Abstract
The objective of the present research was to test the hypotheses that: (1) Iraq/Afghanistan war veterans experience a wide range of psychiatric symptomatology (e.g., obsessive-compulsive symptoms, hypochondriasis, somatization); and (2) General psychiatric symptomatology among Iraq/Afghanistan war veterans is associated with their warzone experiences. To achieve this objective, Iraq/Afghanistan war veterans (N = 155) completed a screening questionnaire that assessed a wide range of psychiatric symptoms along with a measure of warzone experiences. As expected, returning veterans reported significant elevations across a wide range of clinical scales. Approximately three-fourths screened positive on at least one clinical subscale, and a third screened positive on five or more. In addition, nearly all of these conditions were associated with veterans’ warzone experiences (average r = 0.36); however, this association was much stronger among veterans with PTSD (average r = 0.33) than among veterans without PTSD (average r = 0.15). We also observed that approximately 18% of the variance in total psychiatric symptomatology was attributable to warzone experiences above and beyond the effects of childhood trauma and demographic factors. Taken together, these findings suggest that returning veterans experience a broad array of psychiatric symptoms that are strongly associated with their warzone experiences.
Keywords: Veterans, trauma, combat, PTSD, anxiety, depression, psychopathology
1. Introduction
Over 2.5 million soldiers have deployed to the conflicts in Iraq and Afghanistan since September 11th 2001 (Department of Defense, 2014). While many veterans are resilient, a sizable minority experience significant mental health problems (Hoge et al., 2004; Seal, Bertenthal et al., 2007). The most well-studied mental health conditions among returning veterans include posttraumatic stress disorder (PTSD), depression, and substance-use disorders, all of which commonly co-occur among Iraq/Afghanistan veterans (Seal et al., 2007; Boulos and Zamorski, 2013). While these are the most commonly studied conditions, veterans returning from these wars also frequently experience other anxiety disorders, including social phobia and panic attacks and adjustment disorder (Sareen et al., 2007; Seal et al., 2007; Boulos and Zamorski, 2013). Less common are bipolar disorder, agoraphobia, and somatoform disorder (Sareen et al., 2007; Boulos and Zamorski, 2013).
One of the most robust predictors of PTSD following warzone deployment is combat exposure (Hoge et al., 2004; Rachmand et al., 2010; Castro and McGurk, 2013). Moderate levels of combat exposure predict the presence of a mental health diagnosis (Booth-Kewley et al., 2013), and the occurrence of new onset mental health diagnoses increases among soldiers upon return from a warzone deployment (Hoge et al., 2004; Booth-Kewley et al., 2013). Beyond warzone exposures, civilian trauma history, particularly childhood trauma, can also increase risk for PTSD and other mental health conditions in veterans (Bremner et al., 1993; Clancy et al., 2006; Cabrera et al., 2007). Thus, while the majority of research on veterans’ psychiatric health has focused on PTSD, depression, and AUDs, it is likely that the combination of elevated rates of childhood trauma along with increased trauma exposure from warzone deployments places returning veterans at risk for a much wider range of psychiatric conditions.
Within the civilian literature, childhood trauma exposure has been related to the development of obsessive compulsive disorder (OCD; Lochner et al., 2002; Matthews et al., 2008; Grisham et al., 2011), social anxiety disorder (Cougle et al., 2009; Simon et al., 2009), panic disorder (Friedman et al., 2001; Cougle et al., 2009), generalized anxiety disorder (Cougle et al., 2009), specific phobia (Cougle et al., 2009), eating disorders (Wonderlich et al., 1997; Rayworth et al., 2004; Jonas et al., 2011) drug-use disorders (Wilsnack et al., 1997), psychosis (Read et al., 2005; Fisher et al., 2010; Alvarez et al., 2011), hypochondriasis (Barsky et al., 1994), and somatization (Sanson et al., 2001; Paras et al., 2009). To date, however, far less research has examined whether critical warzone experiences might also be broadly associated with psychiatric symptomatology.
1.1 Objectives and Hypotheses
The objective of the present study was to address this gap in the literature regarding whether warzone experiences are broadly associated with mental health problems among returning Iraq/Afghanistan veterans. We hypothesized that Iraq/Afghanistan war veterans would report significant elevations on a wide range of psychiatric conditions, such as OCD, social anxiety disorder, generalized anxiety disorder, panic disorder, specific phobia, somatization, hypochondriasis, psychosis, and bulimia, in addition to the more well-studied conditions of PTSD, depression, and AUD.
Second, we hypothesized that elevations in mental health symptoms would be significantly associated with veterans’ level of exposure to critical warzone experiences during their deployments (e.g., being wounded during combat, being responsible for the death of an enemy combatant, seeing injured civilians and being unable to help). Because childhood experiences and demographic variables, such as gender, are also associated with a wide range of psychiatric outcomes, we also examined the association between critical warzone experiences and total mental health symptoms after accounting for demographic variables and childhood trauma. We hypothesized that critical warzone experiences would be associated with total psychiatric symptoms above and beyond demographic variables and childhood trauma.
