Abstract
To report a patient with juxtapapillary choroidal osteoma (CO) with serous retinal detachment (SRD) not associated with choroidal neovascularization (CNV) who was successfully treated with a single intravitreal injection of bevacizumab. A 20-year-old woman presented with decreased vision in her right eye. Ultrasonography, fundus autofluorescence, fluorescein angiography (FA) and optical coherence tomography (OCT) were performed. She was diagnosed with juxtapapillary CO with SRD in the absence of CNV. The treatment involved a single intravitreal injection of bevacizumab. Visual acuity (VA) was 20/100 pre-injection which was dramatically improved to 20/20 one week after the injection without any additional treatment. Fundus examination and OCT one week after the injection revealed complete absorption of the subretinal fluid (SRF) in the macula. Eighteen months after the injection, vision remained stable and she did not show re-accumulation of SRF in her right eye. Intravitreal injection of bevacizumab may be effective in managing CO associated with SRF without CNV.
Keywords: Choroidal Osteoma, Intravitreal Bevacizumab, Serous Retinal Detachment
INTRODUCTION
Choroidal osteoma (CO) is a rare ossifying tumor typically diagnosed in young women. Ophthalmoscopic characteristics of the tumor include a slightly elevated, white to cream or orange lesion with sharp geographic borders located in the peripapillary or macular choroid.[1,2] The origin of the tumor is believed to be choristomatous; however, despite its benign nature, visual acuity can be affected in these patients due to lesion enlargement, decalcification, atrophy of overlying retina or choroidal neovascularization (CNV) which might lead to subretinal fluid (SRF) accumulation and hemorrhage.[3,4] Most patients develop CNV associated with SRF and hemorrhage, although SRF and serous retinal detachment may occur in the absence of CNV.[5,6] Recent studies using orbital computed tomography (CT) have revealed CO as well-defined radio-opaque lesions with bony density at the choroidal level. In addition, fluorescein angiography (FA) shows a zone of diffuse fluorescence whereas optical coherence tomography (OCT) indicates the presence of a highly reflective lesion.[7] Injection of intravitreal bevacizumab has been suggested as an efficient method to manage CO associated with CNV.[8,9,10,11]
Herein, we describe a 20-year-old woman with CO complicated by serous retinal detachment (SRD) without CNV who demonstrated an impressive positive response to intravitreal bevacizumab injection alone.
CASE REPORT
A 20-year-old woman was referred to Feiz Eye Hospital, Isfahan, Iran, with decreased vision in her right eye lasting for a week. She did not mention any relevant medical and surgical histories or a past family history of ophthalmic diseases. Examination revealed best corrected visual acuity (BCVA) of 20/100 in her right eye and 20/20 in the left one. Slit lamp examination in both eyes was within normal limits. Fundus examination of the right eye revealed a yellow oval lesion with well-defined margins in the juxtapapillary area. The size of the lesion was about 2 disc areas. In addition, we observed subtle elevation of the retina in the maculopapillar area and fovea. Subretinal hemorrhage or exudates and subretinal membrane were not observed. Fundus examination of her left eye provided similar results to those in the right eye, however the size of the lesion was smaller and the retina was not elevated [Figure 1a].
Figure 1.
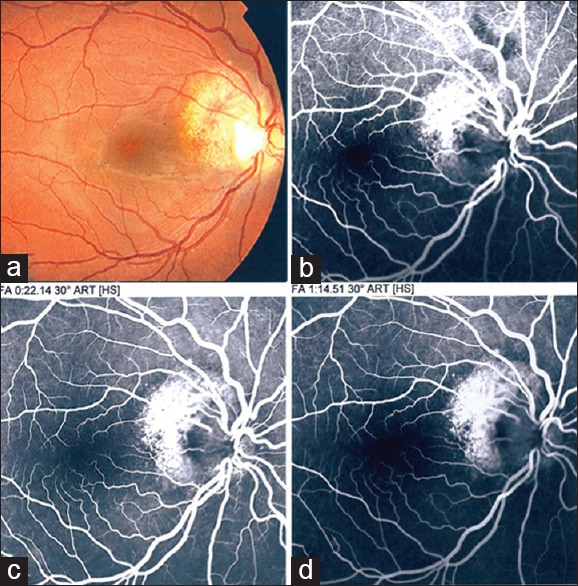
(a) Fundus photograph shows a well-demarcated yellow lesion in the juxtapapillary area of the right eye before injection. (b-d) Fundus fluorescein angiogram of the right eye before injection. Early hyperfluorescence and late staining of the lesion reveals the lack of leakage.
