Abstract
To describe the clinical and optical coherence tomography (OCT) characteristics of ischemic maculopathy in two patients with acquired immunodeficiency syndrome (AIDS). Two patients with AIDS and cytomegalovirus (CMV) retinitis developed ischemic maculopathy. Both patients presented with central visual loss and active granular CMV retinitis. The presence of opacification of the superficial retina in the macular area and intraretinal edema suggested the diagnosis. Fluorescein angiography changes were similar in the two cases with enlargement of the foveal avascular zone and late staining of juxtafoveal vessels. OCT changes were suggestive of retinal ischemia: Increased reflectivity from the inner retinal layer and decreased backscattering from the retinal photoreceptors due to fluid and retinal edema. Ischemic maculopathy may cause a severe and permanent decrease in vision in AIDS patients. Fluorescein angiography and OCT should be considered in any patient with AIDS and unexplained visual loss. The mechanism of ischemic maculopathy may be multifactorial.
Keywords: Unilateral Ischemic Maculopathy, Cytomegalovirus Retinitis, Acquired Immunodeficiency Syndrome, Optical Coherence Tomography, Foveal Avascular Zone
INTRODUCTION
Numerous studies have shown that individuals with human immunodeficiency virus (HIV) disease have microvascular abnormalities and changes in blood flow.[1,2] The retinal microvasculopathy of HIV disease is characterized by ultrastructural changes similar to diabetic retinopathy.[3]
The combination of abnormal blood flow and microvasculopathy is believed to result in focal ischemia with the development of microaneurysms, retinal hemorrhages and cotton-wool spots. An electron microscopic study in patients with acquired immune deficiency syndrome (AIDS) revealed ischemic maculopathy in 6% of eye autopsies.[3] Human immunodeficiency virus associated with microvascular ischemia and damage, in theory, facilitates access of opportunistic infections into the retina.[4]
Herein, we report two patients with AIDS and CMV retinitis who developed decreased vision secondary to foveal ischemia manifesting as macular edema and irregular enlargement of the foveal avascular zone; fluorescein angiography (FA) and optical coherence tomography (OCT) findings are presented.
CASE REPORTS
Case 1
A 60-year-old man was diagnosed with HIV at the age of 57. He complained of decreased visual acuity (VA) and floaters of 45 days duration in his right eye. The patient was not on highly active antiretroviral therapy (HAART). He had a CD4 + T-lymphocyte count of 20 cells/µl. Visual loss was gradual, progressive, painless, and involved both central and peripheral vision. Examination revealed best corrected visual acuity (BCVA) of 20/400 in the right eye (RE) and 20/30 in the left eye (LE). Evaluation of the LE was unremarkable. Slit lamp biomicroscopic examination showed rubeosis iridis, 1 + cells and flare in the anterior chamber, and 1 + cells in the anterior vitreous in the RE. Intraocular pressure (IOP) was 24 mmHg in the RE and 12 mmHg in the LE. Posterior segment examination of the RE showed juxtafoveal retinal opacification and macular edema [Figure 1a], and a large area of peripheral CMV retinitis in zones 2 and 3 occupying 30% of the nasal retina.[5] Fluorescein angiography (Topcon TRC, Oakland, NJ, USA) revealed an enlarged and irregular foveal avascular zone extending to the temporal retina with faint, late staining of juxtafoveal vessels. Optical coherence tomography (Stratus OCT, Carl Zeiss, Dublin, CA, USA) demonstrated increased reflectivity at the inner retinal layer with a preponderance in the nasal area of the macula [Figure 1b and c]. The patient was treated with oral valgancyclovir, started on HAART, and administered a high dose of intravitreal ganciclovir (5.0 mg/0.1 ml once a week) for 5 doses followed by panretinal photocoagulation in the RE, which controlled the retinitis and rubeosis iridis. Six months later, BCVA was 20/300 in the RE with an increase in retinal thickness in the temporal area of the fovea, an epiretinal membrane and healed CMV retinitis, as demonstrated by OCT [Figure 1d].
Figure 1.
