Abstract
Background:
Burnout among junior doctors can affect patient care. We conducted a longitudinal cohort study designed to explore the incidence of burnout in medical interns and to examine the changes in burnout during the course of the intern year.
Methods:
Interns were recruited at two tertiary hospitals in Brisbane, Australia (n=180). Participants completed surveys at four time points during their internship year. All interns (100%) completed the baseline survey during their orientation. Response rates were 85%, 88%, and 79%, respectively, at 5-week, 6-month, and 12-month follow-up.
Results:
Interns reported high levels of personal and work-related burnout throughout the year that peaked at 6 months with mean scores of 42.53 and 41.81, respectively. Increases of 5.1 points (confidence interval [CI] 2.5,7.7; P=0.0001) and 3.5 points (CI 1.3,5.6; P=0.0015) were seen at 6 months for personal and work-related burnout, respectively. The mean score for patient-related burnout at 12 months was 25.57, and this number had increased significantly by 5.8 points (CI 3.2,8.5; P<0.0001) throughout the year. Correlation with demographic variables (age, sex) were found. The total incidence of burnout was 55.9%.
Conclusion:
Our study showed that burnout is a common problem among interns. The high incidence of burnout demonstrates the need for appropriate strategies to prevent adverse effects on doctors' quality of life and on the quality of care patients receive.
Keywords: Burnout–professional, education–medical, internship and residency, stress–psychological
INTRODUCTION
The life of a doctor is a busy one, and adjustment may be difficult for junior doctors making the transition from university life to full-time work. Reasons for this difficulty include the junior doctor's inexperience in coping with a stressful environment, as well as concerns related to training and career prospects.1 High levels of occupational stress are associated with burnout.2 Burnout is defined as a prolonged physical, emotional, and psychological exhaustion experienced as disengagement, blunting of emotions, feelings of helplessness/hopelessness, and loss of motivation. Doctors experience higher levels of burnout than the general population.3,4 For medical professionals, the negative implications of burnout are wide ranging and include decreased quality of patient care,5 increased anxiolytic use,1 and increased suicidality.6 The lifestyle and stresses inherent in medical practice, combined with a lack of experience, may make first-year doctors (interns) especially susceptible to burnout.
The phenomenon of burnout has been extensively researched and is usually identified through the use of validated surveys. The Copenhagen Burnout Inventory (CBI)4 assesses three types of burnout: personal, work related, and client related. The CBI has been used to identify burnout in a range of human services professions, including nurses and midwives, social workers, prison wardens, and doctors.4 The general population of human service workers was found to have mean burnout scores of 30.9-35.9. Kristensen et al reported that the CBI had excellent internal validity in test populations and low nonresponse rates.4 In an Australian study, the CBI was found to be a superior measure of burnout in dentists compared to the Maslach Burnout Inventory (MBI), another commonly used survey instrument.7
Past research has provided an impression of the incidence of burnout in Australian junior doctors. A study published by the Australian Medical Association (AMA) in 2009 reported a 69% incidence of burnout among junior doctors, but interns were excluded from this study.8 A national study of junior medical officers that included interns, carried out by The University of Western Australia (UWA) in 2009, reported low levels of job satisfaction and described a propensity for burnout.9 However, low response rates (22% for the AMA study, 39% for the UWA study) were an issue for both of these studies and restrict interpretation of these results. The stressed, burned-out doctors these surveys were designed to identify may not have had the time and energy to complete the survey. A longitudinal study published by Willcock et al followed medical graduates through the last 6 months of medical school and their first year as doctors.10 They found that burnout rises steeply in the early months of internship and peaks after 9 months of graduate medical practice, with a point prevalence of 75%.
Further research is needed to accurately describe the incidence of burnout in medical interns. We examined the incidence and longitudinal changes in burnout experienced by a cohort of interns at two tertiary metropolitan hospitals. We also examined whether certain demographic factors influenced burnout levels.