A and B-scan ultrasonography of the right eye showed a hyperechoic lesion of about 4 × 3.5 mm in diameter and 1 mm in thickness adjacent to the superotemporal disc margin. The shadow behind the lesion was remarkable. Ultrasonography also showed a highly reflective small lesion temporal to the optic nerve with a distinct shadow in the left eye. Autofluorescence imaging using HRA2 (Heidelberg Engineering, Heidelberg, Germany) revealed the presence of granular hypoautofluoresence in the peripheral and central parts of the lesions in both eyes. FA showed early hyperfluorescence with late staining of the lesions in both eyes. The late frame angiogram showed no increase in size or intensity of hyperfluorescence, suggesting lack of leakage [Figure 1b-d].
OCT of the right eye revealed an elevated retinal pigmented epithelium (RPE) just near the disc, with no subretinal neovascular membrane. Additionally, we observed elevation of the retina with SRF in the maculopapillar area along with foveal detachment. OCT of the left eye showed hyper-reflectivity of the lesion near the disc. No remarkable features were observed in any other anatomical structures [Figure 2a].
Figure 2.
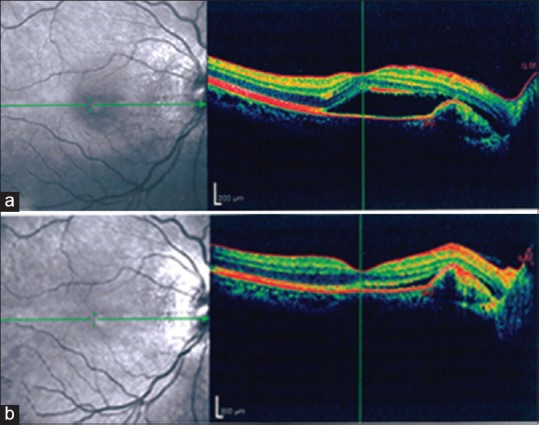
Optical coherence tomography (OCT) of the right eye before and after treatment. (a) OCT shows accumulation of subretinal fluid (SRF) before bevacizumab injection. (b) OCT one week post bevacizumab injection shows complete absorption of the SRF and a flat retina.
Juxtapapillary CO in both eyes was diagnosed based on fundus examination and ultrasonography findings. In addition, OCT revealed SRF accumulation in the fovea, and fluorescein angiography ruled out choroidal neovascularization in the right eye.
Following this diagnosis, the patient was provided with information regarding the risks and benefits of treatment, including intravitreal bevacizumab injection. After informed written consent was obtained, a single dose of 1.25 mg of bevacizumab was injected into the vitreous cavity of her right eye. One week after the procedure, we observed a remarkable response: Vision of the right eye had improved to 20/20 and the retina had completely reattached. One week post-injection, OCT revealed complete absorption of subretinal fluid in the macular area and the retina showed a completely flat configuration [Figure 2b]. At final follow-up examination 18 months after the injection, visual acuity remained 20/20 and the lesion was not active.
DISCUSSION
CO is an uncommon benign tumor, more frequent in women than men, composed of mature osseous tissue in the choroid.[12] This lesion tends to occur unilaterally, although in one in four cases, the tumor develops in both eyes. Murthy et al described a 15-year-old girl with decreased vision because of bilateral CO which led to optic atrophy.[13] In most previously reported cases, CNV was the main cause of visual loss; however, some researchers have suggested the presence of SRD as the main cause of reduced vision in eyes without CNV.[4]
Although the best treatment strategy for management of CO without CNV is still debatable, two different approaches are recommended: A) light-intensity focal laser photocoagulation for resolution of subretinal fluid,[14] and B) injection of intravitreal bevacizumab, a vascular endothelial growth factor (VEGF) inhibitor.[4] Herein, we report the results of intravitreal bevacizumab injection in a patient with decreased vision due to CO not associated with CNV. In this case, the patient responded remarkably well to the injection without any additional treatment. In the five cases of CO without definite signs of CNV reported by Song et al (2009), the best post-injection BCVA was 0.9 after repeated treatment. In contrast, our patient showed complete improvement, from 20/200 to 20/20 after only one injection. This is the first report of complete improvement in a case of CO not associated with CNV. Our patient demonstrated complete absorption of SRF and recovery of VA after only a single injection without the need for additional treatments.
