Abstract
Background
It is unclear whether oral anticoagulants are beneficial for atrial fibrillation (AF) patients with low CHA2DS2-VASc score. Age could be important in determining the risk of thromboembolism in low risk AF patients (CHA2DS2-VASc score of 1 for male or 2 for female).
Methods
The Taiwan National Health Insurance Research Database (NHIRD) was used and 27,521 AF patients with CHA2DS2-VASc score of 1 (male) or 2 (female) not receiving anticoagulants were acquired as the study cohort, which were classified into three age groups: 20–49, 50–64, and 65–74 years. The clinical endpoint was the occurrence of ischemic thromboembolism within one year of follow up.
Results
During the follow-up of 0.94 ± 0.19 years, 385 (2.19%) male patients experienced ischemic thromboembolism, with annual rate of 2.32%. The annual risk ranged from 1.29%, 2.43% to 2.77% for male patients aged 20–49, 50–64 and 65–74 years respectively. Of the female patients, 218 (2.20%) experienced clinical event with annual rate of 2.32%. The annual risk increased from 1.87%, 2.28% to 2.64% for female patients aged 20–49, 50–64 and 65–74 years respectively. There was no difference in risk between the male patients aged 20–49 years with CHA2DS2-VASc score of 1 and overall male patients with CHA2DS2-VASc score of 0. (P = 0.631) The female patients aged 20–49 years with CHA2DS2-VASc score of 2 was associated with a higher risk of thromboembolic events than overall female patients with CHA2DS2-VASc score of 1 (HR = 1.93; P = 0.008).
Conclusions
Age is important in determining the risk of thromboembolism in AF patients with single risk factor. In male patients <50 years old with CHA2DS2-VASc score of 1, the risk of ischemic thromboembolism was low. Considering the benefits and the risk of bleeding, oral anticoagulation therapy may not be favorable in these patients.
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia and causes a 4- to 5-fold increased risk of thromboembolic stroke.[1] Current guidelines for oral anticoagulants (OACs) advocate using the CHA2DS2-VASc (heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke or transient ischemic attack (TIA), vascular disease, age 65 to 74 years, female gender) scoring system to stratify the risk of stroke.[2–6] The guidelines virtually recommend anticoagulants for AF patients with a CHA2DS2-VASc score of 2 and above. However, the recommendations for AF patients with CHA2DS2-VASc score of 1 are not consistent. The ESC, Asia Pacific Heart Rhythm Society, and National Institute for Health and Care Excellence guidelines suggest OACs for AF patients with CHA2DS2-VASc score of 1 which is not due to gender (female).[7–9] On the other hand, the 2014 ACC/AHA guidelines do not firmly recommend OACs for these low risk patients (class IIb).[10] The actual risk of ischemic thromboembolism and whether or not anticoagulants should be given to these AF patients remain uncertain.
Limited data are available for AF patients with minimal risk factors at age less than 65 years old. In young people, risk factors in CHA2DS2-VASc score may not be as important as in elderly people. We hypothesized that the risk of ischemic thromboembolism in AF patients under the age of 65 is low when only one risk factor in CHA2DS2-VASc score exists. Therefore, this study was to investigate the one-year risk of ischemic thromboembolism in young AF patients with single risk factor not due to female (CHA2DS2-VASc score of 1 for male or 2 for female) and the impact of different component risk factors.
Materials and Methods
Study Population
The NHI system is a mandatory universal health insurance program which offers comprehensive medical care coverage to all Taiwanese residents. The NHIRD is released by the National Health Research Institutes of Taiwan, and is a national database consisting of detailed health care data from >23 million enrollees, representing >99% of the population of Taiwan. This study was exempted from review by the Chang Gung medical foundation institutional review board (104-1177B) because the original identification number of each patient in the NHIRD is encrypted and de-identified to protect their privacy, using a consistent encrypting procedure so that it was feasible to link and continuously follow all of the claims belonging to the same patient within the NHIRD.
