Abstract
Objective:
Diabetes mellitus is recognized as a risk factor for mortality and morbidity after coronary bypass grafting. We aimed to determine the association between preoperative hemoglobin HbA1c and AF after isolated off-pump coronary bypass grafting (OPCAB).
Methods:
The seventy-two diabetic patients undergoing isolated off-pump coronary bypass grafting were retrospectively analyzed for AF. They were divided into; Low (4.8–5.4%), Medium (5.5–8%) and High (8.1–11.5%) groups. The three groups were compared with respect to demographic, echocardiographic, intraoperative and postoperative clinical characteristics correlation.
Results:
Three patients died during postoperative period. AF occurred in 12 patients (16.6%) after surgery. The incidence of postoperative AF was 15.3% in the lower, 4.4% middle and 57.1% upper group. There was statistically significant correlation between preoperative HbA1C and preoperative stroke, preoperative MI history, Left atrial (LA) size, preoperative levosimendan, preoperative clopidogrel, postoperative AF, postoperative dopamine and dobutamine use, IABP, duration of extubation time, 24-hour chest tube drainage, duration of ICU and hospital mortality. Univariate logistic regression analysis showed significant correlation between postoperative AF and variables like preoperative HbA1c levels, LVEF<30%, history of preoperative MI, preoperative use of levosimendan, preoperative use of clopidogrel, postoperative dopamine, dobutamine adrenaline use, left atrium size, 24-hour chest tube drainage and length of stay in the intensive care unit.
Conclusion:
Preoperative HbA1c levels could predict the occurrence of postoperative AF in diabetic patients and may entail to administer protective strategies.
KEY WORDS: HbA1c, Off-pump coronary surgery, Atrial fibrillation
INTRODUCTION
Atrial fibrillation (AF) is the most common arrhythmic complication of coronary artery bypass grafting surgery (CABG). Depending on the type of cardiac surgery, its incidence varies between 30% and 50%.1 The exact factors affecting its incidence are largely unknown. Postoperative AF has been showed to increase both postoperative and 10-year mortality rates, with the latter being increased by 29%.2 Some studies have reported that elevated HbA1c levels preceding surgery are linked to the severity of adverse outcomes after CABG.3 An elevated HbA1c level is reportedly related to a greater incidence of cardiovascular events.4 We aimed to determine the association between preoperative hemoglobin A1c and AF after isolated off-pump coronary bypass grafting (OPCAB).
METHODS
Seventy-two diabetic patients undergoing OPCAB at our hospital from January 2012 to June 2014 were retrospectively analyzed for AF. The study was approved by the hospital ethic committee. OPCAB was performed in all patients and a shift to cardiopulmonary bypass was not necessary for any patients. Baseline demographic and clinical data were available for all patients, and medical records were accessed for the initial medical data. We divided these patients into three groups (control of diabetic regulation was very good, good and bad) according to the preoperative HbA1c levels. The cutoff points for the groups were selected as follows: Low group; 4.5–5.4% (n =13), Medium group; 5.5–8% (n = 45), and high group: 8.1–11.5% (n =14). Continuous electrocardiographic monitoring via a bedside monitor at the intensive care unit and a telemetry unit at the hospital ward were carried out in all patients after completion of the surgery.
A 12-lead electrocardiogram was taken and evaluated by an experienced physician when the automatic alarm function detected an arrhythmic episode. HbA1c levels were measured before surgery by liquid chromatography. During the bypass surgery, multiple and complete coronary revascularization were attempted at all times, using a composite or sequential grafting in all cases. Arterial grafts in general, and in situ arterial grafts in particular, were used whenever possible. Continuous infusion of diltiazem (0.5-1. 0 µg/kg) was utilized to prevent arterial spasm during and within 24 hours after the operation, followed by oral diltiazem (90 mg/day), acetylsalicylic acid(100 mgr/day) and clopidogrel (75 mg/day) commenced at the next morning.
Anesthetic & surgical technique
Intravenous fentanyl citrate, midazolam, and vecuronium bromide were employed for anesthesia induction while intravenously administered remifentanyl, vecuronium bromide and low concentrations of inhaled sevoflurane as necessary served for anesthesia maintenance. Heparin was administered to anticoagulated patients after harvesting bypass conduits. The activated clotting time was maintained at more than 250s. The off-pump technique was used for all patients. Intravenous administration of Magnesium (Mg levels were kept over 2 mgr/dl) and potassium were given (K levels were kept over 4 mgr/dl) before pericardiotomy was done for all patients.
