Abstract
HIV prevalence is eight times higher in young South African women compared to men. Grassroot Soccer (GRS) developed SKILLZ Street (SS), a single-sex intervention using soccer to improve self-efficacy, HIV-related knowledge, and HIV counselling and testing (HCT) uptake among girls ages 12–16. Female community leaders—“coaches”—deliver ten 2-hour sessions bi-weekly. Attendance and HCT data were collected at 38 programmes across 5 GRS sites during 24 months in 2011–2012. 514 participants completed a 16-item pre/post questionnaire. Focus group discussions (FGDs) were conducted with participants (n=11 groups) and coaches (n=5 groups), and coded for analysis using NVivo. Of 1,953 participants offered HCT, 68.5% tested. Overall, significant pre/post improvement was observed (p<0.001). FGDs suggest participants: valued coach-participant relationship; improved self-efficacy, HIV-related knowledge, communication, and changed perception of soccer as a male-only sport; and increased awareness of testing’s importance. Results suggest SS helps at-risk girls access HCT and HIV-related knowledge while promoting self-confidence.
Keywords: South Africa, HIV/AIDS, HIV education, girls’ empowerment, sport, sexual reproductive health and rights
Background
Across sub-Saharan Africa, HIV prevalence among young people ages 15–24 fell by 42% from 2001 to 2012 (UNAIDS 2013). However, HIV prevalence among young women continues to be more than twice as high as among young men (UNAIDS 2013). In South Africa, trends in HIV prevalence among young people mirror these global trends. Yet, the disproportionate impact of HIV on young women is more severe: HIV prevalence among young women ages 15–19 is eight times higher than among young men of the same age (Shisana et al. 2014).
While women are more vulnerable to HIV than men given the physiology of the female genital tract, women are also at higher risk due to various cultural and societal norms (Jewkes, Dunkle, et al. 2010; Ramjee and Daniels 2013; UNAIDS 2013). Inter-related factors influencing HIV risk among female adolescents include high prevalence of reported gender-based violence, age-disparate sex, and multiple partnerships (Jewkes, Dunkle, et al. 2010; Shisana et al. 2014; UNAIDS 2013). Research has shown that these factors stem from a cultural setting of gender inequality and male dominance through violence and control. These cultural norms reduce women’s ability to choose when and with whom to have sex and to protect themselves in sexual encounters (Jewkes, Dunkle, et al. 2010; Jewkes and Morrell 2010). Additionally, women face barriers in accessing health services due to economic constraints, cultural norms, and gender-related discrimination (Nudelman 2013; UNAIDS 2013).
Despite evidence of disproportionately high HIV risk among female adolescents, prevention agendas continue to focus on promotion of male condom use, treatment for STIs, HIV testing, and more recently male circumcision and antiretroviral treatment (Jewkes, Dunkle, et al. 2010). Most youth-targeted HIV prevention programmes do not place attention on the gender-sensitive aspects of the HIV epidemic (Jewkes, Dunkle, et al. 2010). In response, there has been a movement to promote and mainstream gender in HIV/AIDS programming (UNAIDS 1999; WHO 2003). In 2011, the UN Political Declaration on HIV/AIDS stated that addressing gender inequalities is a critical component of an effective HIV response for women. While 100 out of 109 reporting countries in 2013 indicated that elimination of gender inequalities is a national priority, country policies and resource allocation within these countries is lagging behind (UNAIDS 2013). In particular, the need to promote women’s access to HIV prevention services, such as HIV testing, is not being sufficiently met (UNAIDS 2013; WHO 2003).
Single-sex HIV prevention programming has been shown to be effective in building girls’ self-confidence and self-efficacy for self-care and protection from HIV (UNAIDS 1999; UNFPA 2003). Since the HIV risks for females and males stem from harmful cultural and societal norms, discussions around risk avoidance need to be gender-specific (Jewkes, Dunkle, and et al. 2010; UNAIDS 1999; WHO 2003). An important component of girls-only programming is the construction and maintenance of a ‘safe space,’ allowing participants to feel comfortable speaking among peers and constructing a public voice. Safe space is particularly important for girls who are often taught to be quiet or passive in front of boys (Brady and Arjmand 2002; UNFPA 2003). Participants in girls-only HIV prevention programmes were found better able to express an opinion and ask questions than in mixed-sex groups (Busayawong et al. 1996).
While single-sex HIV education interventions have been shown to be effective in educating girls, increasing access to health services is another important aspect of a comprehensive HIV prevention approach, especially for girls and women (UNAIDS 2013; WHO 2013). HIV Counselling and Testing (HCT) is regarded as a highly valued and effective HIV prevention strategy (Croce-Galis et al. 2014; Rosenberg et al. 2013). Exposure to HCT has been shown to increase safe sexual behaviours and reduce risk of HIV acquisition among youth (Croce-Galis et al. 2014; Rosenberg et al. 2013). HCT has also been shown to promote greater social acceptance and destigmatization of the HIV/AIDS epidemic (De Kock and Johnson 1998). Guidelines on HIV testing recommend that HCT be widely accessible on a voluntary and confidential basis (Mashale et al. 2012; UNAIDS 2001; WHO 2013).
In South Africa, HCT has been available since the early 1990s. In 2000, expansion of HCT services within the public health sector was initiated as part of the national strategic plan on HIV/AIDS and STIs (Birdsall et al. 2004). In 2006, the President assented to the South African Children’s Act, mandating that children over the age of 12 could legally access health care services, including HIV testing, without parental consent.