Study Cohort
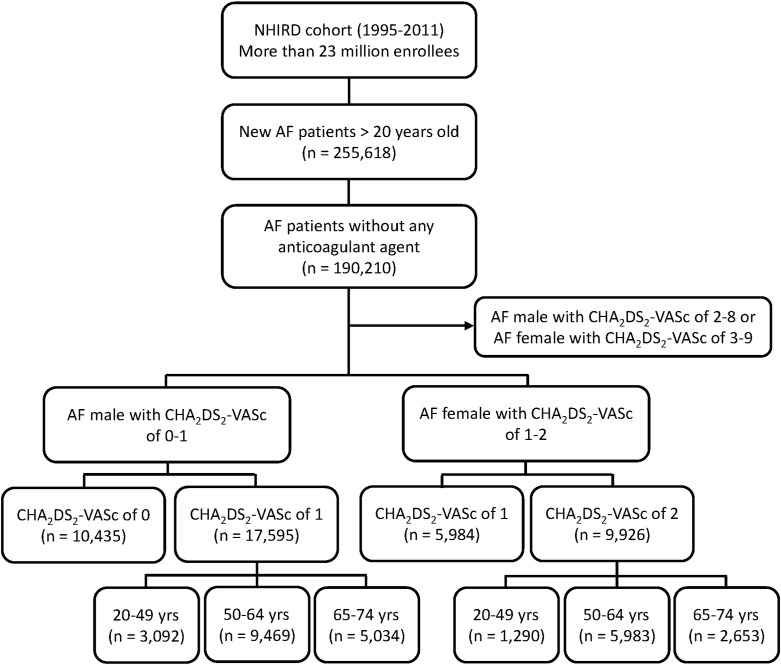
From January 1, 1995, to December 31, 2011, a total of 255,618 patients with AF who were older than 20 years of age were identified in the NHIRD. AF was determined using International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) code (427.31). To ensure diagnostic accuracy, patients were defined as having AF only when there was a discharge diagnosis or more than two outpatient visits related to AF. The diagnostic accuracy of AF based on the definition was validated before.[11, 12] The patients who received treatment with warfarin or any antiplatelet agent including aspirin and clopidogrel were excluded from the study population. A total of 190,210 AF patients were finally enrolled as the study cohort, including 17,595 males with a CHA2DS2-VASc score of 1 and 9,926 females with a CHA2DS2-VASc score of 2. Among the 17,595 male patients, there were 3,092, 9,469, and 5,034 patients in the age groups of 20 to 49, 50 to 65, and 65 to 74 years of age, respectively. Among the 9,926 female patients, there were 1,290, 5,983, and 2,653 patients in the age groups of 20 to 49, 50 to 64, and 65 to 74 years of age, respectively. Another 10,435 males had a CHA2DS2-VASc score of 0 and 5,984 females had a CHA2DS2-VASc score of 1, and they served as the reference group. We defined the young age group in the range of 20 to 49 years of age, because ischemic strokes attacked after adolescence and before the 50 years of age are typically considered as “young stroke” based on previous definition.[13] A flowchart of the enrollment of the study cohort is shown in Fig 1.
Fig 1. Flow Chart of Study Cohort Enrollment.
Patients who received treatments with warfarin or any antiplatelet agent, including aspirin and clopidogrel, were excluded from the study population. A total of 190,210 patients were finally enrolled in the study cohort with 17,595 males with CHA2DS2-VASc score of 1 and 9,926 females with CHA2DS2-VASc score of 2. Among the 17,595 male patients, there were 3,092, 9,469, and 5,034 patients in the age groups of 20 to 49, 50 to 64, and 65 to 74 years of age, respectively. Among the 9,926 female patients, there were 1,290, 5,983, and 2,653 patients in the age groups of 20 to 49, 50 to 64, and 65 to 74 years of age, respectively. There were other 10,435 males with CHA2DS2-VASc score of 0 and 5,984 females with CHA2DS2-VASc score of 1 used as the reference group, respectively. AF = atrial fibrillation; CHA2DS2-VASc = heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke/transient ischemic attack, vascular disease, age 65 to 74 years, female.
Calculation of CHA2DS2-VASc Score and Determination of the Endpoint
The CHA2DS2-VASc score was calculated for each patient by assigning 1 point each for an age between 65 and 74 years, a history of heart failure, hypertension, diabetes, vascular disease (myocardial infarction or peripheral artery disease), and female gender, and 2 points each for a history of an ischemic stroke, TIA, or an age more than 75 years. The ICD-9-CM codes used to identify the risk factor components of the scoring scheme are shown in S1 Table. To ensure diagnostic accuracy, patients were defined as having ischemic stroke, TIA, myocardial infarction, peripheral artery disease and heart failure only when it was a discharge diagnosis. The diagnoses of hypertension and diabetes were considered when the diagnostic codes were confirmed more than twice in outpatient visits. The diagnostic accuracies of comorbidities with hypertension, diabetes mellitus, congestive heart failure, myocardial infarction, and peripheral vascular disease had been validated before.[14, 15] The clinical endpoints were defined as the occurrence of ischemic stroke or systemic embolism with concomitant imaging studies of the brain or target organs, including computed tomography, magnetic resonance imaging and ultrasound imaging. The study endpoint of ischemic stroke/systemic embolism was considered only when it was a discharge diagnosis. The accuracy of the diagnosis of ischemic stroke in the NHIRD has been validated in previous studies, with a positive predictive value of 88.4% and sensitivity of 97.3%.[15, 16]
Statistical Analysis
Data are presented as mean values ± standard deviation for continuous variables, and proportions for continuous variables. The risk of ischemic thromboembolism was assessed using Cox regression analysis. The curve of ischemic thromboembolism-free rate after AF diagnosis was plotted using the Kaplan-Meier method, with statistical significance examined by the log-rank test. Statistical significance was defined as a P value of less than 0.05. All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
The annual risk of ischemic thromboembolism of the 190,210 study patients and the corresponding CHA2DS2-VASc scores are summarized in Table 1. As expected, the annual risk of a clinical event increased with increases in CHA2DS2-VASc score, with an annual risk of 1.18% for a CHA2DS2-VASc score of 0 to as high as 20.26% for a CHA2DS2-VASc score of 7 or higher. In order to investigate the risk of ischemic stroke/systemic emboli in AF patients by age and gender, we further separated the total AF patient group into four age subgroups in both genders: 20 to 49, 50 to 64, 65 to 74, and more than 75 years (Table 2). The results showed that were distinct annual risks of clinical events even with the same CHA2DS2-VASc score in each gender. It is noted that AF patients who were younger than 50 years of age had the lowest annual risk of clinical events compared to the older age groups in both genders with one additional risk factor (CHA2DS2-VASc score of 1 for male or 2 for female). We also found that young females with a CHA2DS2-VASc score of 6 (47.71%) carried an unusual high annual risk of clinical events, which may have been due to the limited number of patients and clinical events in these young patient groups.