METHODS
Interns were recruited during their orientation week with the assistance of the Junior Doctor Societies from two major Queensland tertiary hospitals (Princess Alexandra Hospital [PAH] and Royal Brisbane and Women's Hospital [RBWH]). The study was designed as a 12-month, prospective, longitudinal cohort study, with surveys administered at four designated time points.
The first survey was administered during the interns' orientation week. This survey collected demographic information and included questions exploring the interns' concerns, expectations, and perceived preparedness for the year ahead. The longitudinal follow-up component of the study consisted of three surveys administered at 5 weeks, 6 months, and 12 months.
The follow-up surveys included the CBI questionnaire with questions that allow respondents to detail their perception of stress related to the work environment. The CBI also includes questions concerned with work-life balance, frustration with work and patients, and emotional stress. The responses are collated into the three burnout subscores (personal, work related, and client [patient] related), with scores ranging from 0-100.
Surveys were administered via an online survey tool called SurveyMonkey (www.surveymonkey.com). Participants were emailed a link to the survey at the relevant time points throughout the year, and electronic responses were collected. Participation was voluntary, and interns were assured that all answers were confidential. Data were deidentified prior to analysis.
Statistical analysis was conducted using generalized estimating equations to analyze the longitudinal change of mean burnout scores in each burnout type (personal, work related, patient related).11 Four demographic variables were analyzed as independent variables: age, sex, type of medical degree (undergraduate or postgraduate), and hospital (PAH or RBWH). Univariate analysis without a longitudinal component was used for these demographic variables.
RESULTS
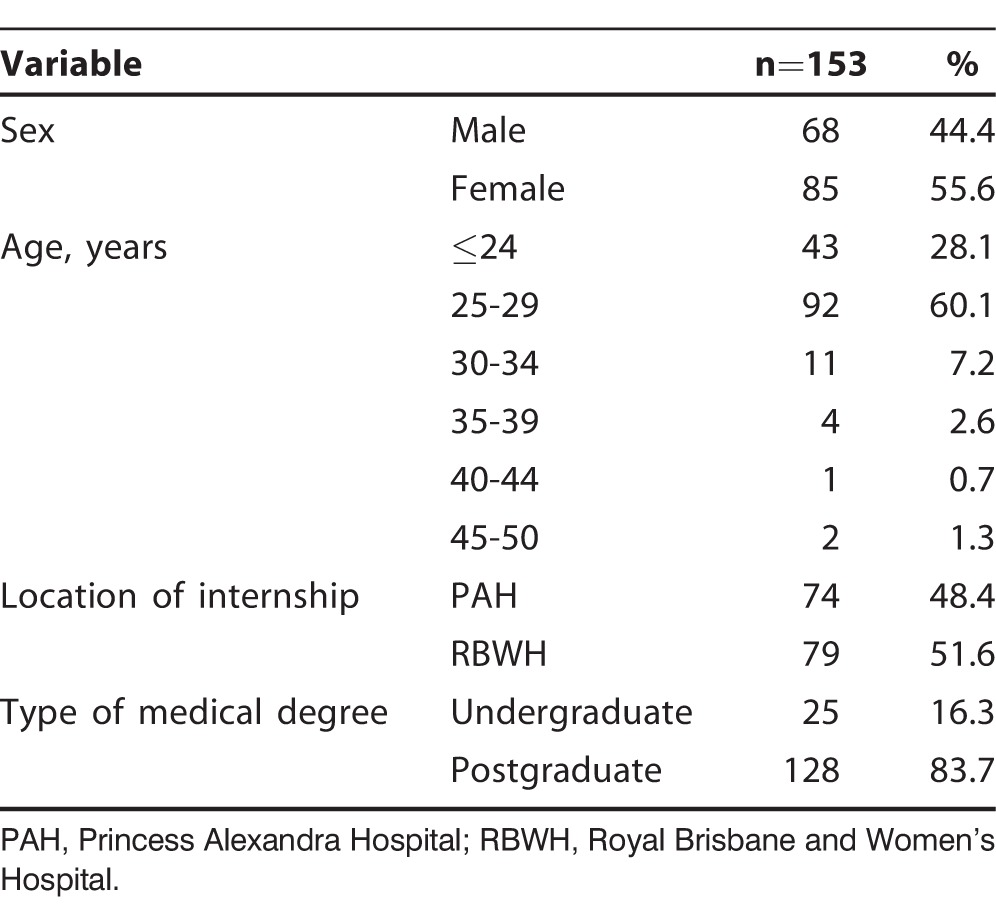
All interns at both hospitals (n=180) completed the baseline survey (the baseline survey did not include the CBI questions) and were enrolled into the study. The follow-up surveys included the CBI questionnaire and had satisfactory response rates. Because of inadequate responses (ie, <1 response in each burnout category), 5 responses were excluded from the 5-week survey and 3 responses from the 6-month survey. Final response rates were 85% (n=153) for the 5-week follow-up survey, 88% (n=159) for the 6-month survey, and 79% (n=143) for the 12-month survey. Demographic information for respondents to the 5-week follow-up survey is shown in the Table.