Statistical Analysis
Statistical analysis was performed on SPSS 15.0 for Windows software package with 95% confidence. Independent Sample t-test was used for the parametric features like age, BMI and HbA1c in the men and women. Kruskal Wallis H statistical analysis was used for the comparison between the non-parametric features in continuous variables of more than two groups. Relationships between variables were assessed by Pearson and Spearman correlation analysis. The effects of variables on postoperative AF occurrence were examined using logistic regression analysis. P <0.05 was considered statistically significant.
RESULTS
Demographic findings of the patient groups can be seen in Table-I. Fig.1 shows the distribution of HbA1c and the median value of HbA1c (25th–75th percentile) was 6.0 (5–7.5). AF occurred in 12 of 72 patients (16.6%) after surgery, most often on postoperative day 2 (75%), with 24.9% of occurrences on postoperative day 3. The incidences of postoperative AF were 15.3% (2/13) in the Low group, 4.4% (2/45) in the Median group, and 57.1% (8/14) in the High group. Three patients died at postoperative period in the High group (hospital mortality, P = 0.000) (Table-I).
Table-I.
Baseline characteristics & operative variables.
| Preoperative HbA1C | P value | ||||
|---|---|---|---|---|---|
| Low (n=13) | Median (n=45) | High (n=14) | |||
| Sex | Male/Female | 7/6 | 26/19 | 7/7 | 0,831* |
| Age | 62,85±7,84 | 62,4±10,27 | 66,21±10,21 | 0,302* | |
| LVEF | (<30) | 0 (0) | 2 (4,4) | 4 (28,6) | 0,910* |
| (30-50) | 10 (76,9) | 20 (44,4) | 3 (21,4) | ||
| (>50) | 3 (23,1) | 23 (51,1) | 7 (50) | ||
| Chronic renal failure | 1 (7,7) | 5 (11,1) | 1 (7,1) | 0,950 | |
| Hypertension | 10 (76,9) | 36 (80) | 11 (78,6) | 0,922 | |
| Previous cerebrovascular disease | 3 (23,1) | 1 (2,2) | 0 (0) | 0,011 | |
| Chronic pulmonary disease | 3 (23,1) | 3 (6,7) | 2 (14,3) | 0,499 | |
| Peripheral vascular disease | 1 (7,7) | 2 (4,4) | 0 (0) | 0,319 | |
| Previous Myocardial infaction | 1 (7,7) | 12 (26,7) | 4 (28,6) | 0,213 | |
| Left atrial dimension (cm) | 3,64±0,4 | 3,82±0,41 | 3,99±0,44 | 0,144 | |
| Number of anastomoses | 2,92±1,26 | 2,62±1,3 | 3,14±1,23 | 0,245 | |
| Number of arterial anastomoses | 1,15±0,55 | 1,27±0,5 | 1,5±0,52 | 0,066 | |
| Number of vein grafts | 2±0,82 | 1,66±0,55 | 1,7±0,95 | 0,462 | |
| Preoperative used of Beta- Blockers | 1 (7,7) | 15 (33,3) | 3 (21,4) | 0,451 | |
| Use of Levosimendan | 1 (7,7) | 3 (6,7) | 5 (35,7) | 0,025 | |
| Angiotensin converting inhibitors use | 4 (30,8) | 16 (35,6) | 8 (57,1) | 0,157 | |
| Use of Angiotensin receptor blockers | 2 (15,4) | 8 (17,8) | 1 (7,1) | 0,540 | |
| Use of Statins | 3 (23,1) | 14 (31,1) | 5 (35,7) | 0,482 | |
| Use of Oral antidiabetics | 11 (84,6) | 24 (53,3) | 10 (71,4) | 0,521 | |