Table 1. AnnuaI Risk of Ischemic thromboembolism by CHA2DS2-VASc Score among AF patients without anticoagulants.
| Ischemic thromboembolsim | |||
|---|---|---|---|
| Events | Person-years | Risk | |
| CHA2DS2-VASc | |||
| 0 | 116 | 9822 | 1.18% |
| 1 | 440 | 22233 | 1.98% |
| 2 | 1114 | 31787 | 3.50% |
| 3 | 2017 | 40572 | 4.97% |
| 4 | 2570 | 36162 | 7.11% |
| 5 | 2155 | 20197 | 10.67% |
| 6 | 1425 | 8610 | 16.55% |
| 7–9 | 828 | 4087 | 20.26% |
AF = atrial fibrillation; CHA2DS2-VASc = heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke/transient ischemic attack, vascular disease, age 65 to 74 years, female
Table 2. AnnuaI Risk of Ischemic Thromboembolism Stratified by CHA2DS2-VASc Score, Gender, and Age among AF patients without anticoagulants.
| Age = 20–49 | Age = 50–64 | Age = 65–74 | Age = 75 up | All | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Events | Risk | Events | Risk | Events | Risk | Events | Risk | Events | Risk | |
| Female | ||||||||||
| 0 | - - | - - | - - | - - | - - | - - | - - | - - | - - | - - |
| 1 | 14 | 0.56% | 41 | 1.30% | - - | - - | - - | - - | 55 | 0.78% |
| 2 | 23 | 1.87% | 129 | 2.28% | 66 | 2.64% | - - | - - | 218 | 1.94% |
| 3 | 22 | 5.75% | 111 | 3.31% | 327 | 3.60% | 184 | 5.63% | 644 | 3.16% |
| 4 | 7 | 11.68% | 85 | 11.45% | 394 | 5.59% | 885 | 6.14% | 1371 | 4.19% |
| 5 | 2 | 12.76% | 62 | 21.90% | 282 | 12.87% | 888 | 7.38% | 1234 | 5.04% |
| 6 | 1 | 47.71% | 13 | 20.61% | 210 | 21.76% | 775 | 14.59% | 999 | 7.19% |
| 7–9 | 0 | 0.00% | 7 | 59.02% | 65 | 23.17% | 647 | 20.98% | 719 | 9.56% |
| Male | ||||||||||
| 0 | 22 | 0.50% | 94 | 1.75% | - - | - - | - - | - - | 116 | 1.18% |
| 1 | 38 | 1.29% | 216 | 2.43% | 131 | 2.77% | - - | - - | 385 | 2.32% |
| 2 | 41 | 4.73% | 205 | 4.56% | 446 | 3.68% | 204 | 4.14% | 896 | 4.00% |
| 3 | 19 | 9.10% | 163 | 12.97% | 440 | 5.91% | 751 | 4.82% | 1373 | 5.61% |
| 4 | 4 | 8.79% | 90 | 17.93% | 410 | 15.47% | 695 | 6.50% | 1199 | 8.63% |
| 5 | 2 | 12.37% | 31 | 34.08% | 245 | 22.12% | 643 | 14.43% | 921 | 16.24% |
| 6 | 0 | 0.00% | 6 | 17.87% | 53 | 21.72% | 367 | 18.45% | 426 | 18.78% |
| 7–9 | - - | - - | - - | - - | 14 | 20.30% | 95 | 14.81% | 109 | 15.35% |
AF = atrial fibrillation; CHA2DS2-VASc = heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke/transient ischemic attack, vascular disease, age 65 to 74 years, female
Male patients with a CHA2DS2-VASc score of 0 had a relatively low annual risk of clinical events with 1.18% (Table 2). Of note, the annual risk of clinical events remained low (1.29%) in male patients with a CHA2DS2-VASc score of 1 who were less than 50 years of age. The older AF male patients (more than 50 years) with a CHA2DS2-VASc score of 1 and overall male patients with a CHA2DS2-VASc score of more than 1 had a significantly increased annual risk of clinical events (more than 2.43%). In contrast to the male patients, the young female patients with a CHA2DS2-VASc score of 2 had an increased annual risk of clinical events (1.87%) as compared with the overall female patient groups with a CHA2DS2-VASc score of 1 (0.97%).
We then specifically focused on the patients with a CHA2DS2-VASc score of1 for males or 2 for females, since the recommendations for anticoagulation treatment in patients with a low CHA2DS2-VASc score remain unclear based on the current guidelines. Table 3 summarizes the baseline data of the patient groups with one single additional stroke risk factor. The proportions of each age group (20 to 49, 50 to 64 and 65 to 74 years) to all AF patients were 17.6%, 53.8%, and 28.6% in the males with a CHA2DS2-VASc score of 1, and 13.0%, 60.2%, and 26.7% in the females with a CHA2DS2-VASc score of 2, respectively. The mean age and prevalence of each risk factor in the study patients by age group are shown in Table 3. The mean ages were 42.9 ± 5.8, 58.0 ± 4.2, and 69.7 ± 2.8 for the male patients and 43.6 ± 5.5, 58.3 ± 4.2, and 69.5 ± 2.8 for the female patients in the 20 to 49, 50 to 64 and 65 to 74 years age groups, respectively. Hypertension and vascular diseases were the most and least prevalent risk factors for the AF patients aged 20 to 49 and 50 to 64 years in both genders, respectively. Of note, the young AF patients had a higher prevalence of congestive heart failure compared with the older AF patients with the same CHA2DS2-VASc score in both genders (12.3% vs. 6.3% for the males; 15.0% vs. 5.0% for the females).