Finally, since combat-related PTSD is common among veterans and known to be comorbid with a variety of other psychiatric conditions (Seal et al., 2007; Boulos and Zamorski, 2013), we examined the relationship between PTSD and the other clinical conditions assessed by the Psychiatric Diagnostic Screening Questionnaire (PDSQ; Zimmerman, 2002). We hypothesized that all of the clinical conditions assessed by the PDSQ would be more prevalent among veterans that met current criteria for a diagnosis of PTSD based on a clinical interview. We also conducted an exploratory analysis to determine if the association between critical warzone experiences and non-PTSD clinical outcomes might vary as a function of PTSD status. We hypothesized that the association between critical warzone experiences and non-PTSD clinical outcomes would be strongest among individuals with PTSD due to the high rates of comorbidity we expected to observe.
2. Method
2.1 Participants & Procedures
Participants included 155 Iraq/Afghanistan veterans enrolled in one of two larger studies on the etiology of PTSD (total N = 197). Participants with PTSD were oversampled through targeted mailings, flyers, and hospital staff recruitment. The primary eligibility criteria for the two larger studies were that participants were (1) Iraq/Afghanistan veterans and (2) did not meet criteria for schizophrenia or bipolar disorder. An additional eligibility criterion was that participants had to have completed the PDSQ (Zimmerman, 2002) to be eligible for the current analyses, which resulted in a final sample of 155 participants. Approximately 34% (53/155) of the sample met full criteria for a diagnosis of PTSD at the time of the assessment. PTSD diagnostic status was assessed with one of two structured clinical interviews (Blake et al., 1995; Sheehan et al., 1998) depending on the study in which participants originally participated in. The final sample of 155 veterans was predominantly male (93%) and Caucasian (66%; African American, 28%). The average age of participants was 40 years (SD = 10). Approximately 90% had been deployed to Iraq, whereas 17% had been deployed to Afghanistan (numbers are not mutually exclusive). The majority of participants were Army veterans (84%).
2.2 Measures
The PDSQ (Zimmerman, 2002) is a 125-item self-report measure designed to screen for a broad range of Axis I mental health disorders, including PTSD, depression, AUD, drug use disorder, bulimia/binge-eating disorder, OCD, panic disorder, agoraphobia, social anxiety disorder, generalized anxiety disorder, psychosis, somatization disorder, and hypochondriasis. In addition, the PDSQ total score provides a global measure of psychopathology. The PDSQ has good psychometric properties, including good internal consistency (avg = 0.85), test-retest reliability (avg. = 0.81), and validity (average validity coefficient = 0.64; Zimmerman, 2002). The PDSQ is also an effective screening device with an average area under the curve (AUC) value of 0.85. Recommended cut-off scores for use in clinical practice have been developed for each subscale based on setting sensitivity to approximately 90%. Using these clinical cut-offs, the PDSQ subscales’ average negative predictive value is around 97%. In the current study, the PDSQ PTSD subscale had an AUC value of 0.88 in relation to clinician-based PTSD diagnosis. In addition, the recommended cut-off score of 5 resulted in 88% sensitivity, 74% specificity, a positive predictive value of 63%, and a negative predictive value of 93%.
The Critical Warzone Experiences scale (Kimbrel et al., 2014) is a 7-item version of the widely-used U.S. Army and Marine Corps Mental Health Advisory Team's Combat Experiences Scale (MHAT-CES), which has been used in numerous studies of Iraq/Afghanistan veterans (e.g., Hoge et al., 2004; Morissette et al., 2011; Guyker et al., 2013). Kimbrel and colleagues (2014) found that the Critical Warzone Experiences scale demonstrated good internal consistency (average α = 0.83), good test-retest reliability (r = 0.73), and good concurrent validity with longer measures of combat and warzone experiences (average r = 0.74). The Critical Warzone Experiences scale also demonstrated a unidimensional factor structure (average factor loading = 0.69) and was associated with a number of key clinical outcomes, including clinician-rated PTSD symptom severity and global functional impairment.
The Childhood Trauma Questionnaire (Bernstein and Fink, 1998) is a self-report measure of childhood maltreatment. The Childhood Trauma Questionnaire includes 28 items to which participants respond on a 5-point Likert scale. Five different types of childhood maltreatment are assessed, including sexual abuse, emotional abuse, physical abuse, emotional neglect, and physical neglect. For the purposes of the current study, we used the more parsimonious total score, comprised of a sum of all five subscales. The Childhood Trauma Questionnaire has demonstrated good psychometric properties in previous research, including good test-retest reliability (r = 0.86) and good correspondence with therapists’ best-estimate maltreatment ratings (Bernstein and Fink, 1998).