| Use of Insulin | 1 (7,7) | 15 (33,3) | 2 (14,3) | 0,741 | |
| Use of Clopidogrel | 2 (15,4) | 8 (17,8) | 5 (35,7) | 0,189 | |
| Endartterectomy | 2 (15,4) | 4 (8,9) | 0 (0) | 0,150 | |
| Use of Intra-aortic balloon pump | 0 (0) | 0 (0) | 4 (28,6) | 0,001 | |
| Use of insulin during intensive care | 7 (53,8) | 18 (40) | 10 (76,9) | 0,243 | |
| Postoperative use of Dopamin | 4 (30,8) | 20 (44,4) | 9 (64,3) | 0,081* | |
| Postoperative use of Dobutamin | 2 (15,4) | 2 (4,4) | 7 (50) | 0,010* | |
| Postoperative use of Adrenalin | 1 (7,7) | 0 (0) | 4 (28,6) | 0,028* | |
| Postoperative use of Diltizem | 1 (7,7) | 8 (17,8) | 5 (35,7) | 0,066* | |
| Postoperative AF occurrence | 0 (0) | 4 (8,9) | 8 (57,1) | 0,000 | |
| Post-discharge AF | 0 (0) | 1 (2,2) | 4 (28,6) | 0,003 | |
| Mortality | 0 (0) | 0 (0) | 3 (21,4) | 0,005 | |
| Intubation time(hr) | 9,08±3,73 | 7,54±2,56 | 17,68±29,8 | 0,072 | |
| Chest tube drainage (ml) | 457,69±181,25 | 432,22±183,76 | 539,29±301,39 | 0,658 | |
| Intensive care unit stay time(hr) | 46,15±23,42 | 39,33±10,97 | 63,43±31,02 | 0,006 | |
| Mean time to AF occurrence (day) | - | 1,5±1 | 1,38±0,74 | 0,911 | |
Data are number (percent), mean ± standard deviation, or median [25th–75th percentile]. Low 4.5-5.4%; Median, 5.5-8%; High, >8.%.
Fig.1.
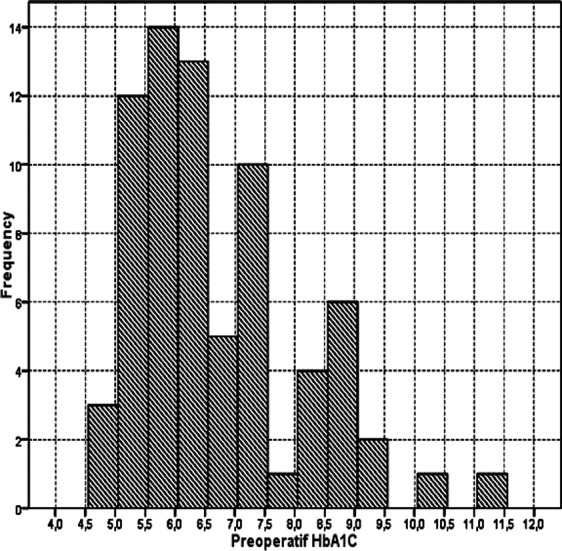
Distribution of Preoperative HbA1c.
In univariate logistic regression analysis between the presence of postoperative AF and variables like LVEF <30 (p=0.015), preoperative MI history (p = 0.004), preoperative use of levosimendan (p = 0.003) and clopidogrel (p = 0.011), postoperative dopamine (P = 0.036), dobutamine (p = 0.000) and adrenaline use (p = 0.004), LA size (P = 0.002), 24-hour chest tube drainage (p = 0.029), length of stay in the ICU (p = 0.003) and preoperative HbA1c (p = 0.000) showed values were statistically significant (p <0.05) (Table-III). Higher HbA1c levels were correlated with intraaortic balloon counter pulsation use (IABP) (p=0.01), preoperative cerebrovascular disease rate (p=0.011), use of preoperative levosimendan usage (p=0.025), use of postoperative dobutamine (p=0.01) and adrenalin (p=0.028) and longer intensive care unit stay (p=0.006). Correlation analysis showed that there is statistically significant correlation between preoperative HbA1C and occurrences of SVO (p = 0.020), postoperative AF with preoperative MI history (p = 0.002), Left atrial (LA) size (p = 0.000), preoperative use of levosimendan (p = 0.001), preoperative use of clopidogrel (p = 0.006), postoperative dopamine (p = 0.000) and dobutamine use (p = 0.000), IABP usage (p = 0.011), duration of extubation (p = 0.011), 24 hour chest tube drainage (p = 0.011), duration of ICU (p = 0.01) and hospital mortality (p = 0.000) (p <0.05) (Table-II).
Table-III.