Table 3. Baseline Characteristics for AF Patients with One Additional Risk Factor of CHA2DS2-VASc Score*.
| Male | Female | |||||
|---|---|---|---|---|---|---|
| Onset age of AF | 20–49 | 50–64 | 65–74 | 20–49 | 50–64 | 65–74 |
| Number | 3,092 (17.6%) | 9,469 (53.8%) | 5,034 (28.6%) | 1,290 (13.0%) | 5,983 (60.3%) | 2,653 (26.7%) |
| Age, years | 42.9 ± 5.8 | 58.0 ± 4.2 | 69.7 ± 2.8 | 43.6 ± 5.5 | 58.3 ± 4.2 | 69.5 ± 2.8 |
| CHA2DS2-VASc score | 1 | 1 | 1 | 2 | 2 | 2 |
| Risk factors according to CHA2DS2-VASc: | ||||||
| Heart failure | 381(12.3%) | 601 (6.3%) | 0 (0%) | 193 (15.0%) | 301 (5.0%) | 0 (0.0%) |
| Hypertension | 2351(76.0%) | 7738 (81.7%) | 0 (0%) | 898 (69.9%) | 5052 (84.4%) | 0 (0.0%) |
| Age 65–74 years | 0 (0.0%) | 0 (0.0%) | 5034 (100%) | 0 (0.0%) | 0 (0.0%) | 2653 (100%) |
| Diabetes mellitus | 316 (10.2%) | 965 (10.2%) | 0 (0.0%) | 190 (14.7%) | 606 (10.1%) | 0 (0.0%) |
| Vascular disease | 44 (1.4%) | 165 (1.7%) | 0 (0.0%) | 9 (0.7%) | 24 (0.4%) | 0 (0.0%) |
*CHA2DS2-VASc score of 1 for males and 2 for females
AF = atrial fibrillation; CHA2DS2-VASc = heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke/transient ischemic attack, vascular disease, age 65 to 74 years, female
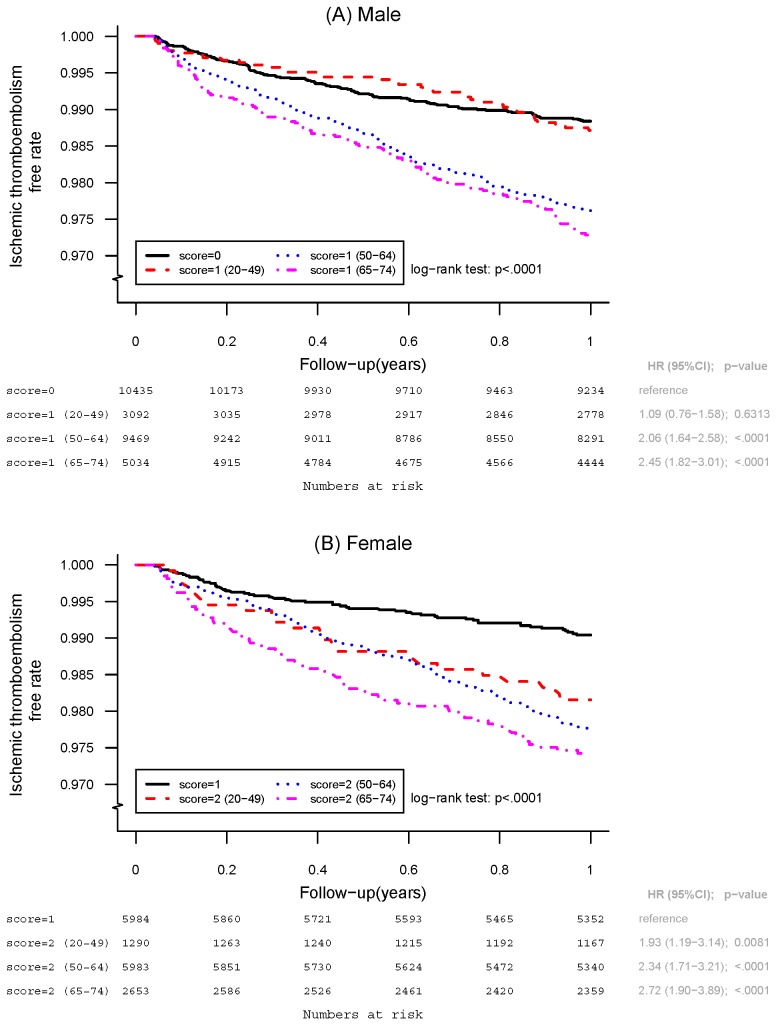
Fig 2 shows the ischemic thromboembolism-free curves of the AF patients with one additional risk factor for three age subgroups. Using the patients overall without any additional risk factors (CHA2DS2-VASc score of 0 for males or 1 for females) as the reference group in each gender, the male patients with a CHA2DS2-VASc score of 1 in both the 50 to 64 and 65 to 74 years age groups had a significantly higher cumulative risk of ischemic stroke/systemic embolism compared with the reference group (HR, 2.06; 95% CI, 1.64–2.58; P < 0.0001 for 50 to 64 years of age; HR, 2.45; 95% CI, 1.82–3.01; P < 0.0001 for 65 to 74 years of age). However, the young male patients with a CHA2DS2-VASc score of 1 did not have a higher cumulative risk of clinical events than the male patients overall with a CHA2DS2-VASc score of 0 (HR, 1.09; 95% CI, 0.76–1.58; P = 0.6313). In addition, the 50 to 64 and 65 to 74 years old patients had a significantly higher risk compared with the 20 to 49 years old patients with a CHA2DS2-VASc score of 1 (HR, 1.88; 95% CI, 1.33–2.65; P = 0.0003 for 50 to 64 versus 20 to 49 years of age; HR, 2.14; 95% CI, 1.49–3.07; P < 0.0001 for 65 to 74 versus 20 to 49 years of age).