However, HCT uptake in South Africa remains low, especially among adolescents. In a 2014 survey, only 50.6% of adolescents ages 15–24 reported having ever been tested for HIV, although 90.5% reported awareness of an HIV testing site nearby (Shisana et al. 2014). Major barriers to willingness to access HCT services include fear of being seen at a healthcare facility, transport difficulties, stigma of testing positive, and concerns about confidentiality (Obermeyer and Osborn 2007). Increasing access to and acceptability of HCT among adolescents, particularly by creating adolescent-friendly testing environments, is a priority (WHO 2013). Incorporating HCT events into a single-sex HIV prevention intervention could be a novel and effective approach to increase HCT uptake among adolescent girls.
Sport-based HIV prevention
Interest is growing internationally in the use of sport-based HIV prevention (SBHP) approaches to change behaviour and improve health outcomes (Kaufman, Spencer, and Ross 2012). Sport provides an engaging and accessible platform to spread health information and foster life skills necessary for knowledge, attitude, and behavioural change (Khan 2010; Koss and Alexandrova 2005). Additionally, a recent study that found SBHP organizations can play an important role in increasing HCT uptake among youth (Mashale et al. 2012).
Incorporating sports into HIV prevention programming may have additional benefits for girls and women. Evidence shows that sport participation is linked with decreased reporting of risky sexual behaviour, increased reporting of health-seeking behaviour, and increased self-efficacy and self-esteem among girls and women in the United States (Lehman and Koerner 2004; Sabo et al. 1999; Taliaferro et al. 2010). Globally, however, girls and women have historically experienced limited opportunity to participate in sport (Brady 1998, 2005; Hancock, Lyras, and Ha 2013). In low- and middle-income countries, there is a need to investigate whether girls-only SBHP interventions can effectively build self-efficacy among adolescent girls to avoid risky sexual behaviours and adopt health-seeking behaviours, such as HIV testing (Brady 1998).
One SBHP organization, Grassroot Soccer (GRS), implements soccer-based HIV prevention interventions in schools across sub-Saharan Africa. The GRS model and the efficacy of GRS’s mixed-sex SBHP programming in sub-Saharan Africa have been documented previously (Clark et al. 2006; Fuller, Junge, Dorasami, et al. 2011; Kaufman, Spencer, and Ross 2012). In this article, we aim to present findings from a mixed-methods study evaluating the efficacy of SKILLZ Street (SS), GRS’s girls-only SBHP programme.
The SKILLZ Street intervention: Conception, launch and development
In response to the disproportionate impact of HIV on young women, GRS developed a girls-only SBHP intervention, called SKILLZ Street (SS), in 2010. SS is structured as an after-school educational intervention consisting of 10 two-hour sessions, integrating soccer, life skills activities, and voluntary HCT offered by local testing partners. Soccer is included to enable adolescent girls to challenge the common South African belief that soccer is a male-only sport. Young role models, or ‘coaches,’ are recruited from the local communities to deliver SS. Specifically, the intervention aims to: (1) increase self-efficacy to avoid risky sexual behaviour, (2) increase belief in gender-equitable norms, and (3) facilitate access to and uptake of HCT services.
GRS’s methodology is based on Bandura’s Social Learning Theory (1977), which posits that observational learning allows one to develop an idea of how a new behaviour is formed without actually performing the behaviour oneself. Additionally, the observer is most likely to model behaviours of people that are most like themselves. This concept provides the core rationale behind the programme’s use of slightly older peer educators (coaches) from the same community. Coaches undergo significant training to prepare them to provide positive and healthy models of behaviour for SS participants, allowing participants to ‘transcend the boundaries of their own environment’ (1986).
The SS curriculum and programme design was developed in 2010 through a pilot at GRS’s site in Khayelitsha, South Africa. The initial development process followed what a 2012 DFID report on theories of change later described as an evolutionary model of change (Vogel 2012). GRS introduced various activities into the initial SS intervention (e.g. community outreach, soccer, guest speakers, educational videos), with the ‘promising activities selected by the team or by natural selection’ and then sought to amplify the activities that survived (Vogel 2012).
After the SS pilot in 2010, the programme was scaled-up in January 2011 for delivery in five GRS South Africa peri-urban sites. Data collected and presented here were used to inform curriculum development, with key changes including the addition of content on sexual reproductive health and rights (SRHR) and the involvement of females only as coaches (rather than recruiting male and female coaches).
The aim of this paper is to contribute to literature on the effectiveness of SBHP and to help inform the development of future single-sex HIV prevention programmes.
Methods
Intervention design
At the time of data collection, each of the ten SS practices consisted of a life skills activity, a soccer session, and informal ‘team time’ sessions facilitated by coaches. The SS programme was led by 10 coaches and targeted about 100 participants. GRS staff recruited participants on a voluntary basis from local schools through an assembly or class presentation. During the first session or ‘practice,’ each female coach was assigned a team of 10 participants. Throughout the rest of the programme, each coach led ‘team time’ and life skills sessions with her team. During soccer sessions, teams paired up to play a non-competitive soccer match. Life skills activity topics included: body image; SRHR knowledge; HIV-related knowledge; and decision-making in relationships. The seventh practice integrated an HCT event, during which external testing partners were invited to the SS venue, and participants were given the opportunity to get tested for HIV with a counsellor present.
SS coaches participated in at least 80 hours of training, led by local GRS staff before implementing SS. The training focused on building HIV and SRHR knowledge, facilitation techniques, and skills in working with youth.
Data collection
Quantitative and qualitative data were collected between January 2011 and December 2012 at five GRS sites in peri-urban areas across four provinces in South Africa: Alexandra, Khayelitsha, Kimberley, Port Elizabeth, and Soweto.