All variables with the presence of postoperative AF in univariate logistic regression analysis.
| AF+ (n=12) | AF – (n=60) | Odds Ratio (95% C.I.) | p | ||
|---|---|---|---|---|---|
| Sex | M/F | 4/8 | 28/32 | 1,75 (0,48-6,44) | 0,400 |
| Age | 65,92±11,1 | 62,68±9,6 | 1,04 (0,97-1,11) | 0,299 | |
| LVEF | (>50) | 5 (41,7) | 28 (46,7) | Referance | 0,015 |
| (30-50) | 3 (25) | 30 (50) | 0,56 (0,12-2,56) | 0,455 | |
| (<30) | 4 (33,3) | 2 (3,3) | 11,2 (1,6-78,4) | 0,015 | |
| Chronic renal failure | 1 (8,3) | 6 (10) | 0,82 (0,09-7,49) | 0,859 | |
| Hypertension | 11 (91,7) | 46 (76,7) | 3,35 (0,4-28,25) | 0,267 | |
| Previous cerebrovascular disease | - (-) | 4 (6,7) | 0 (0-) | 0,999 | |
| Chronic pulmonary disease | 3 (25) | 5 (8,3) | 3,67 (0,74-18,08) | 0,110 | |
| Peripheral vascular disease | - (-) | 3 (5) | 0 (0-) | 0,999 | |
| Previous Myocardial infaction | 7 (58,3) | 10 (16,7) | 7 (1,84-26,56) | 0,004 | |
| Preoperative used of Beta- Blockers | 5 (41,7) | 14 (23,3) | 2,35 (0,64-8,56) | 0,196 | |
| Levosimendan | 5 (41,7) | 4 (6,7) | 10 (2,16-46,26) | 0,003 | |
| Angiotensin converting inhibitors | 6 (50) | 22 (36,7) | 1,73 (0,5-6,01) | 0,391 | |
| Angiotensin receptor blockers | 1 (8,3) | 10 (16,7) | 0,45 (0,05-3,93) | 0,474 | |
| Statins | 4 (33,3) | 18 (30) | 1,17 (0,31-4,37) | 0,819 | |
| Oral antidiabetics | 7 (58,3) | 38 (63,3) | 0,81 (0,23-2,86) | 0,744 | |
| Insulin | 3 (25) | 15 (25) | 1 (0,24-4,18) | 1,000 | |
| Clopidogrel | 6 (50) | 9 (15) | 5,67 (1,49-21,54) | 0,011 | |
| Endartterectomy | - (-) | 6 (10) | 0 (0-.) | 0,999 | |
| Postoperative use of Dopamin | 9 (75) | 24 (40) | 4,5 (1,1-18,34) | 0,036 | |
| Postoperative use of Dobutamin | 7 (58,3) | 4 (6,7) | 19,6 (4,24-90,67) | 0,000 | |
| Postoperative use of Adrenalin | 4 (33,3) | 1 (1,7) | 29,5 (2,92-297,9) | 0,004 | |
| Postoperative use of Diltizem | 1 (8,3) | 13 (21,7) | 0,33 (0,04-2,79) | 0,308 | |
| Use of Intra-aortic balloon pump | 4 (33,3) | - (-) | 0,999 | ||
| Use of insulin during intensive care | 9 (75) | 26 (44,1) | 3,81 (0,94-15,5) | 0,062 | |
| Post-discharge AF | 5 (41,7) | - (-) | 0,999 | ||
| Hospital Mortality | 3 (25) | - (-) | 0,999 | ||
| Left atrial dimension (cm) | 4,23±0,38 | 3,73±0,39 | 21,84 (3,25-146,71) | 0,002 | |
| Number of anastomoses | 2,92±1,24 | 2,75±1,3 | 1,1 (0,69-1,77) | 0,679 | |
| Number of arterial anastomoses | 1,25±0,45 | 1,3±0,53 | 0,82 (0,23-2,94) | 0,758 | |
| Number of vein grafts | 2±0,93 | 1,68±0,65 | 1,9 (0,64-5,64) | 0,245 | |
| Intubation time(hr) | 18,83±32,25 | 7,98±2,86 | 1,13 (0,96-1,34) | 0,153 | |
| Chest tube drainage (ml) | 587,5±296,28 | 431,67±182,95 | 1 (1-1,01) | 0,029 | |
| Intensive care unit stay time(hr) | 67±32,14 | 40,9±14,51 | 1,05 (1,02-1,09) | 0,003 | |
| Preoperative HbA1C | 8,58±1,38 | 6,31±1,06 | 3,92 (1,92-7,99) | 0,000 | |
Values are odds ratio (95% confidence interval), LV, left ventricle; EF, Ejection fraction.