Fig 2. Kaplan-Meier Survival Curves in AF patients with One Additional Risk Factor of CHA2DS2-VASc Score.
A. Cumulative survival curves in male patients with CHA2DS2-VASc Score of 1 in the age groups of 20 to 49, 50 to 64, and 65 to 74 years of age, respectively. There is no difference of the cumulative risk of ischemic thromboembolism between male AF patients with CHA2DS2-VASc score of 1 for 20 to 49 years of age and overall patients with CHA2DS2-VASc score of 0. B. Cumulative survival curves in female patients with CHA2DS2-VASc Score of 2 in the age groups of 20 to 49, 50 to 64, and 65 to 74 years of age, respectively. Young female patient with CHA2DS2-VASc score of 2 and 20 to 49 years of age showed significantly higher cumulative risk of clincial event as compared with overall female patients with CHA2DS2-VASc score of 1.
For female gender, the female patients with a CHA2DS2-VASc score of 2 for all age subgroups had a significantly higher risk compared with the female patients overall with a CHA2DS2-VASc score of 1 (HR, 1.93; 95% CI, 1.19–3.14; P = 0.0081 for 20 to 49 years of age; HR, 2.34; 95% CI, 1.71–3.21; P < 0.0001 for 50 to 64 years of age; HR, 2.72; 95% CI, 1.90–3.89; P < 0.0001 for 65 to 74 years of age) compared with the reference group. Of note, neither the 50 to 64 nor 65 to 74 years old patients had a significantly higher risk compared with the 20–49 years old patients with a CHA2DS2-VASc score of 2 (HR, 1.21; 95% CI, 0.78–1.89; P = 0.3916 for 50 to 64 versus 20 to 49 years of age; HR, 1.41; 95% CI, 0.88–2.26; P = 0.1575 for 65 to 74 versus 20 to 49 years of age).
Among the 3,092 male patients with a CHA2DS2-VASc score of 1 who were younger than 50 years of age, only heart failure (HR, 3.34; 95% CI, 1.92–5.82; P < 0.0001) had a significantly higher risk of thromboembolic events compared with the reference group (Table 4). For the 1,290 female patients with a CHA2DS2-VASc score of 2 who were younger than 50 years of age, both heart failure (HR, 2.88; 95% CI, 1.15–7.20; P = 0.0235) and hypertension (HR, 1.92; 95% CI, 1.10–3.35; P = 0.0216) have a significantly higher risk of a clinical event compared with the reference group. Among the 9,469 male patients with a CHA2DS2-VASc score of 1 who were 50 to 64 years of age, all four risk factors (heart failure, hypertension, diabetes, and vascular disease) contributed to a significant risk of a clinical event compared with the reference group (all P < 0.01). For the 5,983 female patients with a CHA2DS2-VASc score = 2 who were 50 to 64 years of age, heart failure, diabetes and hypertension all had a significant risk of a clinical event compared with the reference group (all P < 0.05).
Table 4. Risk of Ischemic Thromboembolism in AF Patients with One Additional Risk Factor of CHA2DS2-VASc Score*.