Recent developments include the use of transpupillary thermotherapy, which could be successful in combination with intravitreal injection in cases where CO is not associated with CNV; however, so far, none of the cases reported have shown such a dramatic VA improvement. The period between injection and visual improvement is also very important. In the patient reported herein, improvement was observed as early as seven days post-injection which is a remarkably shorter time interval compared with previously reported cases.[4]
Choroidal neovascularization can also lead to VA loss in association with CO. Ahmadieh et al reported a young female patient with decreased VA in her right eye. After a diagnosis of juxtafoveal CNV, an intravitreal injection of 1.25 mg of bevacizumab was administered, resulting in dramatic improvement of VA and resolution of metamorphopsia.[3] As previously discussed, in cases of CO associated with CNV, a single intravitreal injection of bevacizumab may be an efficient alternative to address decreased vision and to prevent further progression of the lesion.[3,15] Ranibizumab, another VEGF inhibitor used for neovascular age-related macular degeneration, has also been recommended to manage CNV in patients with CO.[16,17]
Bevacizumab injection can decrease choroidal vascular permeability by inhibiting VEGF. Because of retinal pigmented epithelial degeneration, Bevacizumab may penetrate more in subretinal space and affect better.[3,4]
In summary, the administration of intravitreal bevacizumab may be a successful treatment modality for patients with CO in the absence of CNV. Longer follow-up is necessary to confirm the long-term effectiveness of this treatment.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Pandey N, Guruprasad A. Choroidal osteoma with choroidal neovascular membrane: Successful treatment with intravitreal bevacizumab. Clin Ophthalmol. 2010;4:1081–1084. doi: 10.2147/OPTH.S13730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shields CL, Shields JA, Augsburger JJ. Choroidal osteoma. Surv Ophthalmol. 1988;33:17–27. doi: 10.1016/0039-6257(88)90069-0. [DOI] [PubMed] [Google Scholar]
- 3.Ahmadieh H, Vafi N. Dramatic response of choroidal neovascularization associated with choroidal osteoma to the intravitreal injection of bevacizumab (Avastin) Graefes Arch Clin Exp Ophthalmol. 2007;245:1731–1733. doi: 10.1007/s00417-007-0636-z. [DOI] [PubMed] [Google Scholar]
- 4.Song JH, Bae JH, Rho MI, Lee SC. Intravitreal bevacizumab in the management of subretinal fluid associated with choroidal osteoma. Retina. 2010;30:945–951. doi: 10.1097/IAE.0b013e3181c720ca. [DOI] [PubMed] [Google Scholar]
- 5.Aylward GW, Chang TS, Pautler SE, Gass JD. A long-term follow-up of choroidal osteoma. Arch Ophthalmol. 1998;116:1337–1341. doi: 10.1001/archopht.116.10.1337. [DOI] [PubMed] [Google Scholar]
- 6.Shields CL, Sun H, Demirci H, Shields JA. Factors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes with choroidal osteoma. Arch Ophthalmol. 2005;123:1658–1666. doi: 10.1001/archopht.123.12.1658. [DOI] [PubMed] [Google Scholar]
- 7.Ascaso FJ, Villén L. Fundus autofluorescence imaging findings in choroidal osteoma. Retina. 2011;31:1004–1005. doi: 10.1097/IAE.0b013e31820d37a6. [DOI] [PubMed] [Google Scholar]
- 8.Avery RL, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA, Giust MJ. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113:363–372.e5. doi: 10.1016/j.ophtha.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 9.Bashshur ZF, Bazarbachi A, Schakal A, Haddad ZA, El Haibi CP, Noureddin BN. Intravitreal bevacizumab for the management of choroidal neovascularization in age-related macular degeneration. Am J Ophthalmol. 2006;142:1–9. doi: 10.1016/j.ajo.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 10.Costa RA, Jorge R, Calucci D, Cardillo JA, Melo LA, Jr, Scott IU. Intravitreal bevacizumab for choroidal neovascularization caused by AMD (IBeNA Study): Results of a phase 1 dose-escalation study. Invest Ophthalmol Vis Sci. 2006;47:4569–4578. doi: 10.1167/iovs.06-0433. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen QD, Shah S, Tatlipinar S, Do DV, Anden EV, Campochiaro PA. Bevacizumab suppresses choroidal neovascularisation caused by pathological myopia. Br J Ophthalmol. 2005;89:1368–1370. [PMC free article] [PubMed] [Google Scholar]
- 12.Gass JD, Guerry RK, Jack RL, Harris G. Choroidal osteoma. Arch Ophthalmol. 1978;96:428–435. doi: 10.1001/archopht.1978.03910050204002. [DOI] [PubMed] [Google Scholar]
- 13.Murthy R, Das T, Gupta A. Bilateral choroidal osteoma with optic atrophy. J AAPOS. 2010;14:438–440. doi: 10.1016/j.jaapos.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 14.Browning DJ. Choroidal osteoma: Observations from a community setting. Ophthalmology. 2003;110:1327–1334. doi: 10.1016/S0161-6420(03)00458-5. [DOI] [PubMed] [Google Scholar]
- 15.Song WK, Koh HJ, Kwon OW, Byeon SH, Lee SC. Intravitreal bevacizumab for choroidal neovascularization secondary to choroidal osteoma. Acta Ophthalmol. 2009;87:100–101. doi: 10.1111/j.1600-0420.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- 16.Kourlas H, Abrams P. Ranibizumab for the treatment of neovascular age-related macular degeneration: A review. Clin Ther. 2007;29:1850–1861. doi: 10.1016/j.clinthera.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 17.Song MH, Roh YJ. Intravitreal ranibizumab in a patient with choroidal neovascularization secondary to choroidal osteoma. Eye (Lond) 2009;23:1745–1746. doi: 10.1038/eye.2008.313. [DOI] [PubMed] [Google Scholar]