Table-II.
Correlation analysis of preoperative & postoperative variables with HbA1c values associated with AF.
| Preoperative HbA1C | Postoperative AF | |||
|---|---|---|---|---|
| r | p | r | p | |
| Previous cerebrovascular disease | -0,273 | 0,020 | -0,108 | 0,364 |
| Previous Myocardial infaction | 0,057 | 0,632 | 0,366 | 0,002 |
| Left atrial dimension (cm) | 0,151 | 0,204 | 0,441 | 0,000 |
| Levosimendan | 0,201 | 0,090 | 0,394 | 0,001 |
| Clopidogrel | 0,089 | 0,458 | 0,321 | 0,006 |
| Postoperative used of Dopamin | 0,081 | 0,501 | 0,262 | 0,026 |
| Postoperative used of Dobutamin | 0,232 | 0,049 | 0,535 | 0,000 |
| Postoperative used of Adrenalin | 0,253 | 0,032 | 0,464 | 0,000 |
| Use of Intra-aortic balloon pump | 0,361 | 0,002 | 0,542 | 0,000 |
| Intubation time(hr) | 0,167 | 0,161 | 0,300 | 0,011 |
| Chest tube drainage (ml) | 0,113 | 0,346 | 0,276 | 0,019 |
| Intensive care unit stay time(hr) | 0,349 | 0,003 | 0,472 | 0,000 |
| Mortality | 0,303 | 0,010 | 0,466 | 0,000 |
Corrected Bonferroni Mann Whitney U test was used to find out the correlation of HbA1c level and several clinical conditions like the use of dopamine and ICU durations between medial and high groups (p = 0.008, p=0.001 p<0.016 respectively) (Table-I). The mortality was significantly higher in High group (n=3, 100%) compared to low and median groups.
When examined all variables of preoperative HbA1c groups, statistically significant differences were found between groups of postoperative AF, AF after discharge and hospital mortality (p<0, 05) (Table-I).
DISCUSSION
Association of OPCAB surgery with decreased incidence of AF was shown in a meta analysis and provided evidence that OPCAB surgery may be associated with a reduced incidence of postoperative AF than on-pump CPB techniques in a generalized population. The off-pump and on-pump groups had postoperative AF incidences of 19% (1612/8265) and 24% (1976/8240).5 Our study revealed that AF complicated 16.6% of off-pump operations. Limited number of patients in our study can be shown to be the main reason of this low rates. In a prospective cohort study of 3089 patients with and without diabetes, Halkos et al.6 showed a significant correlation between HbA1c and in-hospital mortality and postoperative morbidity. The rates of postoperative complications, e.g. renal failure and cerebrovascular accident, were higher in patients with HbA1c ≥ 8.6%. AF occurred in 20.9% of patients having an HbA1c of less than 7.0% vs. 15.1% in those with an HbA1c level equal to or greater than 7.0%. Patients with a poor glycemic control evidenced by an HbA1c ≥7% had more complications than those with an HbA1c of less than 7%. Similarly, in 101 diabetic subjects operated with off-pump CABG, Matsuura et al.7 found a postoperative AF rate of 29.7% for an HbA1c of less than 6.5% and 22.2% for an HbA1c that was greater than 6.5%. In our study 72 diabetic patients undergoing OPCAB were retrospectively analyzed. We divided these patients into three groups according to the preoperative HbA1c levels (Low group; 4.5–5.4%, Medium group; 5.5–8%, and high group: 8.1–11.5%). Corrected Bonferroni Mann Whitney U test was used to find out the correlation of HbA1c level and several clinical conditions like the use of dopamine, ICU durations and mortality rates between medial and high groups. As a reason for this result, all of the patients in a low group LVEF values greater than 30%. However, Matsuura et al the two groups did not differ significantly with regard to early and late postoperative mortality, wound dehiscence, number of anastomosis, use of bilateral internal thoracic arteries, and patency rates. On the other hand, in 805 diabetic subjects operated with OPCAB surgery, Kinoshita et al.8 reported that the lower group, the