Abstract
Background & objectives:
One of the major strategies being pursued for malaria control by the National Vector Borne Disease Control Programme is the distribution of long lasting insecticidal nets (LLINs) in endemic areas since 2009. Information on durability of insecticidal efficacy and physical integrity of LLINs and community usage at different time intervals of their use is essential to plan net replacements to maintain universal coverage for an effective and sustainable malaria control strategy. Therefore, a study was undertaken to assess these parameters in two malaria endemic districts of the Odisha State.
Methods:
A total of 309 households were selected in 15 villages of two community health centres (CHCs) (Borigumma and Laxmipur) from Koraput district and one (Khairput) from Malkangiri district. Data on net usage were collected during March to July 2014 using semi-structured questionnaires. PermaNet 2.0 were sampled from all households, replaced with new ones, and bioassays were carried out to determine the insecticidal efficacy of LLINs after four and half, four and two years of field use following the standard procedure of World Health Organization.
Results:
LLIN use rate varied from 57.9 to 90.2 per cent in the study CHCs. The annual washing rate per net in Borigumma, Khairput and Laxmipur was 6.6, 3.2 and 4.8, respectively. The LLINs used two years in the field caused 100 per cent mortality and four to four and half years caused below 80 per cent mortality, except one net.
Interpretation & conclusions:
Nearly 20 per cent of the people were out of net coverage and hence the Programme to ensure 100 per cent coverage. The community should adequately be educated so as to increase the net use rate and avoid incorrect washing practices.
Keywords: India, insecticidal efficacy, long lasting insecticidal nets, Odisha, PermaNet 2.0, physical integrity, use rate, washing practice
Plasmodium falciparum the predominant malaria parasite in India, contributed to 65.6 per cent of the total malaria cases in 2014, followed by P. vivax1. Effective and large scale implementation of conventional tools has distinctly brought down the burden of malaria during 2005 to 2013 in India2. The use of insecticide treated mosquito nets (ITN) and curtains has been recognized globally as the key intervention tool for malaria prevention3. A long-lasting insecticidal net (LLIN) is an ITN designed to remain effective for three or more years without requiring re-treatment4. According to World Health Organization (WHO) guidelines, an LLIN must retain effective biological activity against mosquitoes for at least 20 standard laboratory washes and three years of recommended use under field conditions5. In practice, however, these nets are reported to last between 3 to 5 years, and in some instances these have been shown to remain effective even after five years of use6.
WHO has recommended use of 11 different LLIN brands, six insecticides and a long-lasting treatment for treating the nets7. PermaNet 2.0 is a LLIN made of 100 per cent polyester net coated with deltamethrin (55 mg/m2)8 and was evaluated by the WHO Pesticide Evaluation Scheme (WHOPES), and given a full recommendation in 2009 for use in malaria prevention and control7.
Odisha State of India has been afflicted with high incidence of malaria since many decades and in 2013 contributed to nearly 45 per cent of the total falciparum malaria cases recorded in the country1. One of the major strategies being pursued by the National Vector Borne Disease Control Programme (NVBDCP) for malaria control is distribution of LLINs in endemic areas since 20099. In this process, nearly 600, 000 PermaNet 2.0 with 100 denier (40g/m2 fabric weight) have been distributed by NVBDCP during 2009, 2010 and 2012 in Koraput and Malkangiri districts of the State, which are highly endemic for falciparum malaria [Source: Chief District Medical Officer, CDMOs Office, Koraput and Malkangiri]. Updating information on persistence of insecticidal efficacy, and physical integrity of LLINs and community usage practices at different time intervals of field use is essential to select appropriate LLIN tools. A study was, therefore, carried out to assess the insecticidal efficacy, usage pattern, washing practices and physical integrity of PermaNet 2.0 distributed during 2009 and 2012 in Koraput district and 2010 in Malkangiri district, Odisha, India.