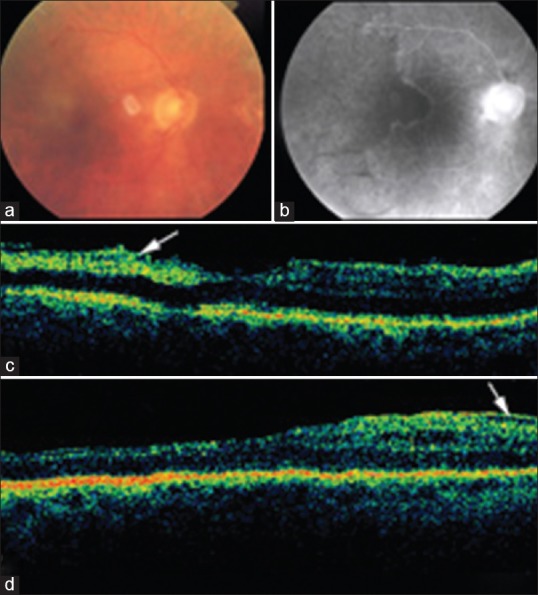
Case 1: (a) Color fundus photograph of the posterior pole shows juxtafoveal retinal opacification and macular edema. (b) Fluorescein angiography reveals an enlarged foveal avascular zone extending to the temporal retina. (c) Optical coherence tomography (OCT) demonstrated increased reflectivity from the inner retinal layers (arrow). (d) Six months later, OCT demonstrates increased retinal thickness in the temporal fovea with an epiretinal membrane (arrow).
Case 2
A 50-year-old white man was diagnosed with HIV/AIDS at the age of 49. He had a history of progressive outer retinal necrosis (PORN) in the LE treated with antivirals and three-port pars plana vitrectomy 1 year earlier. The patient was not on HAART. He had a CD4 + T-lymphocyte count of 30 cells/µl. The patient complained of floaters, red eye and visual loss in the RE of two months duration. Visual acuity was 20/400 in the RE and no light perception (NLP) in the LE. Slit-lamp examination was unremarkable OU. Fundus examination revealed an active granular CMV retinitis lesion in the nasal periphery of the RE. Cotton wool spots in fovea and parafoveal area were seen in the RE [Figure 2a]. Fluorescein angiography revealed an enlarged foveal avascular zone [Figure 2b], and OCT showed exudative inner limiting membrane detachment in the macular area and an increase in reflectivity from the inner retinal layers corresponding to retinal ischemia of the RE [Figure 2c]. The lesion was diagnosed as ischemic maculopathy on the basis of fluorescein angiography findings. The patient was treated with oral valgancyclovir, started on HAART, and administered a high dose intravitreal ganciclovir (5.0 mg/0.1 ml once a week); the CMV retinitis healed after 3 doses. Nine months later, best corrected visual acuity was 20/300 in the RE with reduction in retinal thickness at the foveal area as demonstrated by OCT [Figure 2d].
Figure 2.
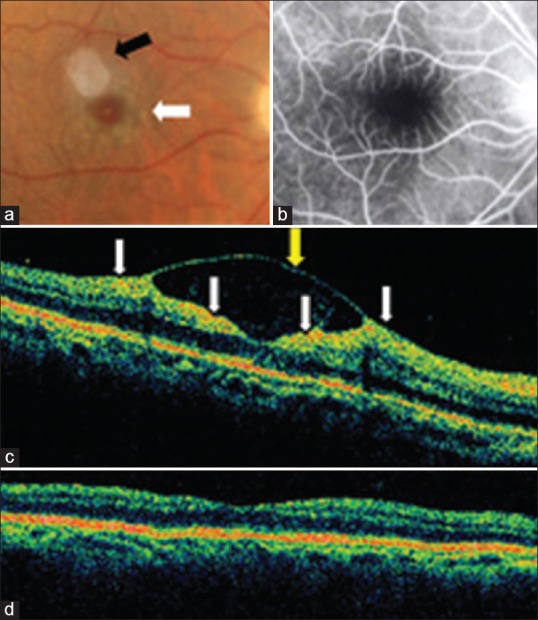
Case 2. (a) Color fundus photograph shows cotton-wool spots in the fovea and parafoveal area in the right eye (white arrow). The white reflex superotemporal to the fovea is an artifact (black arrow). (b) Fluorescein angiography revealed enlargement of the foveal avascular zone. (c) Optical coherence tomography (OCT) showed internal limiting membrane (ILM) detachment (yellow arrow) in the macular area with increased reflectivity at the inner retinal layer (white arrows) corresponding to retinal ischemia. Note the presence of reflective material within the ILM detachment. This shows that the ILM detachment was not serous and contained inflammatory/proteinaceous fluid (exudative ILM detachment). (d) Nine months later, OCT demonstrates normalization of the foveal contour.
DISCUSSION
Ocular findings of HIV microvasculopathy include sluggish blood flow in the conjunctival capillaries in addition to cotton-wool spots, intraretinal hemorrhage and microaneurysms in the retina[3] affecting up to 50% of patients with AIDS at some point in their disease. Using fluorescein angiography, Faber et al[2] noted focal loss of capillary perfusion in HIV-infected individuals supporting histologic findings of retinal capillary cell loss and focal occlusion of small vessels. Pepose et al[3] described retinal changes attributed to the microvasculopathy of HIV disease because of its similarity to changes seen with diabetic retinopathy. They termed the condition “ischemic maculopathy”.