| Age | Risk Factor Components of the CHA2DS2-VASc Score | Patients | Events | Person-Years | Annual Risk (%) (95% CI) | Hazard Ratio (95% CI) | P Value |
|---|---|---|---|---|---|---|---|
| CHA2DS2-VASc Score of 1 for Males | |||||||
| 20–49 | Heart failure | 381 | 14 | 354.79 | 3.95% (1.88%-6.01%) | 3.34 (1.92–5.82) | <0.0001 |
| Diabetes mellitus | 316 | 2 | 297.28 | 0.67% (0.08%-2.43%) | 0.57 (0.14–2.30) | 0.4298 | |
| Hypertension | 2351 | 22 | 2249.83 | 0.98% (0.57%-1.39%) | 0.83 (0.53–1.31) | 0.4210 | |
| Vascular disease | 44 | 0 | 40.37 | 0.00% (- -) | - - | - - | |
| 50–64 | Heart failure | 601 | 19 | 552.94 | 3.44% (1.89%-4.98%) | 2.89 (1.78–4.70) | <0.0001 |
| Diabetes mellitus | 965 | 20 | 898.07 | 2.23% (1.25%-3.20%) | 1.88 (1.17–3.02) | 0.0092 | |
| Hypertension | 7738 | 170 | 7289.03 | 2.33% (1.98%-2.68%) | 1.97 (1.56–2.50) | <0.0001 | |
| Vascular disease | 165 | 7 | 156.07 | 4.49% (1.80%-9.24%) | 3.81 (1.78–8.17) | 0.0006 | |
| 65–74 | — | 5034 | 131 | 4735.07 | 2.77% (2.29%-3.24%) | 2.34 (1.82–3.01) | <0.0001 |
| CHA2DS2-VASc Score of 2 for Females | |||||||
| 20–49 | Heart failure | 193 | 5 | 177.64 | 2.81% (0.91%-6.57%) | 2.88 (1.15–7.20) | 0.0235 |
| Diabetes mellitus | 190 | 2 | 182.02 | 1.10% (0.13%-3.97%) | 1.13 (0.28–4.64) | 0.8628 | |
| Hypertension | 898 | 16 | 859.12 | 1.86% (0.95%-2.77%) | 1.92 (1.10–3.35) | 0.0216 | |
| Vascular disease | 9 | 0 | 8.08 | 0.00% (- -) | - - | - - | |
| 50–64 | Heart failure | 301 | 15 | 277.73 | 5.40% (2.67%-8.13%) | 5.54 (3.13–9.81) | <0.0001 |
| Diabetes mellitus | 606 | 12 | 577.08 | 2.08% (0.90%-3.26%) | 2.14 (1.15–4.00) | 0.0168 | |
| Hypertension | 5052 | 102 | 4789.16 | 2.13% (1.72%-2.54%) | 2.19 (1.58–3.04) | <0.0001 | |
| Vascular disease | 24 | 0 | 23.67 | 0.00% (- -) | - - | - - | |
| 65–74 | — | 2653 | 66 | 2499.41 | 2.64% (2.00%-3.28%) | 2.72 (1.90–3.89) | <0.0001 |
*CHA2DS2-VASc score of 1 for males and 2 for females
AF = atrial fibrillation; CHA2DS2-VASc = heart failure, hypertension, age 75 years or older, diabetes mellitus, previous stroke/transient ischemic attack, vascular disease, age 65 to 74 years, female
Discussion
This study is a nation-wide large population-based investigation to analyze the risk of ischemic thromboembolism focusing on CHA2DS2-VASc score of 1 in males and 2 in females, specifically in patients < 65 years old with AF who did not receive OACs. We found that age is an important factor in determining the risk of stroke in these low risk patients who were younger than 65 years old. The risk of ischemic thromboembolism in male patients < 50 years old was extremely low (less than 1.29%) for those with a CHA2DS2-VASc score of 1. The cumulative event rate was similar between the young male patients with a CHA2DS2-VASc score of 1 and the male patients overall with a CHA2DS2-VASc score of 0 (P = 0.6313). In contrast, the young female patients with a CHA2DS2-VASc score of 2 had an increased risk of clinical events compared with the female patients overall with a CHA2DS2-VASc score of 1 (P = 0.0081). Since the risk of major bleeding due to non-vitamin K antagonist OACs has been reported to be as high as 0.25% to 1.45% per year and even higher for warfarin,[17–21] the actual benefit of anticoagulation therapy is questionable in young male AF patients with one risk factor in CHA2DS2-VASc score. For male patients with 50 to 64 years of age and female patients with all age groups carrying one single additional stroke risk factor, we observed that OACs is still recommended, since the annual risk of ischemic thromboembolism was more than 1.87% and the cumulative event rate remained significantly high in these AF patients compared to the reference group (Fig 2). Heart failure rather than other risk factors including diabetes, hypertension and vascular disease was the most important risk factor for thromboembolism in the young AF patients with one additional risk factor of the CHA2DS2-VASc score in both genders. Since the recommendations for anticoagulation treatment in patients with a CHA2DS2-VASc score of 1 are not consistent between the current guidelines, our observations should help to improve the rationale of using OACs in patients < 50 years old or between 50–65 years old with CHA2DS2-VASc score of 1 not due to gender.
Age has been reported to be a more important non-modifiable risk factor for ischemic stroke compared to other factors.[22] Several possible mechanisms may explain the vulnerability to ischemic stroke due to aging. Aging is often associated with other independent risk factors such as hypertension, diabetes, vascular disease, or heart failure in the CHA2DS2-VASc scoring system, and the CHA2DS2-VASc score only reflects the presence or absence of risk factors rather than the actual impact caused by the duration of the risk factor itself. The same risk factor in older AF patients may therefore have a more obvious impact on the risk of stroke than in younger AF patients, since the same risk factor may have already existed in the older AF patients for more than several decades. Old age is associated with the severity of vascular endothelial dysfunction and contributes to the formation of vascular atherosclerosis and abnormal homeostasis.[23–29] Therefore, aging itself may have a more important impact in contributing to the risk of ischemic stroke and disease severity compared to other risk factors. Our results indicated a cut-off point in the cumulative event rate of ischemic stroke/systemic emboli between the male AF patients younger than 50 years of age and those 50 to 64 years of age (Fig 2). Considering the risk of major bleeding increases with the duration of anticoagulation therapy, it is essential to incorporate a young age into the scoring scheme to assess the rationale of very long-term anticoagulation therapy for young AF patients compared to older AF patients.