Table.
Baseline Demographics of 5-Week Survey Respondents
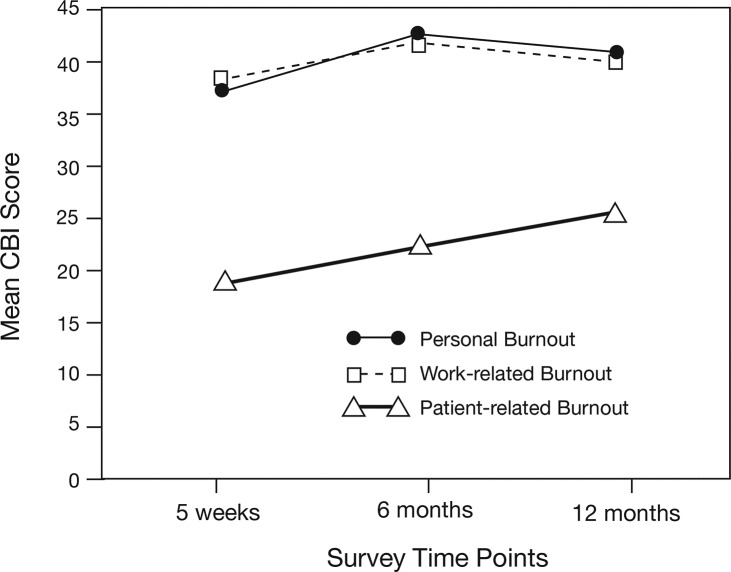
The cohort's mean burnout scores during the internship year are shown in Figure 1. These cohort mean scores provide a view of the overall level of burnout among the resident population. While this population-based measure does not provide information about how many individuals met the criteria for burnout (ie, a CBI score ≥50), it is a comparable measure used in previous cohort and population studies utilizing the CBI.4
Figure 1.
Mean Copenhagen Burnout Inventory (CBI) scores at three time points during the internship year.
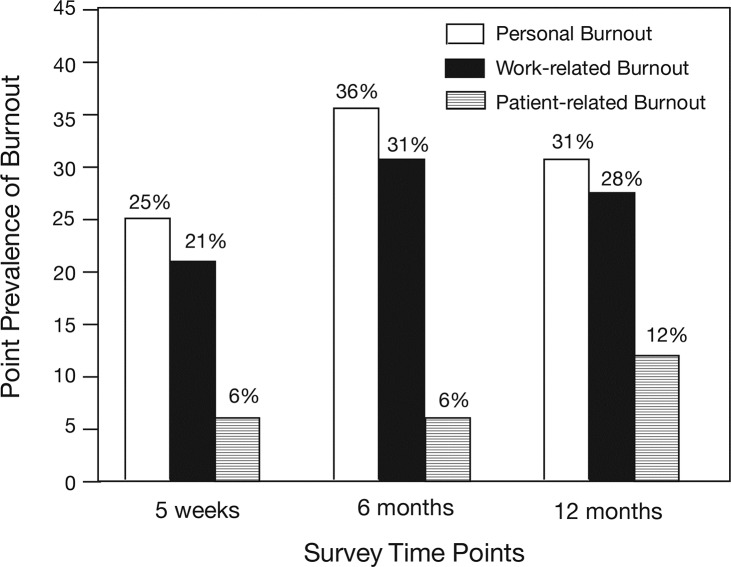
We also explored the number of individual cases of burnout (defined as a CBI score ≥50)4 using both point prevalence and annual incidence to show the percentage of the study population suffering from burnout at each specific time point and throughout the year, respectively. The point prevalence of burnout for the three categories is shown in Figure 2. Prevalence of personal- and work-related burnout was highest at the 6-month time point (36% and 31%, respectively). Prevalence of patient-related burnout peaked at the 12-month time point (12%), although the number of cases was low throughout the year. Annual incidence was calculated by determining the number of individuals who reported a score ≥50 in any burnout category throughout the year. The incidence of burnout in at least one CBI category during the entire year was 55.9%.