3. Results
3.1 Descriptive Statistics
Descriptive statistics for the PDSQ are provided in Table 1. Consistent with our recruitment methods of oversampling for participants that were experiencing symptoms of PTSD, high levels of PTSD (45.8%) were endorsed on the PDSQ PTSD subscale. Elevations on a number of other PDSQ subscales were also observed: OCD (40.6%), somatization (38.7%), agoraphobia (34.8%), depression (32.9%), social anxiety disorder (29.7%), generalized anxiety disorder (28.4%), hypochondriasis (26.5%), AUD (25.8%), panic disorder (21.3%), and psychosis (20.0%). These findings are consistent with our first hypothesis that returning Iraq/Afghanistan veterans experience a much wider range of mental health conditions than those conditions that typically receive the most attention (e.g., PTSD). The least common clinical elevations were for drug-use (10.3%) and bulimia/binge-eating (7.7%).
Table 1.
Descriptive Statistics for the PDSQ among Iraq/Afghanistan Veterans (N = 155)
| Scale Name | Mean | SD | Min | Max | Cut Score | n ≥ Cut Score | % ≥ Cut Score |
|---|---|---|---|---|---|---|---|
| PDSQ-PTSD | 5.4 | 2.3 | 0 | 24 | 5 | 71 | 45.8% |
| PD SQ-Obsessive-Compulsive | 1.2 | 1.8 | 0 | 7 | 1 | 63 | 40.6% |
| PDSQ-Somatization | 1.3 | 1.1 | 0 | 5 | 2 | 60 | 38.7% |
| PD SQ-Agoraphobia | 2.7 | 3.2 | 0 | 11 | 4 | 54 | 34.8% |
| PDSQ-Depression | 6.0 | 5.1 | 0 | 21 | 9 | 51 | 32.9% |
| PDSQ-Social Phobia | 3.1 | 4.5 | 0 | 15 | 4 | 46 | 29.7% |
| PDSQ-Generalized Anxiety | 3.8 | 3.7 | 0 | 10 | 7 | 44 | 28.4% |
| PDSQ-Hypochondriasis | 0.6 | 1.3 | 0 | 5 | 1 | 41 | 26.5% |
| PDSQ-Alcohol Use Disorder | 0.6 | 1.3 | 0 | 6 | 1 | 40 | 25.8% |
| PDSQ-Panic | 1.6 | 2.5 | 0 | 8 | 4 | 33 | 21.3% |
| PDSQ-Psychosis | 0.4 | 0.9 | 0 | 6 | 1 | 31 | 20.0% |
| PDSQ Total Scorea | 28.9 | 26.8 | 0 | 125 | 58 | 21 | 13.5% |
| PDSQ-Substance Use Disorder | 0.3 | 1.1 | 0 | 6 | 1 | 16 | 10.3% |
| PDSQ-Bulimia | 1.5 | 2.5 | 0 | 10 | 7 | 12 | 7.7% |
Note: Measures are arranged in descending order of prevalence based on scoring above a pre-determined cut score. PDSQ = Psychiatric Diagnostic Screening Questionnaire.
The cut-off score for the PDSQ Total Score corresponds to a T-score of 60 within an outpatient clinical population.
Overall, 129 participants completed each of the 125 items from the PDSQ. Among this subset of participants with complete data available for all 125 PDSQ items, we calculated the percentage that met one or more of the clinical cut-offs for the thirteen PDSQ subscales to assess the level of comorbidity present in the sample. Nearly three-fourths of Iraq/Afghanistan veterans (73.6% or 95/129) exceeded the established clinical cut-off score for at least one PDSQ subscale. Approximately half (51.2% or 66/129) exceeded the established clinical cut-off score for at least three PDSQ scales. More than one of every three veterans (34.9% or 45/129) exceeded the established clinical cut-off score for five or more PDSQ scales.
Next, we examined the relationship between clinician-based PTSD diagnoses and screening positive on non-PTSD PDSQ subscales. As expected, veterans that met criteria for PTSD were significantly more likely to screen positive for depression, χ2 = 28.010(1), p < 0.001, bulimia/binge-eating, χ2 = 9.625(1), p = 0.002, OCD, χ2 = 17.486(1), p < 0.001, panic disorder, χ2 = 38.065(1), p < 0.001, agoraphobia, χ2 = 62.169(1), p < 0.001, psychosis, χ2 = 9.813(1), p = 0.002, social phobia, χ2 = 19.636(1), p < 0.001, generalized anxiety disorder, χ2 = 23.303(1), p < 0.001, somatization, χ2 = 30.248(1), p < 0.001, and hypochondriasis, χ2 = 17.463(1), p < 0.001, compared with veterans that did not meet current criteria for PTSD. However, contrary to hypotheses, PTSD diagnosis was not associated with either AUD, χ2 = 2.808(1), p = 0.094, or drug-use, χ2 = .180(1), p = 0.672, in the present study.