middle group, and the upper group had postoperative AF rates of 28.3%, 17.4%, and 12.5%, respectively. Postoperative AF was less likely when an elevated preoperative HbA1c was present. Our study demonstrated that the lower group, the middle group, and the upper group had postoperative AF incidences of 15.3%, 4.4%, and 57.1%, respectively. The risk of postoperative AF was greater with an elevated preoperative HbA1c. Dublin et al.9 demonstrated an elevated risk in parallel with HbA1c level in a population-based case control study conducted in 1410 patients with newly-diagnosed AF. Another population-based study in 75-year-old subjects similarly showed higher HbA1c levels in patients who developed AF.10 Diabetics with higher HbA1c levels also suffer a higher rate of perioperative myocardial infarction.6,11. Our study also showed similar results in that higher HbA1c levels significantly associated with risk of death. Faritous et al.12 demonstrated that a higher incidence of IABP, massive bleeding, and multi-organ failure result from higher HbA1c levels. Morbidity, but not mortality, is increased by elevated HbA1c levels following CABG. We showed that elevated HbA1c level increased the likelihood of IABP use (p=0.01), rate of preoperative cerebrovascular disease (P=0.011), use of preoperative levosimendan (P=0.025), use of postoperative dobutamine (p=0.01) in conjunction with adrenaline (p=0.028), longer intensive care unit stay (p=0.006), postoperative and post-discharge AF, and mortality rate (p<0, 05). Goksedef et al.13 reported that in 150 diabetic and non-diabetic patients enrolled in a prospective fashion the rates of postoperative mediastinitis and local sternal infection (P = 0.8) were not significantly altered by an HbA1c level of >7%. On the other hand, Sato et al.14 in a prospective study of 273 diabetic and non-diabetic patients, demonstrated that diabetics with a HbA1c greater than 6.5% suffered significantly more postoperative complications (minor infections and a more labor-intensive hospital stay). Alserius et al.15 Prospectively investigated the relationship between HbA1c level and infection and mortality rates in 605 subjects. HbA1c level greater than 6% was associated with significantly increased incidence of superficial sternal wound infections and mortality.
Limitations of the study
First, off-pump technique was performed at a single center. Second, it was not a randomized controlled study. Third, it solely used preoperative laboratory data including HbA1c level but not assessed postoperative HbA1c alterations.
CONCLUSION
Our study showed that preoperative HbA1c level was associated with AF in diabetic patients undergoing OPCAB. In conclusion, preoperative HbA1c could be predicts the occurrence of postoperative AF after isolated off-pump CABG.
Footnotes
Disclosure Statement: The authors declare no conflict of interest in this study.
Authors’ Contribution
Suleyman Surer, Mustafa Seren and Ali Bulut conceived, designed and did statistical analysis & editing of manuscript.
Onur Saydam did data collection and manuscripwof manuscript.
REFERENCES
- 1.Crystal E, Garfinkle MS, Connolly SS, Ginger TT, Sleik K, Yusuf SS. Interventions for preventing post-operative AF in patients undergoing heart surgery. Cochrane Database Syst Rev. 2004;18(4):CD003611. doi: 10.1002/14651858.CD003611.pub2. doi:10.1002/14651858.CD003611. [DOI] [PubMed] [Google Scholar]
- 2.Benussi S, Galanti A, Alfieri O. Restoring sinus rhythm in patients at a high risk for postoperative atrial fibrillation. Arch Med Sci. 2008;4(2):108–115. [Google Scholar]
- 3.Filardo G, Hamilton C, Hebeler RF, Hamman BL, Grayburn PA. New-onset postoperative atrial fibrillation after isolated coronary artery bypass graft surgery & long-term survival. Circ Cardiovasc Qual Outcomes. 2009;2(3):164–169. doi: 10.1161/CIRCOUTCOMES.108.816843. doi:10.1161/CIRCOUTCOMES.108.816843. [DOI] [PubMed] [Google Scholar]
