topical ozonated olive oil as a monotherapy and an adjunct to scaling and root planing in the treatment of chronic periodontitits patients: A randomized, double blind, controlled, clinical and microbiological study. Minerva Stomatol. 2012;61:1–18. [PubMed] [Google Scholar]
- 26.Montevecchi M, Dorigo A, Cricca M, Checchi L. Comparison of the antibacterial activity of an ozonated oil with chlorhexidine digluconate and povidone-iodine. A disk diffusion test. New Microbiol. 2013;36:289–302. [PubMed] [Google Scholar]
- 27.Asokan S, Kumar RS, Emmadi P, Raghuraman R, Sivakumar N. Effect of oil pulling on halitosis and microorganisms causing halitosis: A randomized controlled pilot trial. J Indian Soc Pedod Prev Dent. 2011;29:90–4. doi: 10.4103/0970-4388.84678. [DOI] [PubMed] [Google Scholar]
- 28.Asokan S, Emmadi P, Chamundeswari R. Effect of oil pulling on plaque induced gingivitis: A randomized, controlled, triple-blind study. Indian J Dent Res. 2009;20:47–51. doi: 10.4103/0970-9290.49067. [DOI] [PubMed] [Google Scholar]
- 29.Asokan S, Rathan J, Muthu MS, Rathna PV, Emmadi P, Raghuraman, et al. Effect of oil pulling on Streptococcus mutans count in plaque and saliva using Dentocult SM Strip mutans test: A randomized, controlled, triple-blind study. J Indian Soc Pedod Prev Dent. 2008;26:12–7. doi: 10.4103/0970-4388.40315. [DOI] [PubMed] [Google Scholar]