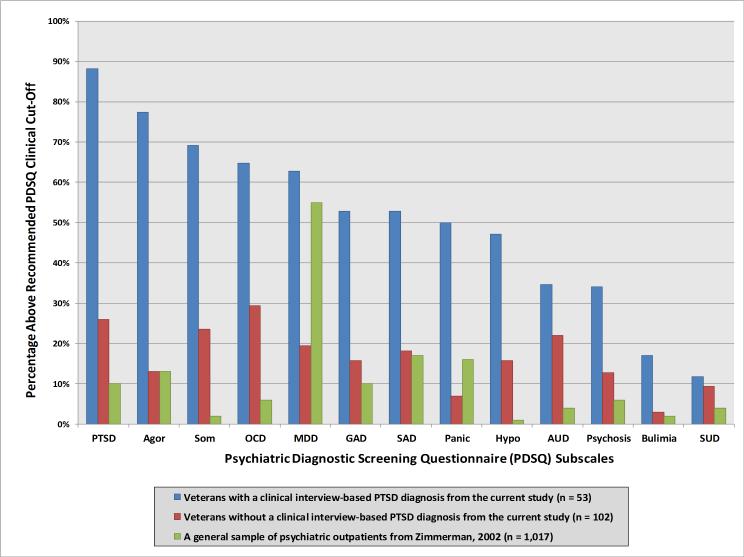
As can be seen in Figure 1, the percentage of veterans with PTSD that screened positive for other clinical conditions on the PDSQ was quite high. For comparative purposes, we also provide the prevalence rates of these clinical conditions taken from a large sample of general psychiatric outpatients (n= 1,017) reported by Zimmerman (2002) in the PDSQ manual. The magnitude of the differences between veterans diagnosed with PTSD and civilians seeking general psychiatric outpatient care was striking. For example, veterans with PTSD were approximately 47.2 times more likely to screen positive for hypochondriasis (47% vs 1%), 34.6 times more likely to screen positive for somatization (69% vs 2%), 10.8 times more likely to screen positive for OCD (65% vs. 6%), and 8.7 times more likely to screen positive for AUD (35% vs. 4%) than general psychiatric outpatients. Notably, these same conditions were also markedly elevated among veterans without PTSD relative to the general psychiatric outpatient sample from Zimmerman et al. (2000). Specifically, veterans without PTSD were approximately 15.8 times more likely to screen positive for hypochondriasis (16% vs 1%), 11.8 times more likely to screen positive for somatization (24% vs 2%), 4.9 times more likely to screen positive for OCD (29% vs. 6%), and 5.5 times more likely to screen positive for AUD (22% vs. 4%) compared with the general psychiatric outpatient sample reported by Zimmerman (2002).
Figure 1.
Percentage of veterans with and without PTSD who screened positive on one or more of the Psychiatric Diagnostic Screening Questionnaire subscales.
3.2 Correlations
A correlation matrix was generated to test our second hypothesis. As can be seen in Table 2, critical warzone experiences were significantly correlated with 12 of the 14 PDSQ subscales (avg. r = 0.36). Critical warzone experiences were most strongly associated with total psychiatric symptoms, PTSD, panic disorder, OCD, agoraphobia, depression, and generalized anxiety disorder. Childhood trauma was significantly associated with 10 of the 14 PDSQ scales (avg. r = 0.20) and was most strongly associated with depression, somatization, total symptoms, and PTSD. Contrary to hypotheses, neither critical warzone experiences nor childhood trauma was associated with symptoms of AUD or drug use. We also explored whether the association between critical warzone experiences and the PDSQ subscales might vary as a function of PTSD diagnosis. As can be seen in Table 2, critical warzone experiences were more strongly associated with psychopathology among veterans diagnosed with PTSD (avg. r = 0.33) than among veterans without PTSD (avg. r = 0.15). Interestingly, the opposite pattern was observed for childhood traumatic experiences, such that the association between childhood trauma and psychopathology was stronger among veterans without PTSD (avg. r = 0.20) compared to veterans with PTSD (avg. r = 0.07).
Table 2.