- 4.Elley CR, Kenealy T, Robinson E, Drury PL. Glycated haemoglobin & cardiovascular outcomes in people with Type 2 diabetes: a large prospective cohort study. Diabet Med. 2008;25(11):1295–1301. doi: 10.1111/j.1464-5491.2008.02581.x. doi:10.1111/j.1464-5491.2008.02581. [DOI] [PubMed] [Google Scholar]
- 5.Athanasiou T, Aziz O, Manqoush O, Al-Ruzzeh S, Nair S, Malinovski V, et al. Does off-pump coronary artery bypass reduce the incidence of post-operative atrial fibrillation?A question revisited. European J Cardio-thoracic Surg. 2004;26(4):701–710. doi: 10.1016/j.ejcts.2004.05.053. doi:10.16/j.ejcts.2004.05.053. [DOI] [PubMed] [Google Scholar]
- 6.Halkos ME, Puskas JD, Lattouf OM, Kilgo P, Kerendi F, Song HK, et al. Elevated preoperative HbA1c level is predictive of adverse events after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2008;136(3):631–640. doi: 10.1016/j.jtcvs.2008.02.091. doi:10.1016/j.jtcvs.2008.02.091. [DOI] [PubMed] [Google Scholar]
- 7.Matsuura K, Imamaki M, Ishida A, Shimura H, Niitsuma Y, Miyazaki M. Off-pump coronary artery bypass grafting for poorly controlled diabetic patients. Ann Thorac Cardiovasc Surg. 2009;15(1):18–22. [PubMed] [Google Scholar]
- 8.Kinoshita T, Asai T, Suzuki T, Kambara A, Matsubayashi K. Preoperative hemoglobin A1C predicts atrial fibrillation after off-pump coronary bypass surgery. Euro J Cardio-Thoracic Surg. 2012;41(1):102–107. doi: 10.1016/j.ejcts.2011.04.011. doi:10.1016/j.ejcts.2011.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dublin S, Glazer NL, Smith NL, Psaty BM, Lumley T, Wiggins KL, et al. Diabetes mellitus, glycemic control, and risk of atrial fibrillation. J Gen Intern Med. 2010;25(8):853–858. doi: 10.1007/s11606-010-1340-y. doi:10.1007/s11606-010-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johansen OE, Brustad E, Enger S, Tveit A. Prevalence of abnormal glucose metabolism in atrial fibrillation: A case control study in 75 year-old subjects. Cardio-vascular Diabetol. 2008;7:28. doi: 10.1186/1475-2840-7-28. doi:10.1186/1475-2840-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knapik P, Ciesla D, Filipiak K, Knapik M, Zembala M. Prevalence & clinical significance of elevated preoperative glycosylated hemoglobin in diabetic patients scheduled for coronary artery surgery. Eur J Cardiothorac Surg. 2011;39(4):484–489. doi: 10.1016/j.ejcts.2010.07.037. doi:10.1016/j.ejcts.2010.07.037. [DOI] [PubMed] [Google Scholar]
- 12.Faritous Z, Ardeshiri M, Yazdanian F, Jalali A, Totonchi Z, Azarfarin R. Hyperglycemia or high hemoglobin A1C: Which one is more associated with morbidity & mortality after coronary artery bypass graft surgery?Ann Thorac Cardiovasc Surg. 2014;20(3):223–228. doi: 10.5761/atcs.oa.13.02282. doi:10.5761/atcs.oa.13.02282. [DOI] [PubMed] [Google Scholar]
- 13.Goksedef D, Ömerolu S, Yalvac E, Bitargil M, Ipek G. Is elevated HbA1c a risk factor for infection after coronary artery bypass grafting surgery. Turk J Thorac Cardiovasc Surg. 2010;18(4):252–258. [Google Scholar]
- 14.Sato H, Carvalho G, Sato T, Lattermann R, Matsukawa T, Schricker T. The association of preoperative glycaemic control, intraoperative insulin sensitivity & outcomes after cardiac surgery. J Clin Endocrinol Metab. 2010;95(9):4338–4344. doi: 10.1210/jc.2010-0135. doi:10.1210/jc.2010-0135. [DOI] [PubMed] [Google Scholar]
- 15.Alserius T, Anderson RE, Hammar N, Nordqvist T, Ivert T. Elevated glycosylated hemoglobin (HbA1c) is a risk marker in coronary artery bypass surgery. Scand Cardiovasc J. 2008;42(6):392–398. doi: 10.1080/14017430801942393. doi:10.1080/14017430801942393. [DOI] [PubMed] [Google Scholar]