Figure 2.
Point prevalence of burnout at three time points during the internship year. Burnout is defined as Copenhagen Burnout Inventory score ≥50.
For the longitudinal analysis, the 5-week survey data were considered to be the baseline values, as this was the earliest time point that included the CBI survey. The change in personal burnout was statistically increased at 6 months; the mean score of 42.53 was an increase of 5.1 points compared to baseline (confidence interval [CI] 2.5,7.7; P=0.0001). However, this effect diminished to a nonsignificant trend at 12 months when the increase over baseline was 2.43 points (CI −1.9,5.1; P=0.0693).
The results for work-related burnout were similar. A significant increase in the work-related burnout score of 3.5 points (CI 1.3,5.6; P=0.0015) was seen at 6 months (mean score of 41.81). Again, this effect diminished and was not significant at 12 months when the increase over baseline was 1.5 points (CI −0.7,3.6; P=0.1823).
At 6 months, patient-related burnout scores had increased by a mean of 3.1 points (CI 0.8,5.5; P=0.0078) compared to baseline. This value significantly increased to 5.8 points (CI 3.2,8.5; P<0.0001) at 12-month follow-up (mean score of 25.57). Although this difference was significant, the overall level of patient-related burnout reported by survey respondents was low.
Demographic data were analyzed as independent variables, with a grouped analysis of all three follow-up time points. Significant differences were noted. Female sex was associated with higher personal burnout scores (5.7 points; CI 0.9,10.5; P=0.0187), but no sex differences were noted in work- or patient-related burnout. Age differences were found when using the ≤24-year-old group for comparison. The 25- to 29-year-old group had higher levels of work-related burnout (4.0 points; CI 0.8,7.0; P=0.0132), the 30- to 34-year-old group had higher levels of patient-related burnout (12.9 points; CI 2.6,23.1; P=0.0143), and the 40- to 44-year-old group had significantly lower levels of patient-related burnout (−15.5 points; CI −21.9,–9.0; P<0.0001) compared to the ≤24-year-old group. Although statistically significant, these age comparisons may represent a sampling error, as the numbers of participants in the 30- to 34-year-old and 40- to 44-year-old groups were low (n=14 and n=2, respectively). Neither the type of medical degree completed by interns (undergraduate or postgraduate) nor the hospital where they were placed (PAH or RBWH) showed any impact on burnout scores with univariate analysis.
DISCUSSION
We administered a validated survey assessing burnout to interns in two large Australian metropolitan hospitals with the aim of establishing the incidence and longitudinal changes in burnout throughout the internship year. A good response rate was achieved, and the results confirmed the hypothesis that burnout is common among interns. Furthermore, longitudinal analysis showed that burnout was most prevalent in the middle of the year in this population. The implication of these findings is that prevention strategies need to be considered to reduce the impact of burnout on junior doctors' quality of life and the care they provide to patients.
Response rates were a limiting factor in the UWA and AMA studies, but using our two hospitals' Junior Doctor Societies helped us achieve a total response rate of 75%. The Junior Doctor Society is a voluntary organization that seeks to engage and support residents throughout their placement at the hospital. This response rate is an important achievement, as the ability of a study to engage its target population directly influences the generalizability and accuracy of its findings.