Material & Methods
Study area: The study was carried out in Borigumma and Laxmipur Community Health Centres (CHCs) of Koraput district and in Khairput CHC of Malkangiri district, from March to July 2014. One sub-centre (SC) in each of the three CHCs was selected for the study. The selected SCs were Sargiguda, Kadamguda and Panchada of Borigumma, Khairput and Laxmipur CHCs, respectively. The LLINs were distributed in Sargiguda in November 2009, Kadamguda in May 2010 and Panchada in June 2012 (Source: CDMOs Office, Koraput and Malkangiri) at the rate of one net for 2.5 persons as per the NVBDCP guidelines9. Five villages were randomly selected from each of the three SCs for conducting sociological survey and bioassay. The villages selected were Sargiguda, Badadubuli, Sandubuli, Dumarjodi and Moniguda of Sargiguda SC, Pokanaguda, Kenduguda, Kadamguda, Rauliguda and Khemaguru of Kadamguda SC and Panchada, Alachi, Kunjariguda, Bamankot and Maligaon of Panchada SC. There were 1624 households in the 15 villages with a total population of 7,178. Villagers in the study area preferred to sleep in the open places available in front of their houses during summer months and during rainy and winter months they were sleeping indoors. Anopheles fluviatilis and An. culicifacies are the known malaria vectors in this area10. Studies conducted in the study area showed that An. fluviatilis was susceptible to synthetic pyrethroids (SP) while An. culicifacies developed resistance to this insecticide (unpublished observation). The annual parasite incidence (API) of Borigumma, Khairput and Laxmipur CHCs was 23.9 in 2009, 38.7 in 2009 and 90.8 in 2011, respectively (Source: CDMOs Office, Koraput and Malkangiri). Ethical clearance was obtained from the Ethics Committee of the Vector Control Research Centre, Puducherry. Written informed consent was obtained from the heads of households selected for the study.
Sample size and design: The sample size for the monitoring surveys was calculated based on the estimated percentage of households sleeping under LLINs during the previous night i.e. use rate (40 per cent) with an error margin of 10 per cent and 95 per cent confidence interval. Since, nets were expected to be damaged over a period of their use; the sample size was adjusted for an attrition rate of 15 per cent, 10 per cent and 7.5 per cent in Borigumma, Khairput and Laxmipur CHC, where nets were distributed four and half, four and two years ago, respectively. Thus, a total of 106, 100, and 103 households were selected for assessing net use rates in the villages of the three CHCs, respectively.
A two-stage cluster sampling design was followed for selecting villages as the stage 1 sampling unit and households as the stage 2 sampling unit. In stage 1, a sample of five villages was selected from each CHC with probability proportion to the number of households in the respective CHC. In stage 2, in each selected village, households were sampled in proportion to the number of households available in the village. The household members were interviewed by making door-to-door visits to assess the availability of nets in the households at the time of survey, net utilization pattern/frequency of use (including early morning observations of net use), mode and number of washes and type of detergent used, drying practice, physical integrity and attrition rate of the net (size and number of holes). The household head or an adult member of the family was interviewed using pre-tested semi-structured questionnaires which combined a pre-determined set of open questions (questions that promote discussion) with the opportunity for the interviewer to probe specific aspect or responses further.
Physical integrity of nets (e.g. number of holes and their size) was determined by draping the nets over a frame and counting the number of holes and estimating their sizes according to the location on the net (roof, upper side panel, lower side panel). The LLINs, found with holes with their estimated size, were categorized into four size-groups: size 1 (hole smaller than that will allow a thumb to pass through), size 2 (larger hole but will not allow closed fist to pass through), size 3 (hole bigger than a closed fist) and size 4 (hole bigger than a head)5. The two indicators i.e. the proportion of LLINs with holes and the hole index were calculated. The proportionate Hole Index (pHI) which is the measure of physical integrity was also calculated to find out the number of nets in “serviceable” condition11. During the survey, data on the loss of LLINs due to routine wear and tear leading to net disposal (attrition1), selling or stealing (attrition 2) and use for other than intended purposes (attrition 3) were collected.