Correlations between Warzone Trauma, Childhood Trauma, and Psychopathology among Veterans with and without PTSD
| Total Sample (N = 155) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | ||
| Total | PTSD | Panic | OCD | Agor | MDD | GAD | SAD | Hypo | Som | Psych | Bulim | SUD | AUD | Avg | |
| CWE | 0.58*** | 0.55*** | 0.47*** | 0.44*** | 0.43*** | 0.42*** | 0.39*** | 0.36*** | 0.33*** | 0.32*** | 0.29** | 0.28** | 0.07 | 0.06 | 0.36 |
| CTQ | 0.28** | 0.27** | 0.16 | 0.20* | 0.21** | 0.33*** | 0.21** | 0.20* | 0.13 | 0.29*** | 0.25** | 0.07 | 0.12 | 0.02 | 0.20 |
| PTSD (n = 53) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | ||
| Total | PTSD | Panic | OCD | Agor | MDD | GAD | Social | Hypo | Som | Psych | Bulim | SUD | AUD | Avg | |
| CWE | 0.55** | 0.52** | 0.45** | 0.40** | 0.27 | 0.46** | 0.30* | 0.28* | 0.36* | 0.26 | 0.35* | 0.35* | 0.15 | −0.12 | 0.33 |
| CTQ | 0.06 | 0.02 | 0.10 | 0.21 | 0.1 | 0.09 | −0.03 | 0.16 | 0.08 | 0.16 | 0.17 | −0.10 | 0.13 | −0.13 | 0.07 |
| No PTSD (n = 102) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | PDSQ | ||
| Total | PTSD | Panic | OCD | Agor | MDD | GAD | Social | Hypo | Som | Psych | Bulim | SUD | AUD | Avg | |
| CWE | 0.34** | 0.36** | 0.22* | 0.25* | 0.27** | 0.16 | 0.22* | 0.23* | −0.08 | 0.07 | −0.06 | −0.01 | −0.03 | 0.12 | 0.15 |
| CTQ | 0.37** | 0.29** | 0.08 | 0.12 | 0.17 | 0.38** | 0.26** | 0.14 | 0.05 | 0.29** | 0.32** | 0.12 | 0.12 | 0.09 | 0.20 |
Note:
p < 0.05
p <0 .01
p < 0.001
PDSQ = Psychiatric Diagnostic Screening Questionnaire; CWE = Critical Warzone Experiences scale; CTQ = Childhood Trauma Questionnaire; PTSD = Posttraumatic stress disorder; OCD = Obsessive-compulsive disorder; Agor = Agoraphobia; MDD = major depressive disorder; GAD = Generalized anxiety disorder; SAD = Social anxiety disorder; Hypo = Hypochondriasis; Som = Somatization; Psych = Psychotic; Bulim = Bulimia/Binge Eating; Drug = Drug use disorder; AUD = Alcohol use disorder; Avg.= Average correlation for the trauma measure across all of the PDSQ scales.
3.3 Regressions
Hierarchical linear regression models were used to determine if critical warzone experiences were associated with total psychiatric symptoms above and beyond the effects of demographic variables and childhood trauma. Demographic variables (age, gender, race, ethnicity) were entered in the first step, the Childhood Trauma Questionnaire total score in the second, and Critical Warzone Experiences total score in the third. In addition, in order to assess whether the influence of critical warzone experiences on overall psychiatric symptoms varied by PTSD status, we ran the model in the total sample (N = 155) as well as among veterans with and without PTSD. As can be seen in Table 3, critical warzone exposure was the only variable that was significantly associated with total psychiatric symptoms in all three models (avg. β = 0.35); however, its effect was much stronger among veterans with PTSD, β = 0.416, p < 0.01, than among veterans without PTSD, β = 0.201, p < 0.05. In addition, consistent with the findings from the correlation analyses, we observed the opposite pattern for childhood trauma, such that it had no effect on total psychiatric symptoms among veterans with PTSD, β = 0.059, ns, but was a strong predictor of total psychiatric symptoms among veterans without PTSD, β = 0.346, p < 0.01.
Table 3.
Summary of the Hierarchical Linear Regressions Predicting Total Psychiatric Symptoms among Veterans with and Without PTSD
| Total Sample (N = 155) | PTSD (n = 53) | No PTSD (n = 102) | |||||
|---|---|---|---|---|---|---|---|
| Step | Variables | β | ΔR2 | β | ΔR2 | β | ΔR2 |
| 1 | 0.05 | 0.11 | 0.07 | ||||
| Gender | 0.004 | 0.055 | 0.013 | ||||
| Age | −0.198* | −0.332* | −0.076 | ||||
| Ethnicity | 0.063 | −0.055 | 0.154 | ||||
| Race | −0.123 | −0.208 | −0.195 | ||||
| 2 | 0.07** | 0.01 | 0.12*** | ||||
| Gender | 0.078 | 0.074 | 0.130 | ||||
| Age | −0.163* | −0.314 | −0.060 | ||||
| Ethnicity | 0.074 | −0.054 | 0.183a | ||||
| Race | −0.138 | −0.212 | −0.201* | ||||
| Childhood Trauma | 0.277** | 0.071 | 0.372*** | ||||
| 3 | 0.18*** | 0.17** | 0.04* | ||||
| Gender | 0.021 | 0.010 | 0.095 | ||||
| Age | −0.124 | −0.291a | −0.043 | ||||
| Ethnicity | 0.073 | −0.087 | 0.199* | ||||
| Race | −0.141 | −0.168 | −0.210* | ||||
| Childhood Trauma | 0.220** | 0.059 | 0.346** | ||||
| Critical Warzone Experiences | 0.437*** | 0.416** | 0.201* | ||||
| Total R2 | 0.30 | 0.29 | 0.23 | ||||
Note:
p < 0.05
p < 0.01
p < 0.001.