The incidence of burnout throughout the year in our study was 55.9%. The UWA study used the Professional Quality of Life scale and found that 31% of interns were susceptible to burnout.9 Using the MBI, the AMA study found that 69% of respondents met the criteria for burnout.8 Our result falls between these two previously published results. The incidence described in this study is higher than the point prevalence at any assessed time point. One explanation for this observation is that interns suffer more burnout on certain rotations. Australian medical residents are required to rotate through a series of core rotations (general surgery, general medicine, and emergency medicine) as well as various elective specialties throughout the course of the year. Shift length and hours per week vary depending on the specialty a resident is assigned. Despite a push to reduce fatigue in the resident workforce in recent years, hard data describing changes to hours worked per week are lacking. Currently, no mandatory limits on duty hours exist, although a fatigue risk-management guideline is used in Queensland.12 Because of the differences among rotations, subsets of interns are more likely to be burned out during the rotations that involve more stressful work. A limited number of interns are on a given rotation at a time, and the group changes with every rotation, potentially explaining the disparity between point prevalence and incidence.
The authors of the CBI carried out a large study of burnout in human services workers in Denmark (the PUMA study).13 Compared to the PUMA study, mean burnout scores in this study population are higher than those reported in a wider population of hospital doctors.13 The pattern of burnout in our study, with high work-related burnout and low patient-related burnout, is similar to the pattern previously described in hospital doctors by those Danish authors.4
Examining changes in burnout during the study year revealed an increasing level of patient-related burnout, although absolute levels were low. Personal and work-related burnout scores peaked in the middle of the year, consistent with previously published longitudinal data.10 The cause for this pattern has not been adequately explored. Whether the interns developed coping mechanisms in the latter half of the year or some other factor is responsible cannot be determined from the data in this study and should be an area for future research.
Compared to other occupations, higher levels of burnout have been observed in hospital personnel.4 For example, the PUMA study also described burnout in administration staff, prison workers, and home-help nurses, with hospital-based workers generally having higher personal and work-related burnout than workers in the other occupations, although lower client-related (patient-related) burnout.13 Much research has examined the impact of burnout on health professionals and how they care for patients.1-6 Despite this attention, research examining why junior doctors might develop burnout has been lacking. In one study, the level of perceived consultant support was inversely correlated to the level of burnout in junior doctors.14 Future research may identify predisposing factors, allowing future interventions to prevent burnout. Various prevention strategies have been studied to this end. Examples include small group sessions, counseling, and techniques to improve communication between doctors and their colleagues and between doctors and patients.15-17 Closer monitoring of interns identified as susceptible to burnout should be implemented early in the year, and strategies to prevent burnout might be best implemented prior to the midyear peak of burnout seen in junior doctors.
Some limitations are evident in our study. First, using a generalized estimating equation is of limited use when numbers are small in certain groups11 and may explain the incongruous results for our age comparisons. Second, interns are required to undertake certain rotations throughout the year that have varying intensities and workloads. These rotation changes may have influenced the level of burnout experienced, independent of the time of year. Future research exploring the factors resulting in burnout could explore the relationship between type of placement and burnout. Finally, our study only included urban-based interns. While no differences were seen between the two major tertiary hospitals in Brisbane, interns are sent to a variety of locations including secondary referral centers and rural locations. High levels of burnout have been cited as contributing to a lack of retention of rural doctors,18 so a comparison of metropolitan, rural, regional, and remote interns may reveal differences and should be considered for future research.
CONCLUSION
Our study showed that burnout is a common problem in a cohort of interns at metropolitan tertiary hospitals in Australia, with 55.9% of our study sample experiencing burnout at some point during their internship and peak incidence occurring midyear. Our results are consistent with those described by previous studies. Future research should examine what factors contribute to burnout in interns. Additionally, previously suggested strategies to combat burnout in doctors should be studied in this population as an attempt at prevention.