Biological assays for insecticide efficacy evaluation: On the day of sociological survey, net samples were collected for conducting bioassay following the WHO procedure5. In each village, six nets selected randomly were withdrawn for bioassays, thus in total 90 PermaNet 2.0 were evaluated for insecticide efficacy. The nets withdrawn were replaced with new ones. From the five positions (1 to 5) of nets as specified by WHO Pesticide Evaluation Scheme (WHOPES)5, five net pieces, each 25 × 25 cm in size, were cut using sharp scissors from each of the 90 selected LLINs and used for bioassays. Since, the density of An. fluviatilis was low in the study area after the introduction of LLINs during 2009 to 2013, adequate number could not be collected to conduct the bioassays. Therefore, the laboratory reared female An. stephensi (susceptible to deltamethrin) mosquitoes were used for the bioassays. Bioassay was done on all the five net pieces placing one WHO cone on each netting sample. Five laboratory-bred 2-5 days old, non-blood fed females of An. stephensi were introduced into each cone and exposed for three minutes. The test was done twice on each net piece. Due to lack of sufficient numbers of laboratory reared female An. stephensi, 100 mosquitoes could not be exposed on each net. Thus, in total 50 mosquitoes were exposed on each net and altogether 4500 mosquitoes (90 nets x 5 positions per net x 5 mosquitoes per piece x 2 tests on each piece) on 90 nets. After the exposure, mosquitoes were removed gently from the cones and kept separately in plastic cups provided with cotton-pads moistened with 10 per cent glucose solution. Mortality was recorded after 24 h. Mosquitoes exposed to untreated nets were used as controls. The bioassays were conducted at 25±2 °C and 75±10 per cent relative humidity (RH). LLIN performance was assessed using the cone bioassay results. If mortality in the bioassays was >80 per cent, the net was considered to be efficacious.
Data analysis: Categorical variables were compared between the three groups (period of net use in the field: 2, 4, and 4.5 years) using Chi-square test. For percentage (rates), exact binomial distribution with 95% confidence intervals were used. Regression analysis was done to examine the relation beween percentage mortality and number of times net washed along with period of net use. Data analysis was performed using EPI DAT 3.1 software and Microsoft Excel 2013 (MS Office 2013, USA).
Results
Distribution and availability of nets: A total of 1406 persons (n=7178, i.e. the total population of 15 villages) from the 309 households (19 per cent of 1624, i.e. total household of 15 villages) selected in the 15 villages of the three CHCs consented to participate in the study. In total, 446 LLINs were distributed to the 309 households. The distribution rate was one LLIN for 2.8 to 4 persons in different CHCs with an average of one net for 3.2 persons. During the survey, a total of 102 (82.9 % of 123), 124 (73.3 % of 169) and 126 (81.8 % of 154) LLINs were physically present in the study villages of Borigumma, Khairput and Laxmipur CHCs, respectively (Table I).
Table I.
Details of study villages, number of long-lasting insecticidal nets (LLINs) provided, physically available during the survey and usage rate

Usage rate of LLINs: Data from the household surveys pertaining to any one sleeping under the LLIN on the previous night showed that 90.2, 68.5 and 57.9 per cent of the LLINs were under use in Borigumma (distributed four and half years before), Khairput (four years before) and Laxmipur (two years before) CHCs, respectively (Table I). The use rate was significantly different between the three CHCs (P<0.001). Further comparison between the CHCs showed that the net use rate was significantly higher in Boriguma CHC than that in Khairput, and Laxmipur (P<0.001) CHCs. The results suggested that the net use rate increased with longer period of net use.
Washing practice of LLINs: In Borigumma CHC, 76.1 per cent of the respondents reported washing their nets >20 times. Whereas, in Khairput and Laxmipur CHCs, 4.8 and 8.3 per cent reported washing >20 times. The annual washing rates per net in Borigumma, Khairput and Laxmipur were 6.6, 3.2 and 4.8, respectively. All (100%) the nets in the study villages were reported to be washed with cold water and dried in sun light after each wash. In the study villages of all the three CHCs, a majority of the households (86 to 100%) washed their nets with commercially available detergent powder.