Quantitative data
Attendance and HIV testing data
Attendance and HIV testing data were collected from 38 programmes from January 2011 through December 2012. At every programme, each coach filled out an ‘Attendance Register’ with each participant’s name, age and sex. Every quarter, attendance data were uploaded by GRS staff to a cloud-based platform called Salesforce for monitoring purposes. Testing data were provided to GRS by the external HCT partners invited to the HCT event. The main outcomes we assessed were: (1) graduation rate defined as number of persons who attended at least seven sessions over the total number of participants who attended at least one session, and (2) HCT rate defined as the number of participants who completed HCT over the total number of participants who attended at least one session at a programme that hosted an HCT event.
Questionnaire data
A random sample of SS participants completed a 16-item self-administered HIV-related knowledge, attitudes and communication questionnaire immediately before and after participation in the programme in 2012 (n=514, mean age =14.2 years). The highest percentages of questionnaires were administered in Soweto (31%) and Khayelitsha (31%) (Figure 1). To determine whether there was evidence of improvement in the responses to the questionnaire, analysis of questionnaire data was performed using a chi square test.
Figure 1.
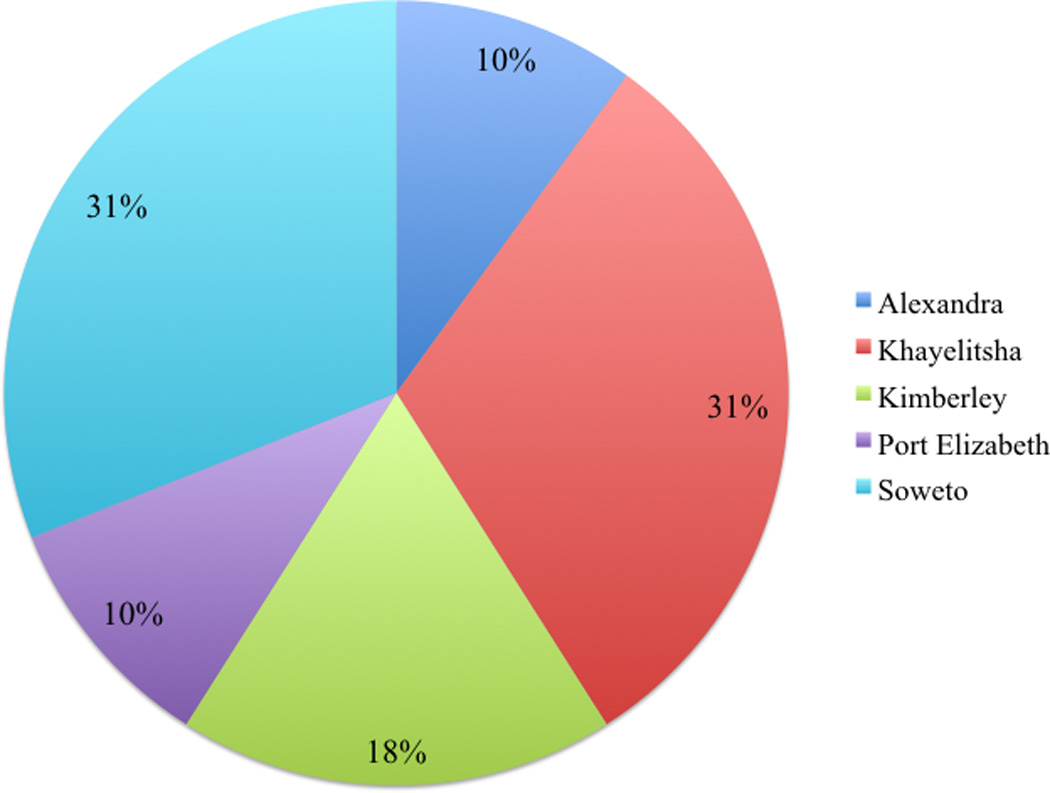
Percentage of questionnaires administered between five GRS South Africa sites, 2012.
Qualitative data
Focus group discussions
Sixteen focus group discussions (FGDs) were conducted with participants (n=11 groups) and coaches (n=5 groups) within two weeks of a programme’s completion. FGDs lasted between 30 and 90 minutes and were held in two rounds, taking place in December 2011 and December 2012. Discussions explored: views on the programme structure and implementation; knowledge acquired; and suggested topics to be addressed in the curriculum. SS participants were selected to participate from different teams to avoid bias related to perceptions of their coaches. Both participants and coaches were purposively sampled to include those who appeared comfortable expressing themselves. Sampling for FGDs may have introduced selection bias, as only those who completed the programme were selected. Additionally, participants and coaches who enjoyed the programme may have been more likely to be expressive than those who disliked or did not enjoy the programme. Staff facilitated FGDs with participants and coaches. FGDs were recorded, translated, and transcribed. Transcripts were coded for analysis by a four-person team using NVivo 10 software.
Voluntary and informed consent
GRS staff obtained both written parental consent and verbal participant assent for all participants regarding involvement in the SS programme. During recruitment, potential participants were provided verbal and written information about the SS programme before being asked to assent to participate.
Prior to the HCT event, participants were given an additional informed consent form to remind and invite participants’ parents or guardians about the upcoming HCT event. All participants were required to verbally assent to get HIV tested.
Additionally, participants that completed the questionnaire or participated in a FGD were asked to assent to participate. Participants were informed that they could end the questionnaire or leave the FGD at any time or skip over any questions they did not wish to answer.
Results
Attendance data
In total, 4,260 participants were enrolled in SS in 2011 and 2012, and 86.3% attended at least seven sessions and were eligible to graduate (n=3,678) (Table 1). The remaining 13.7% of participants were not eligible to graduate as they attended six sessions or less. The number of graduates and percent graduate rate varied from 2011 to 2012 at every GRS site.
Table 1.