Not all risk factors in the CHA2DS2-VASc score were associated with an equal risk in the AF patients. For the AF patients with single risk factor not due to female (CHA2DS2-VASc score of 1 for males and 2 for females), the risk factor of an age of 65 to 74 years carried a significant risk of a clinical event in both genders (HR, 2.34; 95% CI, 1.82–3.01; P < 0.0001 for males; HR, 2.72; 95% CI, 1.90–3.89; P < 0.0001 for females). For the 9,469 male patients with a CHA2DS2-VASc score of 1 who were 50 to 64 years of age, the HRs of the four risk factors (congestive heart failure, diabetes, hypertension and vascular disease) were comparable (Table 4). For the 5,983 female patients with a CHA2DS2-VASc score of 1 who were 50 to 64 years of age, heart failure had the highest risk of a clinical event (HR, 5.54; 95% CI, 3.13–9.81; P < 0.0001), while vascular disease did not contribute to a higher risk of a clinical event in these patients. Our findings showed that for AF patients with vascular disease alone, the risk of ischemic thromboembolism was significantly increased by 3.81-fold for the male patients aged 50 to 64 years, while it did not increase the risk of clinical events for male patients aged 20 to 49 years or for female patients aged 20 to 49 and 50 to 64 years. The number of young patients with vascular disease was thus limited in our study cohort, which may have decreased the statistical power of vascular disease in predicting the risk of ischemic thromboembolism.
Hypertension and diabetes have been independently and consistently associated with ischemic stroke in AF patients in previous studies.[30–32] Although the presence of congestive heart failure would be expected to increase the risk of ischemic stroke in AF patients based on current pathophysiological concepts, previous studies have indicated that a history of congestive heart failure does not seem to be an independent risk factor for thromboembolism in AF patients.[30–32] However, those studies mainly focused on AF patients overall, and the findings may not be the same when focusing on young AF patients. Our results revealed that congestive heart failure rather than other risk factors such as diabetes, hypertension and vascular disease was the most important risk factor for thromboembolism in young AF patients with one additional risk factor of ischemic stroke in both genders. In addition to the presence or absence of hypertension or diabetes as recorded in the CHA2DS2-VASc score, the severity of hypertension and the duration of diabetes may also influence the absolute stroke rate in AF patients with these disorders. The severity and duration of hypertension or diabetes in young AF patients would be expected to be much lower than in older AF patients, which may explain why these risk factors did not play an important role in determining the risk of thromboembolic events in the young AF patients compared with the older patients. Since the recommendations for anticoagulation treatment in patients with a low CHA2DS2-VASc score are unclear based on the current guidelines, the presence of congestive heart failure may help to assess the rationale of using oral anticoagulants in young AF patients with one additional risk factor.
Limitations
Intrinsic limitations exist in nation-wide cohort study like this. This is registry data and therefore the diagnosis is not strictly re-examined. In addition, the CHA2DS2-VASc score was fixed once the patient had been diagnosed with AF in this study. However, the CHA2DS2-VASc score may change dynamically with time.
Conclusions
Age is an important factor in determining the risk of ischemic thromboembolism in AF patients with low CHA2DS2-VASc scores (1 for male or 2 for female). The annual and cumulative risks of ischemic thromboembolism in male AF patients less than 50 years old were very low and similar to the AF patients without any additional risk factors (CHA2DS2-VASc score = 0). Considering the benefits and costs including the risk of bleeding, oral anticoagulation therapy may not be favorable or should be used individually in these patients.
Supporting Information
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by CMRPG3B0991 and CMRPG3E0291. https://www.cgmh.org.tw/. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lin HJ, Wolf PA, Kelly-Hayes M, Beiser AS, Kase CS, Benjamin EJ, et al. Stroke severity in atrial fibrillation. The Framingham Study. Stroke. 1996;27(10):1760–4. . [DOI] [PubMed] [Google Scholar]
- 2.Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137(2):263–72. 10.1378/chest.09-1584 . [DOI] [PubMed] [Google Scholar]
- 3.Olesen JB, Lip GY, Hansen ML, Hansen PR, Tolstrup JS, Lindhardsen J, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342:d124 10.1136/bmj.d124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olesen JB, Torp-Pedersen C, Hansen ML, Lip GY. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study. Thromb Haemost. 2012;107(6):1172–9. 10.1160/TH12-03-0175 . [DOI] [PubMed] [Google Scholar]
- 5.Chao TF, Lin YJ, Tsao HM, Tsai CF, Lin WS, Chang SL, et al. CHADS(2) and CHA(2)DS(2)-VASc scores in the prediction of clinical outcomes in patients with atrial fibrillation after catheter ablation. J Am Coll Cardiol. 2011;58(23):2380–5. 10.1016/j.jacc.2011.08.045 . [DOI] [PubMed] [Google Scholar]