Physical integrity of LLINs: During the survey, of the 446 LLINs distributed, 102, 124 and 126 (a total 352) LLINs were inspected for physical integrity and, only 14.7, 24.2 and 57.1 per cent were without holes in Borigumma, Khairput and Laxmipur CHCs, respectively. The total number of holes of sizes 1, 2, 3 and 4 in the nets in the three CHCs are presented in Table II. The mean hole index of LLINs in Borigumma, Khairput and Laxmipur CHCs was 1896.2, 681.7 and 543.4, respectively (Table II). The total number of nets with pHI 0-64, 65-642 and 643+ in Borigumma, Khairput and Laxmipur CHCs are presented in Table III. The result showed that 35.6, 67.0 and 77.8 per cent nets in Borigumma, Khairput and Laxmipur CHCs, respectively were in serviceable condition among the nets with holes.
Table II.
Physical integrity of LLIN in the study area

Table III.
The proportionate hole index of LLIN in the study area

Attrition rate: The attrition rate (percentage of LLINs lost by all means) was 17, 26.6 and 18.2 per cent in Borigumma, Khairput and Laxmipur CHCs, respectively.
Bioefficacy of LLINs: The range of washing frequency of bioassay nets of Borigumma, Khairput and Laxmipur was 12 to 42, 2 to 25 and 2 to 30, respectively. In Borigumma CHC, of the 30 nets tested for bioassay, 27 were washed >20 times and the remaining three were washed < 20 times during 4.5 years of field use. The bioassay results showed that all the 30 nets tested caused <80 per cent mortality. In Khairput CHC, among the 30 nets tested through bioassay, only 13 were washed >20 times and 17 <20 times. Except one net (showed 80 per cent mortality), which was washed six times during four years of field use, all 29 nets gave <80 per cent mortality. In Laxmipur CHC, of the 30 nets tested through bioassays, seven were reported to be washed >20 times and 23 <20 times during the two years of field use. All the 30 nets tested were found efficacious (>80 per cent mortality) (Table IV). Regression analysis revealed that the corrected mortality declined with the reported number of washes. (Figure, r=-0.74 and P= 0.002).
Table IV.
Results of bioassays
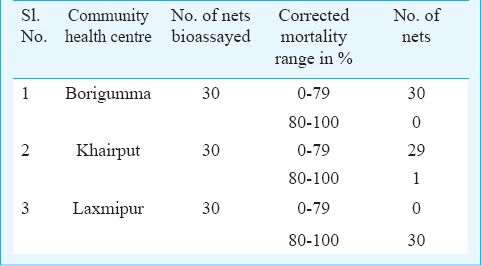
Figure.
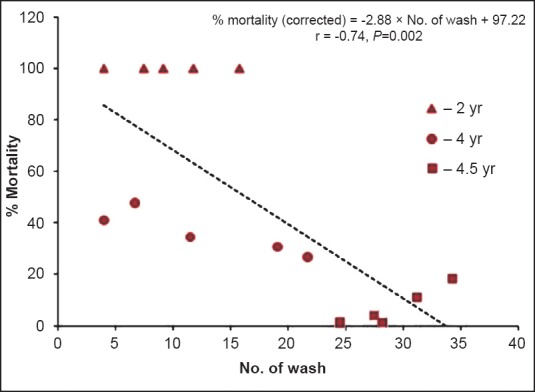
Mortality (corrected) of An. stephensi in relation to number of times net washed along with period of net use. Dotted line is the least square regression line relating percentage mortality with number of times net washed.