In our patients, visual symptoms were unilateral. However, most reported cases are bilateral cases.[6,7] Opacification of the superficial retina in the macular area and intraretinal edema suggested the diagnosis. Fluorescein angiography changes were similar in the two cases with enlargement of the foveal avascular zone and late staining of juxtafoveal vessels. OCT changes consisted of increased reflectivity from the inner retina and decreased backscattering from the retinal photoreceptors due to fluid and retinal edema.
The prevalence of cotton-wool spots in patients with AIDS (70%) is significantly higher than other human immunodeficiency virus-infected individuals. Increased fibrinogen levels in HIV-infected patients contribute to sludging of blood flow by increasing red blood cell aggregation. Sludging of blood flow (probably in association with other factors) causes damage to the retinal microvasculature.[1] Anemia, opportunistic infections, or other unknown factors lead to transient episodes of increased retinal ischemia.[1]
In severely immunosuppressed individuals at risk of opportunistic infections, abnormal blood flow might increase the risk of retinal infection with blood-borne pathogens. In addition, CMV plays a role in the pathogenesis of ischemic maculopathy.[7,8] Although our patients were immunosuppressed, were not on HAART and had concurrent CMV retinitis (which by itself may involve the macula or cause optic neuritis), there were no sign of macular involvement due to CMV.
In summary, ischemic maculopathy causing severe visual loss can be seen in patients with AIDS. The presence of superficial retinal opacification on fundus examination, impaired foveal circulation on fluorescein angiography, and increased foveal and parafoveal inner retina reflectivity on OCT scans suggest the diagnosis. CMV retinitis plays a role in the pathogenesis of ischemic maculopathy. Fluorescein angiography and OCT should be considered in any patient with AIDS and unexplained visual loss. The mechanisms of ischemic maculopathy may be multifactorial and remain unknown.
Financial Support and Sponsorship
Supported in part by the Arevalo-Coutinho Foundation for Research in Ophthalmology, Caracas, Venezuela.
Conflicts of Interest
There are no conflicts of interest.
REFERENCES
- 1.Engstrom RE, Jr, Holland GN, Hardy WD, Meiselman HJ. Hemorheologic abnormalities in patients with human immunodeficiency virus infection and ophthalmic microvasculopathy. Am J Ophthalmol. 1990;109:153–161. doi: 10.1016/s0002-9394(14)75980-x. [DOI] [PubMed] [Google Scholar]
- 2.Faber DW, Wiley CA, Lynn GB, Gross JG, Freeman WR. Role of HIV and CMV in the pathogenesis of retinitis and retinal vasculopathy in AIDS patients. Invest Ophthalmol Vis Sci. 1992;33:2345–2353. [PubMed] [Google Scholar]
- 3.Pepose JS, Holland GN, Nestor MS, Cochran AJ, Foos RY. Acquired immune deficiency syndrome. Pathogenic mechanisms of ocular disease. Ophthalmology. 1985;92:472–484. doi: 10.1016/s0161-6420(85)34008-3. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham ET, Jr, Levinson RD, Jampol LM, Engstrom RE, Jr, Lewis H, Holland GN. Ischemic maculopathy in patients with acquired immunodeficiency syndrome. Am J Ophthalmol. 2001;132:727–733. doi: 10.1016/s0002-9394(01)01217-x. [DOI] [PubMed] [Google Scholar]
- 5.Holland GN, Buhles WC, Jr, Mastre B, Kaplan HJ. A controlled retrospective study of ganciclovir treatment for cytomegalovirus retinopathy. Use of a standardized system for the assessment of disease outcome UCLA CMV Retinopathy Study Group. Arch Ophthalmol. 1989;107:1759–1766. doi: 10.1001/archopht.1989.01070020841024. [DOI] [PubMed] [Google Scholar]
- 6.Romano MR, Valldeperas X, Romano F. Bilateral ischemic maculopathy in a patient with AIDS. Eur J Ophthalmol. 2006;16:761–763. doi: 10.1177/112067210601600518. [DOI] [PubMed] [Google Scholar]
- 7.Turaka K, Reddy R, Golshani A, Khaw WY, Bryan JS. Bilateral ischemic maculopathy in acquired immune deficiency syndrome. J Ophthalmic Inflamm Infect. 2013;3:15. doi: 10.1186/1869-5760-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akduman L, Feiner MA, Olk RJ, Kaplan HJ. Macular ischemia as a cause of decreased vision in a patient with acquired immunodeficiency syndrome. Am J Ophthalmol. 1997;124:699–702. doi: 10.1016/s0002-9394(14)70916-x. [DOI] [PubMed] [Google Scholar]