- 6.Chao TF, Liu CJ, Chen SJ, Wang KL, Lin YJ, Chang SL, et al. Atrial fibrillation and the risk of ischemic stroke: does it still matter in patients with a CHA2DS2-VASc score of 0 or 1? Stroke. 2012;43(10):2551–5. 10.1161/STROKEAHA.112.667865 . [DOI] [PubMed] [Google Scholar]
- 7.Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012;33(21):2719–47. 10.1093/eurheartj/ehs253 . [DOI] [PubMed] [Google Scholar]
- 8.Jung BC, Kim NH, Nam GB, Park HW, On YK, Lee YS, et al. The Korean Heart Rhythm Society's 2014 Statement on Antithrombotic Therapy for Patients with Nonvalvular Atrial Fibrillation: Korean Heart Rhythm Society. Korean Circ J. 2015;45(1):9–19. 10.4070/kcj.2015.45.1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones C, Pollit V, Fitzmaurice D, Cowan C, Guideline Development G. The management of atrial fibrillation: summary of updated NICE guidance. BMJ. 2014;348:g3655 10.1136/bmj.g3655 . [DOI] [PubMed] [Google Scholar]
- 10.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr., et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071–104. 10.1161/CIR.0000000000000040 . [DOI] [PubMed] [Google Scholar]
- 11.Lin LJ, Cheng MH, Lee CH, Wung DC, Cheng CL, Kao Yang YH. Compliance with antithrombotic prescribing guidelines for patients with atrial fibrillation—a nationwide descriptive study in Taiwan. Clin Ther. 2008;30(9):1726–36. 10.1016/j.clinthera.2008.09.010 . [DOI] [PubMed] [Google Scholar]
- 12.Chang CH, Lee YC, Tsai CT, Chang SN, Chung YH, Lin MS, et al. Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis. 2014;232(1):224–30. 10.1016/j.atherosclerosis.2013.11.036 . [DOI] [PubMed] [Google Scholar]
- 13.Maaijwee NA, Rutten-Jacobs LC, Schaapsmeerders P, van Dijk EJ, de Leeuw FE. Ischaemic stroke in young adults: risk factors and long-term consequences. Nat Rev Neurol. 2014;10(6):315–25. 10.1038/nrneurol.2014.72 . [DOI] [PubMed] [Google Scholar]
- 14.Lin CC, Lai MS, Syu CY, Chang SC, Tseng FY. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J Formos Med Assoc. 2005;104(3):157–63. . [PubMed] [Google Scholar]
- 15.Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20(3):236–42. 10.1002/pds.2087 . [DOI] [PubMed] [Google Scholar]
- 16.Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Med Assoc. 2015;114(3):254–9. 10.1016/j.jfma.2013.09.009 . [DOI] [PubMed] [Google Scholar]
- 17.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51. 10.1056/NEJMoa0905561 . [DOI] [PubMed] [Google Scholar]
- 18.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91. 10.1056/NEJMoa1009638 . [DOI] [PubMed] [Google Scholar]
- 19.Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92. 10.1056/NEJMoa1107039 . [DOI] [PubMed] [Google Scholar]
- 20.Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104. 10.1056/NEJMoa1310907 . [DOI] [PubMed] [Google Scholar]
- 21.Lip GY, Wang KL, Chiang CE. Non-vitamin K antagonist oral anticoagulants (NOACs) for stroke prevention in Asian patients with atrial fibrillation: time for a reappraisal. Int J Cardiol. 2015;180:246–54. 10.1016/j.ijcard.2014.11.182 . [DOI] [PubMed] [Google Scholar]
- 22.Wolf PA, D'Agostino RB, O'Neal MA, Sytkowski P, Kase CS, Belanger AJ, et al. Secular trends in stroke incidence and mortality. The Framingham Study. Stroke. 1992;23(11):1551–5. . [DOI] [PubMed] [Google Scholar]
- 23.Higashi Y, Kihara Y, Noma K. Endothelial dysfunction and hypertension in aging. Hypertens Res. 2012;35(11):1039–47. 10.1038/hr.2012.138 . [DOI] [PubMed] [Google Scholar]
- 24.Sohrabji F, Bake S, Lewis DK. Age-related changes in brain support cells: Implications for stroke severity. Neurochem Int. 2013;63(4):291–301. 10.1016/j.neuint.2013.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayhan WG, Arrick DM, Sharpe GM, Sun H. Age-related alterations in reactivity of cerebral arterioles: role of oxidative stress. Microcirculation. 2008;15(3):225–36. 10.1080/10739680701641421 . [DOI] [PubMed] [Google Scholar]
- 26.Park L, Anrather J, Girouard H, Zhou P, Iadecola C. Nox2-derived reactive oxygen species mediate neurovascular dysregulation in the aging mouse brain. J Cereb Blood Flow Metab. 2007;27(12):1908–18. 10.1038/sj.jcbfm.9600491 . [DOI] [PubMed] [Google Scholar]
- 27.Modrick ML, Didion SP, Sigmund CD, Faraci FM. Role of oxidative stress and AT1 receptors in cerebral vascular dysfunction with aging. Am J Physiol Heart Circ Physiol. 2009;296(6):H1914–9. 10.1152/ajpheart.00300.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pena Silva RA, Chu Y, Miller JD, Mitchell IJ, Penninger JM, Faraci FM, et al. Impact of ACE2 deficiency and oxidative stress on cerebrovascular function with aging. Stroke. 2012;43(12):3358–63. 10.1161/STROKEAHA.112.667063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blum A, Vaispapir V, Keinan-Boker L, Soboh S, Yehuda H, Tamir S. Endothelial dysfunction and procoagulant activity in acute ischemic stroke. J Vasc Interv Neurol. 2012;5(1):33–9. [PMC free article] [PubMed] [Google Scholar]
- 30.Stroke Risk in Atrial Fibrillation Working G. Independent predictors of stroke in patients with atrial fibrillation: a systematic review. Neurology. 2007;69(6):546–54. 10.1212/01.wnl.0000267275.68538.8d . [DOI] [PubMed] [Google Scholar]
- 31.Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–70. . [DOI] [PubMed] [Google Scholar]
- 32.Stroke Risk in Atrial Fibrillation Working G. Comparison of 12 risk stratification schemes to predict stroke in patients with nonvalvular atrial fibrillation. Stroke. 2008;39(6):1901–10. 10.1161/STROKEAHA.107.501825 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.