4. Discussion
Within this sample that was recruited to oversample for veterans diagnosed with PTSD, we observed that nearly three-fourths of Iraq/Afghanistan veterans (73.6% or 95/129) exceeded one or more of the PDSQ manual's clinical cut-off scores, which were established through research with a large sample of general psychiatric outpatients. In addition, more than one-third exceeded the established clinical cut-off score for at least five PDSQ scales. As expected, veterans that met current diagnostic criteria for PTSD were significantly more likely to screen positive for a wide range of other psychiatric conditions, such as somatization (69%), OCD (65%) hypochondriasis (47%), and AUD (35%). Notably, these same four conditions were also markedly elevated among veterans without PTSD, which suggests that the high rate of these conditions is not simply due to comorbidity with PTSD. Thus, additional research into the prevalence and functional correlates of these conditions among veterans is warranted.
Supporting our second hypothesis, we observed that critical warzone experiences were positively associated with a broad array of psychiatric symptoms, although a notable exception to this pattern was the absence of a relationship between substance use and either form of trauma. This finding was particularly unexpected given the association between trauma and substance use disorders that has been observed in previous studies (Wilsnack et al., 1997; Min et al., 2007; Wu et al., 2010). These findings are, however, consistent with recent research demonstrating that combat exposure is much more strongly associated with internalizing disorders, such as anxiety and depression, than externalizing disorders, such as AUD (e.g., Guyker et al., 2013).
Another notable finding was that the impact of critical warzone experiences on psychiatric symptoms was greatest among veterans with PTSD, whereas the impact of childhood trauma on psychiatric symptoms was greatest among veterans without PTSD. One possible explanation for this interesting pattern of results is that the strong association between critical warzone experiences and general psychiatric symptomatology may be mediated by PTSD symptoms, whereas the strong association between childhood trauma and general psychiatric symptomatology may be mediated by MDD symptoms. While such an analysis was beyond the scope of the current study, it would be interesting to test this hypothesis in larger samples of veterans that would be better powered to test this intriguing hypothesis.
4.1 Limitations and Future Directions for Research
Several limitations should be noted. First, the cross-sectional design of the current study limits our ability to draw temporal inferences about the association between critical warzone experiences and psychiatric symptomatology, broadly defined. A similar limitation concerns the fact that critical warzone experiences were assessed retrospectively. While retrospective measures of combat experiences are common in this type of research, future research is needed to prospectively evaluate the broad effects of combat exposure on mental health. Third, the findings presented here are based on a convenience sample of predominantly White Iraq/Afghanistan veterans enrolled in the VA system. Notably, the sample used in the present research was older and had a higher proportion of males relative to other recent nationally-representative studies of Iraq/Afghanistan veterans (e.g., Elbogen et al., 2013). Thus, the degree to which the findings from the present research might generalize to more diverse groups of veterans is unclear.
Finally, to our knowledge, the present study is the first to use the PDSQ with a sample of Iraq/Afghanistan veterans. In general, the PDSQ performed well, demonstrating a good AUC for PTSD; however, it must be noted that there was still considerable disagreement between the clinician-based PTSD diagnoses and the PDSQ screening scores for PTSD in a number of cases, primarily in the direction of false positives. Of course, screening measures like the PDSQ are designed to have high levels of sensitivity to ensure that individuals who might be at risk for a particular disorder receive additional evaluation; however, such sensitivity always comes at the expense of specificity. Thus, the high rates of positive screens observed in the present research should be considered exactly that: positive screens—not clinical diagnoses. While there is often good convergent validity between self-report measures and clinician assessments (e.g., Adkins et al., 2008), the overlap is far from perfect. Moreover, in the case of the PDSQ, additional research on the psychometrics and utility of this measure with returning veterans is needed. Thus, the findings from the present study should be interpreted cautiously in light of the limited research on the psychometric properties of the PDSQ among Iraq/Afghanistan veterans.
In sum, we observed significant clinical elevations across a broad array of mental health symptoms among returning Iraq/Afghanistan veterans. Nearly all of these conditions were strongly associated with veterans’ warzone experiences; however, this association was strongest among veterans diagnosed with PTSD.