Data collected regarding attendance at SS programmes implemented at five South Africa GRS sites by year, 2011–2012.
| Site | # Programmes |
# Participants |
# Graduates (% Rate) |
Average # participants per programme |
Average # graduates per programme |
|
|---|---|---|---|---|---|---|
| Alexandra | 3 | 403 | 338 (83.9%) |
134 | 113 | |
| 2012 | 3 | 403 | 338 (83.9%) |
134 | 113 | |
| Khayelitsha | 14 | 1,237 | 1,160 (93.8%) |
88 | 83 | |
| 2011 | 6 | 668 | 617 (92.4%) |
111 | 103 | |
| 2012 | 8 | 569 | 543 (95.4%) |
71 | 68 | |
| Kimberley | 9 | 1,155 | 996 (86.2%) |
128 | 111 | |
| 2011 | 4 | 445 | 416 (93.5%) |
111 | 104 | |
| 2012 | 5 | 710 | 580 (81.7%) |
142 | 116 | |
| Port Elizabeth | 7 | 785 | 633 (80.6%) |
112 | 90 | |
| 2011 | 4 | 476 | 399 (83.8%) |
119 | 100 | |
| 2012 | 3 | 309 | 234 (75.7%) |
103 | 78 | |
| Soweto | 8 | 680 | 551 (81.0%) |
85 | 69 | |
| 2011 | 3 | 225 | 179 (75.7%) |
75 | 60 | |
| 2012 | 5 | 455 | 372 (81.8%) |
91 | 74 | |
| TOTAL | 38 | 4,260 |
3,678 (86.3%) |
112 | 97 | |
In 2011, graduates on average were 12.3 years old, with a majority (71%) between 11 and 13 years old. In 2012, graduates on average were 13.5 years old with a majority (69%) between 12 and 14 years old.
HIV testing data
GRS hosted 17 HCT events at 38 SS programmes held between January 2011 and December 2012 (Table 2). GRS was not able to arrange HCT events at every programme across the sites due to refusals by the participating schools, testing partners or parents to test youth under the age of 18. The GRS sites in Alexandra and Port Elizabeth were unable to host any HCT events. When an HCT event could not be held, GRS staff would organize a guest speaker from a local clinic or a review session to take the place of the seventh session. Overall, there were 1,953 total participants at SS programmes that hosted HCT events, of which 68.5% were tested for HIV (n=1,338). Across 2011 and 2012, the percentage of SS participants that were tested for HIV are similar in all sites except for Soweto, where a lower percentage of participants were tested in 2012 (57.4%) than in 2011 (64.4%).
Table 2.
Data collected on SS HCT events hosted at three South Africa GRS sites by year, 2011–2012.
| Site | # HCT events |
# Participants* | # Participants HIV tested |
% Participants HIV tested |
|
|---|---|---|---|---|---|
| Khayelitsha | 11 | 1004 | 777 | 77.4% | |
| 2011 | 6 | 668 | 517 | 77.4% | |
| 2012 | 5 | 336 | 260 | 77.4% | |
| Kimberley | 3 | 541 | 311 | 57.5% | |
| 2011 | 2 | 445 | 257 | 57.8% | |
| 2012 | 1 | 96 | 54 | 56.3% | |
| Soweto | 3 | 408 | 250 | 61.3% | |
| 2011 | 2 | 225 | 145 | 64.4% | |
| 2012 | 1 | 183 | 105 | 57.4% | |
| TOTAL | 17 | 1,953 | 1,338 | 68.5% | |
Note:
denotes number of participants who attended one or more SS practice at a programme that hosted an HCT event
Questionnaire data
Of the 16 items in the questionnaire, strong evidence of improvement was observed on 14 items related to HIV-related knowledge, attitudes, and communication (Table 3).
Table 3.
Baseline and endline analysis on questionnaire data, 2012.
| Communication about HIV/AIDS | Baseline | Endline | P Value |
| Q1. I have talked to a friend about HIV in the past 2 months (outside of SKILLZ Street). | 38% | 54% | <0.001 |
| Q2. There is no one I can talk to if I have a problem. | 80% | 84% | 0.014 |
| Gender-equitable norms and HIV-related attitudes | Baseline | Endline | P Value |
| Gender-equitable norms | |||
| Q3. A girl’s opinion is as important as a guy’s. | 54% | 64% | <0.001 |
| Q4. It is the man’s responsibility to make decisions in a relationship. | 80% | 83% | 0.081 |
| HIV-related attitudes | |||
| Q5. I can say no to sex without a condom, even if I am pressured. | 82% | 89% | <0.001 |
| Q6. I have the right to say no to sex if I don’t want it. | 94% | 97% | <0.001 |
| Q7. I would support a friend, even if they have HIV. | 95% | 96% | 0.309 |
| Q8. I believe I have many good qualities. | 85% | 89% | 0.005 |
| Q9. I can explain my goals to others. | 88% | 92% | 0.004 |
| Q10. I believe I will complete my Grade 12. | 95% | 98% | 0.003 |
| HIV prevention knowledge | Baseline | Endline | P Value |
| Q11. I know where to go for family planning services in my community. | 62% | 84% | <0.001 |
| Q12. Unprotected sex is the most common way HIV is spread in my community. | 84% | 88% | 0.008 |
| Q13. As a girl I have a greater risk of getting HIV than guys my age. | 46% | 70% | <0.001 |
| Q14. Having an older partner increases my risk of getting HIV. | 80% | 91% | <0.001 |
| Q15. Having more than one sexual partner at the same time increases my risk of getting HIV. | 83% | 90% | <0.001 |
| Q16. If a girl is sexually violated, she can reduce her risk of getting HIV by taking Post-Exposure Prophylaxis (PEP) 1 to 3 days afterwards. | 29% | 74% | <0.001 |
| TOTAL | 74% | 84% | <0.001 |
Communication about HIV
At baseline, 38% of participants reported that they had communicated about HIV with a peer in the past 2 months, and 80% of participants reported that they were able to communicate with someone when faced with a problem. Very strong evidence of improvement was observed in communication about HIV with a peer (p<0.001), and strong evidence of improvement was observed in ability to communicate with someone when faced with a problem (p<0.014).