Discussion
The current study was aimed to find out the coverage, usage rate, washing practices, physical integrity and retention of insecticidal efficacy of LLINs distributed four and half, four and two years before in tribal areas in Odisha State. The study showed that although all the surveyed households received LLINs, on an average only 79.3 per cent people in the study areas were covered. As per WHO recommendations, for mass campaigns, one LLIN should be distributed for every two persons at risk of malaria12. Deviating from the national guidelines on LLIN distribution, i.e. average one net per 2.5 persons in a targeted household9, actually one net was given per 2.8 to 4.0 persons (average 3.2 persons). Thus, nearly 20 per cent of the people were out of net coverage and more vulnerable to malaria infection that would favour for a persistent transmission of malaria in the area. This was a key issue identified, and hence the programme must ensure 100 per cent net coverage. Earlier studies conducted elsewhere pointed out that greater reductions of malaria morbidity among children could be achieved with more coverage of LLINs13,14.
Another important observation of the current study was that, nearly three fourth (73%) of the households possessed LLINs in all the study villages after two to four and half years of distribution indicating that the people were aware of the importance of mosquito nets. However, the percentage of LLINs used during the previous night was 57.9 in Laxmipur, 68.5 in Khairput and 90.2 in Borigumma. The low use rate in Khairput and Laxmipur CHCs would adversely affect the benefit of interrupting malaria transmission. The reason for higher usage rate of LLINs in Borigumma CHC in comparison to Khairput and Laxmipur CHCs could be due to the better access to communication and relatively higher level of literacy among the tribes, Paraja, Bhatra and Amanatya, living in Borigumma, who are more health conscious. The Kandha and Paraja tribes in Laxmipur and Bonda and Didayi tribes in Khairput are socio-economically poor in comparison to tribes living in Borigumma15. A similar study carried out in central India showed that about 33 to 40 per cent of households reported sleeping under LLIN seasonally (generally during post monsoon months) but every night16.
The limitation of the current study was that the survey was carried out in summer when ambient temperature was above 40 °C. In order to avoid such a hot climate, people preferred to sleep outside the houses without using nets. In the study CHCs, in rainy season, people slept inside the net during night time. However, in winter season, most people slept near fire without using nets to get relief from the cold. Sometimes, because of low socio-economic conditions of the tribes, they go to forest for collection of fire woods and spend the night in the forest itself during winter and summer months. This was another area drawing the attention of the Programme that should, through appropriate information, education and communication (IEC) package, motivate the people to use nets regularly and in all seasons to interrupt the transmission. The manufacturers of LLINs should also consider this aspect and make the nets more user friendly, facilitating more aeration during summer season. The annual parasite incidence (API) in Borigumma CHC, where LLINs distribution was done during 2009, reduced from 23.2 (2009) to 4.3 (2013). In Khairput CHC, with LLINs were distributed in 2010, the API decreased from 38.7 in 2009 to 14.6 in 2013. Similarly, in Laxmipur CHC, where LLINs were distributed in 2012, there was a decrease in API from 90.8 in 2011 to 35.3 in 2013 (Source: CDMOs Office, Koraput and Malkangiri). Marked reduction of malaria incidence was noted in each study area after LLINs distribution. The Programme should ensure universal coverage and high usage of LLINs, and strengthen early diagnosis and appropriate treatment to further reduce the malaria incidence.
The washing frequency of the nets recorded in the current study almost met the manufacturer recommendation of 20 washes. The annual washing rate of LLIN in Borigumma was relatively higher than Khairput and Laxmipur. However, the data on washing frequency generated in the current study may not be accurate considering the low literacy level and the longer recall period, and this could be another limitation of the current study. All the nets were reported to be washed with running cold water and dried in sun light. Drying in shade would be the appropriate method to preserve the insecticide in the nets after washing. Such information need to be communicated to the beneficiaries at the time of distribution to get full benefit of the nets. Washing nets with commercially available detergent powder was the general practice (90%) in the study area.