Acknowledgements
This project was supported by a Career Development Award (IK2 CX000525) to Dr. Kimbrel from the Clinical Science Research and Development Service of the VA Office of Research and Development, a VA VISN 17 New Investigator Award to Dr. Kimbrel entitled “Genetic and Environmental Effects on PTSD, Depression, and Alcohol Misuse,” a Merit Award (I01 RX000304) to Dr. Morissette from the Rehabilitation Research and Development Service of VA Office of Research and Development, a Research Career Scientist Award to Dr. Beckham from the Clinical Science Research and Development Service of the VA Office of Research and Development, the VA VISN 17 Center of Excellence for Research on Returning War Veterans, the Central Texas Veterans Health Care System, the Research & Development and Mental Health Services of the Durham Veterans Affairs Medical Center, and the VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
References
- Adkins JW, Weathers FW, McDevitt-Murphy M, Daniels B. Psychometric properties of seven self-report measures of posttraumatic stress disorder in college students with mixed civilian trauma exposure. Journal of Anxiety Disorders. 2008;22:1393–1402. doi: 10.1016/j.janxdis.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Alvarez M, Roura P, Oses A, Foguet Q, Sola J, Arrufat F. Prevalence and clinical impact of childhood trauma in patients with severe mental disorders. Journal of Nervous and Mental Disease. 2011;199(3):156–161. doi: 10.1097/NMD.0b013e31820c751c. [DOI] [PubMed] [Google Scholar]
- Barsky AJ, Wool C, Barnett MC, Cleary PD. Histories of childhood trauma in adult hypochondriacal patients. American Journal of Psychiatry. 1994;151(3):391–401. doi: 10.1176/ajp.151.3.397. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-Report Manual. Psychological Corporation; San Antonio, TX: 1998. [Google Scholar]
- Blake D, Weathers FW, Nagy LM, Kaloupek DG. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Booth-Kewley S, Schmied EA, Highfill-McRoy RM, Larson GE, Garland CF, Zaijko LA. Predictors of psychiatric disorders in combat veterans. BMC Psychiatry. 2013;13(1):130. doi: 10.1186/1471-244X-13-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulos D, Zamorski MA. Deployment-related mental disorders among Canadian Forces personnel deployed in support of the mission in Afghanistan, 2001-2008. Canadian Medical Association Journal. 2013;185:E545–E552. doi: 10.1503/cmaj.122120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner JD, Southwick SM, Johnson DR, Yehuda R, Charney DS. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. American Journal of Psychiatry. 1993;150(2):235–239. doi: 10.1176/ajp.150.2.235. [DOI] [PubMed] [Google Scholar]
- Cabrera OA, Hoge CW, Bliese PD, Castro CA, Messer SC. Childhood adversity and combat as predictors of depression and post-traumatic stress in deployed troops. American Journal of Preventive Medicine. 2007;33(2):77–82. doi: 10.1016/j.amepre.2007.03.019. [DOI] [PubMed] [Google Scholar]
- Castro CA, McGurk D. The intensity of combat and behavioral health status. Traumatology. 2007;13:6–23. [Google Scholar]
- Clancy CP, Graybeal A, Tompson WP, Badgett KS, Feldman ME, Calhoun PS, Erkanli A, Hertzberg MA, Beckham JC. Lifetime trauma exposure in veterans with military-related posttraumatic stress disorder: Association with current symptomatology. Journal of Clinical Psychiatry. 2006;67(9):1346–1353. doi: 10.4088/jcp.v67n0904. [DOI] [PubMed] [Google Scholar]
- Cougle JR, Timpano KR, Sachs-Ericsson N, Keough ME, Ricardi CJ. Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbity Survey-Replication. Psychiatry Research. 2010;177:150–155. doi: 10.1016/j.psychres.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Cromer KR, Schmidt NB, Murphy DL. An investigation of traumatic life events and obsessive-compulsive disorder. Behavior Research and Therapy. 2007;45:1683–1691. doi: 10.1016/j.brat.2006.08.018. [DOI] [PubMed] [Google Scholar]
- Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, Timko C, Beckham JC. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatric Services. 2013;64(2):134–141. doi: 10.1176/appi.ps.004792011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher HL, Jones PB, Fearon P, Craig TK, Dazzan P, Morgan K, Hutchinson G, Doody GA, Morgan C. The varying impact of type, timing, and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychological Medicine. 2010;40(12):1967–1978. doi: 10.1017/S0033291710000231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman S, Smith L, Fogel D, Paradis C, Viswanathan R, Ackerman R, Trappler B. The incidence and influence of early traumatic life events in patients with panic disorder: A comparison with other psychiatric outpatients. Journal of Anxiety Disorders. 2002;16:259–272. doi: 10.1016/s0887-6185(02)00097-x. [DOI] [PubMed] [Google Scholar]
- Grisham JR, Fullana MA, Mataix-Cols D, Moffitt TE, Caspi A, Poulton R. Risk factors prospectively associated with adult obsessive-compulsive symptom dimensions and obsessive-compulsive disorder. Psychological Medicine. 2011;41:2495–2506. doi: 10.1017/S0033291711000894. [DOI] [PubMed] [Google Scholar]