Gender-equitable norms and HIV-related attitudes
The questionnaire data showed evidence of improvement in participants’ attitudes. Very strong evidence of improvement in gender-equitable responses was observed for Question 3, regarding whether a girl’s opinion is as important as a boy’s opinion (p<0.001). Weak evidence of improvement in greater gender-equitable beliefs was observed on Question 4, regarding whether it is the man’s responsibility to make decisions in a relationship (p=0.081).
The remaining attitude-focused questionnaire items were intended to measure self-efficacy, stigma, and self-confidence among participants. Very strong evidence of improvement in self-efficacy to avoid risky sexual behaviour was observed for Questions 5 and 6 (p<0.001). For Question 7, 95% of participants reported supportive attitudes towards people living with HIV at baseline, yet there was weak evidence of improvement observed after the programme (p=0.309). For Questions 8, 9, and 10, strong evidence of improvement in self-confidence and self-efficacy to voice and achieve educational goals was observed (p<0.01).
HIV prevention knowledge
The questionnaire data demonstrated strong evidence of improvement in HIV prevention knowledge (p<0.01). Very strong evidence of improvement in knowledge was observed on Question 11 regarding location of family planning services in the community (p<0.001), Question 13 regarding high HIV risk for young women as compared to young men (p<0.001), and Question 16 regarding the benefits of using Post-Exposure Prophylaxis (PEP) (p<0.001).
For the remaining three knowledge questionnaire items, strong evidence of improvement in knowledge was observed (p<0.01) regarding the high HIV risks associated with the following: unprotected sex (Q12); having an older sexual partner (Q14); and having multiple concurrent sexual partners (Q15).
Focus group discussions
Knowledge among participants
During FGDs, when participants were asked what they learned in SS, the majority responded that they knew how to better protect themselves from HIV. Participants commonly specified abstinence and PEP as HIV prevention methods. Additionally, participants said they learned about SRHR, referring to menstruation, pregnancy prevention methods, and risk reduction strategies to avoid abuse or rape. ‘Especially in SA, there’s a lot of teenage pregnancy. And, [through SS], we get to know you can abstain (Female participant, Khayelitsha, 2012).’ For the majority of participants, the knowledge they received through the life skills activities was the primary reason they gave for attending and completing SS.
Attitudes among participants
In FGDs, many participants explained that they had experienced positive changes in attitudes through SS. ‘[SS] has made us gain more confidence in ourselves and prepared us mentally on how should we face the challenges of life out there (Female participant, Alexandra, 2012).’ Mostly, participants attributed these changes in self-confidence to coach-led discussions that took place during SS life skills activities.
[The coaches] taught me how wonderful it is being a woman. Being a woman is not all about having sex or being with boys, but you must at least know your body, how your body works and what happens in your body, how to protect yourself and how to say ‘No!’ (Female participant, Kimberley, 2012)
Communication among participants
FGDs suggest that SS increased communication between participants and their peers and/or family members about topics including sex, HIV prevention, and SRHR. For some participants, their experience at SS helped them to identify and connect with people outside of the programme.
[A participant] told the mother about the whole programme of [SS], because the mother was unable to speak to her child about issues, such as HIV and menstrual cycle, and the mother was pleased with the work of [SS]. (Female coach, Port Elizabeth, 2011)
Some participants also discussed the absence of reliable female role models and supporters in their lives.
I feel comfortable speaking with my [SS] coaches, because when I speak with my mom, it’s like I’m getting out of the way, I’m getting rude. I’m just not used to being open with my mom in that way, so I feel comfortable with my [SS] coaches. (Female participant, Kimberley, 2012)
Views of SS intervention
Soccer
During FGDs, participants and coaches stated that they felt soccer was an important part of SS. Participants explained that their experience playing soccer at SS changed their perception of soccer as a male-only sport.
I love the part of soccer, it helped me a lot and it showed again us girls…we can also make our dreams come true with soccer. It’s not only for boys, but it’s also for us… (Female participant, Kimberley, 2012)
Some coaches did not enjoy leading soccer sessions, because they were unfamiliar with the sport. ‘[Soccer sessions are] unfair, because we are not masters of soccer, but we’re teaching the girls how to play soccer (Female coach, Khayelitsha, 2012).’ Other coaches felt their participants appreciated that they were not highly skilled soccer players. ‘With a girl in charge, they just feel really free. They feel that their coach doesn’t even know soccer, so we can learn together (Female coach, Soweto, 2011).’
Coach-participant relationship
Qualitative data suggests that participants highly valued the relationships they built with their coaches. Participants felt comfortable talking to coaches about challenges they faced in their communities, often related to relationships, alcohol use or sex. They commonly shared the following reasons for this heightened level of comfort: (1) coaches were friendly and approachable; (2) coaches encouraged and praised participants for expressing themselves; and (3) coaches were females. ‘We got empowered. [We were] appreciated by our coaches throughout the entire programme (Female participant, Alexandra, 2012).’
During FGDs in 2011, coaches and participants were asked whether male coaches should be involved in SS. Most of the female coaches responded that the presence of male coaches would be detrimental to the ‘safe space’ built among a girls-only group. Participants also expressed a similar opinion during FGDs. One participant stated: ‘[I prefer a] female coach because they can relate to us and we can tell them about all the challenges girls face (Female participant, Alexandra, 2012).’