ACKNOWLEDGMENTS
The authors have no financial or proprietary interest in the subject matter of this article. This article was presented at The Royal Australasian College of Surgeons 82nd Annual Scientific Congress. Auckland, New Zealand. May 6-10, 2013.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Professionalism, and Systems-Based Practice.
REFERENCES
- 1. . Keswani RN, Taft TH, Coté GA, Keefer L. Increased levels of stress and burnout are related to decreased physician experience and to interventional gastroenterology career choice: findings from a US survey of endoscopists. Am J Gastroenterol. 2011. October; 106 10: 1734- 1740. [DOI] [PubMed] [Google Scholar]
- 2. . Tsai FJ, Huang WL, Chan CC. Occupational stress and burnout of lawyers. J Occup Health. 2009; 51 5: 443- 450. [DOI] [PubMed] [Google Scholar]
- 3. . Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012. October 8; 172 18: 1377- 1385. [DOI] [PubMed] [Google Scholar]
- 4. . Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work Stress. 2005; 19 3: 192- 207. [Google Scholar]
- 5. . Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002. March 5; 136 5: 358- 367. [DOI] [PubMed] [Google Scholar]
- 6. . Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among US medical students. Ann Intern Med. 2008. September 2; 149 5: 334- 341. [DOI] [PubMed] [Google Scholar]
- 7. . Winwood PC, Winefield AH. Comparing two measures of burnout among dentists in Australia. Int J Stress Manag. 2004. August; 11 3: 282- 289. [Google Scholar]
- 8. . Markwell AL, Wainer Z. The health and wellbeing of junior doctors: insights from a national survey. Med J Aust. 2009. October 19; 191 8: 441- 444. [DOI] [PubMed] [Google Scholar]
- 9. . Heredia DC, Rhodes CS, English SE, Law DB, McElrea AC, Honeyball FX. The national Junior Medical Officer Welfare Study: a snapshot of intern life in Australia. Med J Aust. 2009. October 19; 191 8: 445. [DOI] [PubMed] [Google Scholar]
- 10. . Willcock SM, Daly MG, Tennant CC, Allard BJ. Burnout and psychiatric morbidity in new medical graduates. Med J Aust. 2004. October; 181 7: 357- 360. [DOI] [PubMed] [Google Scholar]
- 11. . Ballinger GA. Using generalized estimating equations for longitudinal data analysis. Organ Res Methods. 2004. April; 7 2: 127- 150. [Google Scholar]
- 12. . Queensland Health. Fatigue risk management [human resources policy]. Queensland, Australia: Department of Health; December 2014. Policy no.: I1 (QH-POL-171) http://www.health.qld.gov.au/qhpolicy/docs/pol/qh-pol-171.pdf. Accessed February 10, 2015. [Google Scholar]
- 13. . Borritz M, Rugulies R, Bjorner JB, Villadsen E, Mikkelsen OA, Kristensen TS. Burnout among employees in human service work: design and baseline findings of the PUMA study. Scand J Public Health. 2006; 34 1: 49- 58. [DOI] [PubMed] [Google Scholar]
- 14. . Sochos A, Bowers A, Kinman G. Work stressors, social support, and burnout in junior doctors: exploring direct and indirect pathways. J Employ Couns. 2012. June; 49 2: 62- 73. [Google Scholar]
- 15. . Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009. September 23; 302 12: 1284- 1293. [DOI] [PubMed] [Google Scholar]
- 16. . Kuerer HM, Breslin T, Shanafelt TD, Baile WF, Crawford W, Balch CM. Road map for maintaining career satisfaction and balance in surgical oncology. J Am Coll Surg. 2008. September; 207 3: 435- 442. [DOI] [PubMed] [Google Scholar]
- 17. . Rø KE, Gude T, Tyssen R, Aasland OG. Counselling for burnout in Norwegian doctors: one year cohort study. BMJ. 2008. November 11; 337: a2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. . Thommasen H, Berkowitz J, Grzybowski S. Community factors associated with long-term physician retention. Br C Med J. 2000. November; 42 9: 426- 429. [Google Scholar]