- Guyker WM, Donnelly K, Donnelly JP, Dunnam M, Warner GC, Kittleson J, Bradshaw CB, Alt M, Meier ST. Dimensionality, reliability, and validity of the Combat Experiences Scale. Military Medicine. 2013;178:377–384. doi: 10.7205/MILMED-D-12-00223. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Jonas S, Bebbington P, McManus S, Meltzer H, Jenkins R, Kuipers E, Cooper C, King M, Brugha T. Sexual abuse and psychiatric disorder in England: Results from the 2007 Adult Psychiatric Morbidity Survey. Psychological Medicine. 2011;41:709–719. doi: 10.1017/S003329171000111X. [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, Evans LD, Patel AB, Wilson LC, Meyer EC, Gulliver SB, Morissette SB. The Critical Warzone Experiences (CWE) scale: Initial psychometric properties and association with PTSD, anxiety, and depression. Psychiatry Research. 2014;220:1118–1124. doi: 10.1016/j.psychres.2014.08.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lochner C, du Toit PL, Zungu-Dirwayi N, Marais A, van Kradenburg J, Seedat S, Niehaus DJH, Stein DJ. Childhood trauma in obsessive-compulsive disorder, trichotillomania, and controls. Depression and Anxiety. 2002;15:66–68. doi: 10.1002/da.10028. [DOI] [PubMed] [Google Scholar]
- Morissette SB, Woodward M, Kimbrel NA, Meyer EC, Kruse MI, Dolan S, Gulliver SB. Deployment-related TBI, persistent post-concussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabilitation Psychology. 2011;56:340–350. doi: 10.1037/a0025462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews CA, Kaur N, Stein MB. Childhood trauma and obsessive-compulsive symptoms. Depression and Anxiety. 2008;25:742–751. doi: 10.1002/da.20316. [DOI] [PubMed] [Google Scholar]
- Paras ML, Zirakzadeh A, Muras MH, Chen LP, Goranson EN, Sattler AL, Colbenson KM, Elamin MB, Seime R, Prokop LJ. Sexual abuse and lifetime diagnosis of somatic disorders. JAMA. 2009;302(5):550–561. doi: 10.1001/jama.2009.1091. [DOI] [PubMed] [Google Scholar]
- Rachmand R, Schell TL, Karney BR, Osilla K, Burns RM, Caladrone L. Disparate prevalence estimates of PTSD among service members who served in Iraq and Afghanistan: Possible explanations. Journal of Traumatic Stress. 2010;23:59–68. doi: 10.1002/jts.20486. [DOI] [PubMed] [Google Scholar]
- Rayworth BB, Wise LA, Harlow BL. Childhood abuse and risk of eating disorders in women. Epidemiology. 2004;15(3):271–278. doi: 10.1097/01.ede.0000120047.07140.9d. [DOI] [PubMed] [Google Scholar]
- Read J, Os JV, Morrison AP, Ross CA. Childhood trauma, psychosis, and schizophrenia: A literature review with theoretical and clinical implications. Acta Psychiatrica Scandinavica. 2005;112(5):330–350. doi: 10.1111/j.1600-0447.2005.00634.x. [DOI] [PubMed] [Google Scholar]
- Sansone RA, Wiederman MW, Sansone LA. Adult somatic preoccupation and its relationship to childhood trauma. Violence and Victims. 2001;16(1):39–47. [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Afifi TO, Stein MB, Belik S, Meadows G, Asmundson GJG. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care. JAMA Psychiatry. 2007;64:843–852. doi: 10.1001/archpsyc.64.7.843. [DOI] [PubMed] [Google Scholar]
- Seal KH, Berthenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: Mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at the Department of Veterans Affairs Facilities. Archives of Internal Medicine. 2007;167(5):476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001-2010. Drug and Alcohol Dependence. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan K, Amorim P, Janavs J, Weiller E. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Simon NM, Herlands NN, Marks EH, Mancini C, Letamendi A, Li Z, Pollack MH, Van Ameringen M, Stein MB. Childhood maltreatment linked to greater symptom severity and poorer quality of life and function in social anxiety disorder. Depression and Anxiety. 2009;26:1027–1032. doi: 10.1002/da.20604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack SC, Vogeltanz ND, Klassen AD, Harris TR. Childhood sexual abuse and women's substance abuse: national survey findings. Journal of Studies on Alcohol and Drugs. 1997;58(3):264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Brewerton TD, Jocic Z, Dansky BS, Abbott DW. Relationship of childhood sexual abuse and eating disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(8):1107–1115. doi: 10.1097/00004583-199708000-00018. [DOI] [PubMed] [Google Scholar]
- Wilsnack SC, Vogeltanz ND, Klassen AD, Harris R. Childhood sexual abuse and women's substance abuse: National survey findings. Journal of Studies on Alcohol. 1997;58:264–271. doi: 10.15288/jsa.1997.58.264. [DOI] [PubMed] [Google Scholar]
- Wu NS, Schairer LC, Dellor E, Grella C. Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders. Addictive Behavior. 2010;35:68–71. doi: 10.1016/j.addbeh.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M. The Psychiatric Diagnostic Screening Questionnaire. Western Psychological Services; Los Angeles, CA: 2002. [Google Scholar]