Coaches also highly valued the coach-participant relationship and felt that building trust with participants was important, because participants would be more willing to listen and follow the health behaviour messaging. Coaches cited the following as effective ways to build meaningful relationships with participants: (1) be attentive and (2) be honest and open. ‘Usually, at home, [girls] don’t get personal connection with their parents, because the parents are always tired. But, coaches give them the special time (Female coach, Khayelitsha, 2011).’
Both participants and coaches often mentioned the importance of the coach-participant relationship in relation to the HCT event. Many participants attributed their willingness to test with the support they received from their coaches. ‘Mostly, we tested because the coaches were supportive – they supported us, and we felt like it was the right thing to do. It’s right to know your status (Female participant, Khayelitsha 2012).’
HCT event
Qualitative data suggests that participants whom attended an HCT event felt they were better prepared to protect themselves from getting HIV. ‘ The testing part is going to help us use condoms, now that we know our status (Female participant, Khayelitsha 2012).’
While coaches supported the inclusion of the HCT event in the SS intervention, they offered multiple suggestions for improvement when planning and hosting the HCT event at SS. One common recommendation was to ensure that participants’ parents attended the HCT event.
I think we should get parents involved [in the HCT], it would be very nice because the kids won’t be afraid to test, and the parent will know, because they don’t have the idea – they don’t know the importance of testing. (Female coach, Kimberley, 2011)
Coaches also felt that the HCT protocol should be adjusted in order to maintain confidentiality. They shared examples from previous HCT events where external testing partners organized the space in such a way that participants could become aware of their peers’ HIV status.
I think that to improve, testing should be individual. A child should go in alone, and get her results alone…Group counselling is okay, but when you test you should go alone. The way it happened now, it wasn’t really confidential. Confidentiality is bridged when we have group testing. (Female coach, Soweto, 2011)
Additionally, coaches said that they felt unprepared to support their participants during the HCT event. Many coaches requested a formal HIV counselling training.
Discussion
Findings suggest that a girls-targeted SBHP intervention offers a promising approach towards improving adolescent girls’ HIV-related knowledge, attitudes and communication, and increasing HCT uptake. The data presented here highlight the importance of creating a girls-only ‘safe space’ and utilizing young female community leaders as facilitators of HIV prevention and empowerment activities.
Both the quantitative and qualitative findings demonstrate that adolescent girls experience low levels of communication with peers around HIV and often lack access to female role models. Qualitative data suggests that the coach-participant relationships built at SS provide a valuable and unique communication point for participants to ask sensitive questions. Furthermore, findings demonstrate that SS participation can lead to increased communication among participants with adults and peers outside of the programme. Strong evidence of improvement in participants’ communication with peers about HIV was observed (p<0.001). The qualitative data suggests that by virtue of creating this ‘safe space’ where girls have the opportunity to seek help and learn, girls may become more likely to build similar relationships with other women in their lives, such as with sisters or mothers.
The HIV testing data further strengthens the argument that the girls-only space and coach-participant relationship has an effect on girls’ attitudes and decision-making. Qualitative data shows that participants felt comfortable opting to take an HIV test at these events due to support and role modeling from their coaches. The act of HIV testing seemed to resonate with participants at the end of SS, as it was tangible and experience-based. However, due to the lack of long-term follow-up in this study, we cannot comment on whether participants adopted this healthy behaviour in the long-term.
Although there is limited data on HCT uptake among adolescent girls, a 2014 survey in South Africa revealed that only 50.6% of adolescents ages 15–24 reported having ever been tested for HIV (Shisana et al. 2014). Comparatively, our results indicate that 68.5% of SS participants were tested for HIV at HCT events. In South Africa, national surveys have shown that more females are aware of their HIV status than males, which is generally attributed to the prevention of mother-to-child transmission (PMTCT) of HIV programmes (Shisana et al., 2014). Our findings suggest that girls-targeted HCT events integrated into a larger HIV prevention intervention can effectively increase HCT uptake among adolescent girls. Further research should be conducted to investigate whether this model could be applied to link adolescent boys to HCT services, as well as adolescent girls to other relevant health services, such as family planning or sexual violence support services.
It is important to note that community-level support from relevant stakeholders and health services for HCT events is vital to successful implementation. Although the South African Children’s Act (2006) declares the legality of individuals over the age of 12 getting HIV tested without parental consent, local HIV testing partners and stakeholders often refused to participate in HCT events. Furthermore, some HIV testing partners did not adequately maintain confidentiality. Findings suggest that identification of adequate testing partners is vital and future trainings for coaches should include HIV counselling to increase preparedness. Access to treatment and care for adolescents with HIV also remains insufficient. Following HCT, there are poor linkages to and retention in care for most populations, and ART coverage rates for adolescents are lower than for other age groups. Addressing these challenges and adapting systems to deliver youth-friendly health care and social support are urgently needed (WHO 2013).
Qualitative data suggests that incorporating soccer into a girls-only intervention could be effective at shifting perceptions around the gender norm that soccer is a male-only sport. Both coaches and participants expressed feelings of empowerment from playing soccer, in contrast with their previous experiences observing the exclusion of women from the sport. Future studies should investigate whether a correlation exists between the experience of playing soccer and a change in girls’ perceptions of other harmful gender norms (e.g. girls cannot say no to sex).