As expected, in Laxmipur area, where LLINs were distributed two years ago, 57.1 per cent of the nets were without holes and 77.8 per cent of the nets were in serviceable condition among the nets with holes, whereas in Khairput CHC, where nets were distributed four years ago, only around 24.2 per cent of the nets are without holes and 67 per cent of the nets were in serviceable condition among the nets with holes. In case of Borigumma CHC, where nets were distributed four and half years ago, only around 14.7 per cent of the nets were without holes and 35.6 per cent of the nets were in serviceable condition. This showed that the durability of 100 denier PermaNet 2.0 distributed by the NVBDCP, may last for three years.
An. stephensi used for bio-efficacy test is not the target vector in the study area. This was another limitation of the study. Further, contrary to guidelines requirements 100 mosquitoes were not exposed per LLIN tested due to want of laboratory reared An. stephensi. Only 50 mosquitoes were exposed to each net for conducting bioassay. The LLINs supplied four and half (Borigumma) or four years (Khairput) ago had no desired insecticidal effect as the mortality in cone bioassays was <80 per cent except one net. Even if 10 per cent LLINs in Borigumma and 56.7 per cent LLINs in Khairput were washed <20 times during four and half and four years of household use, the mortality observed with these nets was <80 per cent indicating that the duration of use and washing frequency possibly affected the insecticidal efficacy of LLIN. But, people were still using such nets without the desired benefit. To overcome this, such serviceable nets could be re-treated for further use or replaced with new LLINs. In Laxmipur CHC, the bioassay mortality of An. stephensi against all the LLINs was 100 per cent indicating retention of insecticidal efficacy by the nets after two years of field use and thereby meeting the WHOPES efficacy criteria (≥80% mortality at 24 h). However, the insecticidal efficacy of these LLINs needs to be confirmed after three years of use in the field. There are reports of >80 per cent mortality of Anopheles mosquitoes on exposure to 23 times washed PermaNet 2.017 and >97 per cent mortality of anophelines when exposed to 21 times-washed PermaNet 2.018. Similar to the earlier studies, the current study also showed a high mortality rate (100%) after 20 washes and after two years of field use.
After introduction of LLINs in a phased manner from 2009 in Malkangiri and Koraput districts, malaria cases have come down by 60 to 80 per cent during the last four years1. The Programme should distribute LLINs to those who are not yet covered and replace LLINs that are no longer serviceable. For practical reasons, the Programme may consider mass distribution every three years targeting one LLINs per two persons. Behaviour change communications should be intensified to ensure high usage rate and reduced attrition rate of LLINs. In most of the tribal villages, Upper Primary and High Schools are functioning. Empowering the students of these schools in propagating the message of appropriate method of net use, washing and drying would help ensuring proper use of nets and thereby controlling falciparum malaria19 in these areas. In addition, direct motivation of the community should be done using appropriate health education tools to enhance the net use rate and avoid incorrect washing practices of nets.
Acknowledgment
The authors thank Dr P. Jambulingam, Director, Vector Control Research Centre, Puducherry for his constant support to carry out the study, and District Malaria Officer of Koraput and Malkangiri districts for sharing the information on malaria incidences and distribution of LLINs. The technical assistance rendered by the staff of VCRC Field Station, Koraput, Odisha is duly acknowledged.
Footnotes
Conflicts of Interest: None.
References
- 1.National Vector Borne Disease Control Programme. Malaria situation in India. National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India. 2014. [accessed on June 30, 2015]. Available from: http://nvbdcp.gov.in/malaria-new.html .
- 2.Bhatia R, Rastogi RM, Ortega L. Malaria successes and challenges in Asia. J Vector Borne Dis. 2013;50:239–47. [PubMed] [Google Scholar]
- 3.Lengeler C. Insecticide-treated bednets and curtains for preventing malaria. Cochrane Database Syst Rev. 2000;(2):CD000363. doi: 10.1002/14651858.CD000363. [DOI] [PubMed] [Google Scholar]
- 4.Geneva: World Health Organization; 2012. World Health Organization. World Malaria Report 2012. [Google Scholar]
- 5.Geneva: World Health Organization; 2013. World Health Organization. Guidelines for laboratory and field-testing of long-lasting insecticidal nets. WHO/HTM/NTD/WHOPES/2013.1. [Google Scholar]
- 6.Sreehari U, Raghavendra K, Rizvi MM, Dash AP. Wash resistance and efficacy of three long-lasting insecticidal nets assessed from bioassays on Anopheles culicifacies and Anopheles stephensi. Trop Med Int Health. 2009;14:597–602. doi: 10.1111/j.1365-3156.2009.02252.x. [DOI] [PubMed] [Google Scholar]
- 7.Geneva: World Health Organization; 2014. [accessed on May 18, 2015]. World Health Organization. WHO recommended insecticide products for treatment of mosquito nets for malaria vector control. Available from: http://who.int/WHOPES/recommendations/en/ [Google Scholar]
- 8.PermaNet 2.0. [accessed on June 12, 2014]. Available from: http://www.vestergaard.com/ permanet-2-0.
- 9.National Vector Borne Disease Control Programme. Operational manual for implementation of malaria programme 2009. Directorate of National Vector Borne Disease Control Programme, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India. [accessed on March 21, 2015]. Available from: http://nvbdcp.gov.in/Doc/malariaoperational-manual-2009.pdf .
- 10.Sahu SS, Gunasekaran K, Raju HK, Vanamail P, Pradhan MM, Jambulingam P. Response of malaria vectors to conventional insecticides in the southern districts of Odisha State, India. Indian J Med Res. 2014;139:294–300. [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. WHO guidance note for estimating the longevity of long-lasting insecticidal nets in malaria control. September 2013. [accessed on May 18, 2015]. Available from: http://www.who.int/malaria/publications/atoz/who_guidance_longevity_llins.pdf .
- 12.World Health Organization. WHO recommendations for achieving universal coverage with long-lasting insecticidal nets in malaria control. September 2013. (revised March 2014) [accessed on May 18, 2015]. Available from: www.who.int/malaria/publications/atoz/who_recommendations_universal_ coverage_ llins.pdf .
- 13.Fullman N, Burstein R, Lim SS, Medlin C, Gakidou E. Nets, spray or both? The effectiveness of insecticide-treated nets and indoor residual spraying in reducing malaria morbidity and child mortality in sub-Saharan Africa. Malar J. 2013;12:62. doi: 10.1186/1475-2875-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smithuis FM, Kyaw MK, Phe UO, Vander Broek I, Katterman N, Rogers C, et al. The effect of insecticide-treated bed nets on the incidence and prevalence of malaria in children in an area of unstable seasonal transmission in western Myanmar. Malar J. 2013;12:363. doi: 10.1186/1475-2875-12-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.District statistical hand book, Koraput, Government of Odisha. Bhubaneswar: DES; 2011. Directorate of Economics & Statistics (DES), Odisha, Bhubaneswar. [Google Scholar]
- 16.Bhatt RM, Sharma SN, Uragayala S, Dash AP, Kamaraju R. Effectiveness and durability of Interceptor® long-lasting insecticidal nets in a malaria endemic area of central India. Malar J. 2012;11:189. doi: 10.1186/1475-2875-11-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kroeger A, Skovmand O, Phan QC, Boewono DT. Combined field and laboratory evaluation of a long-term impregnated bednet, PermaNet 2.0. Trans R Soc Trop Med Hyg. 2004;98:152–5. doi: 10.1016/s0035-9203(03)00038-5. [DOI] [PubMed] [Google Scholar]
- 18.Lindblade KA, Dotson E, Hawley WA, Bayoh N, Williamson J, Mount D, et al. Evaluation of long-lasting insecticidal nets after 2 years of household use. Trop Med Int Health. 2005;10:1141–50. doi: 10.1111/j.1365-3156.2005.01501.x. [DOI] [PubMed] [Google Scholar]
- 19.Sahu SS, Gunasekaran K, Vanamail P, Jambulingam P. Persistent foci of falciparum malaria among tribes over two decades in Koraput district of Orissa state, India. Malar J. 2013;12:72. doi: 10.1186/1475-2875-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]