The limitations of this study must be noted. First, due to the lack of a control group, we cannot conclude that any observed changes were fully attributable to the intervention. Second, questionnaire and FGD data were collected immediately before and after the six-week SS intervention. Therefore, we are not able to ascertain whether any changes observed were sustained over a long-term period. Third, there may be difficulty in interpreting the questionnaire data due to the small sample size; there were also varying levels of participation across the five GRS sites. Finally, the curriculum and programme design were revised in December 2011 for implementation in January 2012. These changes contributed to the increase in average age among participants, which may have influenced data collected in 2012 (e.g. HIV testing data).
Despite these limitations, the SS programme achieved important success in improving HCT uptake, communication and gender-equitable norms and attitudes. The findings in this study support existing evidence on the importance of delivering single-sex interventions as part of a comprehensive gender-focused HIV prevention programme (WHO 2003). Additionally, our findings suggest that incorporating HCT events into single-sex interventions may be an effective way to engage adolescent youth and promote uptake of health services. Future studies could benefit from including control groups to compare the outcomes of the SS programme with single-sex interventions that do not incorporate soccer or HCT events. This study contributes these valuable findings to the evidence base on gender and HIV prevention.
Acknowledgements
The development, delivery and evaluation of SKILLZ Street were informed by numerous researchers and partners. GRS thanks its many testing and health services partners, including the South African Department of Health, New Start, Partners in Sexual Health (PSH), and MOSAIC, which have provided vital health services to GRS’s young South African SKILLZ Street participants. Many GRS staff members also contributed greatly to this research through programme implementation and data collection – specifically Vuyolwethu Kayi, Boitumelo Rakosa, Annie Shongwe, Christopher Mfiki, Lentswe Ntshegang, Nomathemba Seeku, Lumka Mjana, and Mandisa Nkewu. Additionally, we would like to thank Munro Consulting Actuaries for carrying out the analysis of the questionnaire data.
Funding
This work was supported by Imago Dei; the Elton John AIDS Foundation (EJAF); MAC AIDS Fund; USAID-New Partners Initiative (NPI) under Grant GHO-A-00-09-00002-00; USAID-Public-Private Partnership (PPP) under Grant AID-674-A-12-00007; and USAID-Global Development Alliance (GDA) under Grant AID-OAA-A-12-00085.
Footnotes
Routine monitoring revealed that common reasons given by school administrators, parents, and testing partners included: (1) fear of confidentiality being breached among students with a positive test result; (2) lack of existing structure for health service delivery at school venues; and (3) discomfort providing HIV testing services to youth below the age of 18.
Contributor Information
Rebecca Hershow, Email: rebeccah@grassrootsoccer.org.
Katherine Gannett, Email: katie.gannett@gmail.com.
Jamison Merrill, Email: jamisonmerrill@gmail.com.
Braunschweig Elise Kaufman, Email: elise.braunschweig@gmail.com.
Chris Barkley, Email: cbarkley@grassrootsoccer.org.
Jeff DeCelles, Email: j.decelles@grassrootsoccer.org.
Abigail Harrison, Email: abigail_harrison@brown.edu.
References
- Bandura A. Social Learning Theory. New York: General Learning Press; 1977. [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Birdsall Helen, Nkosi Zinhle, Parker Warren. Voluntary Counselling and Testing (VCT) in South Africa: Analysis of Calls to the National AIDS Helpline. CADRE. 2004 http://www.cadre.org.za/files/CANVCT.pdf. [Google Scholar]
- Brady Martha. Laying the foundation for girls' healthy futures: Can sports play a role? Studies in Family Planning. 1998;29(1):79–82. [PubMed] [Google Scholar]
- Brady Martha. Creating safe spaces and building social assets for young women in the developing world: A new role for sport. Women’s Studies Quarterly. 2005;33(1/2):35–49. [Google Scholar]
- Brady Martha, Arjmand Banu Khan. Letting Girls Play: Mathare Youth Sports Association’s Girls Football Programme. New York: Population Council; 2002. [Google Scholar]
- Busayawong W, et al. HIV/AIDS peer education for Northern Thai single migratory female and male adolescent factory workers. Poster presented at the XI International Conference on AIDS; July 7-12; Vancouver. 1996. [Google Scholar]
- The Presidency. Government of South Africa. No. 38 of 2005: Children’s Act, 2005. Cape Town: Government Gazette; 2006. [Google Scholar]
- Clark Thomas S, Friedrich Gerhard K, Ndlovu Methembe, Neilands Torsten B, McFarland Willi. An adolescent-targeted HIV prevention project using African professional soccer players as role models and educators in Bulawayo, Zimbabwe. AIDS and Behavior. 10(Suppl. 1):77–83. doi: 10.1007/s10461-006-9140-4. [DOI] [PubMed] [Google Scholar]
- Croce-Galis Melanie, Hardee Karen, Gay Jill. Scaling Up Evidence-Informed HIV Prevention for Adolescent Girls and Young Women. Washington DC: Futures Group, Health Policy Project; 2014. http://www,healthpolicyproject,com/pubs/401_WWFWAdolescentPreventionBrief,pdf. [Google Scholar]
- De Kock K, Johnson A. From exceptionalism to normalisation: a reappraisal of attitudes and practice around HIV testing. British Medical Journal. 1998;316:290–293. doi: 10.1136/bmj.316.7127.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department Of Health (DOH) Government of South Africa. 2003. Operational Plan for Comprehensive HIV and AIDS Care, Management and Treatment for South Africa [Google Scholar]
- Fuller CW, Junge A, Dorasami C, DeCelles J, Dvorak J. ‘11 for Health’, a football-based health education programme for children: a two-cohort study in Mauritius and Zimbabwe. British Journal of Sports Medicine. 2011;45:612–618. doi: 10.1136/bjsm.2011.084905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay J, Hardee K, Croce-Galis M, Kowalski S, Gutari C, Wingfield C, Rovin K, Berzins K. What Works for Women and Girls: Evidence for HIV/AIDS Interventions. New York: Open Society Institute; 2010. http://www.whatworksforwomen.org/system/attachments/2/original/what-works-for-women-and-girls.pdf?1278700491. [Google Scholar]
- Hancock M, Lyras A, Ha JP. Sport for Development programmes for girls and women: a global assessment. Journal of Sport for Development. 2013;1(1):15–24. http://jsfdorg/article/sport-for-development-programmes-for-girls-and-women-a-global-assessment/. [Google Scholar]
- Jewkes R, Morrell R. Gender and sexuality: emerging perspectives from the heterosexual epidemic in South Africa and implications for HIV risk and prevention. Journal of the International AIDS Society 9. 2010;13:6. doi: 10.1186/1758-2652-13-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes Rachel K, Dunkle Kristin, Nduna Mzikazi, Shai Nwabisa. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. The Lancet. 2010;376:41–48. doi: 10.1016/S0140-6736(10)60548-X. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)60548-X/fulltext. [DOI] [PubMed] [Google Scholar]
- Kaufman ZA, Spencer TS, Ross DA. Effectiveness of sport-based HIV prevention interventions: a systematic review of the evidence. AIDS and Behavior. 2012 doi: 10.1007/s10461-012-0348-1. [DOI] [PubMed] [Google Scholar]
- Khan Nazir. Football for an HIV-free Generation. Coxswain Social Investment Plus (CSI+); 2010. Using football for HIV/AIDS prevention in Africa. [Google Scholar]
- Koss Johann O, Alexandrova Anna. Essay: HIV/AIDS prevention and peace through sport. The Lancet. 2005;366:S3–S4. doi: 10.1016/S0140-6736(05)67820-8. [DOI] [PubMed] [Google Scholar]
- Lehman Stephanie Jacobs, Koerner Susan Silverberg. Adolescent Women’s Sports Involvement and Sexual Behavior/Health: A Process-Level Investigation. Journal of Youth and Adolescence. 2004;33(5):443–455. [Google Scholar]
- Mashale R, Kelly K, Motuba T, Myers L. TESTING TIMES: A Review of HIV Counselling and Testing within Sports for Development Programmes for Young People in Southern Africa. Centre for AIDS Development, Research and Evaluation (CADRE); 2012. [Google Scholar]
- Nudelman Anita. Gender-Related Barriers to Services for Preventing New HIV Infections Among Children and Keeping Their Mothers Alive and Healthy in High-Burden Countries. Joint United Nations Programme on HIV/AIDS (UNAIDS); 2013. http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2013/201312_discussion-paper_Gender-HIV-services_PMTCT_en.pdf. [Google Scholar]
- Obermeyer Carla Makhlouf, Osborn Michelle. The Utilization Of Testing And Counselling For HIV: A Review Of The Social And Behavioral Evidence. American Journal of Public Health. 2007;97(10):1762–1774. doi: 10.2105/AJPH.2006.096263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabo Donald F, Miller Kathleen E, Farrell Michael P, Melnick Merrill J, Barnes Grace M. High School Athletic Participation, Sexual Behavior And Adolescent Pregnancy: A Regional Study. Journal of Adolescent Health. 1999;25(3):207–216. doi: 10.1016/s1054-139x(99)00070-1. [DOI] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, Labadarios D, Onoya D, et al. South African National HIV Prevalence, Incidence and Behaviour Survey, 2012. Cape Town: HSRC Press; 2014. [DOI] [PubMed] [Google Scholar]
- Taliaferro Lindsay A, Rienzo Barbara A, Donovan Kristine A. Relationships Between Youth Sport Participation and Selected Health Risk Behaviors From 1999 to 2007. Journal of School Health. 80(8):399–410. doi: 10.1111/j.1746-1561.2010.00520.x. [DOI] [PubMed] [Google Scholar]
- Ramjee Gita, Daniels Brodie. Women and HIV in Sub-Saharan Africa. AIDS Research and Therapy. 10:30. doi: 10.1186/1742-6405-10-30. http://www.aidsrestherapy.com/content/10/1/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. The United Nations (UN) General Assembly; 2011. Political Declaration on HIV and AIDS: Intensifying Our Efforts to Eliminate HIV and AIDS. http://www.unaids.org/en/media/unaids/contentassets/documents/document/2011/06/20110610_un_a-res-65-277_en.pdf. [Google Scholar]
- Rosenberg N, Westreich D, Barnighausen T, Miller WC, Behets F, Maman S, Newell ML, Pettifor A. The effect of HIV counselling and testing on HIV acquisition among South African youth. AIDS. 2013;27(17):2765–2773. doi: 10.1097/01.aids.0000432454.68357.6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Peer Education and HIV/AIDS: Concepts, uses, and challenges. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS); 1999. http://data.unaids.org/publications/IRC-pub01/jc291-peereduc_en.pdf. [Google Scholar]
- UNAIDS. Report on the Global AIDS Epidemic. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2013. [Google Scholar]
- UNFPA. State of world population 2003: Making 1 billion count: investing in adolescents’ health and rights. United Nations Population Fund (UNFPA); 2003. [Google Scholar]
- Vogel Isabel. Review of the use of ‘Theory of Change’ in international development. UK Department for International Development (DFID); 2012. [Google Scholar]
- WHO. Integrating Gender into HIV/AIDS Programmes. Geneva, Switzerland: World Health Organization (WHO); 2003. [Google Scholar]
- WHO. HIV and Adolescents: Guidance for HIV Testing and Counselling and Care for Adolescents Living with HIV. Geneva, Switzerland: World Health Organization (WHO); 2013. [PubMed] [Google Scholar]


